The working environment of hairdressers typically involves the use of a vast number of hair products for washing, bleaching, perming, dyeing, and spraying (1). These hair products contain a variety of chemical agents that hairdressers may be exposed to on a continuous daily basis (2, 3). Even though concentrations of single chemicals generally are considered to be low in hairdresser salons (4), the long-term consequences of exposure to the complex chemical mixture are unknown.
Specific chemical ingredients found in hair products have known or suspected hormone-disrupting properties that might interfere with the fetal development of reproductive organs. These compounds include hexane, benzene, toluene and metoxypropanol and endocrine-disruptive chemicals (EDC) (eg, alkylphenolic compounds and phthalates) (4–6). EDC exposures have shown associations with the genital diseases cryptorchidism (incomplete testicular descent) and hypospadias (displacement of the urethral opening along the ventral shaft of the penis) (7, 8). Cryptorchidism is a fairly common condition among boys with a prevalence at three months of age estimated to be 1.9% in Denmark, 1.0% in the USA, and 2.4% in the UK (9–12). In contrast, hypospadias only occurs among 2–4 boys per 1000 male births in Europe (13, 14).
A number of epidemiological studies have addressed whether hairdressers are at increased risk of having children with birth defects compared to women in other professions. Some studies report that female hairdressers have an increased risk of having children with major malformations such as hypospadias (15–17) while others find no support for an increased risk (18–20). Thus, studies have been conflicting, and – so far – no health problems related to reproduction and fetal development have been identified among hairdressers (21). Nevertheless, health concerns persist especially considering pregnant hairdressers.
In this study, we used Danish nationwide registers to collect information about occupational activities and birth defects to assess the possible association between maternal occupation in hairdressing during pregnancy and risk of cryptorchidism and hypospadias among male infants.
Methods
Data sources
Information on childbirths, hospital contacts, and employment status was obtained from the following national registers: the Danish Civil Registration System, the Danish National Patient Registry, the Fertility Database, and the Employment Classification Module from Statistics Denmark. The Danish Civil Registration System is a continuously updated demographic database that covers the entire Danish population (22). It was established on 1 April 1968, after which time all Danish inhabitants have been assigned a unique 10-digit identification number. This register was used to identify children born between 1980–2007. Children and parents were linked through the Fertility Database (23). The Danish National Patient Registry includes information about inpatient hospital contacts in Danish hospitals from 1 January 1977 onwards and outpatient hospital contacts from 1 January 1995 onwards (24) and was used to identify boys diagnosed with cryptorchidism and hypospadias. Since 1976, every person in Denmark ≥15 years old and paying tax has been classified annually according to economic and employment status in the Employment Classification Module, Statistics Denmark (25). This module was used to extract information on the mother’s work during the year of the birth of her children.
Cohort
The cohort included all male offspring born in Denmark from 1 January 1980 to 31 December 2007 and their mothers. We restricted our analyses to male infants of singleton pregnancies whose mothers had an active employment status in the birth year. An active employment status indicated that the most important source of income for a person in a given year came from an employment in the public or private sector.
Exposure
Exposed boys had a mother who was employed as a hairdresser in the birth year while unexposed boys had mothers in other occupations, or specifically mothers working as shop assistants or receptionists (including information clerks). Thus, the three reference groups were (i) all boys with mothers in other occupations than hairdressing, and boys with mothers working as (ii) shop assistants or (iii) receptionists. Shop assistants and receptionists were selected as specific comparison groups due to similarities in educational and socioeconomic backgrounds (shop assistants) and self-exposure to cosmetics (receptionists). It was not possible to identify receptionists as a specific occupational group before 1991, and we thus only included receptionists as a comparison group for the period 1991–2007.
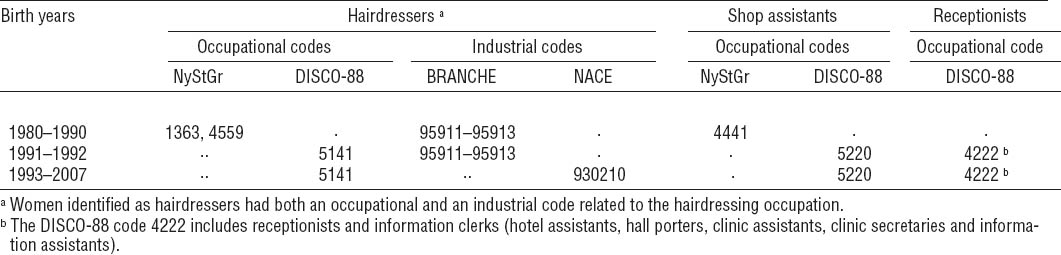
To identify maternal occupation we used occupational and industrial classification codes from the Employment Classification Module, Statistics Denmark. Hairdressers, shop assistants and receptionists were identified as described in table 1. Women categorized in other occupations (including shop assistants and receptionists) had an identifiable occupational and industrial classification code (excluding codes for hairdressers) for the relevant year. Thus, women who were unemployed, retired, or still studying were not included in the group of other occupations.
Table 1
Occupational and industrial codes used to identify maternal occupation as hairdresser, shop assistant and receptionist during birth years from 1980–2007. [BRANCHE=Danish industrial codes (1977–1993); DISCO-88=Danish version of International Standard Classification of Occupations (1991–2007); NACE=Statistical Classification of Economic Activities in the European Community (1992–2007) available from the Employment Classification Module, Statistics Denmark; NyStGr=Danish version of International Standard Classification of Occupations (1980–1995)]
Outcome
Male singleton offspring were followed for the occurrence of cryptorchidism and hypospadias recorded as diagnoses in the Danish National Patient Registry. The study included primary diagnoses of cryptorchidism with International Classification of Diseases (ICD) version 8 codes 75210, 75211, 75219 and ICD-10 codes Q53, Q531, Q532, and Q539 and of hypospadias ICD-8 codes 75220, 75221, 75222, 75228, 75229 and ICD-10 codes Q540, Q541, Q542, Q548, and Q549.
Statistical analysis
Male infants were followed for their first primary hospital contact for cryptorchidism and hypospadias in the time period 1 January 1980 to 31 December 2009. Follow-up began at time of birth (during the period 1980–2007) and continued until a diagnosis of cryptorchidism or hypospadias (analyzed separately), loss to follow-up (emigration, disappearance), death, or end of follow-up (31 December 2009), whichever came first.
We estimated hazard ratios (HR) and 95% confidence intervals (95% CI) using Cox regression to compare the occurrence of cryptorchidism and hypospadias among male infants of mothers working as hairdressers with children of mothers in other occupations. All analyses were adjusted for birth year (1980–1989, 1990–1999, 2000–2007), maternal age (<20, 20–24, 25–29, 30–34, ≥35 years) and parity status (0, 1–2, ≥3 children), and paternal age (<20, 20–24, 25–29, 30–34, ≥35 years).
Supplementary analysis
Supplementary analyses were performed to test the robustness of the main findings. First, we restricted the analysis to firstborns. Second, we restricted our cohort to include only women who did not receive any economical social benefits (ie, women who were employed and not on sick leave) during gestational weeks 8–14 for the birth years 1991–2007. We identified these women through the DREAM database (26), which includes information on all public transfer payments for Danish inhabitants on a weekly basis since 1991. Third, we used a stricter cryptorchidism case definition that only included boys who had both a diagnosis of cryptorchidism and orchiopexy (corrective surgery to move undescended testicles into the scrotum). The boys with orchiopexy were recorded with a KKFH00, KKFH01, or KKFH10 code following the Nordic Classification of Surgical Procedures. Finally, to see if possible associations between maternal occupation and cryptorchidism differed according to birth years (too few cases of hypospadias for this analysis), we compared the associations between maternal occupation and cryptorchidism in specific birth year periods (1980–1989, 1990–1999, 2000–2007).
Results
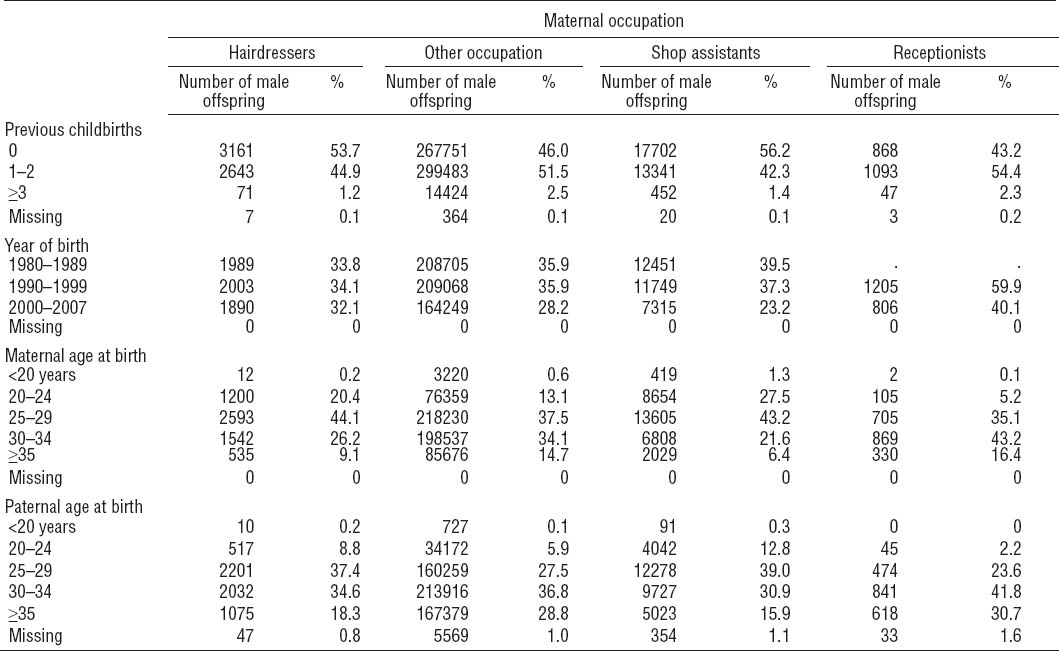
Overall, 924 928 women gave birth to 1 748 881 children in Denmark from 1 January 1980 to 31 December 2007. After excluding 64 382 children from multiple births (including children of pregnancies with unknown number status) and female infants, the cohort comprised 864 747 boys born to 631 904 women. Of these, 587 904 (68%) were born while their mothers were registered with an active employment status (in total 462 523 women). Furthermore, 5882 male infants were born to 4839 maternal hairdressers, 31 515 male infants to 27 483 shop assistants and 2011 male infants to 1840 receptionists. The distribution of male infants according to maternal occupation at birth year and number of previous childbirths, year of birth, and maternal and paternal age at birth is shown in table 2.
Table 2
Distibution of male offspring according to maternal occupation and number of previous childbirths, year of birth, and maternal and paternal age at birth
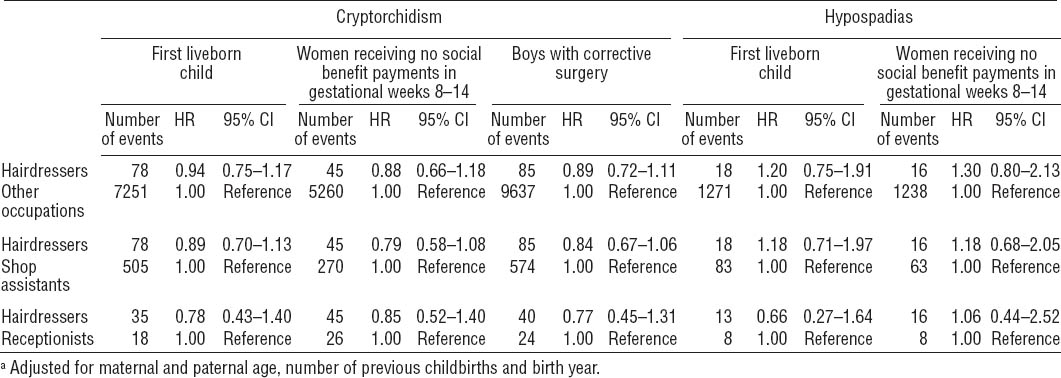
Cryptorchidism
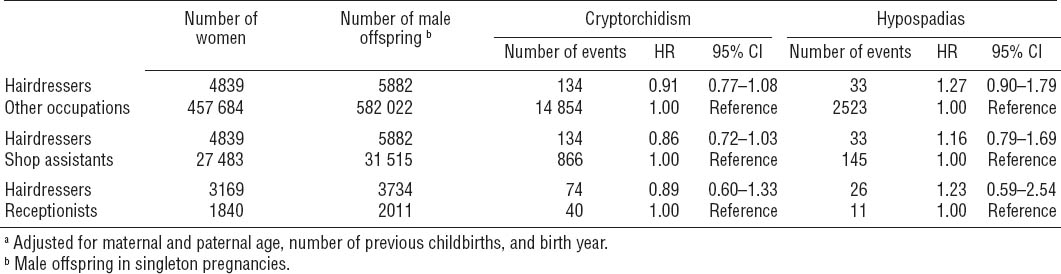
Among the 587 904 boys in the cohort, 14 988 (2.5%) were diagnosed with cryptorchidism during follow-up. Of these, 134 boys had a mother who was employed as a hairdresser during the birth year. This corresponded to an overall HR for cryptorchidism among boys of maternal hairdressers of 0.91 (95% CI 0.77–1.08) compared to boys of mothers in all other occupations. Similar overall associations with cryptorchidism were found when comparing maternal hairdressers with maternal shop assistants (HR 0.86; 95% CI 0.72–1.03) and receptionists (HR 0.89; 95% CI 0.60–1.33) (table 3).
Table 3
Hazard ratios (HR)a of cryptorchidism and hypospadias among boys according to maternal occupation of 462 523 women with 587 904 sons born 1980–2007. [95% CI=95% confidence interval.]
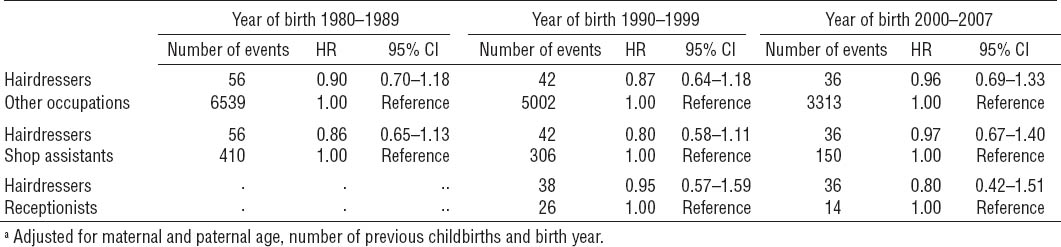
In the supplementary analyses (tables 4 and 5), we observed HR for cryptorchidism among boys of hairdressers similar to those of the main analysis when we restricted our analyses to: (i) first liveborns (in total 270 912 male infants); (ii) women who did not receive any social benefit payments during gestational weeks 8–14; (iii) cases of cryptorchidism to boys who were also treated with orchiopexy in total comprising 9722 children; and (iv) stratifying by birth year (1980–1989, 1990–1999 and 2000–2007). The latter analysis specifically showed that HR were consistent across birth years and that, at none of the studied birth year periods, boys of maternal hairdressers were at significantly increased or reduced risk for cryptorchidism (table 5).
Hypospadias
Altogether 2556 boys (0.4%) were diagnosed with hypospadias in the study period, 33 of whom had a mother employed as a hairdresser within the birth year. Compared to the risk among boys of mothers in other occupations, this corresponds to a HR of 1.27 (95% CI 0.90–1.79) for boys of hairdressers. The HR for hypospadias among boys of hairdressers were 1.16 (95% CI 0.79–1.69) and 1.23 (95% CI 0.59–2.54) compared to boys of maternal shop assistants and receptionists, respectively (table 3).
Restricting the cohort to first liveborn children, the analysis provided similar results, ie, the risk of hypospadias was approximately the same regardless of maternal occupation (table 4). In the analysis restricted to the subset of women who did not receive social benefit payments during gestational weeks 8–14, the results were consistent with those of the main analysis (table 4).
Discussion
We compared the risk of cryptorchidism and hypospadias among boys of mothers working as hairdressers with boys of mothers in other occupations using one of the largest cohorts to have assessed the risk of male reproductive tract malformations in offspring of hairdressers. The salient observation was that the risk of cryptorchidism and hypospadias did not differ among boys born to maternal hairdressers compared to other boys.
Both cryptorchidism and hypospadias are malformations that can be treated with a good prognosis. However, men with a history of undescended testes may have reduced spermatogenic function and possibly reduced fertility in adulthood, especially if the condition is left untreated for a prolonged period of time (27, 28). The development of male reproductive organs depends on androgens and a balanced androgen–estrogen ratio. Therefore, it has been suggested that exposure to high levels of chemicals that interfere with the production or action of sex hormones might disturb the male reproductive tract development (7). This hypothesis has been supported by a number of previous observations. In a Spanish case–control study, placental levels of xenoestrogenic activity were increased among children with cryptorchidism or hypospadias compared to children without these genital tract malformations (29). Assessments of possible adverse health effects of chemicals have generally been restricted to single chemical compounds and not mixtures. One group of chemicals that has been given particular focus is the EDC with possible effects of maternal occupational exposure mostly assessed through a job exposure matrix where hairdressers constituted one of the largest single occupational groups with a probable exposure to EDC (6). These studies have generally included hypospadias as an outcome but not cryptorchidism. Studies from Australia, Italy, and Denmark have shown relative risks of 1.3–2.4 for hypospadias among boys of mothers with a potential exposure to EDC during pregnancy compared to boys of mothers in occupations where EDC exposure is unlikely (30–32). Moreover, an English case–control study found that occupational exposure to hair spray was associated with a relative risk of 2.3 for hypospadias. Although hairdressers as a group displayed a 2.7-fold increase in risk, this did not reach statistical significance (33). Two Swedish cohort studies have assessed the reproductive outcomes of hairdressers and found a relative risk of 1.3 of major malformations, including hypospadias, in a study from 2002 but found no association in a more recent study from 2005 (17, 18).
The results of the current study do not support the notion that boys of female hairdressers are at increased risk of cryptorchidism and hypospadias. Although we only identified 33 boys with hypospadias among children of hairdressers, our findings are in line with other studies on hairdressers reporting no association with hypospadias (18, 19), cryptorchidism (32), or malformations in general (20). Presumably the levels of exposure to chemical agents, for instance with endocrine-disrupting properties, in hairdressing salons are of insufficient magnitude to interfere adversely with the development of the male reproductive tract. The exposure level has plausibly been reduced within the last decades due to a ban of some hazardous chemicals and increased attention to working conditions (eg, in relation to ventilation) (2, 34). It might thus be expected that children of hairdressers born in the 1980s or 1990s had a higher exposure and thus possibly a higher relative risk than children born in the 2000s. However, our results do not suggest that boys of hairdressers born in earlier recent decades were at higher risk than other children born in the same years.
Shop assistants and receptionists were chosen as specific comparison groups to minimize the potential confounding effect of socioeconomic-related factors and personal use of cosmetics. Hairdressers and shop assistants were assumed to have the same level of education, income, and other socioeconomic factors, while receptionists were assumed to have a personal use of cosmetics similar to that of hairdressers. We found the risk of cryptorchidism and hypospadias to be similar among sons of hairdressers and the various comparison groups.
We tested the robustness of our findings in supplementary analyses that were restricted to (i) women who had not previously given birth to liveborn children; (ii) occupationally active women who did not receive any social benefit payments in gestational weeks 8–14, thus increasing the probability that these women were actually working during the gestational period assumed to represent the most important time window for perturbation of development of the male reproductive tract (35); and (iii) cryptorchidism cases with corrective surgery (orchiopexy). Taken together, the consistent and comparable results provided additional support for the finding that the hairdressing occupation is not a high-risk occupation for maldevelopment of the male reproductive tract.
Our study has some potential limitations that need consideration. Congenital cases of transient cryptorchidism may never be clinically recognized and recorded in the Danish National Patient Registry because spontaneous descent is frequent during the first months of life. Furthermore, it has been shown that the register-based cumulative incidence of cryptorchidism and hypospadias in the Danish population increases after the age of 10 (32, 36). Thus, studies relying on register-based recordings of cryptorchidism may likely, to some degree, underestimate mild and transient cases of cryptorchidism. Furthermore, an unknown proportion of mild hypospadias are never hospitalized. Therefore hypospadias reported in the Danish National Patient Registry presumably to a larger degree include more severe than mild cases. Nevertheless, the observed prevalences of 2.5% and 0.4% of cryptorchidism and hypospadias, respectively, in the cohort of sons of employed mothers resemble those reported in other studies (9–14), and high positive predictive values have been found for the diagnosis of cryptorchidism (80%) and the registration of orchiopexy (99%) in the Danish National Patient Registry (37). Finally, the Danish healthcare system is free of charge and accessible to all Danish citizens, and we do not expect underestimation of cryptorchidism and hypospadias to differ between the occupational groups examined in this study. We used the Employment Classification Module provided by Statistics Denmark to determine each individual’s affiliation to the Danish labor market. The Employment Classification Module includes information on the most important employment activity in terms of income throughout each year and, although this information has not been validated, the register is generally considered to be of high quality (25). The total number of women employed as hairdressers in Denmark at some time point during the study period is likely considerably higher than the 4839 women identified in this study; for instance, the Danish Hairdressers and Beauticians Union report that they had 5374 members in 2006. However, this discrepancy was expected as we only included that subset of women who conceived during their employment as hairdressers. Also, when identifying women as hairdressers, we required occupational and industrial classification codes that were specifically related to employment as a hairdresser and in a hairdressing salon, respectively. Consequently, the specificity of women categorized as hairdressers in this study is likely high.
Concluding remarks
This study found no evidence for an increased risk of malformations of the male reproductive tract among boys of maternal hairdressers. It must, however, be stressed that exposure levels and prevalence within the hairdressing occupation may vary substantially, and thus we cannot exclude the possibility that the occupational environment for some hairdressers might potentially disturb fetal development, including urethral fusion and testicular descent. However, when considering the hairdressing occupation as a whole, our findings show that boys of maternal hairdressers have the same risk of cryptorchidism and hypospadias as boys of mothers in other occupations.