Occupational injuries continue to place a tremendous burden on workers as well as employers globally with an estimated 100 million occupational injuries occurring worldwide each year (1). Musculoskeletal disorders (MSD), often referred to as ergonomic injuries, also remain prevalent and often result in a substantial burden of disability and high associated costs (2). For 2011, the US Bureau of Labor Statistics (BLS) reported >2.8 million cases of nonfatal occupational injury among private industries, of which >50% resulted in days away from work, job transfer, or work restriction (3). MSD accounted for 33% of all workplace injuries and illnesses requiring time away from work in 2011 (3). Despite a decline in recent years in both the incidence rate and the number of occupational injuries and work-related MSD, these occupational disorders remain a large burden to society in general and workplaces in particular because of lost productivity, reduced performance, lost-time claims, and medical costs among affected workers in the short term (4–6) and likely effects on turnover, job engagement, and morale over time.
A wide range of physical and psychosocial exposures and work organizational and individual factors (such as anthropometrics, body mass index, disease status, sex, job tenure and hours worked) contribute to increased risk for occupational injury and MSD (6–13). Consequently, individual worker risk can vary markedly even for workers performing identical job tasks. This well recognized, multifactorial nature of causation contributes to the difficulty in studying the impact of ergonomic interventions on injury outcomes.
Physical workplace exposures related to job tasks, workplace environment, and use of tools and materials affect workers in many different occupations and are strongly associated with injury risk (14–18) with some evidence for an exposure–response relationship (14, 19, 20). These exposures may include forceful exertions involved in manual handling; awkward postures of the neck, back, and lower extremities; repetitive motions; contact stress; segmental and whole-body vibration; and exposure to temperature extremes. A recent estimate of physical workplace exposures among the US workforce reported that 27% of workers are exposed continually to repetitive motion, 25% spend more than half of their time at work bending or twisting, 10% are exposed to cramped work spaces that require assumption of awkward postures every day, and 2.7% are exposed to whole body vibration (21).
Recognizing the contribution of these physical workplace exposures to injury and MSD risk, a variety of workplace ergonomic interventions have been implemented to address ergonomic hazards with differing degrees of reported success using a range of outcome measures (19, 22–26). A multifaceted ergonomic approach to risk control with active participation of workers in the process can be an effective means of reducing injury risk from workplace exposures (22). But the evidence for the effect of this participatory ergonomics approach on different outcomes is mixed with some studies showing a positive impact on worker morale and job satisfaction, but failing to show any effect on injury risk, and others showing a reduction in injury incidence, severity, and/or cost (25–27). Still, many countries now require employers to manage the risk of injury with participation of at-risk employees in the process (28, 29).
Despite the burden of exposure to ergonomic hazards among US workers and evidence that modification of workplaces to better suit workers can be effective in reducing risk for injury through participatory ergonomics and others means (19, 30–32), specific ergonomic regulatory requirements are lacking in the US. Although voluntary ergonomics guidelines exist for several industries (33), recent research suggests that, without the plausible threat of enforcement, such efforts may do little to encourage action by employers most in need of improvement (34).
Operating in the US and around the world, a multinational producer of aluminum and related products undertook a focused company-wide effort to identify and control ergonomic hazards in production and maintenance jobs across all operating plants. The effort began in 2001 with a company mandate requiring each operating plant to (i) identify the ten job tasks most in need of ergonomic improvement and (ii) implement controls for at least half of these problem tasks by the end of 2003. This initiative served as a precursor to the company’s adoption of a mandatory ergonomics standard in late 2001, which was modeled to a large extent on the briefly promulgated, then rescinded, OSHA ergonomics rule. Beginning in 2004, plants were required to conduct job task-based quantitative ergonomic risk assessments to identify all ergonomic hazards, save them to the company’s ergonomic hazards database, and implement adequate controls for half of those hazards by the end of 2006. As hazard controls (HC) were implemented, the ergonomic hazards database was updated to reflect new HC.
The primary objective of this study was to examine whether the job-task-based ergonomic hazard identification, quantification, and control intervention resulted in injury risk reduction for incumbent workers in jobs for which HC were implemented for one or more identified ergonomic hazards. A secondary objective was to examine whether any associated injury risk reduction differentially impacted risk for MSD versus acute traumatic injuries in this population. A final objective was to examine whether or not controlling more than one ergonomic hazard in a job further reduces injury risk.
Methods
All data used for this study are available through a unique academic-corporate partnership that began in 1997 for the purpose of developing and implementing workplace safety and occupational health policies for this large, multisite aluminum manufacturer.
Intervention
To facilitate the company’s ergonomic HC initiative, each operating plant within the study company was required to use and report the results of a quantitative ergonomic risk assessment using a tool such as the NIOSH Lifting Equation (35), Liberty Mutual Psychophysical tables (36), Rapid Upper-Limb Assessment (RULA) (37) or the Quick Exposure Check (QEC) (38), in combination with: number of workers exposed, frequency of exposure, history of any injury associated with the task and estimated cost of implementing ergonomic HC into a specified algorithm with a pre-determined hazard threshold to determine whether the specified job task constituted an ergonomic hazard (Appendix A available at http://www.sjweh.fi/data_repository.php). Of note, the history of injury was not limited to MSD, but included any injury that could have been related to task design or execution. Job tasks meeting or exceeding the pre-determined hazard threshold were required to be reported into the company’s ergonomic hazards database. In order to establish that adequate control had been achieved for each ergonomic HC implemented, reanalysis was conducted with control(s) in place using the same risk assessment methodology and algorithm and reporting of results. Once adequate control was achieved for a specified ergonomic hazard, that hazard was flagged in the database as controlled. A wide variety of ergonomic hazards that met the pre-determined hazard threshold were identified across jobs at the 17 plant locations. Examples of identified ergonomic hazards include repeated manual handling of solid aluminum I-beam spacers, manual handling of 110 lb banding coils, hammering valves, and opening/closing pot hoods. Examples of HC that were successfully implemented include developing a smaller, lighter weight I-beam spacer with improved hand-hold design, installing hammerless valve technology, and redesigning the pot hoods to facilitate easier opening and closing.
Study cohort and data
Manufacturing production and maintenance workers (hourly workers) at 17 geographically diverse US operating plants representing a variety of aluminum manufacturing businesses were chosen for study as these plants were active throughout the study period. Workers in management positions (salaried workers) were excluded. Aluminum manufacturing processes represented by these plants include smelting, fabricating, refining, forging, and casting.
Hourly workers contributing any active work time between 1 January 2001 and 31 December 2006 in jobs for which at least one ergonomic hazard was identified in the ergonomic HC database, regardless of HC implementation, comprised the cohort. Workers in jobs for which adequate controls were implemented for one or more of the identified ergonomic hazards constituted the HC or treatment group while workers in the jobs for which no controls were implemented for identified ergonomic hazards comprised the reference or NoHC group.
The human resources database, which contains complete demographic and job history by job title and dates of job change for each employee, as well as employee type (hourly or salary), sex, date of birth, plant location, plant origin (recent acquisition, yes/no), date of entry into the workforce, and where applicable, date(s) of leave, termination, and date(s) of reentry was used to construct job histories for each hourly worker at the 17 study plants and calculate person-time worked for each job held during the study period.
Using the process previously described for this population (12), job titles have been standardized across the various plants and company databases into standardized job categories to enable linkage of exposure information collected by job title to the appropriate individual workers and/or groups of workers exposed. Exposure to ergonomic hazards and ergonomic HC implementation were assigned to the impacted workers and/or groups of workers using these standardized job categories. For the hourly worker population across the 17 plant locations included in this study cohort, there were 59 standardized job categories for a total of 123 unique plant jobs.
Outcome measure
Injury histories for each hourly worker in each job held during the study period were constructed using the incident surveillance database, which contains information on all injuries and illnesses resulting from events or exposures occurring in the workplace. Longstanding company policy requires reporting of all injuries regardless of severity. In the incident surveillance database, injury events are described by a nature of injury variable, which was used to identify all injuries and MSD to include in the analysis. A detailed description of this data system has been published previously (12, 13). Because the company’s ergonomic hazard identification and control implementation process was aimed at any exposure that could cause either acute traumatic injury or more cumulative MSD, all injury events occurring between 1 January 2001 and 31 December 2006 were included for analysis; separate analyses were performed for MSD and acute traumatic injuries.
An encrypted uniform unique identifier was created for each employee to ensure human subject privacy. This unique identifier was used to link the human resources and incident surveillance databases to construct individual job and injury histories for the hourly worker population. The standardized job category was used to link each job in the ergonomic HC database to the corresponding job in the human resources database to determine all workers exposed to identified ergonomic hazards and potentially impacted by any ergonomic hazard controls that were implemented. Using this linkage strategy, for each job held during each year of the 6-year study period, the number of injuries per person-job, and the amount of person-time contributed in that person-job was determined. The number of ergonomic hazards identified and the number of those identified ergonomic hazards for which controls were implemented during the study period was assigned by job for each person-job in the study cohort.
Yale University School of Medicine Human Investigations Committee granted ethical approval for this study.
Statistical methods
Descriptive analysis of demographic characteristics for the study cohort and distribution of the injury outcomes of interest stratified by HC or NoHC group was performed. The effect of implementing HC for one or more job-task-level ergonomic hazards on the relative risk of injury by person-job was modeled for the study cohort using a random coefficient model (39) to account for repeated measures on person-jobs and allow for between-person variation in any effect of ergonomic HC with NoHC as the reference group. A Poisson distribution was chosen with a log link and an offset of person-time contributed to each person-job for each year of the study.
Separate analyses were conducted for each injury outcome of interest, including any injury or MSD, MSD only, and acute, traumatic injuries only. Fixed effects included sex, age, plant origin, and year to control for any difference in temporal trend in injury risk during the 6-year study period between the HC and NoHC groups. Because initial model results indicated that the effect of year was non-linear, year was included as a categorical variable in the final models. Plant origin was included as a dichotomous variable to adjust for differences between new plant locations acquired one year before the start of the study period and plants more accustomed to company safety culture. The intercept for each person-job was modeled as a random effect. For each analysis, an unstructured covariance structure was specified. The variance of the Pearson residuals was examined to ensure that the Poisson distribution appropriately fit the data.
Further analysis of the HC group only was performed, again using a random coefficient model described above and including as a linear effect the number of controlled ergonomic hazards to examine the impact of successfully implementing HC for multiple identified ergonomic hazards within a job. Finally, to ensure that any differences in effect between the HC and NoHC groups were not attributable to longstanding group differences in injury risk, the relative risk (RR) of injury by person-job for the pre-intervention period (1997–2000) was modeled for the subset of plants for which data was available during those years, adjusting for sex, age, and year.
All statistical analyses were performed with SAS version 9.3 (SAS Institute, Cary, NC, USA).
Results
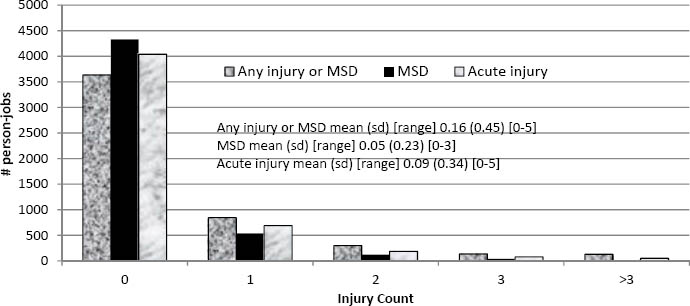
Over the 6-year study period, among a total hourly worker population of 24 041 at the 17 study plants, 14 540 individuals worked in 123 unique plant jobs between 1 January 2001 and 31 December 2006 that were targeted by the ergonomics initiative with at least one ergonomic hazard identified and quantified in one of the job tasks comprising the job. Among the study cohort of 14 540 workers (25% female, 75% male) in 18 013 person-jobs during the 6-year study period, 4604 workers sustained 8624 injuries, including minor injuries requiring first aid treatment only (table 1). The number of measurements by person-job during the 6-year study period ranged from 1–6 with a median of 3 for the HC group and 2 for the NoHC group.
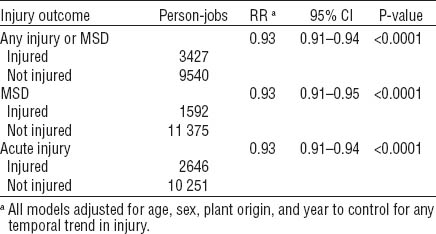
Table 1
Descriptive statistics of covariates and injury distribution by group. [HC=ergonomic hazards identified, controls implemented for ≥1 hazard; NoHC=ergonomic hazards identified, 0 controlled; MSD=musculoskeletal disorder; SD=standard deviation]
Female workers comprised 26% of the person-jobs in the HC group and 22% in the NoHC group. The distribution of injury outcome by sex varied between the groups with 25% of the injury outcomes in the HC group affecting female workers and 27–32% of the injury outcomes in the NoHC group affecting females. The distribution of injury by number of injuries and type (any injury or MSD, MSD only, or acute traumatic injury only) is displayed in figures 1A and 1B for the HC and NoHC groups, respectively.
Figure 1A
Distribution of injury among person-jobs in the HC group (ergonomic hazards identified, controls implemented for ≥1 hazard). [MSD= musculoskeletal disorder; SD=standard deviation]
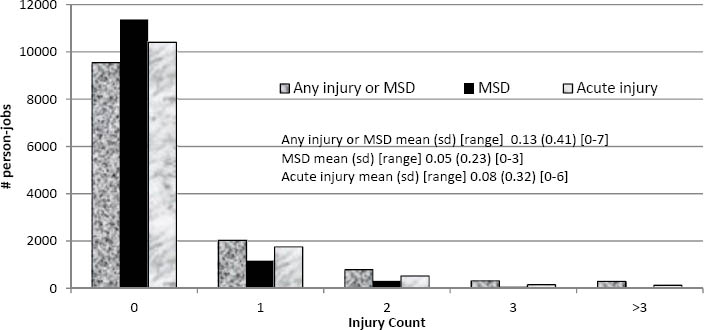
Figure 1B
Distribution of injury among person-jobs in NoHC group (ergonomic hazards identified, 0 controlled). [MSD= musculoskeletal disorder; SD=standard deviation]
Across the 123 targeted plant jobs, 347 ergonomic hazards were identified with quantitative ergonomic risk assessment using the pre-determined hazard threshold. HC were implemented for 204 of the identified hazards across 84 plant jobs. Among jobs comprising the HC group, an average of 4.7 ergonomic hazards were identified per targeted plant job (range 1–22) and HC were implemented for an average of 2.8 identified ergonomic hazards during the study period (range 1–14). Among jobs in the NoHC group, an average of 1.5 ergonomic hazards was identified per targeted plant job (range 1–4) with none of the identified hazards undergoing control implementation during the study period.
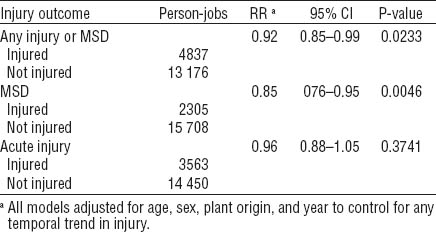
Adjusting for age, sex, plant origin, and year, persons within jobs in the HC group displayed reduced risk for any injury or MSD [RR 0.92, 95% confidence interval (95% CI) 0.85–0.99] and reduced risk for MSD only outcomes (RR 0.85, 95% CI 0.76–0.95) compared to persons within jobs in the NoHC group (table 2). There appeared to be a similar protective effect for acute, traumatic injuries only; however, this effect was not statistically significant at P=0.3742. During the four years prior to the start of the ergonomic initiative (1997–2000), there were no differences in injury risk between the two groups (data not shown) for the subset of plants for which data was available.
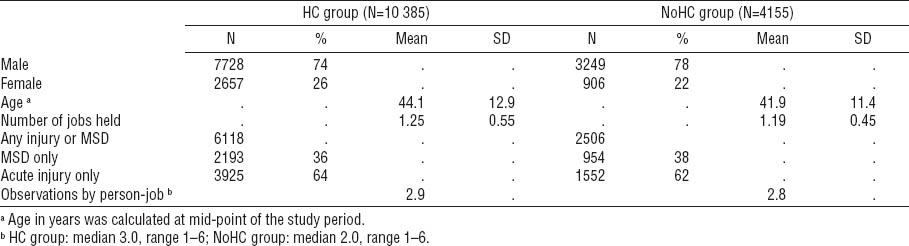
Table 2
Comparing HC (ergonomic hazards identified, controls implemented for ≥1 hazard) and NoHC (ergonomic hazards identified, 0 controlled: reference) group, association of ergonomics hazard control implementation with risk of injury or musculoskeletal disorder (MSD) [RR=relative risk; 95% CI=95% confidence interval.]
Examining only the persons within jobs in the HC group, each ergonomic hazard controlled was associated with an injury risk reduction of 7% [any injury or MSD: RR 0.93, 95% CI 0.91–0.94; MSD only: RR 0.93, 95% CI 0.91–0.95; acute injury only: RR 0.93, 95% CI 0.91–0.94 (table 3)]. This 7% RR reduction for each ergonomic hazard controlled equated to a reduction of 5 injuries or MSD per 100 person-years within the study population. Examination of the Pearson residuals revealed no evidence of over dispersion.
Discussion
In this study, we show an association between systematic ergonomic HC implementation and injury risk reduction in a population of industrial workers performing a diverse array of jobs in a variety of aluminum manufacturing businesses. Although the injury risk reduction achieved in the HC compared to the NoHC group was, not surprisingly, greatest for MSD, the ergonomic HC initiative was also associated with reduced risk for any injury or MSD and showed a trend toward reduced risk of acute traumatic injury in the study cohort, though this latter finding did not achieve statistical significance.
The study company began drafting an internal ergonomics standard in 2000 when the OSHA ergonomics rule was imminent (40). Because company data indicated that approximately one-third of reportable injuries were musculoskeletal in origin, the company ergonomics standard, modeled largely after the OSHA rule, was adopted during the fall of 2001 despite revocation of the OSHA requirement by the US Congress in early 2001. Believing that acute injuries as well as MSD could result from hazards potentially modifiable through ergonomics, the scope of company-mandated ergonomic hazard identification and control intervention was not limited to job tasks for which cumulative exposures might contribute to MSD, but included identification and control of ergonomic hazards with potential to contribute to any injury type. Additionally, the company ergonomics standard required that all employees receive basic ergonomics training, and required each plant to designate an ergonomics task force comprised of both hourly and salaried personnel to spearhead plant ergonomic activities, members of which received more in-depth ergonomics training including how to perform ergonomic risk assessment.
Across the 17 study plants a total of 347 ergonomic hazards were identified and quantified, and 204 were controlled in 123 plant jobs in which 14 540 job incumbents worked during the study period. Each of these job incumbents was at potential risk of work-related injury given the quantified ergonomic hazard(s) in one or more of their job tasks. Because of the contributory role that individual and psychosocial factors play in MSD and injury risk (12–16), exposure to physical ergonomic job hazards is recognized as conferring differential risk of work-related injury to individual workers who are highly variable in terms of anthropometrics, age, sex, disease status, etc. To thoroughly examine the effect of the ergonomic HC initiative on injury risk, a cohort of all hourly workers in jobs with any quantified ergonomic hazard(s) was selected, regardless of the workers’ individual injury experience, as the presence of one or more ergonomic hazards theoretically placed each incumbent at potential risk for injury. Highlighting the divergent injury susceptibility of individuals who perform identical job tasks, 68% of the study cohort sustained no injury or MSD during the study period (N=9936), while 4604 of the study cohort (32%) sustained 8624 acute injuries and MSD.
Critical to this analysis is the comparability between the jobs in the HC and NoHC groups. In an attempt to quantify injury risk between the groups, we modeled acute and MSD injury rates for all job categories prior to the intervention. There was no detectable difference between the HC and NoHC group injury rates, indicating that the injury risks were the same. Given this result, we conclude that the ergonomic initiative, not the selection of the tasks for control implementation, best explains the change in RR after the intervention was undertaken. However, more ergonomic hazards were identified for plant jobs in the HC group on average (mean 4.7, range 1–22), compared to the NoHC group (mean 1.5, range 1–4). There are several possible explanations for this finding. First, it is possible that plant jobs in the NoHC group contained fewer ergonomic hazards than plant jobs in the HC group; however, this would likely have been reflected in divergent injury rates between the two groups prior to the intervention. Second, because plants had autonomy in choosing which hazards to control, some may have prioritized those hazards that had the highest risk score or affected the greatest number of employees while others may have prioritized those hazards that were deemed less expensive to control than others. Of course, different plants may have made different decisions for similar hazards. For example, five of the study plants identified hazards in the pot room operator job; at two plants workers in this job were included in the HC group while, at the other three plants, pot room operators were included in the NoHC group. Two plants identified the same task, pulling bath chunks, as an ergonomic hazard; one plant controlled this hazard while the other did not. Again, this suggests that the jobs in the two groups were not markedly different. Third, the hazard identification process may have been less comprehensive for plant jobs in the NoHC compared to the HC group. Unfortunately, an evaluation of the completeness of the ergonomic hazard identification and prioritization process across study plants is not possible without additional data.
While reduced risk of MSD and acute injuries associated with manual handling has been shown with ergonomic job modifications in several studies (19, 22, 25), to our knowledge this is the first report highlighting the benefit of ergonomic hazard identification and control implementation on risk for any type of acute injury or MSD in an industrial population. Researchers have recently encouraged application of an ergonomics process to identify and mitigate work organizational and psychosocial demands that contribute to injury risk in addition to MSD risk (41). Despite evidence that ergonomic initiatives can positively impact production, worker perception, worker morale, and job satisfaction in manufacturing and other work environments (32, 42, 43), evidence showing positive impact of ergonomic HC on injury risk reduction across a diverse group of workers and jobs has been somewhat limited and conflicting to date (2, 22–24, 27). Several factors are responsible for these issues. First, the differential contributory role played by individual, psychosocial, physical, and organizational factors in MSD and injury risk, makes study difficult (7, 44). Second, benefit derived from ergonomic initiatives may be masked by production rationalization measures that can result in increased risk (45).
In a report describing existing evidence-based best ergonomics practices for prevention of MSD from various systematic reviews, Amick et al (9) suggests that ergonomic best practices focus on integrated approaches to HC rather than on specific ergonomic tools and procedures. This study provides evidence that a systematic approach to ergonomic hazard identification, quantification and control implementation, in conjunction with requirements to establish an ergonomic process at each manufacturing plant, may be effective in reducing risk of MSD and acute injury outcomes among workers in targeted jobs. Our results showing that each additional ergonomic hazard controlled was associated with risk reduction of 7% for MSD and acute injury suggests that the broad scope of the study company’s ergonomic hazard identification and quantification process was effective in focusing attention on job tasks conferring acute injury as well as MSD risk.
The company ergonomics mandate specified a control target of half of all identified ergonomic hazards present in job tasks by the end of the study period for each plant. This mandate translated into the study plants identifying and quantifying between 1–22 ergonomic hazards present among the job tasks comprising targeted plant jobs and implementing changes that resulted in HC for between 0–14 ergonomic hazards for each targeted job. Because ergonomic hazards vary by industry as well as occupation within an industry, identifying workplace physical ergonomic hazards and workers exposed is a crucial first step in mitigating these exposures. However, in the absence of specific requirements to identify and control ergonomic hazards in the workplace with the threat of enforcement, action in this regard may be limited as illustrated by a report which describes the potential risk reduction brought about by the Washington State ergonomics legislation and the reversal of that effect after the rule was repealed (34).
This study has significant strengths, including a large, geographically diverse population of industrial workers exposed to a variety ergonomic hazards in their job tasks; access of investigators to complete worker job and injury history as well as ergonomic hazard identification and control data contained in company maintained databases rather than relying on worker self-report; and familiarity of the research team with company health and safety policies, businesses and jobs. Limitations include lack of available information on other potential individual risk factors for injury, such as hours worked and body mass index; lack of available information on psychosocial workplace exposures and work organizational factors for the study cohort; lack of available data to confirm an equally thorough ergonomic hazard identification process for all plant jobs across study locations; and lack of information on other potential injury reduction initiatives that overlapped the timing of the ergonomic HC initiative. Including year as a covariate in the statistical models helped to reduce the likelihood that our study results are confounded by a downward temporal trend in injury rates. Future analyses will explore any differential impacts of the ergonomic HC process on female workers, examine longer-term effects of ergonomic HC implementation on injury risk and investigate whether HC implementation in targeted jobs impacted other outcomes such as unscheduled absences among the workforce.
Concluding remarks
In this study we show evidence of a substantial, positive impact of systematic ergonomic HC implementation on worker MSD and injury risk in a large industrial cohort. Systematic ergonomic HC implementation was associated with reduced risk for all injuries as well as MSD only. Among the subset of workers in the HC group, implementing controls for each additional ergonomic hazard was associated with reduced risk for each injury outcome examined. Although the specific ergonomic hazards as well as the optimal controls to mitigate those hazards vary from job to job and industry to industry, these study findings highlight the potential for systematic, participatory ergonomic hazard identification and control implementation initiatives to reduce worker injury risk effectively, especially when such initiatives are required by companies or jurisdictions.