Irregular and long working hours, as well as the crossing of time zones are common working conditions of flight crew members, which can lead to a disturbance of the normal sleep/wake pattern and accompanying body functions (1, 2). Short-term effects of these working conditions include digestive problems, fatigue, sleep loss, and an impaired performance capability (3). On the longer term, fatigue and circadian disruption have been associated with a disturbed work–life balance (4), metabolic disturbances (5, 6), cardiovascular diseases (7), gastrointestinal disorders (8), and cancer (9–11).
Fortunately, several studies have shown that circadian disruption can be mitigated by optimizing the timing of exposure to daylight and sleep (2, 12). Furthermore, the optimal timing of physical activity and intake of specific nutrients can enhance sleep duration and quality, and stimulate alertness or relaxation (12–14). In the aviation industry, attempts have been made to translate this knowledge into educational training programs to help flight crew members cope with their flight schedules and accompanying circadian disruption (15, 16). However, few studies evaluated the effects of such programs. Some of these studies combined their educational interventions with alterations in flight schedules, for which it was impossible to address the measured improvements to the programs alone (17, 18). Other studies found improvement in knowledge, awareness (19), layover sleep, and in-flight alertness among flight crew (20) after short-term application of fatigue management advice, but did not measure the effects on the longer term. Altogether, both the short- and long-term effects of educational programs for flight crew members remain unclear.
Web-based interventions aiming at primary prevention have been shown to have positive effects on health knowledge and behavior among adults. The advantage of these types of interventions is that they are able to improve behavior by tailoring information and advice to the specific needs of the individual (21, 22). In recent years, it has become possible to provide such tailored interventions using custom-made mobile applications (apps). In the field of mobile health (mHealth) – the use of mobile devices in healthcare and public health – apps have gradually gained ground due to improvements in technology and an increased usage of smartphones and tablets (23). However, although there are indications that web-based and text messaging interventions can have positive effects on health knowledge and behavior of adults (22, 24), the evidence for such effects of mobile apps is still very limited (25, 26).
Regarding the development of an educational program for flight crew members to cope with irregular working hours, an app would make it possible to translate the relevant information into practical and specific advice, while taking into account the duration and destination of the flight and the number of time zones crossed (16). Moreover, an app would enable the flight crew members to consult personalized advice at any time and place, before, during, and after their flights.
The aim of this study was to investigate the effects of an mHealth intervention among airline pilots consisting of tailored advice on exposure to daylight, sleep, physical activity, and nutrition. We hypothesized that, compared to a minimal intervention, the easy obtainable, tailored advice would improve health-related behavior, resulting in a reduction of sleep problems and fatigue and an improvement in health perception.
Methods
Design
A two-armed randomized controlled trial (RCT) was performed to evaluate the effectiveness of the MORE Energy mHealth intervention. The intervention strategy was developed after focus group interviews with a random sample of 30 pilots, and interviews with key management stakeholders of the airline company. The airline pilots emphasized that they would like to receive advice that was available at any time and place, usable by all types of pilots, dependent on the specific flight schedule, and easy to apply. As a result, it was decided to develop a mobile application in order to transfer the advice to the target population. A detailed description of the development and design of the study has been published elsewhere (27). The Medical Ethics Committee of the VU University Medical Center (Amsterdam, the Netherlands) assessed the study design and procedures, but according to Dutch law, this study proved to be exempt from a medical ethical review.
Participants
The study population consisted of the pilots of all aircraft units of a large internationally operating airline company. The pilots could participate in the study if they were not on sick leave for more than four weeks at the time of recruitment and if they owned a smartphone or tablet with an Android or iOS (iPhone/iPad) operating system. All 2222 potential participants were made aware of the project by means of a publicity campaign, using intranet, internet, and news bulletins. Afterwards, pilots were invited to participate through an information brochure, which was put in their letter box at work. In this brochure, it was explained that by completing the baseline questionnaire, the pilots gave their consent to participate in the study. In addition, it was mentioned in the brochure that the participants could withdraw from the study at any time, without giving any reason. At the end of the brochure, the pilots were directed to an email with a link to the baseline questionnaire (T0).
Randomization
Using the minimization method (28), the researchers randomized participants equally into either the control or intervention group after they had completed the baseline questionnaire. Minimization ensures that the group allocation of the next participant enrolled in the trial takes into account the characteristics of those participants already enrolled, aiming to minimize the imbalance across multiple factors. The factors that were considered for minimization were aircraft unit (five units) and job title (captain, first officer, and second officer).
Intervention group
Participants randomized into the intervention group received an email containing an instruction manual and unique login details for the mobile application that was available in the app stores for iOS and Android and a secure part of the project website (www.more-energy-project.nl). As a result, the content on both the app and the website was only available for the intervention group of this study. The MORE Energy app contained advice tailored to flight schedules and personal characteristics aiming to reduce fatigue and circadian disruption as much as possible. The advice was evidence-based and discussed with experts in the field of chronobiology, physical activity, and nutrition. Flight schedule characteristics included haul type (short- versus long-haul), flight direction (neutral, eastward, westward), departure time (morning, afternoon, evening/night), arrival time (morning, day, night), return time (morning, afternoon, evening/night), and the number of time zones crossed (<4 versus ≥4). In accordance with previous studies (15, 20), the intervention group participants were advised either to hold on to the home-based time or adjust to the local time, depending on the length of the layover (<48 versus >48 hours). In contrast to the studies mentioned, the MORE Energy app enabled users to switch manually between the advised time (local or home-based), depending on their personal preference and situation. The advice was also adapted to the specific flight schedules of the airline company and complemented with recommendations for short-haul pilots. Personal characteristics that were used to tailor the advice were job title (captain, first officer, second officer) and chronotype (morning versus evening-type).
Screenshots of the MORE Energy app are presented in the Appendix (www.sjweh.fi/data_repository.php). After filling out their flight number, departure date and destination (page 2 of the Appendix), participants were directed to a screen (page 3 of the Appendix) where they could choose from personal advice corresponding to three phases of the flight schedule: the preparation from home and departure flight, the time spent during layover abroad, and the return flight and arrival home. Subsequently, the user could choose from three types of advice: sleep and daylight exposure, nutrition, and physical activity.
The advice regarding the optimal timing of exposure to daylight and the timing and duration of sleep, including napping strategies, was based on the strategies presented in the articles by Sacks et al (2) and Waterhouse et al (12). Advice regarding physical activity (optimal timing and type of activity) and nutrition (optimal timing and composition of meals and caffeine intake) was largely based on the strategies presented by Waterhouse et al (12) and Atkinson et al (13). Participants were encouraged to read background information which was available in the glossary menu of the app (page 4 of the Appendix). The composition of the background information was based on the list of topics provided by Avers et al (16). If applicable, the app guided the users to the project website with more information, including videos and audio files (page 5 of the Appendix).
Designed to encourage regular use among the participants, the app had two types of reminders: timed alerts (when the participant did not consult the advice on the app for longer than three weeks) and geofencing alerts (when the participant arrived somewhere outside of the Netherlands, with a maximum of one alert per four days). Due to technical complications, both types of reminders were malfunctioning during the intervention period.
Control group
The participants allocated to the control group received a minimal intervention consisting of access to a secure part of the project website, which contained basic, non-tailored, fatigue and health-related information that was already available within the airline company (such as information about sleep hygiene and the working mechanisms of the biological clock). After randomization, the control group participants received an email with login details to enter the secure part of the website.
Outcome measures
All outcome measures were collected through online questionnaires. At three (T1) and six months (T2) after baseline, an email with a link to the questionnaire was sent to all included participants. Reminders were sent to enhance response.
The primary outcome of the study was fatigue, measured using the 20-item Checklist Individual Strength (CIS) (29), consisting of four dimensions: fatigue (8 items), motivation (4 items), activity (3 items), and concentration (5 items). All questions had seven answer options, ranging from “yes, that is correct” to “no, that is not correct”. Higher scores indicate more fatigue.
Secondary outcomes comprised measures for fatigue, sleep, health-related behavior, and health perception. Need for recovery was measured using the 11-item “Need for Recovery” scale from the Dutch Questionnaire on the Experience and Evaluation of Work (30). Higher scores indicate greater need for recovery.
Sleep quality was measured using the Jenkins Sleep Scale (31). Higher scores indicate lower sleep quality. Sleep duration (ranging from <5 to >7 hours), sleep latency (four categories ranging from severe sleep latency to no sleep latency), and use of sleeping medication (ranging from “more than three times a week” to “none during last month”) were investigated using subscales of the Pittsburgh Sleep Quality Index (32).
Nutritional behavior regarding breakfast usage (one item with four answer categories ranging from “(almost) never” to “every morning”), meal composition choice (two items with four answer categories, ranging from the worst to the best choice), snacking (one item on the number of snacks per day), hydration (one item with four answer categories, ranging from too few to sufficient drinks a day), and caffeine (three true or false items, scores ranging from excessive to strategic caffeine usage), were measured using self-developed questions. Higher scores indicate better sleeping and nutritional behavior. The amount of physical activity per week was measured using the two questions on the recommended frequency of physical activity and exercise among healthy adults in the Netherlands (“how many days per week do you practice moderately intensive physical exercise for at least 30 minutes?” and “how many days per week do you practice strenuous physical exercise for at least 20 minutes?”) (33, 34).
General perceived health was measured using two items of the Dutch version of the Short Form 36-item (SF-36) Health Survey. Current general health had five answer categories ranging from “bad” to “excellent”. Further, appreciation of present health was compared to that of a year before and expressed as a percentage (the better the appreciation, the higher the percentage) (35).
Covariates
The following variables were regarded as potential confounders and collected at baseline only. Work-private life balance was measured using the short version of the Survey Work-home Interference-Nijmegen (SWING) questionnaire (36). Participants’ chronotype was measured using the Dutch version of the Morningness-Eveningness Questionnaire (MEQ) (37). Participants were asked for their body height (m) and body weight (kg), which was computed into body mass index (BMI) (kg/m2). Further, tobacco smoking (“no”, “no, but I used to smoke”, “yes”), alcohol consumption (five answer categories ranging from “never” to “daily”), having a chronic disease (yes/no), and household composition (“alone”, “alone with children”, “together”, “together with children”, “other”) was assessed using single questions. The airline company provided sociodemographic variables age (in years), gender, job title (captain, first officer, second officer), aircraft unit (A330, B737, B747, B777, MD11) and haul type (short- versus long-haul).
Compliance
Compliance with the MORE Energy app was objectively measured through the control management system (CMS) of the application. Through user authentication, this system stored the number of recommendations each participant requested per week. Compliance with the MORE Energy website was measured through a web-analytic tool (Google analytics) that registered and stored the total number of website page views per participant.
Statistical analysis
Effectiveness
Baseline differences in sociodemographic variables between participants and non-participants, and between the intervention and control group, were investigated using Student t-tests for independent samples and Chi-square tests.
For the continuous outcome measures (fatigue, sleep quality, need for recovery, snacking behavior, physical activity, general health, and health appreciation), the overall effectiveness of the intervention was analyzed using linear mixed model analyses. Poisson mixed model analyses were used for the ordinal and count variables (sleep duration, sleep latency, sleep medication, breakfast frequency, meal choice in the morning and evening, hydration, and caffeine usage). In all mixed model analyses, the outcome at follow-up (T1 and T2) was adjusted for the baseline value of the particular outcome.
In all analyses, research condition (control or intervention group) was considered as independent variable. The crude models were constructed first. Next, in order to rule out possible hidden effects of the variables not included in the minimization procedure, adjusted models were also constructed, by adding the potential confounders age, gender, job title, aircraft unit, haul type, work–life balance, chronotype, BMI, smoking, alcohol consumption, having a chronic disease, and household composition.
Per-protocol and dose–response analyses
For the per-protocol and dose–response analyses, the intervention group was divided into four subgroups, depending on the number of weeks the participants had consulted the advice on the app during the intervention (0–1, 2, 3, or ≥4 weeks). To investigate the association between dose (compliance with the intervention) and response (primary outcome variable fatigue), the subgroups were compared using linear mixed model analyses. This type of analysis was also used for the per-protocol analysis, which determined the optimal effect of the intervention by comparing fatigue of the most compliant quartile of participants to the control group participants. Due to loss of power, only the sociodemographic variables measured at baseline were used to adjust the models in both of these analyses.
A two-tailed significance level of P<0.05 was considered to be statistically significant in all analyses. The analyses were conducted with the Statistical Package for Social Sciences (SPSS) version 20.0 (IBM Corp, Armonk, NY, USA).
Sample size
The sample size was based on an expected effect on fatigue, the primary outcome of the intervention, measured with the 20-item CIS. Beurskens et al (29) showed that for healthy employees, the mean total score on this questionnaire was 47.3 (SD 19.8). Consequently, to detect a relevant 10% difference in fatigue, 246 subjects were necessary in each study group (power=0.80; α=0.05). Taking into account a loss to follow-up of 25%, the total sample size was intended to be 656 pilots.
Results
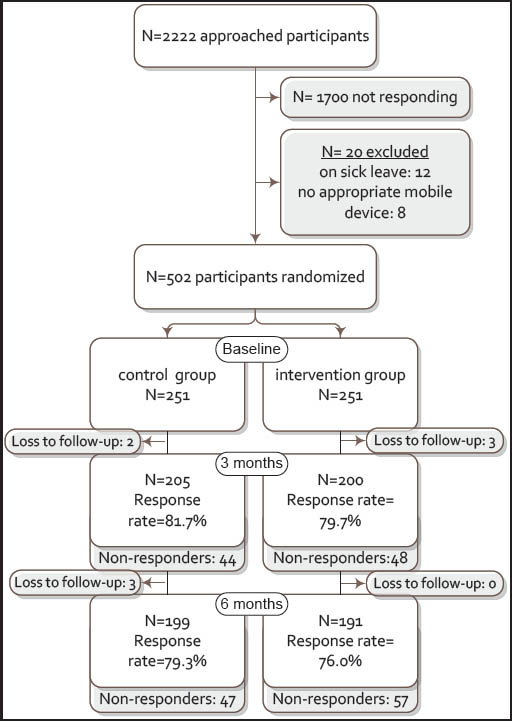
As shown in figure 1, 522 of the 2222 pilots agreed to participate (23.5%). In total, 20 pilots were excluded; three pilots did not have a smartphone or tablet, five pilots had a smartphone or tablet without an Android or iOS operating system, and 12 pilots were on sick leave for more than four weeks at the start of the intervention. The 502 participants proved to be significantly younger than non-participants [mean 40.9, standard deviation (SD) 8.4 versus 42.5 (SD 8.3) years, P<0.001]. The percentage of females among the participants was higher compared to the non-participants (6.8% versus 3.8%, P=0.006). No significant differences in sociodemographic variables were present between the two study groups. Baseline characteristics of the participants are shown in table 1.
Table 1
Baseline characteristics of the potential and included participants. [SD=standard deviation. BMI=body mass index.]
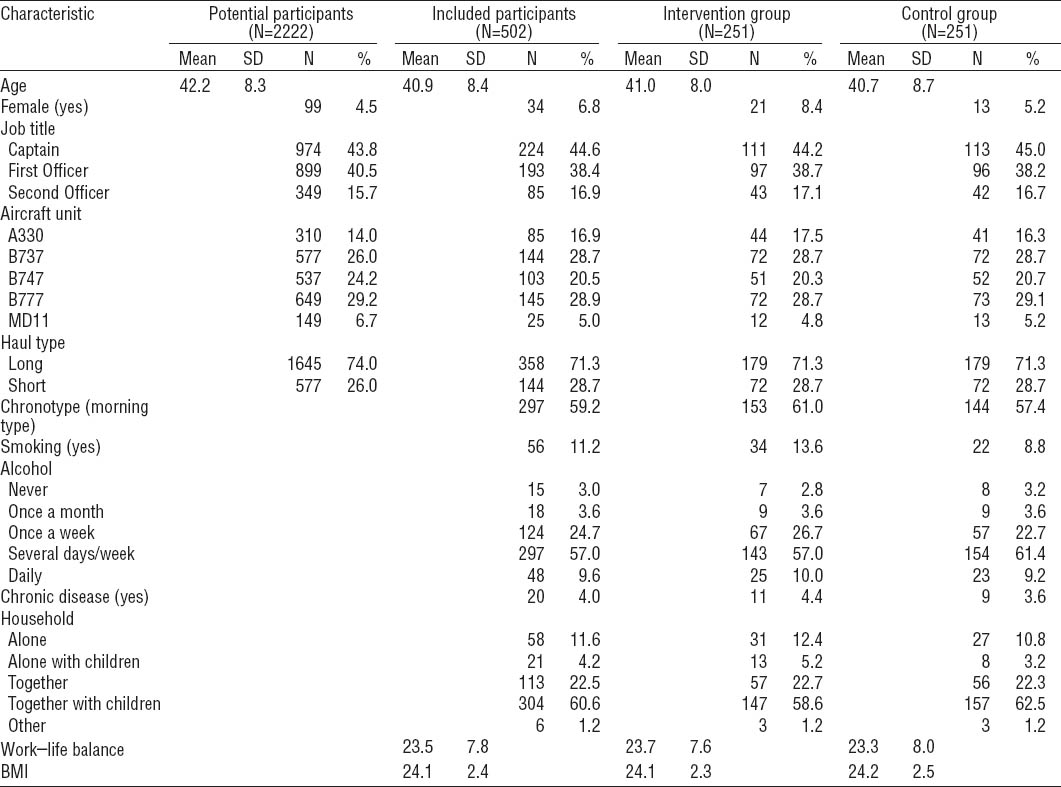
Five participants dropped out of the study during the intervention and three participants left the airline after six months. After three months, 405 participants completed the T1 questionnaire (80.7%), and after six months, 390 participants (77.7%) completed the T2 questionnaire. In total, 361 participants (71.9%) completed all three questionnaires. The attrition rate was 13.5% (68/502), as 68 participants only completed the baseline questionnaire. All these 68 participants were male; this was a significant gender difference in comparison with the remaining participants (P=0.009). Otherwise, no statistically significant differences existed between the remaining participants and the group that only completed the baseline questionnaire.
Compliance with the intervention
During the intervention period, 114 (45.4%) control group participants logged into the project website. Of the intervention group, 49 (19.5%) participants never consulted any advice on either the app or the website. Most of the intervention group participants used the app but never logged on to the website (170 out of 251, 67.7%), while 27 (10.8%) participants used both the app and the website. During the intervention period, 68 (27%) intervention group participants consulted advice during one week only, 54 (22%) consulted advice during two weeks, and 32 (13%) consulted advice during three weeks. A total of 43 (17%) participants consulted the app advice during four weeks or more. The mean number of advice requests per participant was 6.8 (SD 14.0), with a median of 3.
Intervention effects
Table 2 shows the mean observed values for the continuous variables and the crude and adjusted overall effects of the intervention on these outcome measures. Compared to the control group, the intervention group significantly improved on CIS fatigue (including the subscales fatigue, activity and concentration), sleep quality, strenuous physical activity, and snacking behavior, for the crude as well as the adjusted analyses. The intervention did not result in significant effects on: need for recovery, moderately intensive physical activity, general health, or health perception.
Table 2
Overall effects of the intervention on the continuous outcomes. [CIS=Checklist Individual Strength; SD= standard deviation; 95% CI=95% confidence interval; p/w=per week]
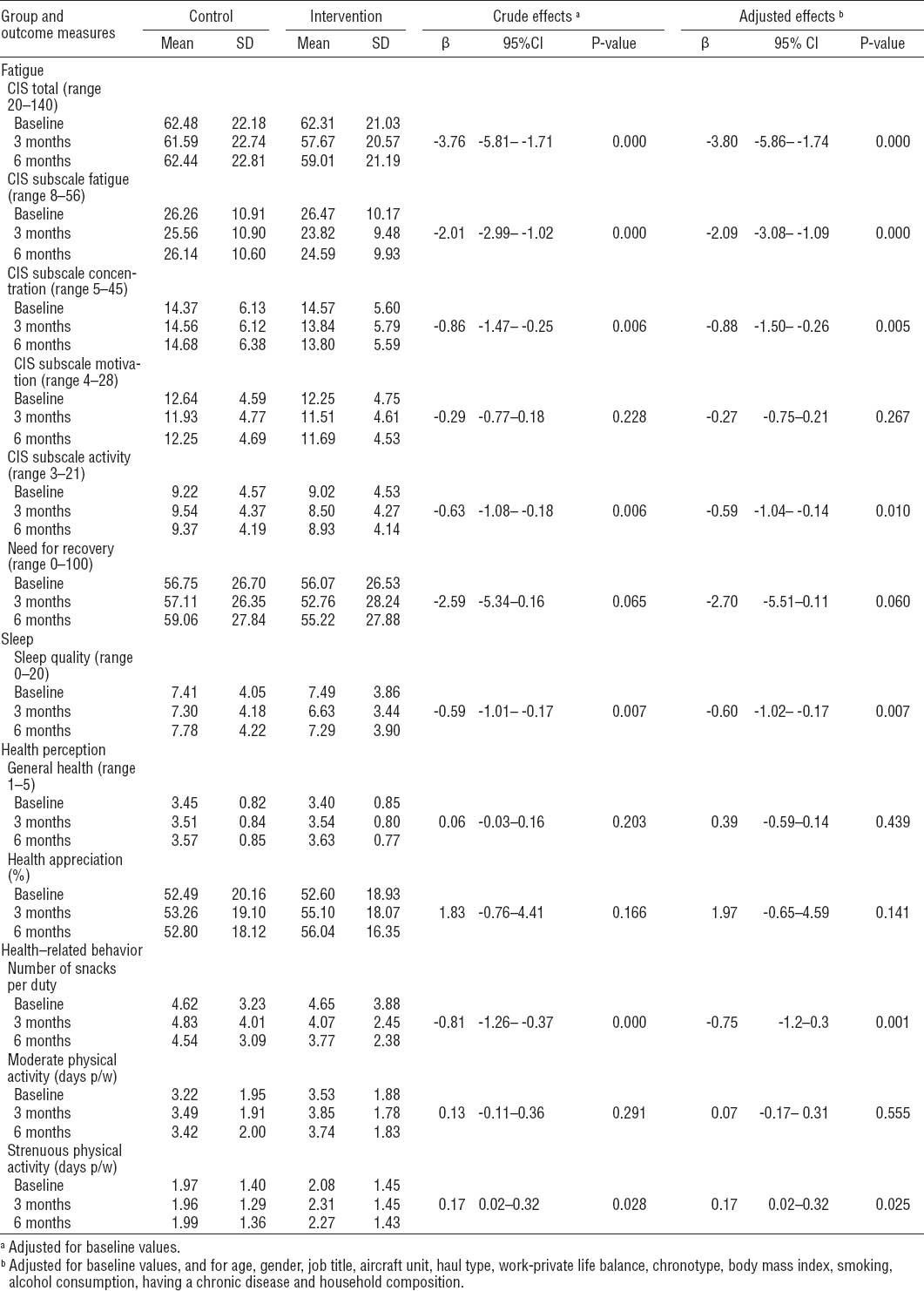
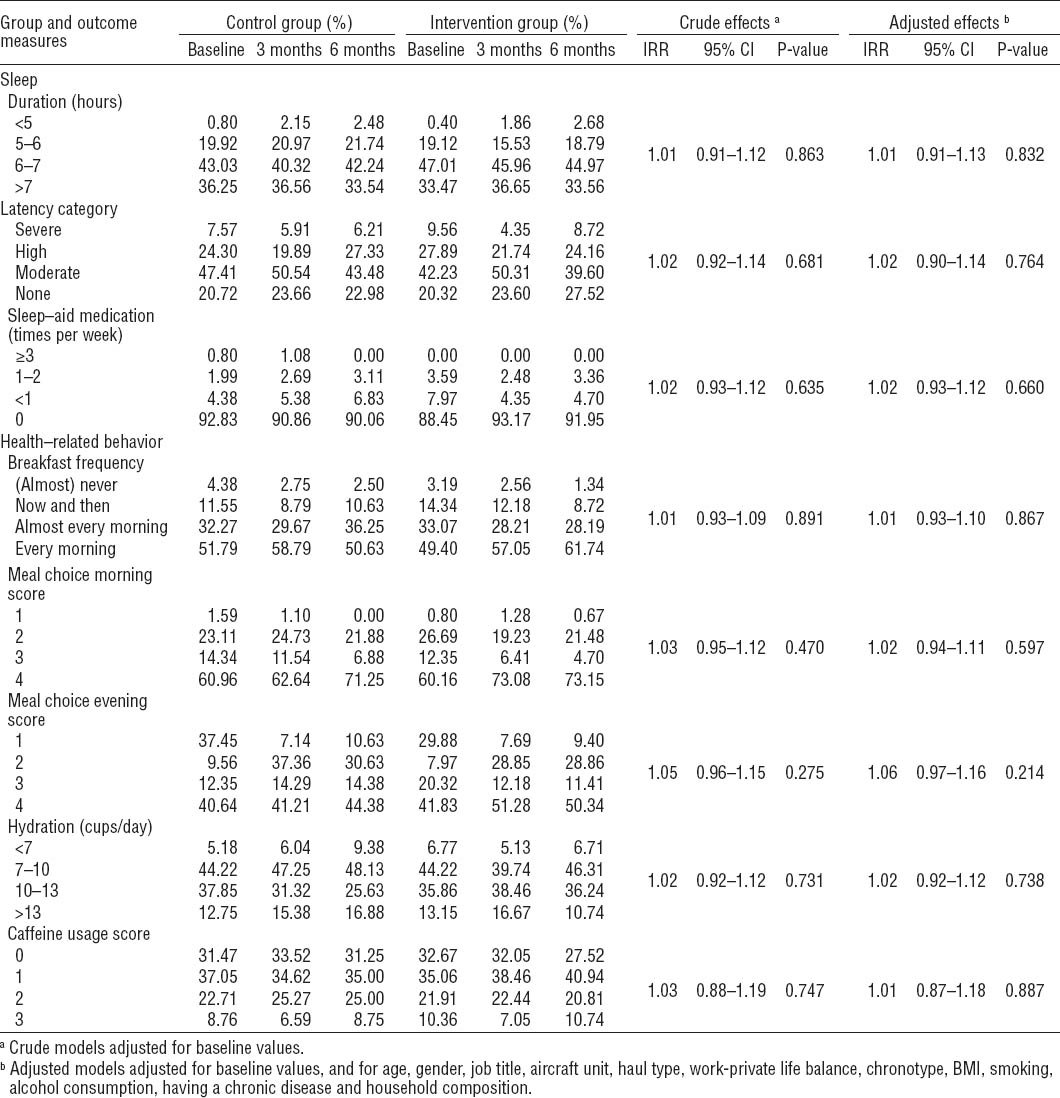
Table 3 shows the mean observed values and the overall effect of the intervention for the count and ordinal variables regarding sleep and health-related behavior (nutrition). The intervention group scored better on all outcome measures, but none of the incidence risk ratios were statistically significant in either the crude or adjusted models.
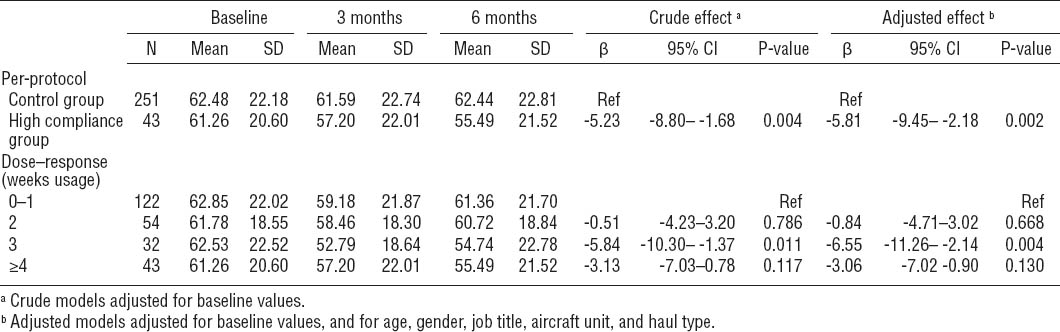
Per-protocol and dose–response analyses
The results for the per-protocol and dose–response analyses are presented in table 4. The per-protocol analysis showed that fatigue of the most compliant group decreased significantly compared to the control group, in both the crude and adjusted analyses. The dose–response analyses showed that the participants that used the app for three weeks had a significantly larger decrease in fatigue than the group that used the app for one week or less, both in the crude and adjusted analyses.
Discussion
This study aimed to improve health-related behavior, reduce sleep problems and fatigue, and improve health perception of airline pilots through an mHealth intervention consisting of specific, tailored advice on exposure to daylight, sleep, nutrition, and physical activity. The randomized controlled trial showed that the MORE Energy intervention, compared to a minimal intervention, was effective in reducing fatigue: three out of four subscales of the primary outcome measure showed a statistically significant improvement, while the effect was marginally significant for need for recovery (P=0.06). We also found an improvement in sleep quality but not sleep latency, sleep duration, and sleep medication. Regarding health-related behavior, the intervention participants showed a significant reduction of snacking behavior and an improvement in the amount of strenuous physical activity. No significant effects were found for any of the other health-related behavior outcomes. For the health perception outcomes, no significant effects were found.
To our knowledge, this is one of the first effective interventions using a mobile application as a medium. Recent publications indicate that interventions delivered through mobile devices can help to quit smoking (38), manage chronic diseases (39), and increase physical activity (26). However, since most studies used text messaging to deliver their intervention, the evidence for a possible behavioral effect of mobile apps is still scarce (25, 26, 38). Therefore, our results are promising as they show that it is possible to reduce fatigue and improve some aspects of health-related behavior and sleep by providing tailored and specific advice through a custom made app combined with a website containing background information. Since it is expected that the usage of mobile devices will further increase in the coming years, mHealth interventions such as this have great potential for both primary and secondary prevention (40).
Earlier, it has been shown that web-based interventions are complicated by the fact that a substantial proportion of participants may drop out because of non-use or loss to follow-up (41). This occurred in our study as well since only 17% of the intervention group participants consulted the advice on the app for more than four weeks over a six-month period. Despite this rather low compliance, MORE Energy proved to be effective on the primary outcome measure fatigue, as well on some secondary outcome measures linked to the topics of the tailored advice (sleep, nutrition, and physical activity). Although not statistically significant, the results for the other secondary outcome measures were in the beneficial direction. Moreover, the per-protocol analysis showed that the decrease in fatigue of the most compliant intervention participants was higher than that of the whole intervention group (β= -5.23 versus β= -3.76, overlap in confidence intervals). Furthermore, the dose–response analysis showed that the decrease in fatigue was larger in subgroups that had consulted the advice more often. However, in contrast to the group that consulted the advice during three weeks, the decrease in fatigue of the most compliant group did not differ significantly from the reference group. This might partly be due to a lack of power because of the small size of the most compliant group. Our findings do indicate that the pilots who used the app had to consult the flight specific advice during at least three weeks in order to benefit from the intervention, and that consulting the advice more often does not have to be of added value. It is possible that participants predominantly used the app when they experienced or had experienced fatigue problems during certain flight schedules, although future research is needed to confirm this assumption.
During the recruitment period, the number of pilots expressing their interest to participate decreased progressively over time. Therefore, we had to acknowledge that it was not feasible to recruit the number of pilots needed according to the sample size calculation. To determine the severity of the problem, we performed a post-hoc calculation, using the mean fatigue score at baseline of the already-included pilot population. Because the mean score proved to be relatively high (62.4), and the SD relatively low (21.6), compared to the reference group of Beurskens et al (29) that we used to calculate the sample size needed for this study, the sample size based on our own population reduced from 656 to 502. Therefore, we decided to recruit at least this lower number of participants before closing study recruitment.
Our study comprised several strengths. First, we performed a RCT according to corresponding quality standards (42). By applying minimization, no baseline differences between the study groups were present. Therefore, possible interference of other factors, such as health initiatives within the different aircraft units, is negligible. Because both study groups were randomized at the individual level and measured during the same period, seasonal influences were prevented as well. The low attrition rate (13.5%) strengthened the internal validity of our study, and we included all participants with at least one follow-up measurement in the analyses, in accordance with the intention-to-treat principle.
A limitation of our study is that we mainly relied on self-reports as our outcome measures were obtained through online questionnaires. It was not feasible to objectively measure the actual change in behavior of the participants. Consequently, it is possible that social desirability may have biased the results. In addition, we did not have any information about individual usage of co-interventions by the participants, possibly influencing the results. Further, as in other web-based or mhealth intervention studies, it was not possible to blind our participants or data assessors, which possibly biased our outcomes. Therefore, the Hawthorne effect, possibly introducing a type one error risk (43), cannot be ruled out, although the dose–response analysis implied that there was an association between the level of compliance to the intervention and the decrease in fatigue.
Another limitation derives from the fact that we aimed to detect a 10% decrease on fatigue. The assumption that a difference of 10% is relevant is arbitrary, especially because we used a continuous variable as the main outcome measure. After six months, however, a significant mean difference of almost four points between the study groups was achieved. Although it is unclear if this difference is “clinically relevant”, it does indicate that the intervention can be effective for pilots who are exposed to long working hours and circadian disruption.
Because the participants were randomized at an individual level, it is also possible that crossover of information has occurred. However, because the app was personalized and both the app and website had a unique login per participant, it is assumed that contamination had a limited effect on the outcome measure differences between study groups.
In contrast with the design of our study (27), participants’ knowledge of the different topics of the advice, was not analyzed. Because it was found at three months that the knowledge questionnaire showed a ceiling effect, these items were excluded from the six-month questionnaire in order to make it shorter.
In total, 522 pilots indicated that they wanted to participate. Due to the exclusion criteria (N=20) and the loss to follow-up (N=68), the total number of participants who completed the questionnaires was lower than the number needed according to the initial sample size calculation (N=492). Although we were able to recruit enough participants according to a post-hoc sample size calculation, our study might still have been underpowered, reducing the probability of detecting intervention effects.
The number of included participants corresponded to a participation rate of 23.5%. Although this rate is quite high compared to the 2% to 8% participation rate published in other mHealth studies (25, 39, 44), there is room for improvement as higher participation rates might increase the generalizability of the results to the whole population of airline pilots. It is possible that due to the impersonal means of communication (email, intranet messages, and news bulletins), we did not reach all potential participants. It was however hard to contact the airline pilots in person since, most of the time, they were either abroad or at home. The generalizability of the results might also be hampered due to selection effects. It is possible that the non-participating pilots did not possess an iOS or Android smartphone or tablet or were not sufficiently familiar with mobile apps. The comparison of the participants versus non-participants also showed that participants were significantly younger and that a relatively large number of female pilots participated. However, all job titles and aircraft units within the target population were well represented in the group of participants. Furthermore, the focus group interviews before the start of the intervention made clear that the vast majority of the airline pilots possessed an appropriate mobile device, and that a mobile application would be the best possible way to transfer the relevant information (27).
During last decades, several attempts have been made to develop effective educational programs for flight crew members to help them cope with their irregular work schedules and accompanying circadian disruption. Because, among other issues, the number of studies evaluating these programs is limited, the effectiveness of the programs remains unclear (18–20). However, education regarding the effects of irregular working hours is becoming increasingly mandatory due to new fatigue risk management regulations within the aviation industry (45). In that perspective, our results are important as they show that by providing relevant person and flight specific information that is available at any time and place, it is possible to reduce flight crew members’ fatigue, thereby possibly increasing performance capability and aircraft safety. The participating pilots were exposed to a wide range of working hours and time zone crossings, including both short- and long-haul schedules. The mean baseline scores of the participants showed that fatigue and need for recovery in this population can be worse than that of the general working population (29, 46), which coincides with the findings of previous studies on airline pilots (47, 48). mHealth interventions like MORE Energy might therefore be implemented throughout other airlines as well, for instance by immediately introducing such an educational tool to new employees (16).
Further research is needed regarding the outcomes on sleep, health-related behavior, and health perception. The working mechanisms of our findings might become more clear when in these future studies, objective measurements of flight schedules, accompanying behavior and coping (eg, napping strategies), and performance capability of the participants are applied. In addition, a longer follow-up period would make it possible to better determine the effects on outcome measures such as sickness absence and health disorders. Furthermore, improving the app with well-timed and adequate prompts, personal feedback, and the introduction of goal setting, might keep users more engaged, increasing participation and compliance rates (38).
Since close to 20% of the European workforce works in shifts including night work, the detrimental effects of prolonged circadian disruption concern employees outside aviation just as well (3, 8, 49). Accordingly, these employees might also benefit from an educational intervention, in line with MORE Energy, providing tailored advice to cope with irregular working hours. However, transferring knowledge using an app does not have to be the solution for every working population, especially as lower smartphone usage has been found in older age groups and people with a lower socioeconomic status (40). Although recent surveys show that both seeking of health information and smartphone ownership keep increasing within every societal subgroup, it is important for future studies, aimed at improving health-related behavior, to determine if mHealth is most appropriate for the target population (40, 50, 51).
Concluding remarks
This RCT showed that, compared to a minimal intervention, the MORE Energy mHealth intervention reduced fatigue of participating airline pilots. Some aspects of health-related behavior (snacking behavior and amount of strenuous physical activity) and sleep (sleep quality) improved as well. Other outcomes related to health-related behavior, sleep, and health perception did not show statistically significant improvements. The results indicate that it is possible to improve fatigue outcomes of employees who have to cope with irregular flight schedules and circadian disruption. Although the working mechanisms have to be further investigated, similar interventions can also be developed for other working populations involved with irregular working hours.