Health and health equity are some of the main goals of social development (1). However, social development does not always facilitate health equity (2). In particular, a low socioeconomic status readily results in a poor health status (3). Some studies have even suggested that a low socioeconomic status renders individuals far from medical utilization, and this vicious cycle aggravates health inequity (4, 5).
Unmet need for access to hospital facilities indicates unmet healthcare need, which occurs when any requirement for medical treatment or examination goes unfulfilled because appropriate medical care is not received (6). Furthermore, unmet healthcare need is one of the well-known indicators of health inequity (7). Hence, many studies have tried to determine the causes of unmet healthcare need in order to recover health equity and improve social development (7–9).
The severity level of a chronic health status, including self-rated health and long- and short-term disability, have also been found to be related to unmet healthcare need (10). Individuals with certain demographic characteristics are at risk of unmet healthcare need, namely, being an older female and having low education and income levels, respectively (11). Furthermore, race, ethnicity, immigration status, employment status, and healthcare coverage are important factors in unmet healthcare need (12, 13). Traditionally, females and males play different role within families, with females generally having more family care responsibilities than males (14). Some studies have suggested that unmet healthcare need differs by gender (10–12); specifically, older and low-income females are at risk of unmet healthcare need (15).
Working hours, which form part of the working environment, have not previously been investigated as risk factors of unmet healthcare need. Workers may work longer hours due to their own ambitions to get better results, such as more money and promotion opportunities. However, excessive work demands can also result in long working hours and bring about various adverse health effects (16). Many previous studies have reported the adverse health effects of long working hours, such as hypertension, diabetes mellitus, metabolic syndrome, and cardiovascular disease (17–19). In addition, long working hours are associated with psychological problems, such as fatigue, depression, anxiety, suicidal thoughts, sleep deprivation, and alcohol use (20–25); and adverse working conditions, such as work disability, occupational injury, and retirement due to disability (26, 27). Working hours are also associated with health-related outcomes such as body mass index (BMI), mortality, general health status, and self-rated health (16, 28, 29). However, there have been few investigations into unmet healthcare need as an adverse effect resulting from long working hours, even though unmet healthcare need can aggravate the numerous adverse health effects of long working hours.
Based on the above observations, research on the effects of long working hours on unmet healthcare need is required. Therefore, we examined the association between long working hours and unmet healthcare need, with gender stratification. To elucidate that association, the study population was selected from a national representative survey of >50 000 people: the Korea National Health and Nutrition Examination Survey (KNHANES) (30). KNHANES includes comprehensive information on socioeconomic status, enabling us to control for potential confounding variables such as age, alcohol intake, smoking, BMI, marriage, region, income, education, occupation, and additional private insurance.
Methods
Study design and participants
We used data from KNHANES IV and V, covering the period 2007–2012. Participation in KNHANES was voluntary. All participants provided written informed consent, and the institutional review board of the Korea Centers for Disease Control and Prevention (KCDC) approved the study (IRB: 2007-02-CON-04-P, 2008-04EXP-01-C, 2009-01CON-03-2C, 2010-02CON-21-C, 2011-02CON-06-C, 2012-01EXP-01-2C). The Korean Ministry of Health and Welfare conducted KNHANES IV and V, which were nationwide cross-sectional studies. Households were randomly selected for participation through stratified multi-stage probability sampling based on geographical areas. A total of 500 and 600 geographical sampling units were used in KNHANES IV and V, respectively. In total, 22 900 households (11 500 in KNHANES IV and 11 400 in V) were selected for participation in the survey. All family members responded to their own questionnaires. The response rates ranged from 78.4–81.9% each year (30). KNHANES IV and V were conducted in accordance with the Helsinki Declaration of 2000.
KNHANES data were obtained from 50 404 participants: 4594 in 2007; 9744 in 2008; 10 533 in 2009; 8958 in 2010; 8518 in 2011; and 8057 in 2012. We selected 12 170 paid workers, who comprised all paid workers in KNHANES IV and V, as our study participants. Of these, 149 participants were excluded because they did not indicate their unmet healthcare need and a further 62 were excluded because they did not indicate working hours. Because part-time workers have very irregular working hours in Korea (23), 1837 participants were excluded because their working hours were <30 hours per week. We also excluded participants who were >54 or <20 years because they are not considered economically active in Korea (31). The general age limit of regular retirement in Korea is around 55 years among permanently employed manual workers. After retirement from a permanent position, Korean workers typically find a new temporary job, although it is less secure than a formal position. Therefore, finally, 8369 participants were used in our study: 4765 males and 3604 females.
Unmet healthcare need
Unmet healthcare need was assessed using a self-reported questionnaire. A response of “yes” to the question, “During the past year, was there any time when you really wanted to visit a hospital but did not?”, was defined as unmet healthcare need. The questionnaire also assessed the cause of unmet healthcare need. A response of, “I do not have enough money”, was defined as “economic burden”; a response of, “Most hospitals were closed when I had free time to visit a hospital”, was defined as “lack of time”; and other responses were defined as “other”, such as, “I have difficulty making a hospital appointment”, “Using transportation is hard”, “I hate waiting for such a long time in hospital”, “Symptoms were mild”, and “other” for other causes.
Working hours per week and other covariates
Working hours per week were assessed through a self-reported questionnaire. The working hours did not include time for meals or breaks. Working hours per week were divided into four categories: 30–39, 40–49, 50–59, ≥60 hours (32).
The smoking group included current smokers and the non-smoking group included those who had never smoked or were former smokers. Heavy drinkers were those who consumed an average of ≥7 units of alcohol for men and ≥5 units for women ≥2 days/week. Moderate drinkers included those who consumed >1 glass of alcohol per month over the past year. Non-drinkers included those who never drink or drank <1 glass of alcohol per month over the past year. According to the guidelines of KCDC, body mass index (BMI) was classified as: <18.5 (low), 18.5–25 (normal), and >25 (obese) kg/m2 (33, 34). Marital status was divided into married/divorced or never married. Region was the stratified variable in KNHANES IV and V so we used residential area as indicated in KNHANES IV and V, which was not self-reported, and classified regions as urban or rural. At the time of KNHANES IV and V, the urban group lived in Seoul, Pusan, Daegu, Incheon, Kwangju, Daejeon, or Ulsan, which are Teuk-byul-si or Kwang-yeok-si, in Korea. All other areas were considered rural. Household income was classified into low, middle-low, middle-high, and high, using the quadrants provided by KNHANES. Education level was divided into those who: (i) only completed middle school or less, (ii) graduated from high school or completed some high school, and (iii) attended college or higher. Occupational type were classified into white-collar (manager and professionals), pink-collar (clerks, service, and sales workers), and blue-collar (agriculture/fishery workers, craft/trades workers, machine operators and assemblers, and elementary manual workers) (21). Additional private insurance was recorded as “yes” or “no”.
Statistical analysis
We conducted a chi-squared test to examine differences between the unmet and non-unmet healthcare need groups, among both males and females. Additionally, we used the Cochran-Armitage trend test to examine the dose-response association between working hours and unmet healthcare need in both males and females. We calculated odds ratios (OR) and 95% confidence intervals (95% CI) for the odds of unmet healthcare need, according to an increment in the working hours’ categories. As they show the significant difference according to unmet healthcare need (table 1), age, smoking, marriage, occupation, and additional private insurance – among males – and age, smoking, and income – among females – were controlled for in gender-stratified multiple logistic regression models.
Table 1
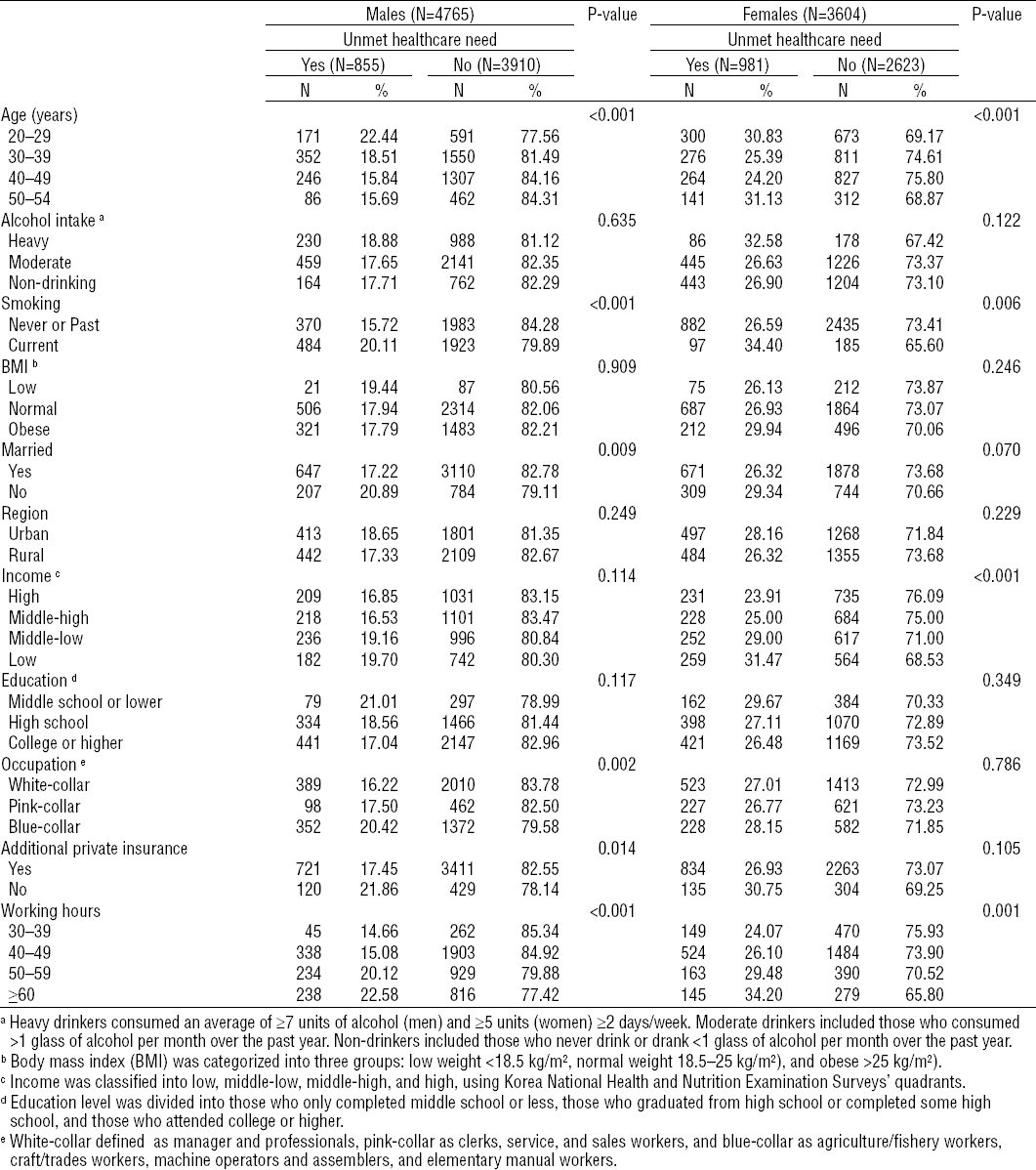
Differences between the unmet and non-unmet healthcare need groups, according to gender. (N=8369)
The P-values for trend were also calculated using a logistic regression model. The SAS 9.2 software (SAS Inc, Cary, NC, USA) was used for all statistical analyses and P<0.05 was considered significant.
Results
Among males, 855 participants (17.94%) experienced unmet healthcare need and the proportion of unmet healthcare need was highest in the youngest age group (22.44% among 20–29 year olds) (table 1). Current smokers experienced more unmet healthcare need than former smokers and those who had never smoked (20.11% versus 15.72%, respectively, P<0.001). The proportion of unmet healthcare need was 17.22% in the married group and 20.89% in the unmarried group (P=0.009). The proportion of unmet healthcare need was highest in the blue-collar group (20.42%, P=0.002). Of workers with additional private insurance, 17.45% experienced unmet healthcare need compared to 21.86% of those without additional private insurance (P=0.014). Among females, 981 participants (27.22%) experienced unmet healthcare need and the proportion of unmet healthcare need was highest in the oldest age group (31.13% among 50–54 year olds). Current smokers experienced more unmet healthcare need than former smokers or those who had never smoked (34.40% versus 26.59%, respectively, P=0.006). The proportion of unmet healthcare need was highest in the low-income group (31.47%, P<0.001).
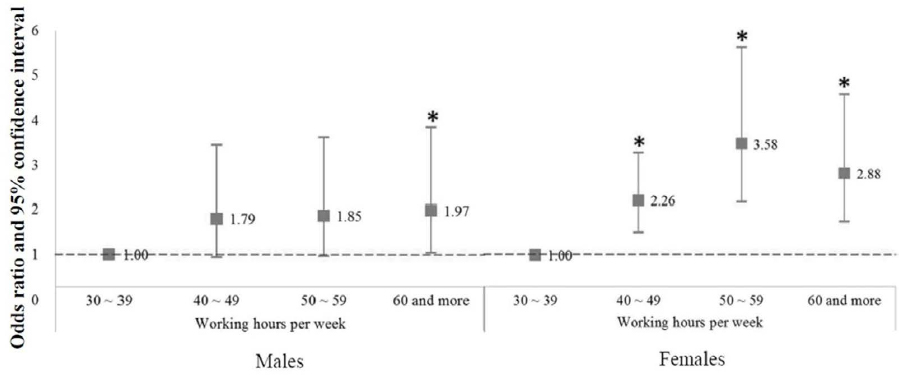
Compared to 30–39 hours per week, among males, the crude OR for unmet healthcare need were 1.03 (95% CI 0.74–1.45) in 40–49 hours per week, 1.47 (95% CI 1.04–2.08) in 50–59 hours per week, and 1.70 (95% CI 1.20–2.40) in ≥60 hours per week. After adjusting for age, smoking, marriage, occupation, and additional private insurance, the adjusted OR for unmet healthcare need were 1.07 (95% CI 0.76–1.51), 1.46 (95% CI 1.03–2.07), and 1.57 (95% CI 1.11–2.23) in 40–49, 50–59, and ≥60 hours per week. Among females, compared to 30–39 hours per week, the crude OR for unmet healthcare need were 1.11 (95% CI 0.90–1.37) in 40–49 hours per week, 1.32 (95% CI 1.02–1.71) in 50–59 hours per week, and 1.64 (95% CI 1.25–2.15) in ≥60 hours per week. After adjusting for age, smoking and income, the adjusted OR for unmet healthcare need were 1.13 (95% CI 0.92–1.40), 1.30 (95% CI 0.99–1.69), and 1.60 (95% CI 1.21–2.10) in 40–49, 50–59, and ≥60 hours per week.
Our findings show that long working hours relate to odds of unmet healthcare need. Particularly, both genders working ≥50 hours per week were more likely to suffer unmet healthcare need. Furthermore, this is a dose–response association (the P-value for trend was <0.001 for both genders in figure 1).
Figure 1
Unmet healthcare need according to working hours, after adjusting for age, smoking, marriage, occupation and additional private insurance in males, and age, smoking and income in females * P<0.05
Of the causes of unmet healthcare need – referring to males and females, respectively – 90 (10.53%) and 136 (13.86%) participants named “economic burden” as a reason, 473 (55.32%) and 490 (49.95%) “lack of time,” and 292 (34.15%) and 355 (36.19%) “other”. The proportion of males who reported lack of time as the reason for unmet healthcare need increased according to working hours, with 37.78%, 55.92%, 56.41%, and 56.72% in the 30–39, 40–49, 50–59, and ≥60 hours per week groups, respectively. The proportion of females who reported lack of time as the reason for unmet healthcare need increased according to working hours, with 30.20%, 50.95%, 62.58%, and 52.41% in the 30–39, 40–49, 50–59, and ≥60 hours per week, respectively.
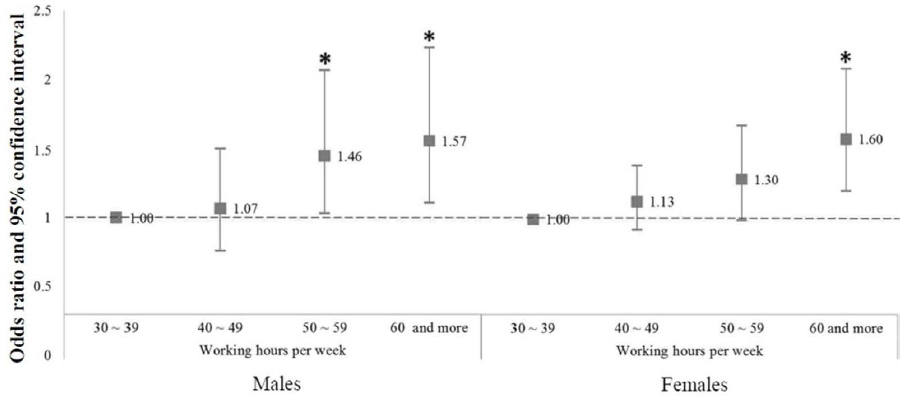
Among males, compared to 30–39 hours per week, the crude OR for lack of time as a cause of unmet healthcare need were 2.09 (95% CI 1.10–3.96), 2.13 (95% CI 1.11–4.11), and 2.16 (95% CI 1.12–4.16) in 40–49, 50–59, and ≥60 hours per week, respectively. After adjusting for age, smoking, marriage, occupation and additional private insurance, the adjusted OR for lack of time as a cause of unmet healthcare need were 1.79 (95% CI 0.93–3.45), 1.85 (95% CI 0.95–3.62), and 1.97 (95% CI 1.01–3.84) in 40–49, 50–59, and ≥60 hours per week. Among females, compared to 30–39 hours per week, the crude OR for lack of time as a cause of unmet healthcare need were 2.40 (95% CI 1.63–3.54) in 40–49 hours per week, 3.86 (95% CI 2.41–6.19) in 50–59 hours per week, and 2.55 (95% CI 1.58–4.10) in ≥60 hours per week. After adjusting for age, smoking and income, the adjusted OR for lack of time as a cause of unmet healthcare need were 2.26 (95% CI 1.52–3.36), 3.58 (95% CI 2.21–5.79), and 2.88 (95% CI 1.76–4.71) in 40–49, 50–59, and ≥60 hours per week. (figure 2)
Discussion
Unmet healthcare need for access to hospital facilities is recognized as an indicator of health inequity that many governments have tried to reduce (7). In this study, we found that there was a dose–response relationship between working hours per week and unmet healthcare need for both genders. These relationships were still significant after controlling for covariates such as age, smoking, marriage, occupation, and additional private insurance in males, age, smoking, and income among females. Those results suggest that the long working hours related to unmet healthcare need in addition to other potential confounding variables, including household income and additional private insurance. To the best of our knowledge, this is the first study to identify working hours as an important factor of unmet healthcare need in Korea. Furthermore, unmet healthcare need due to lack of time is also related to increased working hours.
In Japan, karoshi (sudden death due to overwork) and karojisatsu (suicide due to overwork) are associated with long working hours, particularly overwork, and were an important issue some decades ago (35, 36). The situation in contemporary Korea is the same as in Japan (37). The Organization for Economic Cooperation and Development (OECD) reported that, in 2014, Korea had the second longest working hours among OECD countries, with an average of 44.5 hours per week (38). Therefore, long working hours are a major concern in Korea (39). Physical as well as psychological diseases are related to long working hours (17–19), whereas social and lifestyle factors are also aggravated by long working hours (20–25). Furthermore, our study suggests that long working hours are also related to an increase in unmet healthcare need among paid workers, hence the social concern about reducing working hours to improve workers’ health.
The adverse health effects of long working hours have various mechanisms. Overwork associated with long working hours requires a lot of time for recovery, but people do not have enough time to recover (40). Insufficient recovery caused by lack of sleep disrupts lifestyle and influences health behavior, which leads to depression and cardiovascular disease (16, 22). In this way, long working hours have adverse implications for workers’ health, such as the need for more medical examinations and treatment. However, in the current study, it is suggested that workers do not have sufficient medical examinations and treatment because they lack the time to consult doctors. Lack of time was the most common cause of unmet healthcare need. If workers work for >50 hours over 5 days, they usually have free time after 20:00 hours or later. The usual closing time of hospitals in Korea is 18:00 hours. Therefore, many workers have unmet healthcare need due to lack of time to visit a hospital or a conflicting schedule. Hence, our current results suggest that a vicious cycle might be initiated by long working hours and the effect of unmet healthcare need.
A panel survey in Korea of 9000 people reported that common reasons for unmet healthcare need were economic problems and lack of time to meet doctors (41). However in our study, working hours were not associated with economic problems as a cause of unmet healthcare need. We argue that this difference is due to study participants who, in our study, were paid workers only. As such, these individuals had a lower economic burden than unemployed people. A previous study has shown that unemployed people are more likely to experience unmet healthcare need due to economic burdens (42). In our current study, unmet healthcare need due to lack of time is a more serious problem among females than males. This is supported by a previous study that showed females generally spend more time on family care than males (14).
In the Korean health service system, all Koreans receive public healthcare. In 2011, about 97% of Koreans had national health insurance, and the remaining 3% had national medical protection (43). For this reason, out-of-pocket healthcare costs are not higher than those in other developing countries. However, the Korean welfare system is inadequate, compared to that in developed countries. In Korea, there are no regulations for illness benefits, and many enterprises do not give paid sick leave. The Occupational Safety and Health Act in Korea does not include regulations for onsite physicians in enterprises with <50 workers (44). A total of 98% of workplaces in Korea are small enterprises with <50 workers (45). Those with >50 workers may hire a nurse or an industrial hygiene manager, instead of doctors. So, almost all factories do not have an onsite physician. Actually, only 63 physicians were employed in Korean factories in 2015 (46). Therefore, in general, workers have no access to medical facilities during daytime. When workers fall sick and need to access a hospital, they usually visit the hospital after work or use their vacation leave. In view of this, Korea’s cultural environment can minimize opportunities for workers to access hospital facilities, and long working hours can aggravate unmet healthcare need.
In Korea, the Labor Standards Act (LSA) regulates working hours. Article 50 of the LSA states that “working hours per week shall not exceed forty hours excluding recess hours”. Article 53 of the LSA declares that “if the parties concerned reach agreement, the working hours stipulated in Article 50 may be extended up to 12 hours per week” (47). The 2013–32 notification of the Ministry of Employment and Labor in Korea states that working hours of >60 hours per week are a standard for compensation for death due to overwork (48). In spite of these regulations, in the current study, 46.53% of male workers worked for >50 hours per week, and 22.12% worked for >60 hours per week. This reflects the rampant culture of overwork in Korea. Furthermore, these long working hours are related to the unmet healthcare need. In addition, unmet healthcare need in Korea is higher than in Canada (10.7%), which runs a universal healthcare system, and even higher than in the United States (13.2%), a country that does not provide universal healthcare services (49). Thus, health inequity due to unmet healthcare need proves to be a serious problem in Korea. To prevent such outcomes, we hope that our study provides important insight for Korean labor policy-makers when dealing with working hour regulations. Our study results strongly recommend urgent efforts by the Korean government, employers, and employees to reduce long working hours.
As discussed above, there are no regulations regarding sick leave in Korea and very few factories have their own healthcare facilities. As a result, workers usually use their own vacation leave or free time after work to visit hospitals. However, hospitals close at the same time as workplaces do. Therefore, assess to hospital facilities is not easy when workers are overworked. Korea is a rapidly developing country in Asia, but is not a developed country. The average number of annual working hours per worker in 2014 was 2124 hours in Korea, 1645 in Finland, 1427 in Norway, and 1609 in Sweden (38). In the context of working hours, the current status of Korea (2124 hours per year) is comparable to that of Europe, at 1930 (50). Overwork culture is rampant in Korean society. Due to very strict enterprise-specific organizational cultures, many workers are forced to work excessively. Therefore, overwork is not merely dependent on workers’ willingness, but strongly depends on employer enforcement. The low hourly rate of remuneration is also one of the causes of long working hours. Actually, in Korea, the minimum hourly wage is KRW5580 (about US $5) (51), while the average hourly wage of blue-color workers is about US $10 (52). Hence, some of the workers want to work more to earn more, and not due to personal ambitions. In summary, the rampant overwork culture and low wages might be the cause of long working hours of Korea.
The large sample size of >4700 males and 3600 females is the main strength of the current study. However, our study also had some limitations. First, as it is cross-sectional research, the association between working hours and unmet healthcare need could not be established with certainty. Second, unmet healthcare need is investigated in two ways: clinical unmet healthcare need based on clinical guidelines and subjective unmet healthcare need based on an individual’s opinion (6). Our use of subjective unmet healthcare need in this study meant that we could not infer clinical unmet healthcare need. However, previous studies have indicated that subjective unmet healthcare need is as important as clinical unmet healthcare need because individuals estimate their healthcare needs better than doctors and subjective unmet healthcare need is reflected by demands (6). Many studies use subjective unmet healthcare need (11, 12, 41). Third, the prevalence of unmet healthcare need differs according to type of illness. For example, unmet healthcare need related to mental illness is generally larger than that related to physical illness. Some articles have suggested that subjective poor medical service is regarded as an unmet healthcare need, even though individuals consult medical doctors in hospitals (7). Furthermore, cultural differences affect the level of unmet healthcare need. Hence, our results should be carefully considered when generalizing to other countries. Fourth, we calculated workers’ working hours on the basis of self-reported questionnaire data, which might lead to non-differential misclassification and underestimation. However, it would have been quite difficult to calculate workers’ working hours objectively; many previous studies have also calculated workers’ working hours on the basis of self-reported questionnaire data (21, 23, 29).
In summary, we found that long working hours were associated with unmet healthcare need among both males and females. We also found that the reason for unmet healthcare need among workers with long working hours is lack of time to consult a doctor. We anticipate that our study, with gender stratification and >4700 male participants and 3600 female participants, provides important insight into the occupational health of individuals working long working hours and highlights the need for labor policy change in Korea.