Obesity is increasing worldwide with the 2009–2010 prevalence among US adults surpassing one-third (1, 2). Obesity is associated with genetic, behavioral, occupational, and environmental factors (3–5) and has significant economic impact (6). It is also associated with various health problems including musculoskeletal disorders (MSD), asthma, liver disease, and cardiovascular disease (CVD) (7–10). Moreover, neurohormonal and endocrine pathway disruption has been associated with obesity (11, 12). Work factors, including sedentary work and task-related biomechanics, have been reported as risks for obesity (13–15). Variables such as irregular work hours/sleep schedules, job stress, workplace absenteeism, and reduced productivity also contribute (16–19).
Although the related literature is growing, obesity in the occupational environment requires more study, for example, regarding low-wage workers and genes or other factors (20, 21). Body mass index (BMI), a measure of obesity, varies by population, race, gender, and socioeconomic class (22–24). Genetics may account for ≥40% of the variation in BMI (25), but such estimates can depend on the variability of environmental risk factors observed. Although major genetic changes have not accompanied the rapid rise in obesity, genes play a role in energy expenditure (20–31). The prevailing belief is that the obesity epidemic has arisen from environmental and behavioral factors (1, 2, 7, 15, 16, 22, 32–34). The association of obesity with various occupations (eg, housekeeping, service, motor vehicle operation, nursing) and exposures (sedentary work, work stress, contingent work, low physical job demands, chemicals) suggest it is important as both a risk factor and adverse health outcome in the occupational environment, but as part of a complex matrix of variables (15, 21, 32, 35–39).
Schulte and colleagues’ (38, 40) description of the relationship between occupational hazards and obesity stimulated this paper. Integrated evaluation of occupational and non-occupational factors related to obesity and the workplace have health and economic implications for workers and employers (41). For example, some analyses have found obesity to be associated with higher numbers of worker compensation claims (42). Conceptual models examining combined impacts of occupational risk factors (ORF) and personal risk factors (PRF) can be used to address the multiple factors of relevance to obesity in the workplace setting and understand risks for adverse outcomes (43). As we have noted previously, such models function to classify known or theorized relationships, will require future investigation and validation, and indicate potential avenues for basic research and subsequent design of interventions (40). Understanding risk is important for developing and targeting prevention and intervention strategies (44–47); in essence, it is a risk management strategy to prevent adverse health outcomes. Risk management for primary prevention could include workers in sedentary occupations using sit-stand workstations to increase non-exercise activity thermogenesis (caloric expenditure associated with non-exercise movement), which may have a role in obesity prevention (33, 48–50). Management of risk for tertiary prevention might focus on return-to-work protocols after injury (51). The US National Research Council (NRC) emphasizes assessing risk for chemical and non-chemical hazards for risk-management (52). A comprehensive approach to understanding combined ORF and PRF effects could strengthen risk management at all prevention levels to promote workforce health, greater productivity, and population well-being (52–56). This discussion paper focuses on basic conceptual heuristic models that consider combinations of risk factors related to obesity and the occupational environment.
Evaluating obesity and occupational health issues in a comprehensive approach
In our conceptual model approach (43), models describing combinations of ORF, PRF, and adverse outcomes among working populations are not meant to conclusively delineate specific molecular/cellular/organ/system-level causal pathways, etiologic steps, epidemiological mechanisms, or statistical relationships with respect to the illnesses or injuries discussed. Rather, these models were developed as heuristic frameworks to consider PRF and ORF and health and safety outcomes.
PubMed was searched since 2000 for English language primary studies, journal articles, meta-analyses, and reviews. Reviews were included since conceptual models are presented as a developmental exercise to stimulate hypothesis generation for research, risk assessment, and intervention design. The first search used the terms obesity, occupational health, and specific workplace exposures and health outcomes identified from recent reviews as being important for obesity (7, 8). The second search involved combining the results for these terms and yielded 1245 publications that were the basis for targeted searches (eg, genetics, interventions).
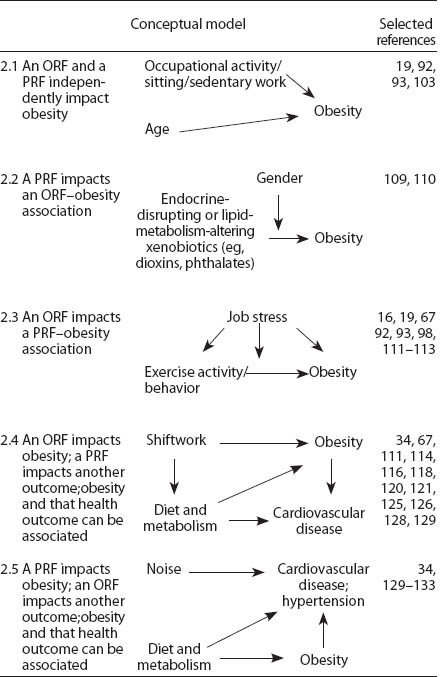
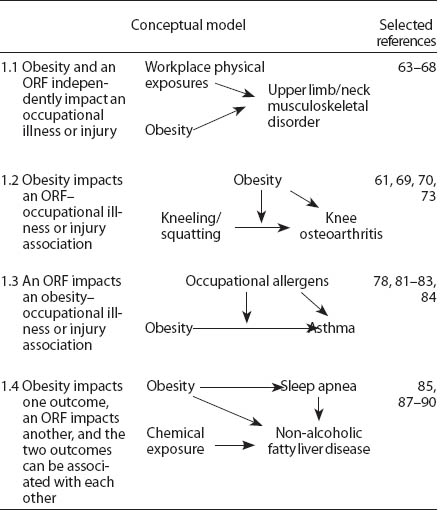
Four models describe obesity as a PRF in an occupational setting (figure 1). In model 1, obesity as a PRF present with an ORF are independent of each other with respect to their impact health outcomes. In models 2, 3, and 4, obesity and an ORF can have combined impacts on outcomes. In models 2 and 3, obesity and an ORF could alternately impact the effect of the other variable on outcomes. In model 4, obesity and an ORF could impact different adverse health processes that are associated with each other.
Figure 1
Conceptual models to delineate the combined impact on outcomes of obesity as a personal risk factor (PRF) with an occupational risk ractor (ORF). Adapted from a figure originally published in Schulte et al (43).
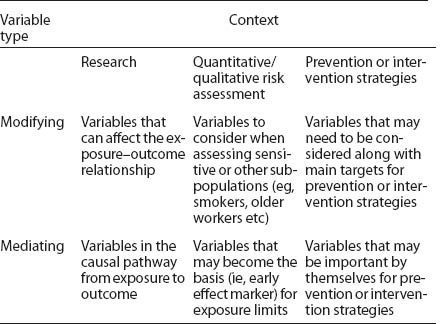
Five models describe obesity as an adverse health outcome (figure 2). In model 1, the PRF and ORF independently impact obesity. In models 2, 3, and 4, a PRF and ORF can have combined impacts. In models 2 and 3, the PRF and ORF alternately impact the effect of the other variable on obesity. In models 4 and 5, the ORF, or alternatively PRF, impacts obesity, in a context where more complex associations are present. For all models, the use of one versus another, or a more complex model, can change as scientific information evolves. More complex models could exist for the examples presented and potentially more complex situations are noted where appropriate.
Figure 2
Conceptual models to delineate the combined impact on obesity of a personal risk factor (PRF) and an occupational risk factor (ORF). Adapted from a figure originally published in Schulte et al (43).
Risk factors related to obesity and the occupational environment: Obesity as a personal risk factor
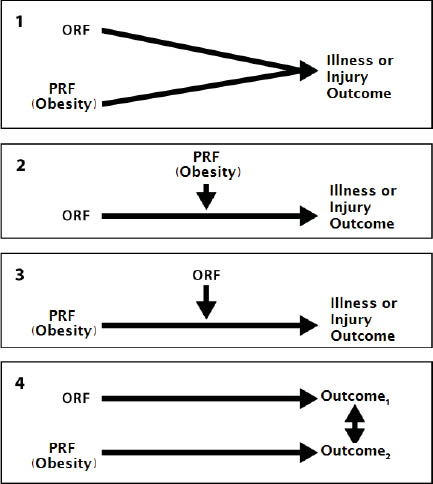
Obesity may increase the risk for various outcomes. Table 1 illustrates four examples where obesity and an ORF impact health outcomes. They are illustrative rather than exhaustive in depicting the complexity of the inter-relationships involved. The examples in this section and table 1 extend examples originally provided by Schulte et al (43).
Table 1
Examples of the impact on illness and/or injury of the combination of obesity as a personal risk factor and various occupational risk factors (ORF). Adapted from a figure originally published in Schulte et al (43).
Example 1.1: Obesity, occupational physical factors, and MSD
The relationship of obesity to MSD is complex (57, 58). For instance, obesity and ineffective job-task training are considered independent risk factors for carpal tunnel syndrome (59, 60). Mechanical loading is considered an etiologic factor in MSD, particularly for concomitant osteoarthritis and obesity; other predisposing factors include joint injury, heredity, and aging (61, 62). In addition to biomechanical factors, studies of animal MSD models suggest multiple biochemical and molecular mechanisms that may interact with obesity to influence MSD development (61).
A systematic review of 21 longitudinal studies demonstrated that workplace physical factors are part of a cause–effect chain for upper-limb/neck MSD (63). These factors include manual material handling, vibration, trunk flexion/rotation, and working with hands above shoulder level. Linking obesity with complex outcomes such as MSD is challenging. For example, a Cochrane review has shown that upper-limb/neck MSD may not be a single entity (64), subgroups of which may have a different relationship to obesity and require different approaches to prevention and intervention.
Some cross-sectional (65, 66, 67) and longitudinal (68) studies have evaluated obesity and the development of MSD symptoms in working populations, but more studies are needed, particularly with more rigorous ascertainment of MSD triggering factors and symptoms. For example, the longitudinal study found associations between incident self-report shoulder pain, in the week prior to survey, and age, BMI, workplace physical factors, and psychosocial factors among workers at baseline and at three years (68). Extended work schedules (eg, shift work, long hours) were an independent risk factor for MSD among nurses (67), but work schedules are also considered an important occupational risk factor for obesity (see example 2.4). Taken together, this breadth of data examining different risk factors or outcomes in animal models as well as cross-sectional and longitudinal studies suggests the importance of considering the impact of obesity and occupational factors on MSD. One such conceptual model could focus on the impact of obesity and workplace physical factors on upper-limb/neck MSD (table 1, example 1.1).
Example 1.2: Obesity, occupational kneeling/squatting, and osteoarthritis
The association of knee osteoarthritis with occupational kneeling and squatting has been shown to increase 7-fold between the lowest and highest categories of BMI (69, 70). The impact of heavy workload, obesity, and traumatic knee injuries on the development of osteoarthritis have been reported from a prospective study of a Finnish cohort with ≥20 years of follow-up (71). The combined impact of kneeling/squatting activities and obesity may also be important for the progression of existing knee osteoarthritis symptoms (72–74). Cross-sectional and longitudinal studies of obesity and occupational risk factors for osteoarthritis in working populations support the importance of a conceptual model of obesity, occupational kneeling/squatting, and osteoarthritis. Animal data suggest that the physiologic impact of obesity on osteoarthritis (61) may be of relevance (table 1, example 1.2).
Example 1.3: Obesity, occupational allergens, and asthma
Obesity increases the risk for asthma and is associated with greater asthma-related healthcare utilization and reduced quality of life (75). Obesity is associated with decreased sensitivity to glucocorticoids, a mainstay of asthma treatment (10, 75, 76). Occupational allergens such as chemicals, dusts, fumes, or other compounds can increase the risk of asthma onset or its exacerbation (77–83). An earlier peer review concluded that controlling obesity and occupational exposures are among the best opportunities for asthma prevention (84). The literature on the relationship of occupational allergens and obesity, respectively, to asthma is long-standing and robust. Thus, an important conceptual model is the impact of occupational exposures on the relationship between obesity and asthma (table 1, example 1.3).
Example 1.4: Obesity, sleep apnea, and non-alcoholic fatty liver disease (NAFLD)
Obesity increases the risk for hypertension through salt retention, insulin resistance, dyslipidemias, sympathetic nervous system activation, systemic inflammation, and risk of sleep apnea (8). Increased risk for sleep apnea stems from the impact of elevated blood pressure and constraints on the pulmonary system from increased BMI (85, 86). NAFLD has been associated with exposures to chemicals such as organic compounds or metals in cross-sectional analysis of population data (87, 88) and among workers with or without metabolic disease (89). The association of sleep apnea with NAFLD is gaining support (90) and the association of obesity with NAFLD is becoming a greater concern given the obesity epidemic (91). Although much of the data is cross-sectional or observational, the situation raises enough concern to suggest a conceptual model in which the combined presence of obesity and an occupational chemical exposure could impact the effects of sleep apnea on NAFLD (table 1, example 1.4). This example illustrates the potential for a disease process due to obesity, along with exposure to chemicals, to be relevant in the occupational setting. Additionally, it raises the issue of more complex associations in the context of occupational exposure to chemicals that may impact NAFLD status because of the role of obesity in both sleep apnea and NAFLD. This emphasizes the need to consider multiple disease processes based on occupational and personal risk factors for evaluating the impact of obesity and the work environment.
Risk factors related to obesity and the occupational environment: Obesity as an adverse health outcome
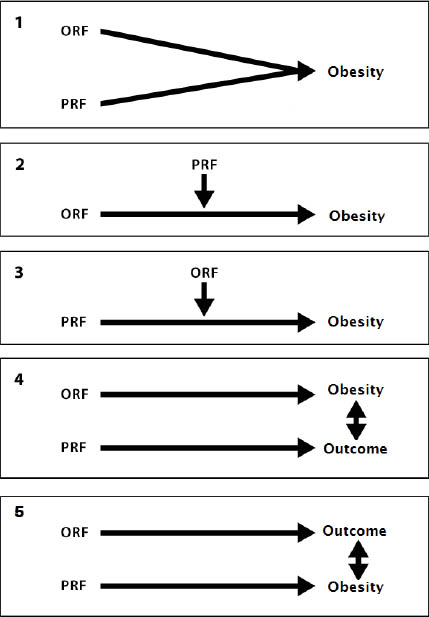
Strong evidence supports the role of genetics, family history, age, diet, physical activity, medications, and environmental factors as risk factors for obesity (2, 7, 8). Understanding the impact of ORF and PRF is important for obesity as an adverse health outcome in and of itself in the work environment. The conceptual models of ORF and PRF impacting obesity (table 2) are illustrative rather than exhaustive in depicting the complexity of the inter-relationships involved.
Example 2.1: Sitting/sedentary work, age, and obesity
One of the most significant modifiable variables affecting obesity is physical activity (7). Recent analysis of 3539 adults from 1999–2004 National Health and Nutrition Examination Survey (NHANES) data found that having high versus low occupational activity decreased the odds risk ratio to 0.37 [95% confidence interval (95% CI) 0.24–0.57] for abdominal obesity (92). Cross-sectional analysis of 10 785 workers from the Australian National Health Survey found that mostly standing at work, versus mostly sitting, lowered the risk for overweight/obesity to 0.88 (95% CI 0.82–0.95); physical activity and leisure-time sitting did not impact this association (93). Although cross-sectional, this evidence suggests that occupational activity levels influence obesity. A meta-analysis of 15 prospective studies suggests that “light” physical activity, or even standing instead of sitting during leisure time, may decrease the risk of obesity-associated diseases, particularly diabetes, with reported associations predominantly independent of overall physical activity (94). Such evidence supports the idea that sedentary behavior and physical activity are separate behaviors. Current thinking suggests that degree of activity may be influenced by environment and genetics (49, 95–97). Studies have found that animals can be bred to be “obesity resistant” demonstrating more spontaneous physical activity (96), and certain genes, such as the brain-specific Bsx or “fidget” gene, may impact spontaneous physical activity (97), although these findings have not been confirmed among humans. A recent examination of the impact of sedentary behavior (hours of TV watching) on the BMI of individuals with a genetic predisposition for obesity (32 well-established BMI-associated genetic variants) found that prolonged sedentary activity exacerbated genetic effects, but increased physical activity independently weakened this genetic association (98). Extended periods of inactivity among both animals and humans cause physiologic and metabolic changes, suggesting that consideration of sedentary behaviors and physical activity may be needed for interventions in the occupational setting (94, 99, 100, 101). If an individual, with a genetic predisposition for low levels of physical activity, is employed in a sedentary profession, then these factors may independently engender obesity or may interact to produce greater weight gain. From the PRF perspective, decreases in exercise levels are considered a significant factor for obesity increasing with age (102). Metabolism, hormone function, body fat distribution patterns, and other biochemical and physiologic processes also change with age, often creating a setting fostering obesity (103). A conceptual model concerning the impact of occupational activity/sitting/sedentary work and age on obesity may be important for consideration in the occupational environment (table 2, example 2.1).
Example 2.2: Chemicals with endocrine-disrupting or lipid-metabolism-altering properties and obesity
The association of obesity with occupational exposure to endocrine-disrupting chemicals is supported by evidence from animal models as well as observational and case–control studies. Fat-soluble xenobiotics, such as benzo(a)pyrene (104) and polybrominated diphenyl esters (105), deposit in adipose tissue and have been shown to affect lipolysis and thyroid function in rodents. A complex causal relationship between polychlorinated biphenyls and obesity has been theorized with varying impact of factors, such as degree of chlorination, and time course of exposure as well as gender, in analyses of US and Swedish cohorts (37). Obesogens, chemicals suspected to be causally related to obesity, also have been proposed to include phthalates, dithiocarbamates, aryl hydrocarbon receptor ligands, and organotins, despite normal diet and exercise activities (37, 106–110). A recent cross-sectional analysis of men and women participating in a prospective cohort study in the Netherlands provided evidence that occupational exposure to endocrine disruptors in either gender was associated with an increased time to pregnancy (109). Recently, a case–control study of 1005 breast cancer cases and 1146 community controls in Canada demonstrated increased exposure to carcinogens and endocrine disrupters in a range of occupations, including agriculture and automotive plastics manufacturing (110). An important conceptual model focuses on gender differences in the impact of various endocrine disruptors on obesity (table 2, example 2.2).
Example 2.3: Job stress, exercise activity/behavior, and obesity
Job stress has been linked to BMI (19, 38, 111). A recent cross-sectional analysis across 13 European studies, with a total of 161 746 participants, found both weight gain and loss to be modestly associated with job strain (16). Job strain may be associated with type 2 diabetes through BMI and gender dependent mechanisms (112) and kidney dysfunction in a BMI dependent manner (113). Personal exercise behavior/activity impacts obesity and type 2 diabetes (15, 92, 93, 98). Although mostly cross-sectional, the association of job stress or strain with obesity supports an important conceptual model involving exercise behavior/activity, job stress or strain, and obesity, with several inter-relationships possible (table 2, example 2.3).
Example 2.4: Shift work, diet and metabolism, cardiovascular disease, and obesity
Shift workers have increased body weight, and working long hours has been positively associated with higher BMI (38, 111, 114). Shift work, sleep deprivation, and exposure to bright light at night have been associated with increased adiposity (115). Cross-sectional studies suggest that disrupting normal eating and sleeping patterns through night shift work or rapidly rotating day/night shifts are risks for obesity and metabolic syndrome (116). Cyclic, clock-like expression of “clock genes,” in central and peripheral tissue neurons, liver, and fat cells, with expression in rhythmic patterns synced to external environments, impacts food intake, energy expenditure, and sleep (117). In animal models of activity during normal sleep times or of fragmented sleep periods, disruption of this mechanism is associated with energy metabolism malfunction, development of obesity, and disrupted glucose utilization (118–121). Shift work and circadian disruption has also been associated with changes in gastrointestinal and metabolic processes such as fat absorption and metabolism, melatonin-related lipid metabolism, enteric autonomic function, and altered insulin signaling in human subcutaneous fat (121–125). Shift work also disrupts workers’ eating behaviors such as those related to food choice and availability as well as eating times and habits (67, 126). Recent studies have found, however, that disrupting only the fat cell clock gene Arntl caused mice to eat during their inactive phase, a type of “night eating syndrome”, and engendered obesity with no changes in activity or other behaviors. As the circadian clock was disrupted in only fat cells, these data suggest a strong communication network between fat stores and the brain (127, 128). Diet and metabolism impact obesity and CVD such as hypertension, with high calorie/high fat intake, metabolism, and high salt ingestion/retention playing differential and important roles (2, 7, 129). Animal data and observational studies in humans provide evidence on the effects of shift work/long work hours on obesity, and review the information on the role of diet and metabolism in obesity and CVD. This information strongly suggests the importance of a conceptual model that considers both physiologic and behavioral perspectives regarding the impact of shift work and diet/metabolism on obesity, with both factors significantly increasing the risk for CVD (table 2, example 2.4). This model also illustrates complexities that can arise when risk factors impact each other.
Example 2.5: Occupational noise exposure, CVD, diet and metabolism, and obesity
Analysis of the 1999–2004 NHANES data showed that chronic occupational noise exposure, compared with no exposure, resulted in 2–3 times greater prevalence of CVD, such as hypertension (130). Other findings strongly support the theory that noise exposure has an impact on hypertension, and some data suggest that hearing loss and hypertension severity is associated (131–133). As such, this cross-sectional data supports the need for further evaluation of noise and CVD. Given the relationship of diet, metabolism, obesity, and CVD (see example 2.4) a conceptual model that may be important to consider is occupational noise exposure, diet/metabolism, obesity, and CVD, providing the potential to examine more complex relationships (table 2, example 2.5).
Combinations of risk factors and special issues
The conceptual, heuristic models in tables 1 and 2 are starting points for describing the combined impacts of personal and occupational risk factors relevant to obesity and the workplace. The involvement of multiple mechanisms for a given ORF/PRF/adverse outcome combination is illustrated by examples 1.2, 1.3, 1.4, 2.3, 2.4, and 2.5. Improved understanding of these complex relationships can inform hazard definition and exposure assessment as well as drive risk assessment and management strategy development to address obesity in the occupational environment.
Defining a factor as a modifying or mediating variable can improve understanding of disease mechanisms or relevant interventions (134). Such definitions can impact the design and analysis of research studies, the conduct of risk assessment to set exposure limits, and the development and application of prevention or intervention strategies for behavioral factors such as physical activity or diet. In table 3, we revisit classic descriptions of modifying or mediating variables (134) with relevance to research, risk assessment, and prevention/intervention strategies (52). Primary, secondary, and tertiary prevention and risk management may require targeting different or multiple risk factors for optimal effect. Ultimately, in addition to assessing relative risk for these endeavors, it may also be necessary to consider attributable risk.
Future considerations
Obesity in the occupational setting can be a personal risk factor or an adverse health outcome. This distinction affects hazard definition, exposure assessment, risk assessment, and risk management. Evaluating issues related to obesity and the workplace using a combined approach could better inform workplace intervention/prevention activities. More research is needed in this regard. For example, defining obesity and workplace physical factors as combined risks for MSD might focus prevention strategies on weight management and occupational tasks. Preventive efforts might also need to target primary versus secondary/tertiary prevention for return-to-work after an MSD differentially. Obesity defined as an adverse health outcome due to exposure to endocrine disruptors, however, might require interventions with improved exposure controls and weight management, with obesity monitoring to measure outcome status. These occupational considerations, of course, support giving greater attention to broader issues of diet, nutrition, and lifestyle in general society.
Targeted intervention/prevention strategies in the occupational setting, such as weight-reduction programs or diet consultations, are evolving; several reviews and interventional studies are currently examining this issue (135–137). Workplace interventions for obesity will likely be effective (38), but systematic evaluation of interventions is sorely needed (136). For example, Sorensen and Barbeau (138) have shown that addressing ORF and PRF together can reduce smoking, but the utility of such approaches for obesity requires investigation. Defining obesity as a personal risk factor or an adverse health outcome, and identifying and examining the combined impact of factors, with risk assessment and management of combined exposures, may lead to improved primary, secondary, and tertiary prevention for issues of obesity in the occupational setting.