Low-back pain (LBP) is highly prevalent among healthcare workers compared to the general population, with an annual prevalence ranging from 45% (1) to 77% (2). Furthermore, the prevalence and incidence of chronic/persistent LBP are particularly high among healthcare workers (3). Persistent LBP among healthcare workers is shown to be a particularly strong risk factor for long-term sickness absence (3) and early retirement from the profession (4). Therefore, identification of risk factors for development of persistent LBP among healthcare workers is needed.
Physical factors in the working environment are assumed to cause or aggravate LBP among female healthcare workers. Patient-handling activities are considered to be the main cause of LPB among healthcare workers (5). The activities during patient handling often include lifting, transferring, and repositioning of patients and devices causing awkward back postures and high exerted forces of the healthcare worker (6). Some studies have investigated the risk for LBP from patient-handling activities (2, 7–10). However, few of these studies are prospective, and most of them did not adjust for potential confounders such as lifestyle and psychosocial work factors and the use of ergonomic devices for patient handling.
Moreover, most existing studies do not distinguish well between onset and aggravation of LBP (11). This is of importance because investigation of risk factors for sub-chronic LBP to develop into a persistent condition is particularly recommended (12). This is due to the long-term physical impediment and psychological effects of persistent LBP, which disables people to a much larger extent than sub-chronic LBP (13). Moreover, there is some debate whether physical or psychosocial factors play an important role in the transition from sub-chronic to persistent LBP. Physical factors may be important because persons with sub-chronic LBP may be particularly susceptible to metabolic disturbances and micro-ruptures of lumbar muscles and discs from extensive patient-handling activities, enhancing the likelihood of increased discomfort, sensitization, and pain-related avoidance behavior, resulting in increased risk for aggravation of the LBP to a persistent state.
The aim of this study, therefore, was to investigate the risk of developing persistent LBP from patient-handling activities among female healthcare workers with no LBP and those with sub-chronic LBP at baseline.
Methods
Study design and population
This study is based on a prospective cohort of employees in the eldercare services in 36 Danish municipalities. The aim of the cohort was to investigate associations between work characteristics, health, and well-being. The first round of data collection started in the winter of 2004, but the main data collection took place in the spring of 2005. Data collection for the second round was, for the most part, conducted in the autumn of 2006 but continued in spring 2007.
In the first round, questionnaires were sent to 12 744 respondents who were employed in the 36 municipalities. Of these potential respondents, 9949 completed a questionnaire, yielding a response rate of 78%. One municipality withdrew from the cohort during the follow-up period, which meant that the follow-up population consisted of 9847 employees from 327 individual workplaces in the eldercare services. Due to drop-outs or other reasons, 7864 were eligible for interviewing in the second round in 2006, and 6307 responded (80% response rate). In the analyses, we excluded male respondents (N=234), respondents who were not directly engaged in the provision of care services (N=1153), and respondents with missing data (N=128).
We also excluded respondents who reported at baseline >30 days of low-back pain (LBP) in the past 12 months. This study therefore consisted of two sub-samples: (i) 1544 female healthcare workers with no LBP at baseline and (ii) 2294 female healthcare workers with sub-chronic LBP (1–30 days in the past 12 months) at baseline.
Predictive variable
The number of patient-handing activities per day was measured with a single question: “Do you perform handling of patients (lifting) or similar activities during your daily work?”, with response options: “no, never”, “seldom”, “1–2 times daily”, “3–10 times daily” “>10 times daily”. In the analyses, the response categories “No, never” and “seldom” were combined and defined as “not performing patient-handling activities”.
Outcome variable
LBP at baseline and follow-up was self-rated by the following questions from the standardized Nordic questionnaires for the analysis of musculoskeletal symptoms (14) ‘‘Have you experienced low-back trouble (pain or discomfort) during the past 12 months? How many days in total?’’, with response options: “No, not at all”, “1–7 days”, “8–30 days”, “31–90 days”, “>90 days, but not each day” and “every day”.
The variable LBP at follow-up was coded into categorical variables: (i) healthcare workers reporting “No, not at all” in the past 12 months (defined as no LBP), (ii) healthcare workers reporting LBP between 1–30 days in the past 12 months (defined as sub-chronic LBP), and (iii) healthcare workers reporting LBP for >30 days the past 12 months (defined as persistent LBP).
Covariates
Age was self-reported in years and treated as a continuous variable.
Smoking behavior was assessed by asking “Do you smoke every day?”, with three response categories: “yes”; “no, but I have smoked before”; “no, I have never smoked”.
Seniority was measured with the self-reported question “How long have you been employed at your current workplace?” and treated as a continuous variable.
Body mass index (BMI) was estimated from self-reported data on height and weight (kg/m2) from baseline and categorized as normal weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), and obese (30.0 kg/m2).
Leisure-time physical activity was classified into four different groups: predominantly sedentary, slightly active, fairly active, or very active.
Indicators of psychosocial work conditions were: (i) emotional demands: 4-item scale from the Copenhagen Psychosocial Questionnaire (COPSOQ) (15). Sample item: “Is your work emotionally demanding?” Cronbach’s alpha: 0.81. (ii) Role conflicts: 4-item scale from COPSOQ. Sample item: “Are contradictory demands placed on you at work?” Cronbach’s alpha: 0.66. (iii) Influence at work: 4-item scale from COPSOQ. Sample item: “Do you have a large degree of influence concerning your work?” Cronbach’s alpha: 0.75. (iv) Quality of leadership: 4-item scale from COPSOQ. Sample item: “To what extent would you say that your immediate superior gives high priority to job satisfaction?” Cronbach’s alpha: 0.89. Responses to the individual items were scored on 5-point Likert scales. Responses were recoded into a scale ranging from 0–100, with 100 representing the highest degree of the measured dimension of the psychosocial work environment.
The use of an ergonomic device during patient-handling activities was measured with the single question: “Do you use ergonomic (lifting) devices when you lift or move a patient?”, with the response options: “no, never”, “seldom”, “sometimes”, “often” and “very often.
Statistical analysis
Differences in baseline characteristics between the healthcare workers attending both the first (2005) and the second (2006) round of data collection (N=5046) compared to those dropping out of the second round of data collection (N=3085) were tested with chi-square tests. As we sought to identify predictors of occurrence of persistent LBP, we analyzed our data using a logistic regression model. In the analyses, we investigated the risk for persistent LBP in two separate logistic regression analyses, where respondents not performing patient-handling activities constituted the reference group. The primary association of interest was the relation between the independent variable (ie, the number of patient-handling activities) and the dependent variable (ie, persistent LBP). This relationship was adjusted in two steps. In the first step, we adjusted for age, seniority, BMI, leisure-time physical activity, and smoking behavior. In the second step, we adjusted for the same variables as in step 1, plus psychosocial work conditions, and use of ergonomic device(s) during patient handling. Moreover, the trend between the number of patient-handling activities and the risk for persistent LBP was analyzed in the second step. The P-value for the trend test was calculated by treating the categories of the daily number of patient-handling activities as an ordinal variable in the linear regression model.
In the model 1 analysis, the risk for developing persistent LBP among participants without any days of LBP in the past year at baseline was investigated. In this model, those developing sub-chronic LBP at follow-up were excluded. In an additional model analysis investigating the potential selected group contrast in the model 1 analysis, all participants with no LBP in the past year at baseline were also included at follow-up (those with 0 days of LBP in the past year versus those with ≥1 days of LBP in the past year). In the model 2 analysis, the risk for developing persistent LBP among participants with sub-chronic LBP in the past year at baseline was investigated. In this model, all participants were also included at follow-up [those developing >30 days of LBP in the past year (persistent LBP) versus those with <30 days of LBP in the past year].
Because the participants were clustered in workplaces, observations were not statistically independent (16). Therefore, all analyses were adjusted for random effects at the workplace level. In the logistic regression analysis, this was done by using the option “repeated subjects” (cluster option) in the SAS program. Data were analyzed using SAS 9.1.3. (SAS Institute, Cary, NC, USA)
Results
Healthcare workers attending both the first and second rounds of data collection (N=5046) were on average older, smokers, and had a higher seniority and level of leisure-time physical activity, but were not different with respect to BMI and the use of ergonomic device(s) at baseline compared to those dropping out of the second round of data collection (N=3085) (data not shown).
Table 1 shows characteristics of the female healthcare workers without LBP in 2005 stratified on the number of patient-handling activities per day. The groups of healthcare workers with different numbers of patient-handling activities were rather similar with respect to most characteristics. However, the group performing >10 patient-handling activities per day reported a higher percentage of current smokers and had a higher seniority, lower influence at work, and a lower quality of leadership compared to the other groups. Moreover, those not performing patient-handling activities (ie, <1 per day) used ergonomic devices less frequently than other groups.
Table 1
Characteristics of female healthcare workers without low-back pain in 2005 (N=1544) stratified on number of patient handling activities per day. [SD=standard deviation.]
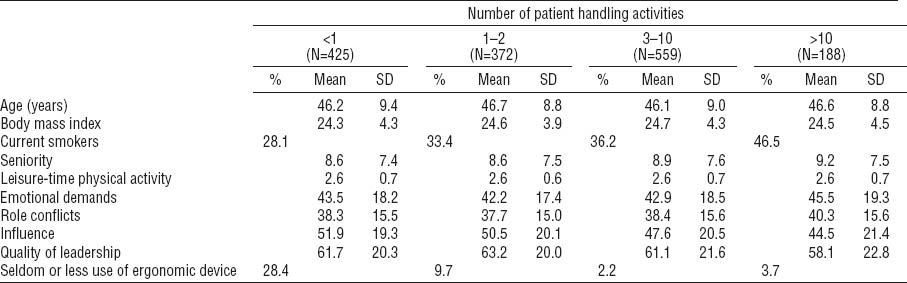
Table 2 shows characteristics of the female healthcare workers with sub-chronic LBP in 2005 stratified on the number of patient-handling activities per day. The groups of healthcare workers with different numbers of patient-handling activities were rather similar with respect to most characteristics. However, compared to the other groups, the group performing >10 patient-handling activities per day had a higher percentage of current smokers and individuals with higher seniority, more role conflicts, lower influence at work, and a lower quality of leadership. Moreover, those not performing patient-handling activities (ie, <1 per day) used ergonomic devices less frequently than other groups.
Table 2
Characteristics of female healthcare workers with sub-chronic LBP in 2005 (N=2294) stratified on number of patient handling activities per day. [SD=standard deviation.]
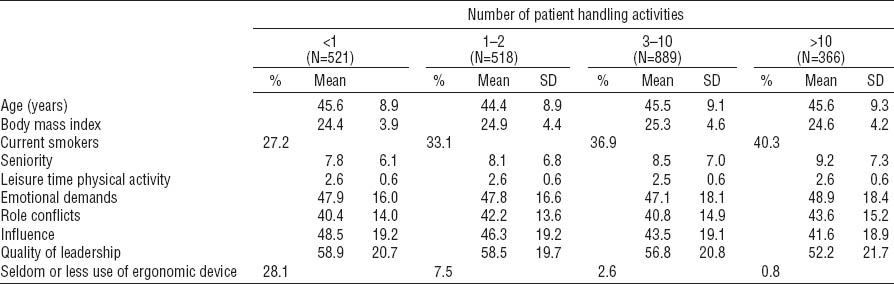
Table 3 shows results of the prospective analyses of the association between the number of patient-handling activities in 2005 and risk for developing persistent LBP in 2006 among healthcare workers with (i) no LBP and (ii) sub-chronic LBP at baseline. Adjustment for potential confounding factors such as age, BMI, smoking, seniority, leisure-time physical activity, psychosocial work conditions, and use of ergonomic device(s) imposed only a minimal effect on the risk estimates for developing persistent LBP. Among female healthcare workers with no LBP at baseline, we found neither significant associations nor a trend between the number of patient-handling activities per day and the risk for developing persistent LBP (P=0.92). Likewise in the additional analysis investigating the risk of developing LBP at follow-up (≥1 days of LBP past year), no significant association was found among female healthcare workers with no LBP at baseline [odds ratio (OR) 1.10, 95% confidence intervals (95% CI) 0.72–1.67 for those performing >10 patient handlings per day referencing those performing <1 patient handling per day].
Table 3
Logistic regression model estimating the association between number of patient handling activities in 2005 and risk for persistent (>30 days in the past 12 months) low-back pain (LBP) in 2006 among healthcare workers without LBP (0 days in the past 12 months) (N=1544) and with sub-chronic LBP (1–30 days in the past 12 months) (N=2294) in 2005. [OR=odds ratio; 95% CI=95% confidence interval.]
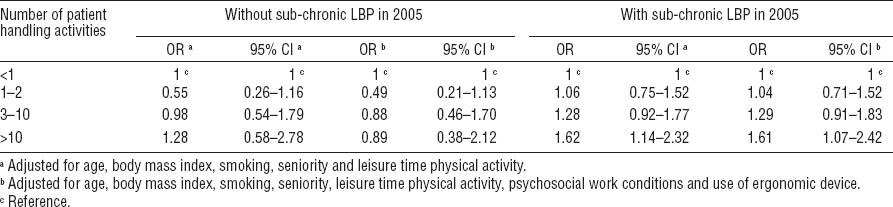
Compared to those not performing patient-handling activities among female healthcare workers with sub-chronic LBP at baseline, the multi-adjusted OR for developing persistent LBP was 1.04 (95% CI 0.71–1.52) for those with 1–2 activities, 1.29 (95% CI 0.91–1.83) for those with 3–10 activities, and 1.61 (95% CI 1.07–2.42) for those with >10 patient-handling activities per day. A significant trend between a larger number of patient-handling activities and an increasing risk for persistent LBP was found among female healthcare workers with sub-chronic LBP at baseline (P=0.01).
Discussion
The main finding of this prospective cohort study among female healthcare workers with sub-chronic LBP at baseline was that those performing >10 patient-handling activities per day had an increased risk for persistent LBP. In contrast, those with no LBP at baseline did not have an elevated risk for persistent LBP from >10 patient-handling activities per day.
These observations may be explained by the following: (i) several patient handlings per day do not contribute to an increased risk for persistent LBP, but may potentially first lead to less severe levels of LBP or (ii) patient handling is a considerable prognostic factor for the aggravation of LBP (ie, from a sub-chronic to persistent level) but not for a first incidence of LBP.
Performing >10 patient-handling activities per day was associated with an increased risk for the aggravation of LBP to a persistent condition. Specifically among the female healthcare workers with sub-chronic LBP, those performing >10 patient-handling activities per day had more than a 60% increased risk for developing persistent LBP compared to those not performing such activities. This is the first study we are aware of that investigated the role of daily frequency of patient-handling activities in the aggravation of LPB as a persistent condition. In a previous study in this cohort, we found that frequent occupational lifting and carrying of moderate and heavy loads with a forward-bent back increased the risk of LBP aggravation from a sub-chronic to a persistent state (17). Therefore, this study supports the finding that there may be significant prognostic factors in the physical work environment for sub-chronic LBP to aggravate to a persistent state.
From a preventive perspective, the observation of an increased risk for persistent LBP from >10 patient-handling activities per day among healthcare workers with sub-chronic LBP indicates that a strategy may be to limit the number of patient-handling activities to <10 per day. On the other hand, this study indicates that decreasing the number of patient-handling activities to <10 per day among female healthcare workers free from LBP at baseline cannot be expected to reduce the the number of new episodes of persistent LBP.
Strengths and limitations
The main strength of our study is the possibility to investigate prospectively the risk for development of persistent LBP among female healthcare workers both with sub-chronic LBP and with no LBP at baseline, respectively. Our study population of only healthcare workers also reduces the risk for confounding and bias from socioeconomic factors. Another strength is the adjustment for potentially confounding factors such as health and lifestyle factors, psychosocial work factors as well as use of ergonomic devices during patient-handling activities. A limitation of the study is the use of a single question on the exposure with rather arbitrary response options limiting the precision and lacking information about the type, circumstances, and mechanical loads during the patient-handling activities. Moreover, other aspects of healthcare workers’ physical work demands, such as awkward postures of the trunk that may generate a relatively high mechanical load on the back (18), were not adjusted for in the model. Moreover, covariates and the outcome are based on self-reported measures. LBP is traditionally divided into acute, sub-chronic, and chronic (persistent) states (12). However, this division in the different states of LBP cannot be properly defined by the Nordic questionnaire. On the other hand, because the natural course of LBP varies considerably between individuals (19), well-founded argumentation for appropriate cut-off points between the states of LBP is problematic. Previously, we have shown that female healthcare workers with 1–30 days of LBP in the past year did not have an increased risk for long-term sickness absence in the following year, whereas female healthcare workers with > 30 days of LBP in the past year had a significantly increased risk for long-term sickness absence (3). Therefore, we consider the applied cut-off points between sub-chronic and persistent LBP to be appropriate for this study population. Normally, ≥90 days of continuous LBP is used as a definition of “chronic LBP” (12), therefore the term “persistent LBP” was used for LBP of >30 days during the past year. The relatively high number of healthcare workers dropping out between the first and second round of data collection (N=3085) being significantly different from those participating at both rounds at several characteristics at baseline may be a bias in this study.
Concluding remarks
In conclusion, this study indicates that performing >10 patient-handling activities per day increases the risk for aggravation of LBP to a persistent condition among female healthcare workers with sub-chronic LBP. Initiatives to prevent persistent LBP among healthcare workers may focus on limiting the number of patient-handling activities to <10 per day among healthcare workers with sub-chronic LBP.



