Work stress has been found to account for a proportion of coronary heart disease (CHD) events in workers (1). Hypertension, although perhaps not the principal pathway between job strain (high job demands and low job control) and CHD, is a preventable risk factor (2), and chronic stress has been acknowledged as a credible cause of high blood pressure (BP) (3). Some recent meta-analyses have concluded that job strain is a risk factor for hypertension (4–6) but others failed to find an association (7). Additionally, the reduction in BP from day- to night-time is of importance. However, further investigations into job strain and nocturnal BP dipping and potential modifiers of this effect are required (4).
High job control has been reported as a relevant positive factor in BP presentation. Workers with low job control have been found to have higher BP than those with high job control (6, 8). However, inconsistent associations have been found between this exposure and outcome. For instance, only half of the relevant studies reviewed by Gilbert-Ouimet et al (6) showed a significant protective effect for high job control. Furthermore, job control is beneficial to nocturnal systolic BP (SBP) dipping (9), an important physiological function (10, 11) as night-time BP is a compelling predictor of cardiovascular mortality (12). Nocturnal SBP dipping is in line with contemporary stress theory, specifically the allostatic model. This model hypothesizes that the body copes with the stresses put on it by the activation of bodily systems and recovers when the stresses cease (13, 14). Stressors at work can increase allostatic load particularly when the demand on the individual carries on for some time. For example, BP may elevate at work in response to activation (stressor). However, for the body to recover there should be a corresponding reduction of BP at rest.
Researchers have found that hypertensive men with low job control had higher sleep SBP and lower SBP dipping compared to men with high job control (9). Inconsistent associations have been reported for job control and diastolic BP (DBP). High job control has been found to be associated with high DBP for females using casual BP readings (15), whereas other researchers using ambulatory BP monitoring (ABPM) readings found low job control to be associated with high DBP (8, 16).
Job control as defined by the demand–control model typically comprises two components: skill discretion (use/develop skills) and decision authority (autonomy/authority over work) (17). Some scholars have found associations to vary for these components (18). This highlights the need to distinguish between the job control dimensions which are commonly collectively seen as beneficial. New job characteristic questionnaires specifically discriminate between the dimension of possibility for development and influence at work (Copenhagen Psychosocial Questionnaire, COPSOQ) (19). To date no investigation of these aspects of the COPSOQ and hypertension has been undertaken.
Research has found older workers to be more vulnerable to adverse work characteristics particularly with regard to physical health (20, 21). Workers >50 years who had a cardiac event were found to be more likely to have low job control whereas no association was found for younger workers (21). Although BP usually increases with age, older workers are thought to adapt to their work environment where control over their work has developed with time (13), but this may vary by social class. Little has been done to investigate job control (specifically) and BP in a sample of older workers. This study investigates the association of different components of job control with BP and BP dipping in a middle-aged Irish primary care-based sample using clinic and 24-hour ambulatory BP measurements. The objectives of this study are to: (i) examine the BP levels of the complete sample including workers and non-workers; (ii) explore the relationship of the job control dimensions with day- and night-time BP; and (iii) investigate nocturnal SBP dipping among workers while taking sociodemographics and lifestyle factors into account. We hypothesize that nocturnal SBP dipping is more pronounced among those with high job control (ie, high influence at work and high possibility for development).
Methods
Participants
The Mitchelstown Study is a cross-sectional study on middle-aged (50–69 year-olds) Irish men and women sampled from a large primary healthcare center in North Cork, Ireland (22). In total, 2047 participants were recruited to the study with a 67% response rate. Written informed consent was obtained from all participants prior to the study. The Clinical Research Ethics Committee of the Cork Teaching Hospitals, Cork, Ireland, granted ethical approval for the study.
Study variables
Work status and job characteristics
The work status of each participant was established by asking whether they were currently working (N=1025), retired (N=605), in unpaid labor (N=234), or unemployed (N=183). Retired, unpaid labor, and unemployed were classified as non-workers for the purpose of this paper.
Job characteristics were ascertained using the COPSOQ (19). Each working participant completed the questionnaire based on the job they had done for the longest period of time. Two scales from the COPSOQ questionnaire were used: possibility for development and influence at work. Each scale was a composite of four items and had a theoretical range of 0–100. The average score for each scale was then calculated only if at least half of the items were complete. A high score was indicative of high possibility for development and high influence at work. Cronbach α for the individual scales were: possibility for development α=0.82 (males α=0.78, females α=0.83) and influence at work α=0.83 (males α=0.84, females α=0.81). Both scales were dichotomized at the median.
Blood pressure
Clinic BP readings were taken using an oscillometry device (Omron™ M7, Omron Corporation, Kyoto, Japan). Hypertension was defined as average SBP ≥140 mmHg or average DBP ≥90 mmHg on clinic BP readings (23).
All participants were offered ABPM, but some declined. The BP was recorded every 30 minutes, day and night, for 24 hours using Meditech ABPM-05 (Meditech Ltd, Budapest, Hungary). These data were then read using dabl® software (24). Each participant recorded bed and rising times, and this was used to calculate average day- and night-time SBP and DBP only if there were ≥10 valid daytime and 5 valid night-time readings (25) and work/non-work status was known. For the purpose of this paper those classified with a high reading had a daytime ABPM of SBP ≥135 and DBP ≥85 mmHg and night-time ABPM of SBP ≥120 and DBP ≥70 mmHg. SBP dipping status was then calculated using the following formula (1-asleep SBP/awake SBP)×100 and categorized as dippers or non-dippers. Dippers were those who had an average SBP reduction during the night-time ≥10% of mean daytime SBP. Non-dippers were those who had a reduction of <10% in nocturnal SBP from daytime recordings (10).
Covariates
Treatment for hypertension was established by asking the participant “Has your doctor given you a prescription for blood pressure tablets?”
Alcohol intake was assessed by asking “How often do you have a drink containing alcohol?” and “During the past seven days how many standard drinks of any alcoholic beverage did you have each day?” Moderate and not-moderate drinkers were established from the first question (26). The weekly units consumed were calculated from the second question.
Physical activity was measured using the short form of the International Physical Activity Questionnaire (IPAQ) (27). Participants were categorized as having low, moderate, or high physical activity. Smoking status was established by asking the questions “Do you now smoke?” and “Have you smoked ≥100 cigarettes in your life?” Smokers were categorized into current and non-/ex-smokers.
Other variables used in this analysis included age, gender, BMI, education, and ABPM worn on a work day. Age was used categorically, 50–59 or 60–69 years of age and continuously in the regression models. The standard formula for BMI calculation was used from weight and height measurements (22). Educational level was established by enquiring about the highest level of schooling achieved (primary, secondary/tertiary). Self-reports of whether the ABPM was worn on a work or leisure day were recorded when the participant returned the device.
Descriptive analysis was carried out on the demographic characteristics and clinic BP of all participants (N=2042) using independent sample t-test. This analysis was then carried out for those who had an ABPM done (N=1112), investigating specifically awake and asleep SBP, DBP, and nocturnal SBP dipping. Logistic regression analysis was then performed to investigate the association between job control for workers who did not report taking anti-hypertensive treatment (N=401) and clinic BP, awake and asleep BP from ABPM readings, and finally nocturnal SBP dipping. These models were adjusted for sociodemographic factors. Data were analyzed using PASW version 18 (IBM, Armonk, NY, USA).
Results
Table 1 shows the clinic BP readings by sociodemographic, lifestyle-related factors, and work characteristics. SBP significantly increased by age, male gender, in the overweight/obese category, drinking level, consumption of anti-hypertensive medication, non-work status, and reported low physical activity levels in the entire sample of workers and non-workers. SBP also increased significantly with level of influence at work for workers only.
Table 1
Mean and standard deviation (SD) for clinic systolic blood pressure (SBP) and clinic diastolic blood pressure (DBP) by demographic details, lifestyle and work characteristics of the complete sample. [BMI=body mass index.]
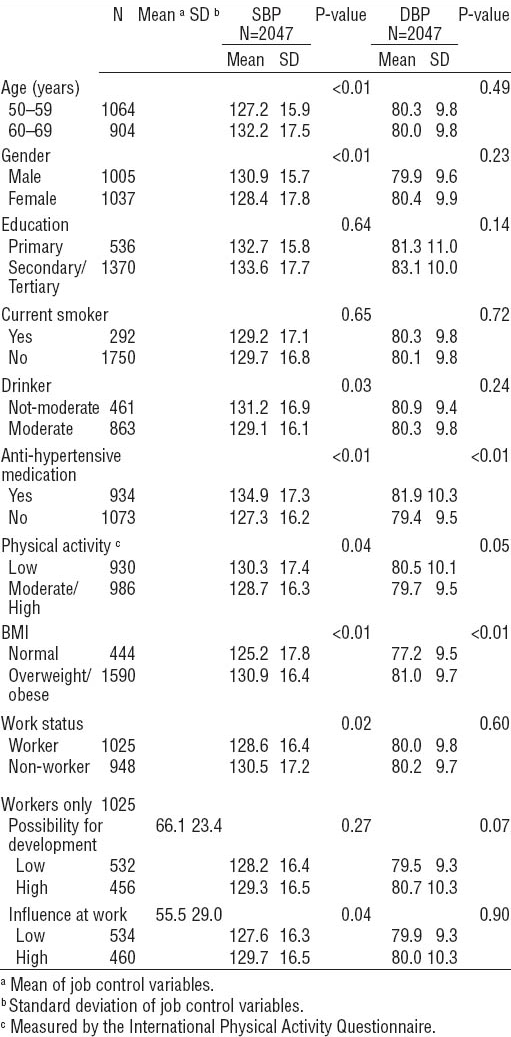
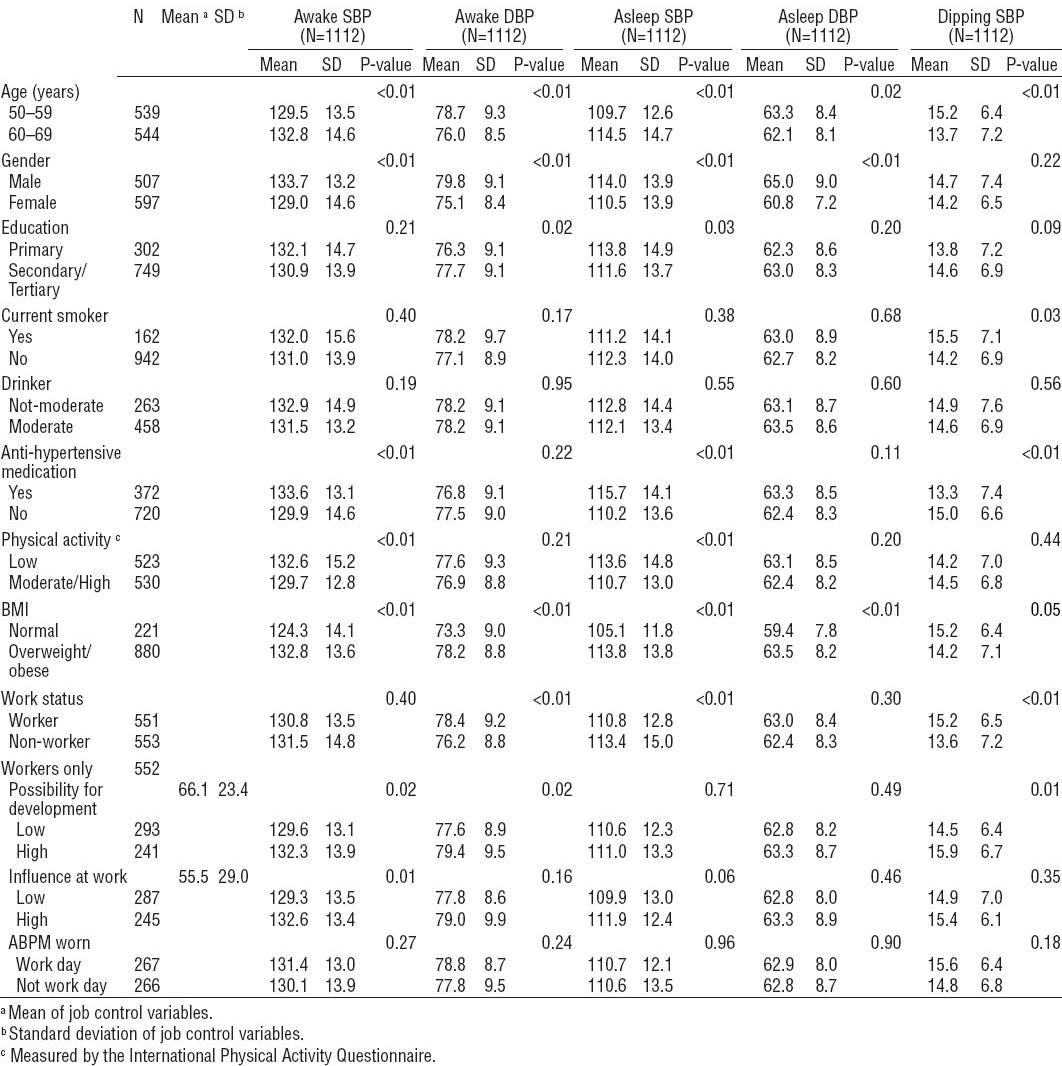
SBP measurements from ABPM showed similar results to those from clinic measurements across most sociodemographic and lifestyle-related factors, whereas DBP measurements varied (table 2). However, workers had significantly lower SBP in the clinic reading than non-workers (table 1), where no significant association was found with awake ABPM SBP (table 2). The reverse was true for DBP with workers having significantly higher awake ABPM DBP levels (table 2) with no significance difference in clinic DBP (table 1). The components of job control were more consistently positively associated with awake than clinic SBP. Within ABPM results, similar patterns can be seen between awake and asleep SBP and DBP by sociodemographic factors except for education, work status, and job control. Workers with high possibility for development had higher average nocturnal SBP dipping than those with low possibility.
Table 2
Mean and standard deviation (SD) for ambulatory blood pressure (ABPM) – awake/asleep systolic (SBP), diastolic (DBP) blood pressure and dipping SBP – by demographic details, lifestyle, and job characteristics of the complete sample. [BMI=body mass index]
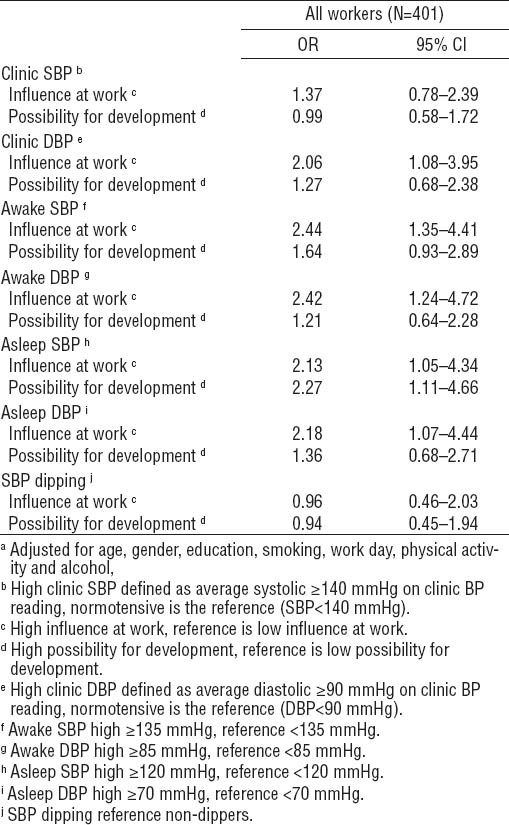
The association between influence at work and possibility for development with clinic and ABPM BP in addition to nocturnal SBP dipping can be seen in table 3 for all workers who were not on anti-hypertensive medication (N=401). High influence at work was associated with high clinic DBP and high awake and asleep SBP and DBP with odds ratio (OR) of 2.06–2.44. High possibility for development was associated with high asleep SBP [OR 2.27, 95% confidence interval (95% CI) 1.11–4.66) P=0.03]. No association was seen for the job control dimensions and clinic SBP or SBP dipping.
Discussion
This study set out to examine BP in relation to sociodemographic factors for a primary healthcare-based sample (objective 1). Furthermore, we investigated the association between job control and BP for a subset of that sample who were current workers (objective 2) and specifically examined whether workers with high job control were more likely to reduce BP during sleep (objective 3). We found a clear association between influence at work and BP, however the association between possibility for development and BP was not so clear. The null hypothesis was accepted as no evidence of a pronounced reduction in SBP at night was found among those with high job control, despite evidence of activation during the day (albeit inconsistent) with higher SBP for those with higher control at work. Incomplete recovery from the stresses of the day has been discussed as a principal component in the hypothetical causal pathway between an acute stressor and chronic ill-health (28). Our study showed workers with high job control had awake SBP levels of up to 3 mmHg higher than those with low job control. The clinical significance of this difference is evident from previous work where a 2 mmHg reduction in usual SBP for middle-aged people resulted in a 10% reduction in stroke mortality and approximately a 7% reduction in mortality from ischemic heart disease (29).
Systematic reviews and meta-analyses done in this area typically focus on job strain as a combination of high work demands and low control (4–7), but this present paper specifically examines job control. No conclusive association between job control and BP levels has been found (6). However, ABPM has not always been used. As discussed by Schnall et al (30) ABPM readings are preferable to casual readings in research. Additionally ABPM results are also recommended for the diagnosis of hypertension (31). ABPM gives a more reliable measurement yielding a valid average BP with no observer bias. Recent work has highlighted the importance of examining both dipping status and absolute BP levels (32). Our study failed to find an association between job control and SBP dipping, resulting in OR close to 1. We excluded participants diagnosed with hypertension where other scholars specifically investigated those with high clinic BP (9). Our workers with high job control were more likely to have high asleep SBP. High influence at work or skill discretion was consistently associated with high SBP and DBP in clinic and ABPM readings with the exception of clinic SBP. This could result in increased cardiovascular risk (32–34). Possibility for development did not show the same significant associations. This reinforces the importance of examining job control components separately. The use of clinic BP readings would not allow identification of such a risk owing to its once-off measurements; however it is informative for BP researchers to compare clinic and ABPM results as we have done in this paper.
Job control can be seen as a proxy measure for social class implying that those with high job control had higher occupational status and were generally in a higher socioeconomic group with better life resources and healthier lifestyles. However, contrary to our expectations, high job control in our sample was associated with high BP, unlike earlier research (8, 35). Scholars have previously found a significant association between low job control, hypertension, and SBP dipping when using the job control dimensions collectively (6, 9, 16). Our study examined these dimensions separately owing to recent findings of differing associations for these components (18).
Some of the variables we adjusted for may have resulted in an over-adjustment, such as alcohol intake. High alcohol consumption has been found to increase BP (36, 37) and is a valid confounding factor in the association between job control and hypertension. Nevertheless, not all researchers adjust for this variable (8, 16, 35) perhaps owing to alcohol being a causal factor for hypertension.
It could be postulated that older workers in this study with high control and hypertension were exhibiting the defense reaction and those with low control the defeat reaction (38, 39). Although in positions of authority, older workers may feel threatened by younger workers bringing new ideas into the workplace. Furthermore, in competitive, economically unstable times, management may view younger workers as more cost effective than older workers.
It is important to take into consideration that workers who wore the ABPM device on a work day were not engaged in work for the full quota of daytime measurements as their BP was averaged over the entire awake hours. This may result in dilution of the association between job control and BP. Although this is not ideal, data on specific work hours were not available in this mixed-occupation sample.
There are some limitations to this paper. Not all those who were recruited into the study had ABPM. However, we are confident that this did not systematically bias the findings. Although the sample with ABPM were older (P<0.01) and comprised a higher proportion of females (P=0.01), there were no differences in level of education, smoking, or alcohol intake compared to those who did not have the recording. Furthermore, investigating workers only, there was no difference for possibility for development (P=0.21) or influence at work (P=0.93) between workers who had or did not have an ABPM.
Although the internationally validated scales from the COPSOQ performed well in the group studied (Cronbach a were >0.70), the use of self-reported job-control measures may have systematically biased the associations between job control and hypertension towards the null. For example, Greiner et al (40, 41) argued that some people may deny or suppress stress experiences and report lower work stressor levels. However, denial and suppression are also known personality factors that may play an important role in the etiology of high BP. By comparing self-reported with observed stressor levels, the authors showed that those with high observed stressor levels but low self-reported stressor levels (so-called “deniers”) were at highest risk for hypertension. However, our outcome variable (ABPM) was not measured by self-report somewhat balancing the self-reported exposures and avoiding common methods variance bias. An over- or indeed underestimation of job control could be reduced by using job analysis data by independent observers (40). However, this was not possible in the current study.
It is conceivable that a number of healthy males, who typically are not good at visiting the doctor, may have been inadvertently omitted from the sample as all participants had to be registered patients. However, samples taken from a primary care setting in Ireland have previously been found to be representative of the general population (42). The healthy worker effect may have influenced our results with healthier people staying in work or highly stressful occupations (20). The use of a cross-sectional study design prohibits causality to be determined (43). Finally, education was used as a proxy measure for social class but this may have resulted in residual confounding. Nevertheless it was seen as preferable to classifying participants by the occupation they had held for the longest period of time, a method used previously (44, 45) which could result in an arbitrary classification (46). A more accurate approximation of social class could have been made if data were available on income levels. Although there was very little movement between jobs for this group of older workers, it is necessary to acknowledge the issue of recall bias when basing job characteristics on the longest held occupation. Retrospectively participants could overestimate their control at work resulting in greater associations between job control and high BP.
Nevertheless, this study included a large sample of older heterogeneous workers with ABPM data. Both activation and recovery of BP were investigated in relation to reported job control for workers. Further research should aim to incorporate observer and self-reported stressor data to examine the associations between job control and hypertension using ABPM. For generalizability, it would be advantageous if this was carried out on a number of different occupations investigating specific work hours, evening and night-time BP. Gender may explain some of the unexpected associations in our study and further analysis should be done. However, this goes beyond the scope of the present paper.
In conclusion, older workers with high job control may be at risk of cardiovascular disease resulting from high day- and night-time BP with no evidence of nocturnal SBP dipping. It appears older workers’ level of influence impacts negatively on their BP. Attempts should be made in the workplace to support workers with high job control. This could take the form of health promotion initiatives, in addition to enhancing, supporting and up-dating skills.