Worldwide, musculoskeletal pain is a leading cause of years lived with disability. In the 2010 Global Burden of Disease Study, lower-back pain (LBP) was found to be the number one cause of years lived with disability, neck pain the fourth, and other musculoskeletal disorders the sixth (1). Additionally, musculoskeletal pain is well documented to increase risk of disability pension retirement and long term sickness absence (2, 3).
The most common sites for musculoskeletal pain among office workers are pain in neck-shoulders and the lower back (2, 4). Annual prevalence of neck-shoulder pain in office workers has been found to be 27–48% (2, 4, 5) and, for 11–14%, the pain has limited sufferers’ ability to perform daily activities (5). The annual prevalence of LBPhas been found to be 16–25% (2, 6). The workday of office workers is characterized by desk-based work, which entails many hours of sitting. Several studies have found high sitting time to be a risk factor especially for neck-shoulder pain (5, 7–12).
As high sitting time is associated with musculoskeletal pain, it is relevant to test if addressing sitting time affects musculoskeletal pain. However, only very few studies have considered this. Thorp et al (13) conducted a 5-day cross-over intervention study among 23 overweight/obese office workers and found that transitioning between sitting and standing work in 30-minute bouts reduced lower-back discomfort, but not other musculoskeletal discomfort.
The aim of this study was to evaluate the effects of a 3-month intervention aimed at reducing occupational sitting time on musculoskeletal pain.
Methods
Trial design
Take a Stand! was a cluster randomized controlledtrial (RCT) conducted in Denmark and Greenland from November 2013 to June 2014 aiming to reduce sitting time among office workers. An RCT design was used as the intervention was delivered at office level. Primary outcomes of the intervention were sitting time at work, prolonged sitting periods, and sit-to-stand transitions at 1-month follow-up. Secondary outcomes were the sitting outcomes at three months, waist circumference and body fat percentage at three months and musculoskeletal pain at one month. Findings on sitting behavior and anthropometry are reported elsewhere (14). The local Ethics Committee in Denmark (H-6-2013-005) and in Greenland (project 20914-3, id: 2014-095402) approved the study, which was prospectively registered at www.clinicaltrials.gov (NCT01996176). Procedures were designed in accordance with the Helsinki Declaration.
The intervention and its effect on sitting time
The Take a Stand! intervention included five elements: (i) appointment of local ambassadors and management support, (ii) environmental changes, (iii) a lecture, (iv) a workshop aiming at ensuring local adaptation at individual, office and workplace level, and (v) e-mails and text messages. The intervention focused on four strategies to reduce sitting: using a sit-stand desk, breaking up prolonged periods of sitting, having standing and walking meetings, and setting common goals at office level. Control participants were instructed to behave as usual. A detailed description of the intervention is reported elsewhere (14).
Sitting time at work was reduced by 71 minutes after one month and 48 minutes after three months in the intervention compared to the control group. The reduced sitting time at work was primarily replaced by increased standing time. There were no changes in leisure sitting time or in time spend on physical activity during work or leisure. Further results on sitting outcomes are reported elsewhere (14).
Participants
Four workplaces participated in the trial. At each workplace, 4–6 offices (clusters) participated, totalling 317 participants. Eligible workplaces were office-based, with employees who sat most of the workday, and each workplace had to have at least four offices constituting well-defined spaces separated by walls, floors, or locations. In addition, management had to agree to participate in activities and invest resources in the project. Details of the assigned offices are shown in table 1. Eligible individuals were ≥18 years old, understood Danish, and worked >4 days/week (>30 hours/week). Exclusion criteria were pregnancy and sickness or disabilities affecting the ability to stand or walk. All participants had sit-stand desks prior to inclusion. Participants gave informed consent prior to the study. Details on recruitment are described elsewhere (14).
Table 1
Baseline office (cluster) characteristics (N=317). [I=intervention; C=control; IQR=interquartile range.]
| Office number | Status | N | Women | Age | Pain score (0–6)a | |||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||
| % | N | Median | Range | Median | IQR | |||
| Workplace A | ||||||||
| 1 | I | 33 | 55 | 18 | 48 | 28–63 | 1.0 | 0–2 |
| 2 | I | 18 | 56 | 10 | 51 | 26–61 | 1.0 | 0–2 |
| 3 | C | 24 | 75 | 18 | 43 | 19–60 | 2.0 | 0–3 |
| 4 | C | 22 | 77 | 17 | 43 | 28–64 | 1.0 | 0–4 |
| Workplace B | ||||||||
| 1 | I | 10 | 90 | 9 | 46 | 24–61 | 2.0 | 1–4 |
| 2 | I | 10 | 70 | 7 | 42 | 27–57 | 0.0 | 0–1 |
| 3 | I | 27 | 52 | 14 | 47 | 27–64 | 1.0 | 0–2 |
| 4 | C | 6 | 67 | 4 | 57 | 42–61 | 1.0 | 1–1 |
| 5 | C | 21 | 67 | 14 | 44 | 32–64 | 1.0 | 0–2 |
| 6 | C | 6 | 33 | 2 | 49 | 32–57 | 1.5 | 0–3 |
| Workplace C | ||||||||
| 1 | I | 14 | 93 | 13 | 41 | 26–57 | 2.0 | 1–3 |
| 2 | I | 21 | 62 | 13 | 50 | 27–61 | 1.0 | 0–3 |
| 3 | C | 20 | 60 | 12 | 51 | 29–60 | 1.0 | 1–3 |
| 4 | C | 20 | 95 | 19 | 43 | 24–62 | 2.0 | 2–3 |
| Workplace D | ||||||||
| 1 | I | 10 | 30 | 3 | 49 | 32–62 | 0.5 | 0–1 |
| 2 | I | 10 | 40 | 4 | 47 | 28–58 | 1.5 | 0–2 |
| 3 | I | 20 | 70 | 14 | 51 | 28–61 | 1.0 | 0–1.5 |
| 4 | C | 15 | 60 | 9 | 45 | 25–65 | 0.0 | 0–1 |
| 5 | C | 10 | 100 | 10 | 48 | 32–63 | 2.0 | 1–3 |
| Total (19) | 10/9 | 317 | 66 | 210 | 46 | 19–65 | 1.0 | 0–3 |
Sample size calculation
Sample size calculations were carried out for the primary outcome of the intervention (ie, sitting time) based on principles for community intervention trials by Donner & Klar (15). The number of offices and employees per office were calculated. We assumed an intra-class correlation coefficient of 0.05–0.2 based on best estimates from existing literature (16, 17), 80% power, a two-sided test, and a significance level of 5%. We expected a reduction in daily sitting time of 60 minutes and a standard deviation (SD) of daily sitting time of 50–100 minutes. Calculations showed that a minimum of 12 offices with 25 employees per office (300 participants in total) were required.
Data collection
Data were collected at baseline and after one and three months. Questionnaire data (web-based) were obtained at all three points in time. Musculoskeletal pain was measured by three items on pain in neck-shoulders, back (including both back and lower back), and extremities (arms, hands, legs, knees, hips or joints). For each pain area, participants reported in three categories (very bothered, little bothered, not bothered) how bothered they had been by pain within the past 14 days.
Sitting behavior was measured with an ActiGraph GT3X+ accelerometer worn on the front of the thigh 24 hours/day for five days (Monday–Friday). During the accelerometer periods, participants noted sleeping and working hours in a log. Data were processed using Acti4 software, specially developed for thigh mounting of the ActiGraph and found to have high sensitivity and specificity (18–20). Acti4 compiles total minutes spent sitting/reclining, standing, walking, climbing stairs, running and cycling. Eligible days had to include ≥4 hours of work or 4 hours of leisure. Further details on the activity monitor and data processing are found elsewhere (14).
Randomization
Within each workplace, offices were randomized for intervention or control at a ratio of 1:1.
Randomization took place before baseline measurements were recorded, but allocation was not disclosed to participants, researchers or data collectors until the baseline assessments had been completed. Further details on randomization are described elsewhere (14).
Outcomes
Musculoskeletal pain at one month follow-up was predetermined as a secondary outcome of the intervention. Musculoskeletal pain was operationalized as pain in neck-shoulders, back, and extremities as well as total pain score combining degree of pain and number of pain sites. These variables were measured at baseline, one and three months at individual level. In addition to the secondary outcome at one month follow-up, this paper will also include exploratory analysis of the pain variables at three months follow-up.
Pain variables were dichotomized combining “very bothered” and “little bothered” in one category versus “not bothered”. In addition, the number of pain sites 0–3) and the degree of pain felt at each site (0–2) were summarized to a total score from 0 (no pain at no sites) to 6 (very bothered by pain at all three sites).
Statistical analysis
Analyses were conducted using STATA/IC-14.0 (StataCorp, College Station, TX, USA).
Multilevel mixed-effects logistic regression was used for analyses with site-specific pain variables as outcome, while negative binomial regression was used for total pain score as outcome. First analyses were carried to assess the intervention effect at 1 and 3 months follow-up, taking baseline values into account and including a random effect to account for the cluster-structure of data. Then an interaction term was included between randomization status (ie, intervention or control) and month (baseline, and one and three months follow up), allowing for differences in intervention effect between follow-up assessments. This was done to assess the intervention effects between intervention and control, and the difference between baseline and follow-up in the control group. The interaction term defines whether the level of the outcome in the intervention group differed from what would have been expected if there was no effect of the intervention.
All models included fixed effects of workplace, gender and age, and a random intercept was included to account for repeated measurements on participants. Accordingly, the equation for the statistical model was:
µij = α + β1×gender + β2×age + β3×workplace +β4×group + β5×time + β6×group×time + ϒparticipant
where µij is the outcome for person i in workplace j.
Sensitivity analyses were carried out with pain dichotomized as “very bothered” versus “little/not bothered” and handling missing with last observation carried forward.
Results
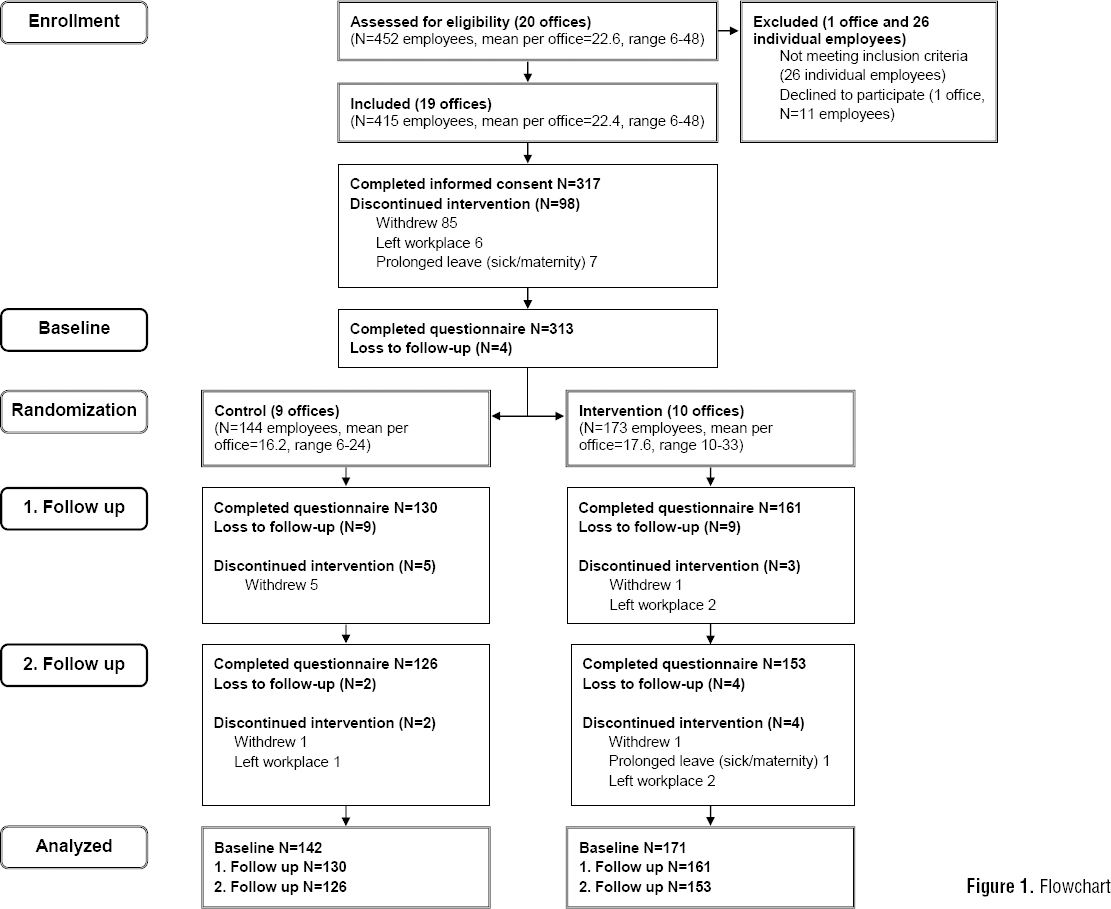
A flow chart of offices and participants is shown in figure 1. Of the eligible individuals, 317 participants (76%) completed informed consent. Of those 313 participants (99%) completed the baseline questionnaire, 291 (92%) completed the questionnaire one month follow-up and 279 (88%) completed the questionnaire three months follow-up.
Baseline participant characteristics
Of the 317 participants, 66% were women and mean age was 46 years, baseline characteristics on health and sitting time are displayed in table 2. At baseline, 51% of participants felt bothered by pain in neck-shoulders the past 14 days, while 41% were bothered by pain in the back and 38% by pain in the extremities. On average, participants scored 1.6 (SD 1.6) on the total pain score at baseline. Pain levels were almost equal in intervention and control groups and across clusters (table 1 and table 3).
Table 2
Baseline participant characteristics in Take a Stand! (N=317) (SD=Standard Deviation. BMI=Body Mass Index. MVPA=Moderateto-Vigorous Physical Activity (total time spent walking fast (>100 steps/min), running, climbing stairs, rowing and cycling))
| Intervention (N=173) | Control (N=144) | All (N=317) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||||
| N | % | Mean | SD | N | % | Mean | SD | N | % | Mean | SD | |
| Demographic factors | ||||||||||||
| Age (years) | 47 | 10 | 46 | 11 | 46 | 10 | ||||||
| Women | 105 | 61 | 105 | 73 | 210 | 66 | ||||||
| Higher education | 130 | 76 | 82 | 57 | 212 | 67 | ||||||
| Health and health behavior | ||||||||||||
| Body mass index | 26 | 5.0 | 27 | 4.8 | 26 | 4.9 | ||||||
| Self-rated health, less good/bad | 17 | 10 | 11 | 8 | 28 | 9 | ||||||
| ≥1 day of sickness absence, past 14 days | 27 | 16 | 13 | 9.4 | 40 | 13 | ||||||
| Smoker | 18 | 11 | 25 | 18 | 43 | 14 | ||||||
| Sitting and physical activity | ||||||||||||
| Sitting time (minutes/8-hour workday) | 345 | 54 | 335 | 59 | 340 | 57 | ||||||
| Standing time (minutes/8-hour workday) | 82 | 45 | 96 | 52 | 88 | 48 | ||||||
| Sit-to-stand transitions, N/hour workplace sitting | 6.2 | 2.8 | 6.4 | 2.8 | 6.3 | 2.8 | ||||||
| Prolonged sitting periods a, N/8-hour workday | 3.0 | 1.3 | 2.7 | 1.1 | 2.8 | 1.3 | ||||||
| Steps (N/hours work) | 482 | 172 | 442 | 144 | 464 | 161 | ||||||
| Sitting time (minutes/8-hour leisure) | 291 | 53 | 289 | 49 | 290 | 51 | ||||||
| MVPA in leisure (minutes/8-hour leisure) | 45 | 22 | 44 | 19 | 45 | 21 | ||||||
| Steps (N/hours leisure) | 709 | 312 | 702 | 278 | 706 | 297 | ||||||
Table 3a
Pain in intervention compared to control group. The number of participants in intervention and control group feeling little or very bothered by pain at the three different pain sites and at three time points. Adjusted for workplace, age and sex. [OR=odds ratio. 95% CI=95% confidence interval.]
| Intervention group | Control group | Difference between intervention and control | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||||
| Baseline (N= 171) | 1 month follow-up (N=161) | 3 months follow-up (N=153) | Baseline (N=142) | 1 month follow-up (N=130) | 3 months follow-up (N=126) | 1 month follow-up | 3 months follow-up | |||||
|
|
|
|
|
|
|
|
|
|||||
| Pain a | Pain a | Pain a | Pain a | Pain a | Pain a | OR | 95% CI | P-value | OR | 95% CI | P-value | |
| Neck-shoulder | 87 | 71 | 63 | 73 | 64 | 69 | 0.73 | 0.40–1.32 | 0.30 | 0.52 | 0.30–0.92 | 0.02 |
| Back b | 68 | 61 | 59 | 61 | 56 | 52 | 0.80 | 0.44–1.45 | 0.46 | 0.91 | 0.51–1.63 | 0.74 |
| Extremities c | 60 | 54 | 61 | 60 | 48 | 55 | 1.03 | 0.57–1.86 | 0.93 | 1.00 | 0.59–1.69 | 0.99 |
Table 3b
Pain in intervention compared to control group. The number of participants in intervention and control group feeling little or very bothered by pain at the three different pain sites and at three time points. Adjusted for workplace, age and sex. [SD=standard deviation.]
| Intervention group | Control group | Difference between intervention and control | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||||||||||
| Baseline (N= 171) | 1 month follow-up (N=161) | 3 months follow-up (N=153) | Baseline (N=142) | 1 month follow-up (N=130) | 3 months follow-up (N=126) | 1 month follow-up | 3 months follow-up | |||||||||||
|
|
|
|
|
|
|
|
|
|||||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | β | 95% CI | P-value | β | 95% CI | P-value | |
| Pain score, all sites (0–6) a | 1.57 | 1.59 | 1.34 | 1.34 | 1.38 | 1.39 | 1.74 | 1.63 | 1.56 | 1.47 | 1.72 | 1.59 | -0.13 | -0.23– -0.03 | 0.01 | -0.17 | -0.32– -0.01 | 0.04 |
Effect on specific pain sites
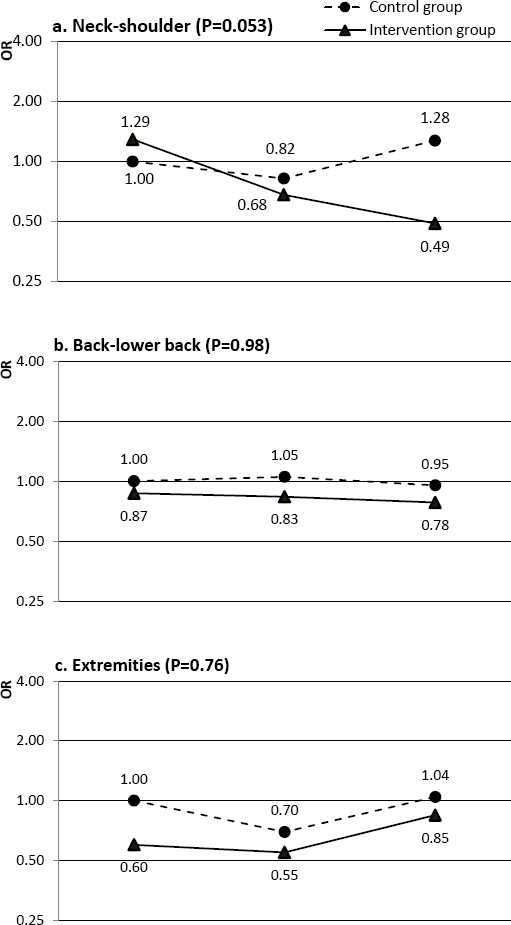
At one month, there was no difference in odds ratio (OR) for pain in neck-shoulders between the two groups. However, after three months OR for pain in neck-shoulders in the intervention group compared to the control group was 0.52 (95% CI 0.30–0.92, P=0.02) when taking baseline values into account. For pain in the back and extremities, there were no differences between intervention and control, neither at one nor three months follow-up (table 3a). Looking at the overall group×time interaction for neck-shoulder pain test for trend was P=0.053, mainly due to a reduction in neck-shoulder pain in the intervention group between one and three months follow-up. For pain in the back and extremities, there was no over-time effect (figure 2).
Figure 2
Odds ratio (OR) for pain experience during Take a Stand! Pain in neck-shoulder (a), back (b) and extremities (c) at baseline, 1 and 3 months follow-up for intervention group and control group. P-values represent the nested log likelihood test for the model with the interaction between time and randomization compared to the model without and thus whether there is a time effect in the model. Adjusted for age and sex.
Effect on total pain score
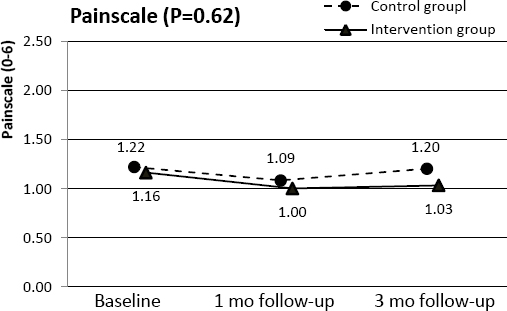
When comparing intervention and control groups at one and three months, taking baseline levels into account, there was a slight reduction in total pain score. At one month follow-up, the intervention group had a score of -0.13 (95% CI -0.23– -0.03, P=0.01) compared to the control group and, at three months follow-up, a score of -0.17 (95% CI -0.32– -0.01, P=0.04) (table 3b). However, when looking at the overall time effect there was no difference between intervention and control group over the three month intervention period (test for trend P=0.62) (figure 3).
Figure 3
Pain score during Take a Stand! Mean pain score at baseline, 1 and 3 months follow-up for intervention group (Take a Stand!) and control group (treatment as usual). P-values represent the nested log likelihood test for the model with the interaction between time and randomization compared to the model without and thus whether there is a time effect in the model. Adjusted for age and sex.
Sensitivity analyses
For the specific pain areas, sensitivity analyses were carried out using a dichotomization with not or little bothered versus very bothered. These sensitivity analyses did not materially change the results found for the primary analysis (supplementary table A, www.sjweh.fi/index.php?page=data-repository).
Missing numbers are displayed in the flowchart (figure 1). When handling missing values with last observation carried forward, results did not change (supplementary table B, www.sjweh.fi/index.php?page=data-repository).
Harms
At the three months follow-up, participants in the intervention group were asked about negative consequences of the intervention. Increased level of noise was experienced by 8% whereas, decreased personal productivity, decreased meeting quality, persistent pain in back or legs/feet, or other negative consequences were reported by <6%.
Discussion
After one month intervention in Take a Stand! there were no changes in prevalence of pain in any of the three pain sites: neck-shoulder, back, or extremities (secondary outcomes of the intervention). After three months, prevalence on neck-shoulder pain was slightly reduced in the intervention compared to the control group, but for pain in back and extremities no changes were found (exploratory analyses). For total pain score, there was a slight reduction in the intervention compared to the control group at one and three months follow-up. However, due to the exploratory nature and multiple statistical testing, the results must be interpreted with caution and verified in a randomized setting focusing primarily on the effectiveness of the intervention on musculoskeletal pain.
Compared to other intervention studies, Pronk et al (21) found a reduction in upper-back and neck pain after their four-week intervention among the 23 office workers in the intervention group, who received a sit-stand device to their desk. They found no change in lower back pain. Those results are confirmed in a larger group of participants in the present study. Thorp et al (13) found a slight reduction in lower-back discomfort but no effect on discomfort in neck, shoulders, upper-back, or extremities. However their intervention only lasted for five days as compared to three months in the present study, and their measure of pain differed from the one used in the present study.
From the present analysis of the study, it is not possible to determine whether the effect on musculoskeletal pain is a result of the reduced sitting time after the intervention or other components of the intervention. An evaluation of this requires a mediation analysis. However, as the effect is small, this would not be feasible. Nevertheless, as observational studies on sitting time and musculoskeletal pain show a positive relationship between sitting time and prevalence of neck-shoulder pain (5, 7, 8), but not LBP (9–12), and we found an effect on neck-shoulder pain and not LBP, these findings are in line with the program theory that the Take a Stand! intervention reduced sitting time, which lead to reduced neck-shoulder pain.
Regardless of the mechanism a reduction in neck-shoulder pain obtained in only three months is very relevant, as musculoskeletal pain is very common and costly (1–3). However, the reduction in total pain score was quite small (-0.13– -0.17) on a 6-point scale. Thus it seems like the intervention was successful in reducing neck-shoulder pain, but not to a degree that positive effects on harder outcomes like sickness absence can be expected.
A major strength of the present study was the RCT making it possible to assess the changes in pain in the intervention compared to the control group. In addition, including 317 participants in three months makes it both larger and longer than previous studies. Finally, sitting behavior was measured with a thigh-placed accelerometer worn 24 hours/day, which results in very good estimates of time used sitting and standing.
However, the pain measure used was not very precise as pain was only measured with three categories (not bothered, little bothered, very bothered). As changes in musculoskeletal pain seem to be small during the intervention period, an instrument with finer categories might be better suitable to detect even small changes. In addition, the intervention period of three months might not be sufficient to detect changes in musculoskeletal pain, which might have developed through years of sedentary work life and thus could take longer time to reverse. Finally, it is important to remember that sitting time was mainly replaced by standing, which might influence the effect on musculoskeletal pain. If for example sitting was replaced by walking or other light activity the effect on musculoskeletal pain might be greater. Substituting sitting with standing could lead to increased pain especially in legs and feet (22), however this was not the case in Take a Stand! as the present study shows that the intervention did not result in increased pain in extremities. When asking directly about negative consequences (harms), the reports of persistent pain in back or legs/feet were few. This indicates that it is acceptable to replace sitting with standing, as it does not result in side-effects in terms of increased pain experience.
Participants had different kind of office work in different office settings, including both small and large offices, private and public sector. Like in previous studies on workers, musculoskeletal pain was prevalent and it is thus expected that the findings from the present study could be generalized to offices in other setting.
Concluding remarks
The present paper reports results of secondary analyses of the cluster RCT Take a Stand! which was effective in reducing sitting time at work among office workers. Our analysis showed that the intervention did not reduce musculoskeletal pain in neck-shoulders after one month, but a reduction was found after three months. No changes were seen for pain in back and extremities, but a slight reduction was seen in total pain score. This is relevant as musculoskeletal pain is very prevalent and costly in office workers. In future intervention studies on sitting time, it is relevant to include a measure of musculoskeletal pain in order to investigate the long-term effects on musculoskeletal pain and whether this affects sick leave and productivity. Additionally, future studies should be designed to explore the causal pathways between intervention components, changes in sitting, and musculoskeletal pain.