Musculoskeletal disorders represent a considerable human and economic burden; lower back and neck pain were the leading global cause of disability in most countries in 2015 (1). In Quebec (QC), Canada, in 2007–2008, one in five workers reported disabling work-related musculoskeletal symptoms and 7% had a work absence due to such symptoms (2). In Canada, in 2012, costs of compensated work injuries and illnesses exceeded CAN$11 billion (3). Despite considerable underreporting of work-related musculoskeletal disorders (WMSD) to workers’ compensation (4), WMSD account for 33–43% of these compensation cases (5–7). WMSD refer to non-traumatic inflammatory or degenerative disorders of the musculoskeletal structures of the neck, back, upper or lower extremities that develop over time, as a result of cumulative micro-trauma from biomechanical or other work exposures, arising when the adaptive and repair capacities of affected structures have been exceeded (8). Several systematic reviews of longitudinal etiologic studies have shown that, in addition to biomechanical exposures and personal factors, psychosocial and organizational work factors, such as high work demands, low decision latitude, low coworker or supervisor support or an effort–reward imbalance, also contribute to the onset of WMSD (8–13). This may occur through stress-induced increases in muscle tension (14), increased serum cortisol levels and changes in soft tissues, alterations in inflammatory and immune responses, tissue hypoxia, and delayed wound healing (15, 16). Various organizational or psychosocial factors may also contribute to WMSD indirectly by influencing the intensity or duration of biomechanical exposures. Stock et al (17) have proposed a model of the complex relations between biomechanical, psychosocial and personal risk factors and psychological distress in the genesis of musculoskeletal disorders.
Despite their role in WMSD development, organizational and psychosocial work factors are not well integrated into WMSD prevention programs (18, 19). This contrasts with the consideration that is given to biomechanical determinants (eg, repetition, force, awkward postures, vibration). Work organization refers to the way in which work is designed and performed. It includes the distribution of work tasks, production methods, work pace, management, scheduling, remuneration, and training practices and policies (20, 21). The psychosocial work environment is the product of an interplay between the working conditions, including cognitive, social and emotional work demands, and the perceptions of these conditions by the worker (eg, intensity of work demands, decision latitude, support from coworkers or supervisors, recognition of worker efforts, emotionally demanding work, cognitive demands, workplace sexual and other harassment) (22, 23). In this review, we include the full range of such factors when we refer to “organizational and psychosocial factors”.
Little evidence regarding the effectiveness of work organizational or psychosocial interventions to prevent WMSD is available to guide prevention efforts. Bongers et al concluded that “few randomized or non randomized controlled trials have been carried out to evaluate the effectiveness of interventions to improve work-related psychosocial factors. Very few have reported on the preventive effect for work-related neck and upper limb symptoms”. (13, p296) Driessen et al (24) concluded on the lack of randomized controlled trials (RCT) on organizational interventions to reduce low back and neck pain. There are few reviews on this topic, and these did not apply a systematic review methodology (13), grouped in their synthesis interventions both with and without an organizational/psychosocial component (eg, workstation adjustments only) (13, 24) or were restricted to specific groups of workers (eg, shift workers) (25). It is also useful to review more recent intervention studies published since these previous reviews.
Our goal was to review the contemporary occupational intervention literature systematically in order to answer the following research question: compared to usual work activity (ie, no intervention), are workplace interventions that target work organization or the psychosocial work environment effective in preventing the onset of or reducing the incidence, prevalence or intensity of work-related musculoskeletal pain or of musculoskeletal disorders of the back, neck, shoulders, or distal upper limbs, or incidence, prevalence or duration of work absence/disability due to such pain or disorders among non-sick-listed workers? We hypothesized that interventions that target work organization or the psychosocial work environment, by mitigating harmful workplace exposures known to contribute to WMSD, should prevent or reduce adverse musculoskeletal health outcomes. In our definition of workplace interventions to prevent or reduce WMSD, we include those that seek to reduce biomechanical exposures through changes in work organization and those that specifically seek to reduce work organizational or psychosocial exposures.
We also hypothesized that interventions would be more effective in reducing WMSD if they included key elements of the intervention process identified by St-Vincent et al (26, 27). These authors have proposed a model for workplace interventions that describes the approach to be taken by the intervention team, guided by an ergonomist, to produce desired changes, including needs identification, work activity analysis, identification of risk factors and their determinants, identification and implementation of solutions with workplace stakeholders and their follow-up. This model is based on broad ergonomic principles and practices developed in Quebec, Canada, and France (28, 29) that has influenced ergonomic practice and professional training in these jurisdictions. At the heart of this approach is the concept of work activity and the differences between prescribed and real work (30). This activity-oriented approach places importance on the inter- and intra-individual variability in work activity. Through observations and interactions with the workers, the ergonomist seeks to understand how the worker constructs their work activity to attain work goals given available resources and constraints. Work activity analysis is more complex and multidimensional than “job analysis” or “task analysis” referred to by ergonomists or researchers in other countries, taking into account physical, psychological, cognitive and social dimensions of work as well as identifying the larger economic, social and organizational context that influences it. Although guided by the ergonomist, the process is done in a highly participatory fashion in collaboration with workers, managers and other key actors in the workplace who also participate in the identification of solutions and their implementation (28).
Our research team identified 12 key elements of workplace intervention described in the St-Vincent et al model (26, 27). The effectiveness of the St-Vincent et al intervention model on preventing or reducing WMSD has not been evaluated in rigorous epidemiological studies; therefore, we did not use the 12 key elements of workplace intervention in assessing the methodologic quality of studies or in evidence synthesis. However, looking at whether interventions included or lacked these intervention process elements may be useful in understanding some of the possible reasons of intervention effectiveness or ineffectiveness, and this aspect of the analysis was therefore part of results interpretation.
Methods
A systematic review methodology was used to address the research question using methods to reduce bias in gathering, summarizing, and reporting research evidence, following approaches outlined by the Centre for Reviews and Dissemination (31), with its chapter 3 focus on public health interventions, and The Cochrane Collaboration (32). The research team included practitioners and knowledge users, as well as researchers with content and methodologic expertise. Members of the team were consulted and/or participated in each step of the review process. This systematic review was not registered.
Search strategy
We searched for English- and French-language peer-reviewed scientific articles published between 2000–2015 in 11 electronic databases: Medline (2000–October week 3 2015) & Medline In-Process & Other Non-Indexed Citations (2000–December 11 2015), Excerpta Medica Database (EMBASE, 2000–October 15 2015), EBM Reviews/Cochrane Library (Cochrane Central Register of Controlled Trials 2000–September 2015, Health Technology Assessment 2000–3rd Quarter 2015, NHS Economic Evaluation Database 2000–2nd quarter 2015, ACP Journal Club 2000–September 2015, Cochrane Methodology Register 2000–3rd quarter 2012, Cochrane Database of Systematic Reviews 2005–November 2015, Database of Abstracts of Reviews of Effects 2000–2nd quarter 2015), Cumulative Index to Nursing & Allied Health Literature (CINAHL), PsycINFO, Psychology & Behavioral Sciences Collection, SocINDEX and Ergonomic Abstracts (all five databases 2000–December 31 2015), CISILO, INRS-Bibliographie and HSELINE (all three databases 2000–December 2015). In addition, we manually searched the reference lists of reviews identified through the bibliographic database search and of primary studies meeting the selection criteria below, and consulted content experts in identifying other potentially relevant studies.
The search combined terms using Boolean logic from four broad concepts: “Psychosocial or organizational interventions”, “Evaluation of effectiveness”, “Musculoskeletal disorders” and “Workplace”. Terms from a fifth concept relating to “Review” were added to the search strategy to identify existing literature reviews. The search strategy and syntax for each database was developed in collaboration with a librarian with expertise in bibliographic searches in occupational health. A detailed example of a search strategy is provided in supplementary table S1 (www.sjweh.fi/show_abstract.php?abstract_id=3696).
Inclusion and exclusion criteria
Two reviewers independently screened titles and abstracts for relevance, and resolved disagreements through consensus. The full paper of those meeting initial selection criteria was retrieved; the same two reviewers confirmed the relevance of all studies upon reading them in full, and discussed points of disagreement to arrive at consensus. We included studies that met the following criteria: they reported on an intervention in the workplace to prevent or reduce WMSD among active, non-sick-listed workers that included a work organizational component or targeted organizational or psychosocial exposures, evaluated the effectiveness of the intervention, and assessed a musculoskeletal health outcome (incidence, prevalence or intensity of work-related musculoskeletal pain or specific disorders in the neck, shoulders, upper limbs and/or back or incidence, prevalence or duration of work absence/work disability due to such pain or disorders). We did not restrict selection by research design. Applying RCT designs to complex workplace-based interventions may often not be possible; moreover ensuring appropriate control groups who undergo similar co-interventions and changes in contextual factors throughout trials that last many months and only differ with respect to the intervention studied is also a major methodologic challenge even when randomized designs are implemented (33, 34). Nonetheless limitations in study design were very much taken into account in the assessment of methodologic quality and evidence synthesis. We excluded interventions that recruited WMSD-disabled workers for rehabilitation or return-to-work interventions. We also excluded individual-level and behavioral interventions consisting solely of worker training/education, or behavioral strategies to reduce anxiety or psychological distress or to improve worker fitness through measures such as relaxation techniques or physical exercise. Studies in which more than half of the participants were lost to follow-up were also excluded, as we considered that such a high level of attrition would seriously compromise the validity of the conclusions on effectiveness of the intervention.
Methodologic quality appraisal of individual studies
Studies that met our selection criteria were assessed for bias according to 15 methodologic quality criteria developed by the research team and, in part, adapted from Rivilis et al (35) and Brewer et al (36). These criteria are listed in table 1; they address various sources of bias, including study design, selection and attrition bias, measurement bias and bias from confounding factors, co-interventions and contextual factors. Each criterion was rated 0, 1, or 2 points, for a maximum total score of 30 points. All reviewers participated in discussions on interpretation and clarification of these ratings to promote inter-rater reliability. The higher the score, the lower the risk of bias, and the higher the quality of the study. All studies were independently rated by two reviewers; disagreements were resolved through consensus or, if consensus was not reached, by consulting a third reviewer. Inter-rater agreement was not calculated. Scores were converted to percentages, and studies grouped into low (0–50%), medium (51–79%), and high (80–100%) quality categories. A low-quality rating reflects important methodological limitations, such that any reported musculoskeletal benefits could be attributable to factors unrelated to the intervention. Therefore, only medium- and high-quality studies were retained for data extraction and analysis.
Table 1
Methodologic quality criteria and method of scoring each criterion
Data extraction & analysis
For each medium- and high-quality study, we extracted information from the primary studies and companion papers by the same authors of the same study, on authors, year of publication, country of research, study population, study design, response rate at recruitment and loss to follow-up rate, intervention, types of changes, duration of intervention and timing of follow-up, compliance and/or degree of implementation of changes, measures of work exposures and/or musculoskeletal health outcomes, measurement of confounding factors, co-interventions and contextual factors and how or whether they were taken into account, statistical analysis, and effect of the intervention on work exposures and/or musculoskeletal health outcomes.
We also documented the presence or absence of the 12 key elements of the St-Vincent et al (26, 27) workplace intervention model.
The information extracted by one author in a standardized data extraction form was confirmed by a second author, and analyzed. In order to ensure meaningful conclusions about effectiveness, interventions were grouped into four categories according to similarities in the actions taken to develop and/or implement changes. We report change in the musculoskeletal indicator from baseline to final follow-up in the intervention versus control group/condition, for each musculoskeletal outcome within a study (there could be more than one). If a study reported measurements at the 6- and 12-month follow-up, we retained only the latter. Because of heterogeneity in outcome measures within intervention categories, or because necessary data was missing, it was not possible to pool results for meta-analysis.
Evidence synthesis
For each intervention category, we synthesized the evidence of effectiveness of the intervention for each musculoskeletal outcome of interest measured in the studies. The quality of the evidence was rated as high, moderate, low, or very low using the Grading of Recommendations Assessment, Development & Evaluation (GRADE) approach (37–43). These ratings reflect our confidence in effect estimates and the level of certainty that they are close to the true intervention effect on the musculoskeletal outcome. For example, a high-quality rating indicates that we are very confident that the true effect lies close to the estimate of the effect; while a low-quality rating indicates that the true effect may be substantially different from the estimate of the effect (44). Evidence based on randomized trials starts as initially high-quality evidence in GRADE, but can be rated down by one or two levels for risk of bias (methodologic limitations), inconsistency (inconsistent results with respect to direction of results or relative effect size across studies), indirectness (lack of generalizability of results with respect to the population, the intervention or the outcomes), imprecision (with respect to the confidence intervals of the difference in effect between the intervention and the control for each outcome) and/or risk of publication bias (37–40). Evidence from observational studies is initially rated as low-quality evidence, but in the absence of any serious limitations, can be rated up, if for example, the body of evidence presents very large effects or marked dose-response relationships (42). As recommended by Guyatt et al (45) and Balshem et al (44), we made an overall assessment of quality of the evidence based on the five GRADE criteria, identifying which criterion most influenced the assessment and which others contributed to the assessment, rather than systematically deduct one point for each criterion that was not met. When published findings were negative (ie, an intervention was ineffective), we considered the risk of publication bias to be low.
Reporting of results
We followed PRISMA guidelines for the reporting of systematic review results (46).
Results
Literature search
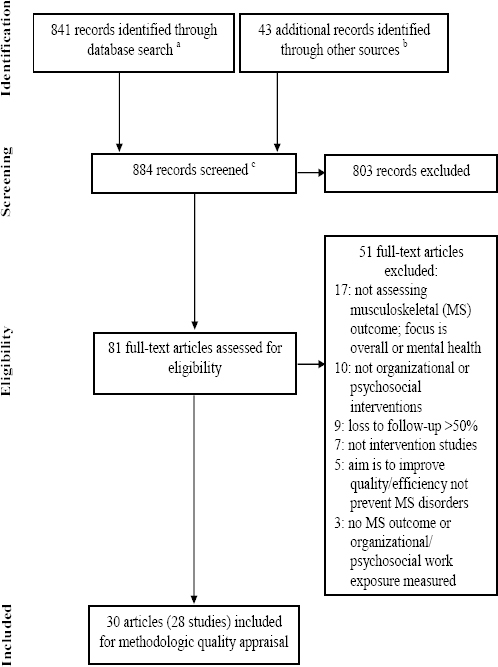
Figure 1 presents detailed results of each phase of the search and reasons for excluding studies. The search identified 884 records. After eliminating studies that did not meet the selection criteria, 28 studies were included for methodologic quality assessment. When two papers reported on the same intervention, they were analyzed as one study, as was the case for Haukka et al (47, 48), Driessen et al (49, 50) and the papers by Ronald et al (51) and Chhokar et al (52). One article by Faucett et al (53) reported two distinct studies, and these were analyzed separately.
Figure 1
PRISMA flow diagram detailing the results of the search. a Number of records identified in individual databases (N=841):
Medline: 94. Medline In-Process & Other Non-Indexed Citations: 6
EMBASE: 89. EBM Reviews-Cochrane Central Register of Controlled Trials (CCTR): 36. EBM Reviews-Health Technology Assessment (HTA): 1
EBM Reviews-NHS Economic Evaluation Database (NHSEED): 0. EBM Reviews-ACP Journal Club: 0. EBM Reviews-Cochrane Methodology Register (CMR): 0. EBM Reviews-Cochrane Database of Systematic Reviews (DSR): 0. EBM Reviews-Database of Abstracts of Reviews of Effects (DARE): 0. CINAHL: 312. PsycINFO: 259. Psychology & Behavioral Sciences Collection: 5. SocINDEX: 4. Ergonomic Abstracts: 30
CISILO: 0. INRS-Bibliographie: 1. HSELINE: 3
b Additional records were identified in the bibliographies of primary studies or reviews. Expert consulting did not yield new records.
c The number of duplicate records is unknown, as the web interface used to probe some of the databases automatically eliminates duplicates during the search.
Methodologic quality appraisal
Results of the methodologic quality appraisal of studies are presented in the last column of table 2. The detailed assessment for each of the 15 methodologic quality criteria is in supplementary table S2 (www.sjweh.fi/show_abstract.php?abstract_id=3696). Two studies were assessed as high-quality, 10 as medium-quality and 16 as low-quality studies. Only 11 of the 12 high- and medium-quality studies were retained for evidence synthesis. A study targeting the work-rest cycle by shortening workweek hours (54) was excluded from further analysis and evidence synthesis because an important proportion of subjects were part-time workers (55%) with an already shortened workweek, and therefore the capacity of the study to measure the effects of work hour reduction was judged to be considerably compromised.
Table 2
Description of the 11 medium and high-quality studies included in evidence synthesis. [ANOVA=analysis of variance; ANCOVA=analysis of covariance; C=control; CI=confidence interval; DASH=disabilities of the arm, shoulder and hand; H=high; I=intervention; M=medium; MSK=musculoskeletal; NS=not significant; RCT=randomized controlled trial; SD=standard deviation; VAS=visual analog scale.]
| Study | Participants analyzed (% men or women at baseline) | Study design | Intervention & types of changes | Control group / condition | Duration of intervention & timing of follow-up measurement | MSK outcome | MSK outcome in intervention vs. control groups/conditions (negative signs indicate worsening) | Method-ologic quality rating |
|---|---|---|---|---|---|---|---|---|
| Interventions targeting the work-rest cycle through supplementary pauses | ||||||||
| Faucett et al, 2007 (study 1) (53) (USA) | 66 strawberry harvesters, C=36, I=30 (79% men) | RCT | Addition of four 5-min rest breaks in each hour without a scheduled break (total addition of 20 min/day), during which worker could stand, stretch, walk or sit | Workers in same strawberry site on conventional break schedule (10-min break after 4 hrs of work, 30-min lunch break after 4 hrs of work) | 2 days (preceded by a baseline day); measurement at end of each workday | Composite measure of pain severity measured at end of each workday based on sum of body regions with symptoms multiplied by severity of symptoms; scores for 3 types of symptoms were summed |
Change in pain score at end of work day from baseline to day 2, I vs. C: [2.30 (SD 2.62) – 1.03 (SD 2.14)] vs. [1.72 (SD 4.50)
– 2.01 (SD 3.56)] = 1.27 vs. -0.29 NS with repeated measures ANOVA (low statistical power) Significant difference in the number of workers whose pain score: worsened: I: 4 vs C: 14 did not change: I: 12 vs C: 16 improved: I: 14 vs C: 6 P=0.01 for Pearson χ2 |
H: 87% |
| Faucett et al, 2007 (study 2) (53) (USA) | 32 tree nursery workers (16 pairs) (72% women) | RCT, cross-over design (paired data) | Same as Faucett et al, 2007 (study 1) | Workers served as own controls, randomly ordered to supplementary or conventional break schedule in alternation | 6 days: baseline day, then 3 days under each break schedule separated by week-end wash-out period | Same as Faucett et al, 2007 (study 1) |
Change in pain score at end of work day from baseline to day 3, I vs. C: Group 1: [10.5 (SD 12.2) – 8.2 (SD 11.4)] vs. [10.5 (SD 12.2) – 17.0 (SD 10.2)] = 2.3 vs. -6.5 Group 2: [9.4 (SD 13.4) – 5.1 (6.0)] vs. [9.4 (SD 13.4) – 18.7 (SD 11.9)] = 4.3 vs. -9.3 P≤0.01 for ANCOVA controlling for group & productivity |
H: 87% |
| Galinsky et al, 2007 (55) (USA) | 51 seasonal data entry workers (92% women) | RCT, cross-over design (paired data) | Additional 5-min break/hr for each hr not containing a break (total addition of 20 min/day), during which participants encouraged to walk away from workstation. Participants randomly assigned to a stretching or no stretching exercise condition, and within each, they were randomly assigned to conventional or supplementary break schedule in alternation | Workers served as their own controls, alternating between supplementary & conventional break schedule (two 15-min breaks & 30-min lunch break) | 8 weeks: 4 weeks under each break schedule, in alternation; measurement daily, 4 times/day: before shift, before lunch, after lunch, after shift | MSK discomfort level (5-point response scale), based on Feeling State Questionnaire for neck, right (R) and left (L) shoulder/upper arm, R and L forearm/wrist/hand, back, buttocks, and legs |
Mean discomfort levela over 4 weeks, I vs. C : Neck: 1.45 vs. 1.55, P<0.03 Back: 1.50 vs. 1.65, P<0.003 R shoulder/upper arm: 1.40 vs. 1.50, P<0.003 R forearm/wrist/hand: 1.35 vs. 1.45, P<0.02 L shoulder/upper arm: 1.15 vs. 1.25, P<0.03 L forearm/wrist/hand: 1.05 vs. 1.15, P< 0.03 Mixed design multivariate analysis of variance; Significant attenuation of increasing discomfort during each half of the workday for all of the above body regions, except for R forearm/wrist/hand; no effect of stretching condition on outcome |
M: 73% |
| McLean et al, 2001 (56)(Canada) | 15 computer workers from university and government offices (100% women) | RCT, cross-over design (paired data) | 30-second micro-breaks according to 3 protocols: at discretion (C), every 20 min (I1), every 40 min (I2); participants prompted to get out of chair and walk away from workstation during micro-breaks | Workers served as own controls, undergoing a no break protocol, then randomly assigned to one of the 3 micro-break protocols | 2 weeks of a no break protocol, then 2 weeks of micro-break protocol, with measurements on last 2 days of each protocol | MSK discomfort level (vertical VAS, 0–100 mm) for neck, low back/buttock, shoulder/upper arm, forearm/wrist/hand |
Difference in VAS score (mm) after 3-hr work session under a micro-break protocol compared to no break protocol, I1 vs. I2
vs. C: Neck: 28 vs. 33 vs. 38 Back: 42 vs. 24 vs. 24 Shoulder/upper arm: 32 vs. 22 vs. 24 Forearm/wrist/hand: 28 vs. 7 vs. 19 All 3 protocols equally and significantly reduced discomfort in the neck, but I1 was the most effective for the other 3 body regions (ANOVA) |
M: 70% |
| Participatory ergonomic (PE) interventions based on training groups of workers to analyze work, identify problems and propose solutions | ||||||||
| Driessen et al, 2011 (50, 62) (The Nether-lands) | 3047 blue & white collar workers from 4 large companies (railway, airline, steel, university & university hospital) C=582, I=588 (57–59% men) | Cluster RCT (unpaired data) | Stay@Work PE program: worksite evaluation by ergonomist who trained (6 hrs) group of 8 workers, department manager & occupational health & safety coordinator in risk identification & solution implementation. 2-3 implementers/group had additional 4-hr implementation training. Working groups prioritized 32 individual ergonomic awareness measures, 27 physical (eg, new equipment) & 7 organizational ergonomic measures (eg, pause software installation, job rotation, restructuring management style) | Workers from departments with comparable workload who watched 3 short films as a sham intervention | 3 months to implement changes 1 month following training; follow-up at 6 months for work exposures and 12 months for MSK outcome | Prevalence of frequent low back & neck pain in past 3 months Mean pain intensity past 3 months (11-point Von Korff scales) Number of days with pain past 3 months All from Dutch MSK Questionnaire |
No change in low back & neck pain prevalence baseline to 12 months (raw data at follow-up not provided, only odds ratios)
Change in mean pain intensity from baseline to 12 months, I vs. C: Neck: [1.7 (SD 2.2) – 1.4c] vs. [1.7 (SD 2.1) – 1.2 c] = 0.3 vs. 0.5 Low back: [2.2 (SD 2.4) – 1.7c] vs. [2.1 (SD 2.3) – 1.5c] = 0.5 vs. 0.6 NS with linear mixed modeling Change in number of days with pain baseline to 12 months, I vs. C: neck: [9.7 (SD 19.8) – 8.0c] vs. [8.9 (SD 18.6) – 7.0c] = 1.7 vs. 1.9 Low back: [12.0 (SD 21.7) – 9.0c] vs. [11.5 (SD 21.0) – 7.0c] = 3.0 vs. 4.5 NS with linear mixed modeling |
M: 70% |
| Haukka et al, 2008; 2010 (47,48)(Finland) | 504 workers in municipal kitchens in several cities, C=241, I=263 (96–98% women) | Cluster RCT (unpaired data + cohort analysis on 307 subjects in same kitchens in study) | PE intervention: two 1-day workshops of worker training to identify problems & possible solutions to decrease physical & mental workload and six 3-hr workshops to implement solutions in collaboration with management & technical staff. 41% of changes were in work organization, methods & practices, 27% in machines, equipment & tools | Workers in different city district but similar type of kitchen continuing normal kitchen activity | 11 - 14 months; follow-up every 3 months for 1 year post-intervention | Prevalence of MSK pain past 3 months for neck, shoulders, forearms/hands, low back, hips, knees, ankles/feet Mean score of trouble caused by any MSK pain past 3 months (7-point scale) Prevalence of MSK sick leave during past 3 months |
Change in pain prevalenced from baseline to 1-year post-intervention, I vs. C: Neck: (67 – 72) vs. (72 – 68) = -5 vs. 4 Shoulders: (32 – 42) vs. (38 – 42) = -10 vs. -4 Forearms/hands: (48 – 58) vs. (50 – 57) = -10 vs. -7 Low back: (48 – 52) vs. (50 – 54) = -4 vs. -4 Change in mean score of trouble caused by any MSK pain from baseline to 1-year post-intervention, I vs. C: (2.0 – 2.1) vs. (2.1 – 2.1) = -0.1 vs. 0.0 Change in prevalence of MSK sick leave (%) from baseline to 1-year post-intervention, I vs. C: (17 – 20) vs. (19 – 16) = -3 vs. -3 All changes NS with mixed logistic regression modelling adjusting for baseline level of MSK outcome, age, gender, job satisfaction, smoking, exercise, body mass index & permanent/fixed-term employment. Similar results with cohort analysis on 307 workers. |
M: 70% |
| Laing et al, 2007; 2005 (57,63) (Canada) | 66 workers in automotive foam parts manufacturing company, C=45, I=21 (80% men) | Non randomized controlled trial (paired data) | PE program with worker-manager ergonomics change teams (ECT) responsible for identifying problems & developing & implementing intervention projects. ECT received 3-day training, 3 weekly 6-hr training sessions & more advanced ‘tutorials’ as necessary. 10 physical ergonomics change projects completed (eg, anti-fatigue mat); 9 workplace “psychosocial interventions” aimed at communicating the ergonomics program to workplace stakeholders (eg, newsletter, suggestion box to solicit opinions about ergonomic issues & solutions, logo contest) | Nearby plant of same company with same product line, union & corporate policies, similar numbers of workers as I plant. Important labour relations & other contextual factor differences between I & C plants | 11 months (1 month training, 10 months intervention); follow-up 1 month after end of intervention | Mean pain severity past 3 months (mean of average pain & worst pain, 5-point scale) for shoulder/ upper arm, forearm/ hand, back & leg/lower limb |
Change in mean pain severity baseline to 12 months post-intervention, I vs. C: Shoulder/upper arm: [1.5 (SD 1.1) – 1.5 (SD 1.0)] vs. [1.8 (SD 0.7) – 1.7 (SD 1.0)] = 0.0 vs. 0.1 Forearm/hand: [0.9 (SD 1.0) – 1.3 (SD 1.1)] vs. [1.5 (SD 0.9) – 1.3 (SD 1.0)] = -0.4 vs. 0.2 Back: [1.9 (SD 1.1) – 1.8 SD (1.0)] vs. [2.0 (SD 1.0) – 1.6 (SD 0.9)] = 0.1 vs. 0.4 NS with two-factor repeated measures ANOVA testing for interaction between group (I or C) & time (pre- or post-intervention) |
M: 53% |
| Participatory organizational intervention targeting psychosocial work exposures | ||||||||
| Gilbert-Ouimet et al, 2011 (58)(Canada) | 1330 white-collar workers in a public insurance company (62% women) | Before-after uncontrolled study (unpaired data, repeated cross-sectional design) | Risk evaluation of psychosocial work factors through questionnaire, setting of intervention priorities with worker focus groups & presentation of solutions to managers, who decided on implementation. Changes included hiring additional staff, improved management practices & organizational restructuring aimed at grouping teams to facilitate use of expertise/promote synergy | No control group | 2 years; follow-up 6 & 30 months post-intervention | Prevalence of MSK pain/discomfort past 6 months & functional limitations at work, home or in leisure activities (modified Nordic MSK Questionnaire) for neck/shoulder, upper limbs & lower back |
Change in pain prevalence (%), from baseline to 30 months post-intervention: Neck/shoulder: 67.7 – 60.4 = 7.3, P<0.05 Upper limbs: data not provided Lower back: 58.0 – 52.0 = 6.0, P<0.05 Generalized estimating equations adjusting for age, gender, education if these confounders induced more than 10% change in effect estimates |
M: 57% |
| Interventions to reduce patient lifting in a hospital setting through safe lifting programs and equipment | ||||||||
| Caspi et al, 2013 (59)(USA) | 303 nurses & patient care aides (90% women) | Before-after uncontrolled pilot study (analysis on unpaired data) | Intervention to promote unit-level safety, social environment changes, and worker safety & wellness through unit safety audit, fitness promotion & safe patient handling training (1-hr unit manager training, 1.5-hr one-on-one safe patient handling training by nurse to each worker, 3 monthly bedside mentoring sessions with guidelines to strengthen worker collaboration in moving patients & use of patient handling equipment) | No control group | 3 months; follow-up completed between months 4–8 | Prevalence of pain past 3 months (adapted Nordic MSK Questionnaire) for lower back, neck/shoulder, forearm/wrist & lower extremities |
Change in pain prevalence (%) from baseline to follow-up: Any pain: 81.85 – 81.37 = 0.48 Neck/shoulder: 50.25 – 46.90 = 3.35 Forearm/wrist: 10.79 – 8.01 = 2.78 Lower back: 61.53 – 59.02 = 2.51 NS with repeated-measures linear model, adjusted for responding at both time points |
M: 53% |
| Yassi et al, 2001 (60)(Canada) | 346 nurses & unit assistants (gender not documented), C=103, I1=127, I2=116 | RCT (paired data) | Two interventions of varying intensity: “No-strenuous lift” program to eliminate manual patient handling (I1) & “Safe lifting” program to reduce manual patient handling (I2) through mechanical patient lift/transfer equipment and 3-hr education on back care, patient assessment, handling techniques & practice using equipment. The 2 programs differed with respect to nature & quantity of equipment purchased & made available to staff. | Workers from different hospital wards with similar type of patient, ward size, staffing & previous injury rates, who continued with usual practice, ie, training on request & only for regularly-used equipment | Duration not documented; follow-up 6 & 12 months after baseline | Frequency of work-related shoulder & low back pain past week (VAS, 0-100) Pain & disability score for back (Oswestry) & upper limb (DASH) Workers’ Compensation Board rate of MSK injuries & time loss injuries (per 100,000 paid hrs) (during study year, year prior to study & averaged over 3 years before study) |
Change in frequency of work-related pain from baseline to 12 months: Shoulder: I1 vs. C: [26.5 (SD 28.1) – 24.2 (SD 25.4)] vs. [20.2 (SD 24.2) – 24.1 (SD 26.5)] = 2.3 (SD 28.5) vs. -4.4 (SD 25.9) NS I2 vs. C: [35.9 (SD 29.7) – 27.1 (SD 24.9)] vs. [20.2 (SD 24.2) – 24.1 (SD 26.5)] = 6.6 (SD 27.3) vs. -4.4 (SD 25.9), P=0.009 Low back: I1 vs. C: [34.0 (SD 27.5) – 31.7 (SD 27.6)] vs. [28.5 (SD 27.1) – 30.2 (SD 29.4)] = 3.3 (SD 27.0) vs. -1.0 (SD 26.1) NS I2 vs. C: [37.3 (SD 27.7) – 29.8 (SD 24.2)] vs. [28.5 (SD 27.1) – 30.2 (SD 29.4)] = 6.5 (SD 27.6) vs. -1.0 (SD 26.1), P=0.041 Two-way repeated-measures ANOVA Change in DASH score, from baseline to 12 months: I1 vs. C: [6.6 (SD 10.0) – 5.5 (SD 8.7)] vs. [5.2 (SD 9.1) – 6.3 (SD 10.9)] = 1.1 vs. -1.1 I2 vs. C: [7.6 (SD 8.9) – 7.3 (SD 10.9)] vs. [5.2 (SD 9.1) – 6.3 (SD 10.9)] = 0.3 vs. -1.1 NS with three-way (group, ward, time) repeated-measures ANOVA Change in Oswestry score, from baseline to 12 months: I1 vs. C: [5.7 (SD 8.0) – 5.4 (SD 7.6)] vs. [5.4 (SD 9.0) – 6.4 (SD 10.6)] = 0.3 vs. -1.0 I2 vs. C: [7.2 (SD 8.8) – 6.7 (SD 8.7)] vs. [5.4 (SD 9.0) – 6.4 (SD 10.6)] = 0.5 vs. -0.1 NS with three-way (group, ward, time) repeated-measures ANOVA Change in injury rate, from previous year to study year: I1 vs. C: (8.2 – 6.1) vs. (5.6 – 7.6) = 2.1 vs. -2.0 I2 vs. C: (4.9 – 5.3) vs. (5.6 – 7.6) = -0.4 vs. -2.0 NS with Mantel Haenszel χ2 (low statistical power) Change in time loss injury rate, from previous year to study year: I1 vs. C: (3.5 – 1.5) vs. (1.7 – 2.7) = 2.0 vs. -1.0 I2 vs. C: (2.2 – 3.2) vs. (1.7 – 2.7) = -1.0 vs. -1.0 NS with Mantel Haenszel χ2 (low statistical power) |
M: 70% |
| Feedback about computer workstation set-up & psychosocial aspects of work | ||||||||
| Eklöf & Hagberg, 2006 (61)(Sweden) | 304 computer workers from 9 companies, eg, banking, transport, manufacturing C=75, I1=76, I2=77, I3=76 (67-88% women) | Cluster RCT (paired data) | Short feedback session by physiotherapist-ergonomist to individual workers (I1), supervisors (I2) or groups of workers & supervisors (I3) about optimal computer workstation layout, work technique & psychosocial aspects of work to reinforce motivation to make changes (eg, adjust chair/keyboard height, work postures, work pace or amount, influence over decisions, support from colleagues) | Workgroups in same organization who did not receive feedback. Non-optimal workstation layout or work technique not documented in C groups | Average duration: I1: 38 min I2: 61 min I3: 85 min; Follow-up 6 months after feedback | 1-month prevalence of MSK pain of more than 10 days of head, neck, shoulders, arms or hands |
Change in pain prevalence (% of workgroup members), from baseline to 6 months, I vs. C: I1: -9 vs. 0 I2: 0 vs. 0 I3: 0 vs.
0 NS for pairwise comparisons (I vs. C) using Mann-Whitney U-test conducted at the group level (n=9 groups/experimental condition) |
M: 73% |
[i] a Data estimated from Figure 1 of original study.
Description of interventions
Among the 11 medium- and high-quality studies, we found four types of interventions: (i) Four studies examined interventions targeting the work-rest cycle through five-minute supplementary pauses (53, 55) or through 30-second micropauses (56). (ii) Four studies were multi-component complex interventions that sought to identify musculoskeletal disorder risk factors and identify and implement solutions in a participatory process with workers and managers; three of these were participatory ergonomic (PE) interventions in which groups of workers were trained to analyze work demands, identify WMSD risk factors and propose and implement solutions to reduce the physical and psychosocial workload (47–50, 57); in the fourth study, researchers identified psychosocial work factor risks by questionnaire, followed by the setting of intervention priorities with worker focus groups, and presentation of solutions to managers, who decided on the implementation of proposed solutions (58). (iii) Two studies reported on interventions with an organizational component to reduce patient handling in a hospital setting through the adoption of safe patient handling policies or programs, worker training and access to patient lifting equipment (59, 60). (iv) Another study included three intervention arms providing feedback about computer workstation set-up and psychosocial aspects of work to promote worker motivation to make changes: feedback was provided to workers individually, to supervisors individually or to groups of workers and their supervisor (61).
A description of the 11 studies included for analysis and evidence synthesis is presented in table 2 and supplementary table S3 (www.sjweh.fi/show_abstract.php?abstract_id=3696).
Effectiveness of work-rest cycle interventions on musculoskeletal symptom intensity
Two RCT (53) provided moderate evidence that interventions targeting the work-rest cycle through supplementary pauses are more effective than conventional break schedules in reducing the intensity of symptoms, based on a composite measure that takes into account all body regions. This evidence was rated down by one level due to indirectness: the assessment of pain at the end of two or three days of work is an indirect measure of the risk of development of a musculoskeletal disorder or longer-term musculoskeletal pain.
Two RCT (55, 56) provided moderate evidence on the effectiveness of such interventions on musculoskeletal symptom intensity separately for the neck, back, shoulder/upper arm and forearm/wrist/hand outcomes (table 2). This evidence was rated down by one level due to the serious risk of bias from high attrition in one of the studies (55) (43% loss to follow-up, with no comparison of the characteristics of study completers and drops-outs) and failure to take in account any confounders in the other study (56).
Effectiveness of participatory ergonomic (PE) interventions on pain prevalence
There was low-quality evidence from two RCT (47, 48, 50, 62) that PE interventions that trained worker groups to analyze work and propose solutions are not more effective than work activity as usual in reducing the three-month prevalence of neck pain and low-back pain. We rated the quality of this evidence down by two levels because of very serious risk of bias related to attrition (>30% loss to follow-up in both studies), insensitivity to change of the musculoskeletal indicators, especially in light of the low baseline pain severity scores in the populations (these ranged from 1.7–2.2 on scales of 7 or 11, see table 2), the low implementation rate, and the presence of major co-interventions and changes in contextual factors (see supplementary table S3). For example, in one study (47, 48) there was an unplanned major organizational reform, whereby food preparation was no longer carried out in half the targeted workplaces but moved to large centralized production kitchens for distribution by other kitchens. This co-intervention drastically modified the nature of the work and working conditions in half the participating workplaces and resulted in a worsening of psychosocial work factors for workers who underwent the intervention and reform (eg, increased hurry at work, decreased supervisor support, see supplementary table S3).
Effectiveness of PE interventions on pain intensity
One RCT (50, 62) and one non-randomized trial (57, 63) provided low-quality evidence that PE interventions are not more effective than work activity as usual in reducing the intensity of back pain. We penalized this evidence by two levels for very serious risk of bias from attrition (>30% in both studies), the low implementation rate, and presence of co-interventions and changes in contextual factors (see supplementary table S3). The quality of the evidence was low with respect to the intensity of neck pain, based on one RCT (50, 62), very low for the intensity of shoulder/upper arm pain or forearm/hand pain, based on one non randomized trial (57, 63) and low for the intensity of any musculoskeletal trouble caused by pain, based on one RCT (47, 48). In all three cases, the evidence was penalized due to very serious risk of bias owing to attrition and the presence of important co-interventions and changes in contextual factors that influenced outcomes, and additionally for the first two cases, due to the low implementation rate.
Effectiveness of PE interventions on number of days with any pain
One RCT (50, 62) provided low-quality evidence that PE intervention is not more effective than usual practice in reducing the number of days with any musculoskeletal pain. We rated the quality of this evidence down by two levels due to very serious risk of bias associated with attrition, the low implementation rate and presence of important co-interventions & changes in contextual factors.
Effectiveness of PE interventions in reducing sick leave
One RCT (47, 48) provided low-quality evidence that PE intervention is not more effective than work as usual in reducing the three-month prevalence of musculoskeletal sick leave. The evidence was downgraded by two levels owing to very serious risk of bias due to attrition, presence of important co-interventions and changes in contextual factors.
Effectiveness of a participatory organizational intervention targeting psychosocial work exposures on prevalence of pain and functional limitations
One before–after uncontrolled study (58) provided very low-quality evidence that a participatory organizational intervention targeting psychosocial work exposures was more effective than work as usual in reducing the six-month prevalence of neck/shoulder and lower back pain with functional limitations. It provided very low-quality evidence that this type of intervention was not more effective than usual work in reducing the six-month prevalence of upper-limb pain with functional limitations. This observational evidence, which is initially low-quality, was penalized by one level due to the serious risk of bias from the presence of an ergonomic co-intervention put in place during the study that may have affected postural risk factors and lack of information about attrition (supplementary table S3).
Effectiveness of intervention to reduce patient handling on pain prevalence
The quality of the evidence was very low that a hospital-based program – promoting unit-level safety through a unit safety audit, safe patient handling training, and guidelines to strengthen worker collaboration in moving patients and improve access to and compliance with use of patient-handling equipment – is not more effective than usual practice in reducing the three-month prevalence of neck/shoulder pain, forearm/wrist pain, lower back pain and musculoskeletal pain in any body region. In all cases, the evidence was based on a single before–after uncontrolled study (59), thus initially low-quality evidence, and was rated down by one level for serious risk of bias from lack of any control group and use of an insensitive musculoskeletal outcome measure.
Effectiveness of safe-lifting program and of no-strenuous lift program on low-back and shoulder pain frequency
One RCT (60) provided low-quality evidence that a safe lifting program is more effective than usual practice in reducing the frequency of work-related shoulder pain and of work-related low back pain after 12-month follow-up (see table 2). The safe lifting program focused on reducing manual lifting through training on safe lifting and the use of equipment (one mechanical total body lift and two large and four small sliding devices available per ward, transfer belts in each room). The same RCT (60) provided low-quality evidence that a no-strenuous lift program is not more effective than usual practice in reducing the frequency of work-related shoulder and low back pain after 12-month follow-up (see table 2). The no-strenuous lift program focused on eliminating manual lifting by providing each ward access to multiple new mechanical total body lifts and sit-stand lifts, with sliding devices for each room. Compliance with the use of the mechanical devices was high at 6 months but declined by 12 months (see supplementary table S3). In both cases, the evidence was rated down by two levels for very serious risk of bias related to the lack of consideration of confounding factors, undocumented changes in contextual factors, and reduced compliance at 12 months.
Effectiveness of safe-lifting program and of no-strenuous-lift program on low-back and upper-extremity functional status
The same RCT provided low-quality evidence that neither the no-strenuous lift program nor the safe lifting program was more effective than usual practice in improving upper extremity or back-related functional status. For each of these outcomes, the evidence was rated down by two levels for very serious risk of bias related to the lack of consideration of confounding factors, undocumented changes in contextual factors and reduced compliance at 12 months.
Effectiveness of safe-lifting program and of no-strenuous-lift program on compensated work injury rate
Based on the same RCT as above (60), the quality of the evidence is low that safe-lifting and no-strenuous -lift programs are not more effective than usual practice in reducing compensated musculoskeletal work injury rates and time loss injury rates. This evidence was rated down by two levels for very serious risk of bias related to the lack of consideration of confounding factors, undocumented changes in contextual factors and reduced compliance at 12 months.
Because of the low to very-low quality evidence for these patient handling interventions, we cannot conclude on their effectiveness or ineffectiveness to prevent or reduce WMSD.
Effectiveness of feedback interventions about computer workstation and psychosocial work aspects on pain prevalence
One RCT (61) provided low-quality evidence that three computer work intervention arms – providing feedback on computer work set-up and psychosocial work conditions to (1) individual workers, (2) only to supervisors or (3) to a collective group of workers and their supervisor – are not more effective than no feedback (work as usual) in reducing the one-month prevalence of any musculoskeletal pain. We penalized the evidence by two levels for very serious risk of bias due to possible contamination of control groups, lack of documentation of changes in contextual factors, lack of sensitivity to change of the musculoskeletal indicator and inclusion in analyses of subjects who were absent for the intervention.
Presence of key workplace intervention elements
Table 3 summarizes our evaluation of the presence of 12 key workplace intervention elements in the 11 retained studies.
Table 3
Evaluation of the presence of 12 key elements of workplace intervention. [ND=not documented.]
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | Intervention objective is to reduce harmful work exposures | Analysis of needs & workplace actors’ viewpoints / expectations | Company context considered throughout intervention a | Particip-atory b process to select work situations to be analyzed | Work activity analysis by ergon-omist | Interviews with concerned workplace parties | Observ-ations of real work situations | Validation of ergonomist observations with workers & managers | Consensus on risk factors & their determinants | Identif-ication of changes to be implemented | Particip-atory b implem-entation | Implementation guided by ergonmist / intervention specialist |
| Faucett et al, 2007 (study 1) (53) | Yes | ND | Yes | ND | No | No | ND | ND | ND | Yes | Yes | No |
| Faucett et al, 2007 (study 2) (53) | Yes | ND | Yes | ND | No | No | ND | ND | ND | Yes | Yes | No |
| Galinsky et al, 2007 (55) | Yes | No | No | No | No | No | No | No | No | Yes | ND | No |
| McLean et al, 2001 (56) | Yes | No | No | No | No | No | No | No | No | Yes | No | No |
| Driessen et al, 2011 (50, 62) | Yes | No | No | Yes | No | No | Yes | Yes | No | Yes | Yes | No |
| Haukka et al, 2008; 2010 (47, 48) | Yes | ND | No | Yes | No | No | Yes | ND | Yes | Yes | Yes | No |
| Laing et al, 2005; 2007 (57, 63) | Yes | ND | ND | Yes | No | ND | Yes | ND | ND | Yes | Yes | Yes |
| Caspi et al, 2013 (59) | Yes | ND | No | No | No | No | No | No | Yes | Yes | Yes | No |
| Yassi et al, 2001 (60) | Yes | No | No | No | No | No | No | No | No | Yes | No | No |
| Gilbert-Ouimet et al, 2011 (58) | Yes | No | No | No | No | Yes | No | Yes | Yes | Yes | Yes | No |
| Eklöf & Hagberg, 2006 (61) | Yes | No | No | No | No | No | Yes | No | No | Yes | No | No |
a Social, organizational and economic contextual factors of the company that may influence the intervention must be taken into account throughout the intervention process, so that the intervention can be adapted should any co-interventions or relevant changes in contextual factors arise, or at the very least, so that these may be taken into account during analysis or results interpretation.
Overall, all intervention studies sought to mitigate exposure to workplace risk factors (key element 1), all identified the changes that were to be implemented or gave examples of these (key element 10), and most of the studies had workers participate in the selection and implementation of changes (key element 11). However, few interventions included or documented a needs analysis and stakeholder viewpoints (element 2), or took into account the social, economic and organizational context of the company (key element 3). An exception is the study by Faucett et al (53). Here, authors considered the cultural, linguistic and low literacy characteristics of their agricultural workers when developing their musculoskeletal symptom questionnaire (64). They also documented the fact that work was fast paced because of the need to preserve fragile commodities and that there was an incentive piece rate pay system, which could cause workers to skip breaks. Therefore, they chose to signal the rest break with a whistle, and asked farm workers to stop their work.
Only the three PE interventions included and documented key element 4 (participatory selection of work situations to be analyzed). For example, in Haukka et al (47, 48), each kitchen selected two or three work tasks that the workers considered physically demanding. In Driessen et al (50, 62), there was an inventory of the workplace, during which each worker of the working group took pictures of risk factors for low back and neck pain at the worksite that were to be discussed at a subsequent group meeting and prioritized based on consensus.
Most notably, none of the studies carried out in-depth work activity analysis (elements 5 to 9). Most of these elements were lacking or inadequate in most studies including all three PE interventions. For example, an ergonomist conducted a worksite observation through checklist in Driessen et al (50, 62) (key element 7), and sent a summary of the observations to the working group (key element 8). But there was no in-depth analysis of work activity or interviews with workers (key elements 5 and 6), and the ergonomist appears not to have participated in the consensus reached by the working group on the work demands and their determinants to be targeted for intervention (key element 9).
Finally, in most studies, there was either no or little guidance during the implementation of change projects (key element 12), the role of the ergonomist or intervention specialist being limited to monthly check-ins (59), a single visit to each worksite and a phone call (47, 48) or follow-up only at the end of the study to collect data (61). In other instances, implementation was solely the responsibility of the workplace (58) or of workers within ergonomic change teams called “implementers” (50, 62).
Discussion
We found moderate evidence that supplementary breaks are more effective than a conventional break schedule in reducing the intensity of symptoms in the neck, shoulder, upper limbs and back or a combination of these. It is noteworthy that supplementary breaks did not negatively impact productivity (see supplementary table S3), and were effective across varied settings (agricultural versus office workers) and intervention characteristics (5-minute versus 30-second pauses), arguing for the potential generalizability of this result. Interestingly, the workers studied for this category of interventions were primarily in precarious work (immigrant agricultural workers, short-term contract office workers) hired to do highly repetitive work, groups thought to be at high risk of WMSD, and in need of more research attention. Further research will need to study whether such rest breaks are effective in other work settings, for example in manufacturing, food processing or assembly work, and what contextual factors influence effectiveness.
The evidence was of low to very low quality for the effectiveness or ineffectiveness of other interventions, many of which suffered from risk of bias related to high attrition rates, confounding factors, co-interventions, and insensitivity to change of outcome measures. Hence, no conclusions or recommendations can be made on the basis of these other studies.
Comparison of findings to other reviews
The effectiveness of added rest breaks was evaluated by three previous reviews, but they were based on studies slightly different from those evaluated by us. Bongers et al (13) found inconclusive evidence on the effectiveness of added rest breaks for preventing neck and upper limb problems. We rated two of their nine studies low-quality and therefore they were not included in our evidence synthesis (65, 66). Several of their other studies did not meet our selection criteria, either because loss to follow-up was >50% (67) or the publication date was outside the scope of our review. Brewer et al (36) concluded on mixed evidence (inconsistent findings) for the effectiveness of rest breaks among office workers. The only study in common with our review was that of McLean et al (56). The authors’ three other studies either did not meet our selection criteria or were published before the period covered in this review. In their meta-analysis and synthesis using GRADE, Hoe et al (68) concluded on low-quality evidence that supplementary breaks produced no difference compared to conventional breaks in end-of-shift discomfort ratings. Their conclusion was based on two studies by Galinsky and colleagues (55, 67), one of which we had excluded because of the high attrition rate (67). They did not include the McLean study in their meta-analysis as no measure of variance was reported or could be imputed from the study. In addition, we based our synthesis on the mean change in discomfort from baseline to four weeks follow-up rather than end-of-shift discomfort.
In a systematic review of the effectiveness of PE interventions (not limited to those targeting work organization or psychosocial work factors), Rivilis et al (35) concluded there was partial-to-moderate evidence of a positive impact on various musculoskeletal outcomes based on 12 studies. None of those studies overlapped with the studies reviewed herein (7 published prior to 2000).
We concluded on low- to very low-quality evidence for the effectiveness or ineffectiveness of patient handling interventions. A systematic review of 1980–2009 WMSD prevention interventions in healthcare settings (69) found moderate evidence for the effectiveness of interventions comprised of the following three components: (i) an organizational policy, (ii) lift or transfer equipment purchases, and (iii) ergonomics training in safe-patient handling and/or equipment use. Training alone was found to be ineffective (69). The Yassi et al intervention (60) was the only study appearing in the evidence synthesis of both the present review and that of Tullar et al (69). We excluded two of the other studies that the authors included in their synthesis because of the high attrition rates (70, 71). Five other studies that were common to both reviews were deemed to be of insufficient methodologic quality and were not used in the synthesis of either review (51, 52, 72–74).
In addition to differences in the studies evaluated and in the approaches to evidence synthesis, other review authors looking at some of the same studies reviewed here proceeded with different classifications. For example, while we classified the intervention by Haukka et al (47, 48) with other PE interventions, it was classified with “physical ergonomic interventions” in Driessen et al’s (24) systematic review of RCT, based on the preponderance of physical changes that were produced in equipment and workstations (the authors’ other category was “organizational ergonomic interventions”); Krungkraipetch et al (75) classified this intervention study as a “modifier” intervention during evidence synthesis and grouped it with exercise interventions (distinguished from “mechanical exposure interventions” and “production systems/organizational culture interventions”). The divergent classification schemes adopted by authors of reviews render comparisons across reviews difficult, and can lead to different conclusions on effectiveness. Such differences may stem from conceptual and disciplinary differences between ergonomists and epidemiologists, ie, ergonomists define intervention as the entire process leading up to the implementation of solutions and their follow-up; epidemiologists may sometimes restrict the term “intervention” to the evaluation of the effects of the implementation of solutions (76).
Explanations of findings
A high proportion of the studies reviewed had negative results and did not demonstrate improvement in musculoskeletal outcomes. We have already alluded to several potential methodologic explanations for the negative findings in the evaluated studies, such as the presence of important co-interventions, changes in contextual factors, confounding factors, high attrition rates, low implementation rates, and the use of outcome measures not sensitive to change. As well, several of these studies demonstrated that the intervention did not improve or actually worsened physical, organizational and/or psychosocial work demands targeted, as for example, in the three PE interventions (refer to supplementary table S3). Our analysis also showed that many of these interventions lacked or failed to document many of the key elements of workplace interventions proposed by St-Vincent et al (26, 27). Where indicated by the study authors, we retrieved and consulted companion papers for more details on the intervention process (49, 77). But in general, such information was either not provided, perhaps due to journal length restrictions, or the steps were not carried out. If the assumptions of the St-Vincent et al model are correct, and these elements are necessary to implement work changes that will successfully reduce exposure to work demands associated with WMSD and thereby reduce incidence, prevalence or intensity of WMSD, this could partly explain some of the lack of effectiveness of interventions observed. Importantly, it raises the possibility of theory failure (33). In the case of the PE interventions evaluated in this review (all of which failed to improve musculoskeletal outcomes), one could question whether, in theory, PE interventions that rely on workers alone to identify risk factors and identify and implement solutions are an effective approach in producing workplace changes that could potentially lead to musculoskeletal health benefits. Although workers are best suited to describe their own work situation, it is the work of the ergonomist to discern the factors that may influence work activity (eg, organizational context, social climate, age, gender, experience, work shift, etc.), integrate this complexity in their analysis of work demands and their determinants, as well as to engage company stakeholders and weigh budget, short- and long-term feasibility, and company priorities in order to arrive at a consensus on the most appropriate solution(s).
Denis et al (78) critically reviewed the advantages and limits of “complete” versus “turnkey” WMSD intervention approaches, prompting the reader to consider which of these may theoretically be more likely to improve musculoskeletal outcomes. It is hypothesized that complete interventions (similar to the St-Vincent et al approach), with their strong emphasis on work activity analysis and diagnosis of determinants of work demands, though time-consuming, have the power to bring changes to several aspects of work, and the solutions are specific to the work environment, increasing the likelihood of success (78). Turnkey interventions, ie, expert-led quick and reusable ready-made solutions to reduce WMSD, often chosen based on the sector and type of WMSD potentially ignore many relevant risk factors and contextual factors that may influence the impact of the intervention, failing to address the complexity of WMSD; further, the generic nature of the solutions may lead to them being rejected and unsuccessful.
It is therefore worth paying attention to the intervention process and how it might influence effectiveness. It would be particularly useful if authors of intervention studies described the intervention in sufficient detail to include all actions and strategies taken by the intervention team throughout their contact with the workplace to develop and implement changes. Authors of intervention studies may also wish to consider using musculoskeletal indicators that are sensitive to change, take into account relevant confounders, document co-interventions and changes in contextual factors throughout the intervention and take them into account in analyses.
Strengths
Our study has several strengths: it is the first systematic review, to our knowledge, to focus on workplace interventions targeting work organization and the psychosocial work environment. Previous reviews looking at work organizational or psychosocial interventions were either not systematic (13), combined in their synthesis interventions both with and without an organizational component (eg, computer workstation adjustments only) (24) or focused on specific groups of workers (25) or body regions (upper limbs) (68). Another strength is the use of an extensive search strategy covering 11 key databases in health sciences, social sciences and occupational health, in both English and French. In addition, we supplemented our main analyses with an analysis of the presence of 12 key workplace intervention elements, which highlight the intervention process. This analysis, among other things, allowed us to bring to light process divergences across interventions and gaps in reporting by authors of intervention studies. But the importance of these divergences and their relation to intervention effectiveness on musculoskeletal outcomes remains to be demonstrated. We recommend that future research study these issues and evaluate the effectiveness of interventions that incorporate the key elements of the intervention model proposed by St-Vincent et al (26, 27) because this approach may potentially lead to advances in prevention of WMSD.
Limitations
Due to time constraints, we did not search “grey literature” (studies published outside of peer-reviewed scientific journals such as dissertations, book chapters, conference proceedings/abstracts, research reports, reports from governmental or non-governmental organizations, etc.). The possibility exists that some studies were missed; the sensitivity of the search strategy was not assessed. Second, although we excluded interventions that specifically recruited injured workers, we did not exclude studies on populations characterized by high pain prevalence at baseline. For example, in Caspi et al (59), the three-month prevalence of low-back and neck/shoulder pain was respectively 62% and 50%, in line with reports among nursing personnel (69). We believe that the inclusion of such populations strengthens the ecological validity of our review, as symptom-free populations are improbable, notably in healthcare settings. However, the inclusion of populations with varying baseline symptom prevalence does increase the heterogeneity among studies. Third, our methodologic quality criteria did not identify studies with “fatal flaws” in the design of the intervention itself, such as the work hour reduction study with a high proportion of part-time workers with already reduced hours (54). This study scored 60% in the methodologic quality appraisal, but in our opinion, did not have the capacity to validly answer the authors’ research question, and was therefore excluded at a subsequent step, prior to analysis and evidence synthesis.
Fourth, our review does not allow us to evaluate or comment on the contexts or worker populations in which a specific intervention is likely to be effective or ineffective. Our findings suggest that supplementary pauses may be effective in different contexts. The numerous negative studies in this review and the high number that did not take into account or describe contextual factors may suggest that taking workplace context into account in the design and evaluation of an intervention may be an important but often neglected aspect of such interventions. The St-Vincent et al model suggests that intervention effectiveness is expected to be context-specific and likely dependent, in part, on the level of commitment and buy-in of workplace stakeholders, which may be influenced by the process of involving workplace stakeholders at various stages of the intervention.
Concluding remarks
We conclude on moderate evidence for the effectiveness of supplementary breaks in reducing musculoskeletal symptom intensity. The evidence was of low to very low quality for the other types of interventions studied. Better quality studies are needed to allow definitive conclusions to be drawn on the effectiveness of work organizational or psychosocial interventions to prevent or reduce WMSD. The results of this review are relevant to occupational health practitioners, public health and occupational health authorities responsible for occupational disease prevention, as well as researchers planning to conduct WMSD prevention intervention studies.



