Work participation among employees with common mental health problems (CMHP) is an increasingly important, yet highly complex phenomenon (1). The complexity of work participation is that work can cause CMHP and on the contrary, it can be the solution to those who are affected by CMHP. Under certain conditions, work contributes to the well-being and work participation of employees with CMHP. As the Organisation for Economic Co-operation and Development (OECD) calls for preventing instead of reacting to negative work outcomes, such as sickness absence and reduced work capacity (2), a thorough understanding of how to promote work participation is needed. Common mental disorders refer to depression, anxiety disorder, or stress-related disorder (3, 4). However, a large number of employees who suffer from such problems are undiagnosed and do not receive treatment (5). We also consider this group of employees at risk of negative work outcomes, as a consequence of psychological complaints. Since most people affected by CHMP or psychological complaints are employed and actually working, this phase needs increased attention while the individual is at work (6, 7). Therefore, we use a relatively broad definition of employees with diagnosed mood, anxiety or stress-related problems as well as self-reported psychological complaints.
Previous studies on work participation among employees with CMHP show that staying at work and being productive is affected by individual factors such as higher symptom severity (eg, a past history of CMHP, co-morbidity), and work-related factors (eg, lower job control, job strain or a supportive work environment) (1, 8). While these studies give an insight into factors that promote or hinder work participation, it remains unclear what really enables employees with CMHP to effectively continue working? As work participation is both a means and a goal to promote one’s level of work performance and the ability to stay at work, we need to unravel these two aspects and how they interact in order to develop effective interventions for employers (8, 9). Other reviews in occupational health have concluded that the interaction between work outcomes, the underlying mechanisms, and how actors in the work environment collaborate have proven crucial to intervene effectively, and yet these are not yet clearly understood (5, 10, 11). Therefore the present study addresses the recommendation to move from ‘what works’ to promote work participation to ‘what works, for whom, under what circumstances and how’ (12, 13). This calls for a novel approach in our attempt to understand work participation, in which realist research may provide a suitable methodological answer. Pawson et al (14) developed the realist review approach from the philosophical tradition of critical realism, which seeks to consider the complexity of causal relations when explaining social interactions and interventions (9, 14). It is a theory-driven evaluation method providing an analysis that is more explanatory in nature.
Our initial program theory to develop an explanatory framework for work participation is the Capability-for-Work model (15). This model is based on the concept of capability, as developed by Sen (16). Capabilities represent a person’s opportunity and ability to achieve certain human functionings, taking into account someone’s particular circumstances. Previous articles have applied the literature on human development and capabilities to the work context (17, 18). Among the many things that human beings might develop the capacity to do, employment and work are addressed as a functioning (19). Furthermore, following Sen (16), it is not enough to establish the resources individuals have, but rather to consider what they can actually do or become with those resources to achieve certain (work) functionings. These so called ‘conversion factors’ refer to the process of converting one’s resources to tangible capabilities, resulting in work functioning that the employee chooses to achieve. In this, Bonvin (20) refers to personal and social conversion factors, which play a key role with regard to capability for work.
In this study, work participation is operationalized by two work outcomes (21). The first outcome is stay at work (SAW), that is, ‘the employee is currently working’ addressing a relatively new concept in the field of occupational health that has no uniform definition in the literature (22). We define SAW as continuing to work, indicated as no absenteeism or not being absent >50% or ≤6 weeks (8, 23). Besides SAW, we are interested in different facilitators of work performance (WP), or ‘how the employee functions at work’. WP refers in the present review to subjective (self- or other rated) performance or objective (externally rated) performance (24). Derived from the Capability-for-work model, we hypothesized that work participation is determined by the way an employee succeeds in converting personal- and work inputs and resources (ie, conversion factors) into capabilities and subsequently into work functioning such as SAW and WP (15).
To the best of our knowledge, a realist synthesis of evidence relating to SAW and WP for employees with CMHP has not been conducted thus far. In this study, we aim to create a better understanding of work participation by providing a robust, systematic overview of current knowledge and by developing an explanatory framework. To do so, this study adopts a systematic realist review approach. The following research question guided this approach: What mechanisms promote SAW and WP (work outcomes), for whom, under what circumstances and how, amongst employees with CMHP?
Methods
Identification and selection process
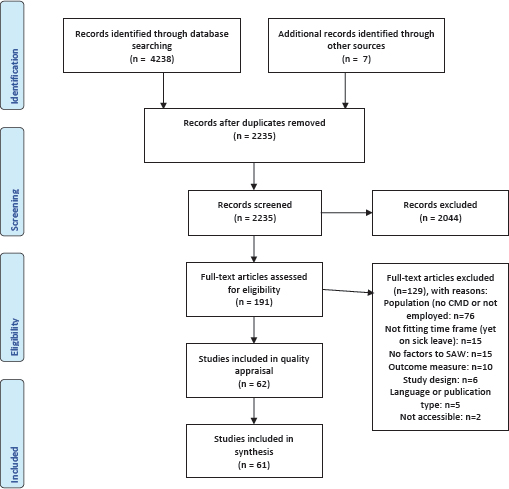
For the sake of readability, in this section we briefly report the steps followed in the review process. A more detailed description of the review methodology is provided in the supplementary material, www.sjweh.fi/article/4005, Appendix A, including the identification and selection process, use of theory and appraisal tools, and data extraction and synthesis. The systematic realist review followed the steps and procedures outlined by RAMESES publication Standards for Realist Synthesis (25). Details of the protocol for this systematic realist review are registered on PROSPERO and can be accessed at www.crd.york.ac.uk/prospero/display_record.php?RecordID=108913 and can be found in the published study protocol (21). Regarding the search strategy and study selection, we adhered to the PRISMA guidelines for the conduct of systematic reviews (26). All scientific peer-reviewed studies available between 1 January 1995 and 26 June 2020 were retrieved in this systematic realist review. We conducted a computer-based search in the following databases, Pubmed, Medline, PsycInfo, Embase, Cochrane, Cinahl and Web of Science. An example can be found in supplementary Appendix A. Three independent authors dually assessed the studies’ rigor and relevance in each of the following phases using the selection criteria (table 1): title and abstract screening, full text screening and quality appraisal using the Mixed Methods Appraisal Tool (MMAT) (27) and data extraction.
Table 1
Inclusion and exclusion criteria.
Extraction and analysis process
For each study, the research team drafted one or more context-mechanisms-outcome (CMO) configurations, first independently and later discussed dually. These configurations described the causal links between context, mechanisms and outcomes (ie, SAW or WP). From each study, information from the methods, results and discussion section regarding relevant contextual factors or mechanisms leading to the selected outcomes were retrieved. Studies of high quality (see table 2) were used to form CMO configurations. Studies with insufficient methodological quality (answering ‘no’ to screening questions) were excluded and studies with risk of bias, rated as ‘medium quality’, were only used to support CMO configurations derived from high quality studies. Several iterative steps were followed to explore patterns within the extracted CMO configurations to develop middle range program theories, using ‘if…(context), then…(outcome), because of…(mechanisms)’ statements. Middle-range program theories are based on at least two included studies. In the final stage of the synthesis, we developed an explanatory framework, using the initial program theory to demonstrate what works, for whom, under what circumstances and how to promote SAW and WP.
Table 2
Overview of the characteristics and design of the studies. [CMD=common mental disorder; MMAT=mixed methods appraisal tool; LCA=latent class analysis; Obs=observational; RCT=randomized controlled trial; Int=intervention; SAW=stay at work: WP=work performance]
| Author and reference | Type of study and study methodology | Number of participants | Study population (type of employees/sector) | Industry/ type of employees | MMAT score (H=rated as ‘high quality’; M=rated as ‘medium’) |
|---|---|---|---|---|---|
| Articles reporting on both SAW and WP | |||||
| Arends et al 2019 (51) | Obs: LCA | 158 | Dutch employees with CMD, mostly highly educated, who are in return to work trajectories | Various sectors | M: 3/5: no data on representativeness, low N for LCA |
| Birney et al 2016 (54) | Int: parallel two group RCT | 300 | US employees with depression, mostly middle-aged, Caucasian, female, highly educated | Unknown, part-time, fulltime and self employed | H: 4/5 blocked on race/ethnicity |
| Chen et al 2011 (69) | Obs: analytical cross-sectional study | 452 (controls) 226 (cases) | Taiwanese young workers with depressive disorder at psychiatric clinics | Micro electronics engineers | H: 5/5 |
| Daley et al 2009 (60) | Obs: cross sectional descriptive | 308 patients | Canadian patients with symptoms of insomnia and 147 with insomnia syndrome, of whom 76.4% worked day shifts | Unknown | H: 5/5 |
| Danielsson et al 2017 (6) | Obs: qualitative | 27 | Swedish workers, of various ages and job types, suffering from common mental disorders | Various sectors | H: 5/5 |
| Duijts et al 2008 (45) | Int: RCT | 57 (int) 61(control) | Dutch employees in 3 companies, with psychosocial health complaints, who are still working in health and educational sector at risk of sickness absence | Health Education | H: 4/5 low adherence to intervention (49%) |
| Dunner et al 2001 (63) | Int: before after studies | 816 | US patients with recurrent major depression who worked part-time or fulltime | Unknown | H: 5/5 |
| Ebert et al 2016 (53) | Int: RCT | 63 | German employees with elevated stress levels, various sectors, mostly women and medium or high educated | Economy, service, social, IT, health, other | H: 5/5 |
| Evans-Lacko & Knapp 2018 (29) | Obs: cross sectional survey | 2985 | Employees with self-reported depression from 15 different countries worldwide, mostly in Asian countries, from several sectors except marketing sector | Unknown, company size and working status varied | H: 4/5 Low response rate, representability of target population unclear |
| Hilton et al 2008 (41) | Obs: cross sectional study | 60,556 | Employees in New Zealand and Australia working in large companies, high level of psychological distress | Large public and private sector employers | H: 4/5 low response rate, blue collar underrepresented |
| Jha et al 2016 (81) | Int longitudinal study | 331 | US employed patients with nonpsychotic chronic or recurrent depression with current episode of more than 2 months | Unknown | M: 3/5 missing information about int., adherence and drop out |
| Johnson et al 2015 (64) | Int: controlled trial, not randomized. | 40 of whom 20 in int. group | US working health care professionals, aged 18-65 years, who are at least 50% or higher employee status. With major depressive disorder, single episode or recurrent | Health care | H: 4/5: No sub group analysis or confounders due to small group of participants |
| Lerner et al 2010 (39) | Obs: longitudinal cohort study | 286 | US employees with depression, despite occupational group, married, gender, recruited through primary health care centres | Various sectors | H: 4/5: incomplete outcome data |
| Lerner at al 2020 (70) | Int: RCT | 253 | US veterans, with mild to moderate depression | Veterans | H: 5/5 |
| Plaisier et al 2010 (59) | Obs, descriptive longitudinal | 1035 | Dutch workers with common mental health disorders | Unknown | H: 5/5 |
| Plaisier et al 2012 (33) | Obs: cross sectional, descriptive | 1522 | Dutch workers who have an employer or who are self-employed (5%) with depression or anxiety disorder | Manual and non-manual jobs, self employed | H: 5/5 |
| Richmond et al 2017 (36) | Int: prospective, quasi experimental design | 344 | US employees, mostly female (71%), white (87%) and non-Hispanic (81%), average education was 16 years, working for the government, with depression or anxiety | Diverse in human service providers | H: 4/5 incomplete outcome data |
| Ridge et al 2019 (48) | Obs: Qualitative | 73 | 73 Australian and UK participants self-identified as having experienced depression | Professional or manual work | H: 4/5 quotes are rather general |
| Rost et al 2004 (47) | Int: RCT | 198 | US employed patients with major depression, mostly female (84.4), high school educated (88.5%), mostly full time employed (80%) | Administrators, managers, sales people, services | H: 4/5 missing information on intended treatment and utilization |
| Sahlin et al 2014 (50) | Int: before and after study | 33 | Swedish female health care workers suffering from high level of stress | Health care workers | H: Mixed method: 5/5 qual, 3/5 for quant: confounders not taken into account in analysis, not representative |
| Swanson et al 2011 (62) | Obs: cross sectional survey | 367 | US workers with any sleep disorder, with shift work | White, grey, blue collar and shift workers | M: 3/5: low response rate, no validated questionnaire |
| Telle et al 2016 (67) | Int: RCT one factorial design with two groups | 99 | German employees who subjectively felt mentally distress due to work-related issues, voluntary participation | 13 different private corporations and federal and public organizations | M: 3/5: incomplete outcome data and low adherence to intervention |
| Uribe et al 2017 (57) | Obs: cross sectional | 107 | Colombian employees with major depression or double depression (N=107) | Unknown, employees part time, full time, self-employed | H: 5/5 |
| van den Berg et al 2017 (40) | Obs: Cross sectional analytical | 661 | Dutch health care employees, mostly female and intermediate or high education, with a mental disorder | Health care workers | H: 5/5 |
| van Mill et al 2013 (44) | Obs: epidemiologic cohort study | 707 CMD and 728 without | Dutch depressed or anxious individuals who work 8 hours or more | Unknown | H: 5/5 |
| Wang et al 2007 (55) | Int: RCT | 604 of whom 304 in int. group | US employees with at least moderate depression, enrolled in a large managed behavioural health care company (insurance) | Diverse sectors: airline, insurance, banking, public utility, government, manufacturing | H: 5/5 |
| Woo et al 2011 (49) | Int: controlled trial | 106 and 91 healthy controls | South Korean employees with major depressive disorder | Employees in highly industrialized areas | H: 4/5 incomplete outcome data |
| Articles reporting on SAW | |||||
| Chakraborty & Subramanya 2013 (31) | Comparison Obs | 43 | Indian, industrial employees who work in an urban aeronautical industry who experience stress | Urban industrial employees | M: 3/5 selection bias |
| Cocker et al 2011 (56) | Obs: descriptive survey data | 320 | Australians with life time depression | Various sectors | H: 5/5 |
| Corbiere et al 2016 (28) | Obs: qualitative | 22 | Canadian, mostly highly educated employees with symptoms of depression | Public, private and non-profit sector | H: 4/5 Recall bias, currently not working but during last 5 years |
| Hammond et al 2017 (30) | Obs: qualitative | 6 | Clinical psychologists in Australia who run a solo private practice, who experienced burnout maximum 2 years ago | Health care: psychologists | H: 5/5 |
| Kawakami et al 1999 (65) | Int: RCT | 81 in int, 77 in control group | Workers, mostly male, who are distressed and employed in Japan | Manufacturing company | M: 2/5: no information on randomization, no baseline comparison between groups, adherence unknown |
| Keus van de Poll et al 2020 (43) | Int: RCT | 100 | Swedish, mostly government workers using occupational health services suffering from CMD or work stress | Mainly public service employees | H: 4/5 not representative study population |
| Kok et al 2017 (32) | Obs: before and after study | 1222 | Dutch employees with an affective disorder | Unknown | H: 5/5 |
| Laitinen-Krispijn & Bijl 2000 (34) | Obs: longitudinal study, follow up 1 year | 3695 | Dutch male employees with major depressive disorder, dysthymia, simple phobia and substance abuse/dependence | Unknown | M: 3/5: unclear outcome measure on duration of sick leave, few confounders |
| Leijten et al 2013 (37) | Obs: longitudinal study | 354 | Older Dutch employees with psychological problems (not specified) | Unknown | H: 5/5 |
| Lexis et al 2009 (58) | Obs: prospective cohort | 3339 | Dutch employees with depressive complaints, from various organizations and companies | Various sectors | H: 5/5 |
| Lexis et al 2011 (68) | Int: RCT | 139 | Dutch employees with depressive complaints, from various organizations and companies | Office workers | H: 5/5 |
| Linden et al 2011 (52) | Int: before after study | 44 outpatients | German employees, with generalized anxiety disorder in outpatient departments | Unknown | M: 3/5 missing info on representativeness and confounders |
| Mackenzie et al 2014 (46) | Int: RCT | 93 | Australian workers with depression, generalizes anxiety disorder and social phobia | Unknown | M: 2/5: randomization not explained, loss to follow up |
| Noordik et al 2011 (23) | Qualitative | 14 | 10 Dutch women and 4 men, aged 25–58 (mean age 38) years, partially returned to work | Various sectors incl. health care | H: 5/5 |
| O’Haire & Rodriguez 2018 (66) | Int: non RCT | 141 in int., 75 control | US veterans working elsewhere and who were identified with PTSD after 9/11 | Veterans | H: 4/5: 24,7% of population is working |
| Sado et al 2014 (61) | Obs: retrospective cohort | 194 | Japanese workers in a manufacturing company with repeated sick leave because of mental disorders | Manufacturing company | H: 5/5 |
| Virtanen et al 2007 (38) | Obs: prospective study, | 6663 female, 1323 male | Finnish local government employees and health care employees in public services with psychological distress | Public sector employees | H: 5/5 |
| Vlasveld et al 2013 (101) | Obs: cross sectional | 1425 | Dutch workers with psychopathology (anxiety or depressive disorder) | Unknown | H: 5/5 |
| Woodall et al 2017 (35) | Qualitative: semi-structured interviews | 15 | UK current or former service users with mental health conditions | Unknown | H: 5/5 |
| Articles reporting on WP | |||||
| Adler et al 2006 (72) | Obs: longitudinal | 286 | US patients with major depressive disorder (N=105) or dysthymia (N=72) or both (N=109) | Mostly women 1) managers, professionals, and technicians; 2) sales, service, and support; | H: 5/5 |
| Beck et al 2014 (78) | Obs prospective cohort | 432 | US working patients, on routine depression treatment | Unknown | H: 4/5: work context not in analysis |
| Bertilsson et al 2013 (74) | Obs qualitative | 17 | Swedish persons with CMD employed in regular job market, mainly women | Private and public sector | H: 4/5 late reflection on data |
| Danielsson et al 2020 (84) | Int: pilot RCT | 147 | Swedish employees with CMD, mainly female, on work-directed rehabilitation | Various sectors | H: 5/5 |
| Furukawa et al 2012 (75) | Int: RCT non-blinded | 108, of whom 58 in int. group | Japanese currently employed, mostly male, fulltime workers with minor depression at a large manufacturing company | Manufacturing company | H: 5/5 |
| Haslam et al 2005 (71) | Obs: Qualitative | 74 | UK workers with personal experience of anxiety/depression in the previous 2 years and who are mostly (2/3) uncompliant with medication | Various sectors | H: 4/5 the interpretation of results insufficiently supported by data |
| Kim et al 2019 (73) | Obs: cross sectional | 173 | South Korean workers with depression | Various sectors | H: 5/5 |
| Lam et al 2011 (80) | Int: pilot study | 31 | Canadian health agency workers (predominantly women, above 40), with symptoms of depression, counselling is purchased by employer and self-referred to the EAP | Health care | M: 4/5: small pilot study, self-referred to intervention, no confounders in analysis |
| Lappalainen et al 2013 (77) | Int: small scale RCT | 11 int and 12 in control (waiting list) | Finnish male workers with stress and mood problems | Unknown | M: 2/5: no information on randomization, self-assessed outcome, no blinding |
| Lindsater et al 2018 (76) | Int: RCT | 50 int. 50 in control | Swedish employees (of whom 82% employed full time or part-time), with adjustment disorder or exhaustion disorder | National sample | H: 5/5 |
| Loukine et al 2016 (42) | Obs: cross-sectional | 2528 | Canadian workers with self-reported mood or anxiety disorders | Unknown | H: 5/5 |
| Nigatu et al 2015 (79) | Obs: descriptive longitudinal | 555 | Dutch employees, currently having a major depression or anxiety disorder, mostly white collar workers | Unknown | H: 5/5 |
| Okajima et al 2020 (83) | Int: RCT | 92 | Young Japanese employees with insomnia | Mostly office employees | H: 4/5: many lost to follow up |
| Petersson et al 2018 (82) | Int: RCT | 132 | Swedish Patients with mild to moderate depressive disorder | Various sectors, white- / blue collar | M: 3/5: low adherence and incomplete outcome data |
| Rothermund et al 2016 (102) | Int: controlled obs. trial | 367 | German employed patients of whom N=174 use psychotherapeutic consultation in the workplace | Three companies, unknown | H: 5/5 |
Results
The search process yielded 2235 records, shown in figure 1. Screening on title and abstract led to the exclusion of 2044 articles, resulting into 191 articles for full text screening. After full text screening and quality appraisal, 61 articles were included. One study was excluded due to insufficient methodological quality. Studies ranked as medium quality were characterized by relatively low response rates or incomplete outcome data, or missing information regarding adherence and randomization procedures. The majority of the studies used quantitative data (N=53), only seven studies used qualitative data and one study used mixed methods. Table 2 provides an overview of characteristics of the included studies per outcome. Below, we first present the middle range program theories, which frame mechanisms and contextual factors that facilitate SAW, followed by the middle range program theories that facilitate WP.
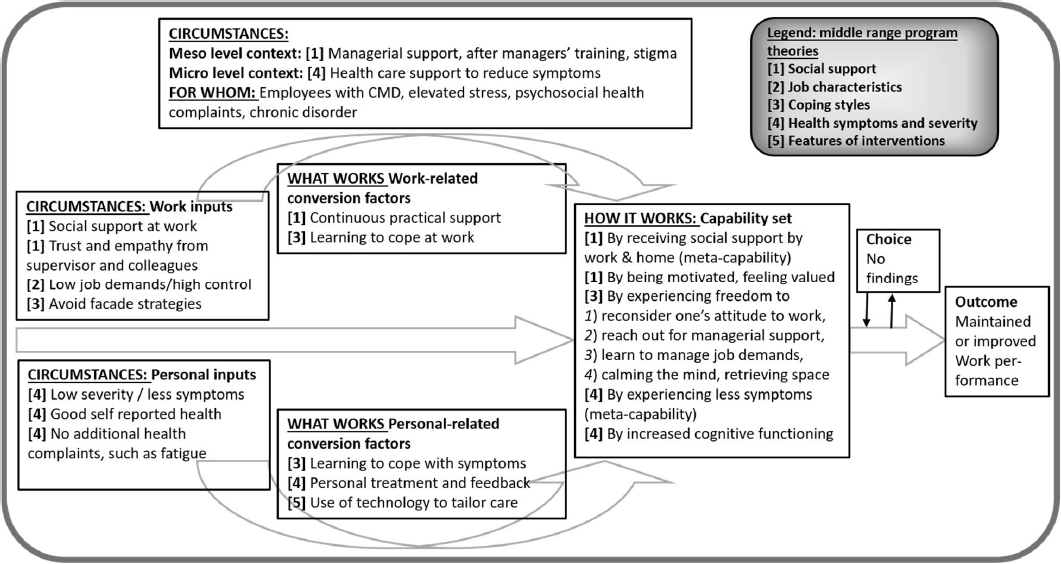
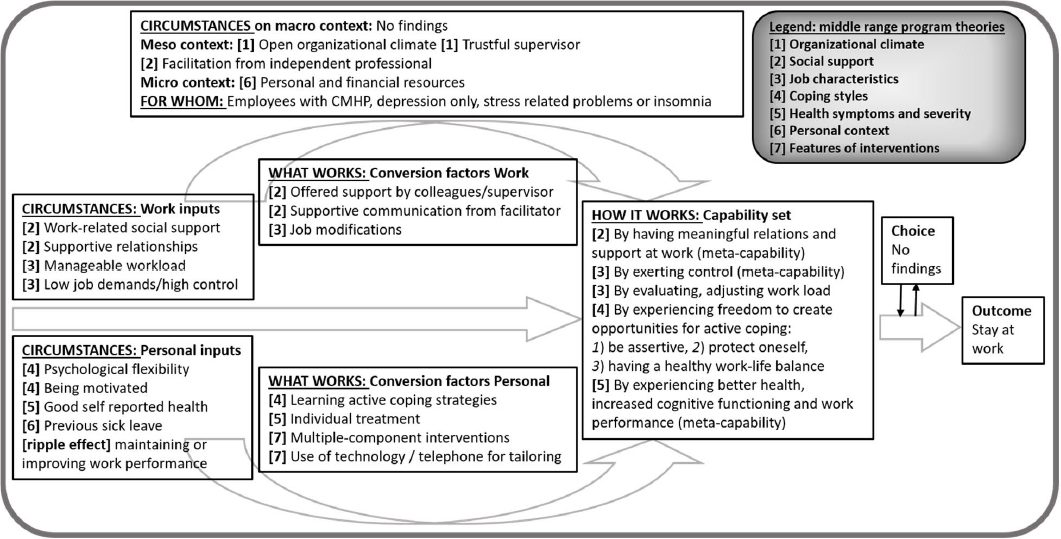
Tables 3 and 4 present the summary of mechanisms that facilitate each outcome, SAW and WP, respectively. To explain the causal relations between context, mechanisms and outcomes we describe each middle range program theory. Thereafter, we present our findings in an explanatory framework. Figures 2 and 3 depict what works, for whom, under what circumstances and how, refining the Capability-for-work model. In-depth information regarding the data synthesis of CMO configurations per study, leading to the middle range program theories, is presented in supplementary Appendix B.
Table 3
Mechanisms that facilitate stay at work (SAW), among employees with CMHP.
Table 4
Mechanisms that facilitate work performance (WP).
Figure 2
How to promote staying at work (SAW) among employees with CMHP, framed by Capability-for-Work model, based on 45 studies.
Stay at work (SAW)
The mechanisms, presented in table 3, reveal how organizational climate, social support in the work context, and perceived job characteristics enable employees with CMHP to stay at work. Furthermore, coping, severity of mental health symptoms, the personal context and features of interventions are factors affecting the chance for SAW.
Middle-range program theory 1: Organizational climate. Trustful relationships in which the supervisor shows openness to talk about mental health conditions in an open climate in general, may contribute to SAW among employees with depression because (a lack of) openness by supervisors is mirrored by employees (28, 29).
Middle-range program theory 2: Social support. Adequate and timely social support and supportive relationships, from colleagues but particularly supervisors who are willing to assist and listen to work related problems, increase the chance for SAW among employees with CMHP because this helps to obtain a manageable workload (23, 30–34). Facilitation, by either a mental health professional or job retention specialist – who (i) acts independently, with sympathy and pragmatism (ii) provides an expert insight and (iii) is familiar with the workplace – also improves the likelihood to stay at work (23, 35, 36).
Middle-range program theory 3: Perceived job characteristics. There is an inconsistent pattern with regard to job demands and control and its effect on SAW. A possible program theory, based on CMO configurations, could be that experiencing low job demands and high job control helps an employee to exert control over one’s own work, including adjustments that can be made (32, 33, 35, 37–40). Heavy workload, overtime and high job strain reduce the chance for SAW, among employees with stress or depression (28, 30, 31, 38). Job modifications help, however in a different way for white- versus blue-collar workers, due to the type of duties and work context (23, 30, 41–43).
Middle-range program theory 4: Coping styles. A lack of adaptive skills, due to reduced psychological flexibility and a different perspective on situations, reduces the capacity to bear responsibilities, which in turn has a negative effect on SAW (30, 32, 44). Useful coping skills for SAW are: being more alert on signals of reduced mental health, reading and understanding own signals, exerting control over one’s own work and workload, balancing positive and negative influences of work, making adjustments and informing colleagues, protecting oneself, taking control, and being assertive (23, 28, 30, 35, 37, 45–49). Also, being highly motivated towards the job increases the likelihood for SAW (23, 31, 50, 51). Adversely, employees who do not talk about their depression, hide themselves or deny their symptoms have a higher risk of absenteeism (6, 28–30, 34, 48). Improving active coping skills and advancing self-management in daily life subsequently contribute to SAW (36, 46, 50, 52–54) by addressing work in counselling besides personal problems (36, 43, 55)
Middle-range program theory 5: Health symptoms and severity. Better mental and physical health contributes to SAW because the employee’s experience of lower severity of symptoms leads to improvement in WP (by increased cognitive functioning or decreased exhaustion) (30, 33, 39, 56–60). Likewise, facing additional health complaints as well as previous sick leave, decreases the chance for SAW (44, 56, 60–62). Interventions offering psychotherapy or pharmacotherapy seem more effective than preventative treatment or stress reduction interventions (45, 47, 50, 52, 54, 62–68).
Middle-range program theory 6: Personal context. Personal characteristics may contribute to SAW based on possible underlying mechanisms, such as financial drive by owning a house, being self-employed, or being married (30, 33, 38, 56). Employees with depressive disorders who had more life events, personal problems or exposures in other life domains than work may experience tension or confusion about symptoms, leading to more absence days (28, 30, 38, 69).
Middle-range program theory 7: Features of interventions. If interventions focus on multiple components, for example if they target both personal inputs (symptom reduction and coping with symptoms) and work inputs (coping at the workplace or a better work-related health), this may lead to an increased likelihood for SAW (35, 46, 47, 49, 50, 52–54). In these interventions, using online or telephone support systems in addition to face-to-face care is successful because it (i) increases adherence and better access to early and regular screening and (ii) tailors messages to needs and integrates learned skills into daily life (46, 47, 53–55). Preventative, worksite-based job retention interventions or adding a work-focused intervention to integrated care did not seem effective on the outcome of SAW (45, 67, 68, 70).
Explanatory framework to stay at work based on the Capability-for-Work model. Based on the initial program theory and the presented middle range program theories, figure 2 depicts an explanatory framework for SAW. The mechanisms (the ‘how’) are mainly to be found under conversion factors and the capability set. The circumstances that facilitate SAW are to be found under Context on macro, meso, micro level and Personal- and Work inputs. We suppose that employees with CMHP can realize SAW through the following set of capabilities: (i) having meaningful relations and social support at work, (ii) exerting control, (iii) evaluating and adjusting the workload, (iv) experiencing freedom to create opportunities for active coping, (v) and experiencing better health, increased cognitive functioning and work performance. Those capabilities reflect the employee “being able” as well as “being enabled” (15). We also found the so-called ‘ripple effects’, in which the outcome of one CMO configuration became the context or mechanisms for the next in the chain of causality. For example, interventions on symptomatology (mechanism) seem to reduce the severity of symptoms (outcome). This outcome acts as an input (severity of symptoms) on SAW (outcome).
Work performance
Table 4 presents the summary of the mechanisms that facilitate WP (outcome 2) for employees with CMHP. Five middle-range program theories are proposed on how social support, perceived job characteristics, coping styles, health symptoms and severity and features of interventions promote the employee’s WP respectively.
Middle-range program theory 1: Social support. A work environment where supervisors feel comfortable to offer help and support to employees, helps employees to feel motivated and valued, which in turn may have a positive effect on their job performance (29, 71). Practical job support from colleagues and managerial support from supervisors, offered continuously while functioning at work despite CMHP, helps to improve WP as the employee experiences trust and empathy (6, 29, 33, 48, 51, 69, 71).
Middle-range program theory 2: Perceived job characteristics. There is inconclusive evidence on interventions regarding job characteristics and their beneficial effect on WP among employees struggling with CMHP. Some studies suggest the combination of (perceived) high job demands and low job control may reduce WP among employees with CMHP (39, 40, 72). However, other studies contradict this suggestion (33, 73).
Middle-range program theory 3: Coping styles. If employees with CMHP experience reduced capacity to work, they initially use working facade strategies (such as increasing hours or taking work home), compensating possible shortcomings to avoid reduced performance because of fear and perceived stigma from colleagues and supervisor. However, these strategies seem counterproductive, as they result in emotional exhaustion, dissatisfaction and loss of refueling in the long run (6, 41, 71, 74). Interventions (eg, counselling) prove to promote WP because they improve effective coping styles in the long term. Examples of these interventions are (i) reconsidering one’s attitude to work, (ii) reaching out for supervisor support, (iii) learning new approaches to manage job demands, and (iv) calming the mind and retrieving space for recovery (6, 36, 39, 53, 54, 67, 75–77).
Middle-range program theory 4: Health symptoms and severity. Self-rated health and severity of symptoms are important predictors of WP among employees with depression, anxiety or sleep disorder because once the employee experiences less symptoms, work productivity improves (39, 57, 59, 62, 72, 78). Chronicity of symptoms has shown to reduce WP (33, 51, 59, 79). Interventions to reduce symptoms result in increased cognitive functioning, a pro-active attitude towards change, better mental-interpersonal task performance, improved time management and output, and subsequently to increased WP (36, 47, 49, 50, 53, 55, 64, 67, 76–78, 80, 81). Among employees with stress, interventions improve stress recovery and symptom management, which subsequently leads to improved productivity (50, 53, 64).
Middle-range program theory 5: Features of intervention. Interventions that use technology, through email, phone or app, may reduce mental health symptoms as well as work limitations. The use of these technologies helps to better monitor the employee’s behavior by tailoring the interventions with personal feedback, fostering belief changes and facilitating the transfer of training components to daily life (53, 55, 70, 76, 77, 80, 82–84)
Explanatory framework on work performance based on the Capability-for-Work model. An explanatory framework on how to realize WP among employees with CMHP is presented in figure 3. This figure illustrates that both personal- and work-related conversion factors promote WP through a set of capabilities. The capability set consists of (i) receiving social support from work and home, (ii) being motivated and feeling valued, (iii) experiencing freedom for active coping, and (iv) experiencing less symptoms and increased cognitive functioning. Where WP acts as a goal (outcome on its own), it also acts as a capability for SAW. This may support the idea of meta-capability suggested by Venkatapuram (85): being a capability in itself and also conditional (contextual factor) for achieving other capabilities. Capabilities may or may not result into work outcomes due to constrained or limited choices, as proposed in the Capability-for-Work model. Unfortunately, the included studies did not provide insights in the opportunity to make individual choices to achieve both work outcomes (see figure 2 and 3).
Discussion
This paper provides a systematic realist review of studies that have assessed work participation among employees with CMHP. This review (i) contributes to the development of a more uniform definition of the concept SAW among the study population at risk of negative work outcomes due to CMHP, (ii) identifies mechanisms that promote work participation through the outcomes of SAW and WP (iii), sheds light on how the work context may promote work participation in practice and research, and (iv) provides an explanatory framework using middle range program theories, based on the Capability-for-Work model. These contributions, their implications for practice and future research as well as the limitations of the present study are discussed below.
Contributions of the present study
The present study adds to our understanding of the complex, multifactorial process of work participation for employees with CMHP. The overall findings of this review are consistent with the findings of previous reviews on related outcomes, finding theoretical support for the dynamic interrelation between personal factors and work-related factors leading to work participation for employees with CMHP (5, 8, 86). However, our review also shows how social support in the work context, perceived job characteristics, coping styles and better experienced health may promote WP and SAW. Furthermore, insight is given in how organizational climate and personal context promote SAW and what features of interventions seem effective. In addition, the findings of this review shed light on underlying mechanisms towards an adequate, supportive, work environment that enables employees with CMHP to remain at work. Because we used a systematic realist review approach rather than summarizing factors that may not provide insights into causal relationships, we were able to “unpack” each mechanism, and reveal under what circumstances these mechanisms lead to the outcome of interest. In this way, it explains what often is experienced by practitioners in individual cases and is hard to support by empirical evidence due to averaged, usually small effects in quantitative studies.
Notwithstanding all efforts regarding preventative mental health interventions, our findings call for more attention to employees already facing CMHP in the work context, in line with the recommendations of the OECD and other researchers (5–7, 87). We operationalized SAW in such a way that it includes employees with CMHP who are currently working or reported partly sick. Interestingly, we observed in the review process that the current research agenda is still focused on absenteeism and return to work concerning employees with CMHP rather than SAW, despite the growing evidence base on prevention and positive psychology in the general working population (88). A possible explanation could be that the phase of being on sick leave or absent as a negative work outcome is directly related to costs of employers and society as a whole and thus of a greater interest in research and practice. Besides, being absent is more visible than being at work while being affected by CMHP. Signals of CMHP usually develop silently and slowly, making it harder for employers to signal and intervene. Also, CMHP are often stigmatized, making it hard for employees to decide whether or not to disclose their condition to their employer (89). This supports our decision to include both diagnosed and self-reported CMHP in this study. To gain insight in the promotion of work participation in a group of at-risk employees, we choose not to emphasize the highly discussed boundary between normality and pathology. Because complaints are often dynamic and fluctuating, such a clear distinction is not necessary for the purpose of this review. We found that the mechanisms and contexts to promote work participation apply to those employees with psychological symptoms in the subthreshold group, to those who did not seek help or had no access to care, as well as to employees with a diagnosed common mental disorder.
Regarding the retrieved mechanisms, more attention in the scientific literature was given to (intervening on) personal factors than work-related or organizational factors. This implies that, in interventions that promote work participation, efforts and effects seem to be attributed to the person rather than the work situation. This is not in line with the literature showing that work-related factors have great causal effects on sustainable work participation among the general working population. For example, the Job Demands Resource theory suggests that in order to effectively continue working despite facing CMHP, solutions can be found in the work context and job designs, more than intervening (only) on personal factors (90). Besides, despite our study approach to search in each included study for contextual factors, it was difficult to identify the organizational circumstances in which each mechanism or outcome occurred apart from the pre-defined intervention components. However, even if organizational circumstances were not analyzed explicitly, we succeeded to identify mechanisms that refer to the role of employers in supporting employees to stay at work (receiving supervisor support, being offered job modifications). This supports the evidence regarding the important responsibility of employers in facilitating employees with CMHP (13, 86, 91, 92). Therefore, more insight into work-related mechanisms and circumstances leading to SAW is needed to develop effective organizational interventions for employees with CMHP (93).
The use of the Capability-for-Work model contributed to the findings of our review in three ways. First, considering the plethora of CMO configurations derived from 61 studies, this model helped us to arrange factors and understand causal effects and underlying mechanisms. As such, we could distinguish inputs (pre-existing work- or personal factors that are often non-changeable) from conversion factors and capabilities (often changeable). Through a capability approach lens, mechanisms (how and why) were identified as conversion factors and capabilities. More specifically, we found that both personal conversion factors and social, work-related conversion factors are needed to realize capabilities to work (20). The framework adds to the understanding of causal relationships between all factors and the outcomes SAW and WP. Nevertheless, we emphasize that what may be a conversion factor or capability for one employee, can be a pre-existing personal factor for the other. Second, our review contributes to the development of the capability set for work, defined by Abma et al (94) in that we add to their seven capabilities, presenting specific capabilities for employees with CMHP. For example, the capability of building and maintaining meaningful contacts at work, is elaborated in our study by the capability of receiving work-related social support and having trustful relations with the supervisor and colleagues. Third, using the Capability-for-Work model, our review reveals that it is not the medical condition itself but its interactive effect with WP and circumstances that influence the employee’s functioning at work and ability to stay at work (95). Therefore, it will be more interesting to investigate whether employees are “being able” and “being enabled” to participate in work, and thus to unravel which set of capabilities is needed to do so, rather than solely to assess their medical condition. In this way, we highlight the importance of placing work participation in a wider spectrum of human development, shifting the focus from having a mental health condition as an impairing factor to the establishment of capabilities and choices (96).
Implications for practice
This review provides valuable information to employers and occupational health professionals as to what implications they should focus on in order to promote work participation for employees with CMHP. The first practical implication refers to the importance of multilevel interventions from employers, addressing overarching themes on an organizational- and team-level combined with tailored interventions on the individual level. Employers could improve the work situation of employees with CMHP, and the teams and organizational culture they work in, by creating a socially safe, open working climate. On the individual level, employers could ask employees who are having a hard time at work what they can still do despite their problems, and what they need in their job or in the work context in order to remain at work. This way, the employer enables the employee to convert inputs and resources into capabilities. Employers should seek advice from occupational health professionals since they can support, on different levels and on both sides, the employer as well as the employee with CMHP.
Next, we highlight the need for early intervention, and suggest professionals to find ways to assess and intervene on capabilities and WP before employees report sick, besides assessing the employee’s (severity of the) condition or other pre-existing personal factors. Occupational health professionals can discuss individual short-term adjustments in the job or work context with the employee and employer. For long term solutions, those professionals can support employers to detect a mismatch between the employee’s capabilities and the work (context).
In line with addressing employee’s abilities rather than problems, we recommend two ways to increase employee’s experience of freedom, often referred to as autonomy in the literature. On the side of healthcare and the psychological treatment of individuals with CMHP, we recommend (mental) healthcare professionals to address work-related problems in the consultation and to transfer lessons learned, such as active coping, to the work context. Likewise, we urge employers to facilitate work and a work environment where lessons learned can be practiced by employees, by enhancing autonomy or facilitating temporary job modifications (97). This may have the twofold effect of increasing employee’s capabilities and employee engagement as well as contributing to mentally healthy workplaces (95).
Finally, providing continuous social and practical support at the workplace is crucial to promote work participation. Employers should take preventative measures whilst the employee is still at work, for example by educating supervisors and colleagues on reading signals and talking about mental health. Also, employers can increase supervisors’ skills on ways to offer support to employees and increase know-how of situations that require referral to occupational health professionals.
Recommendations for future research
The following recommendations for future research result from this study. First, our review showed that WP acts as a meta-capability for SAW, illustrating a possible parallel link between CMHP and the level of work performance during the phase of staying at work (98, 99). Further research is needed to test the link between both work outcomes, verifying whether and how WP can be used as a means to decrease the severity of CMHP, resulting in an increased chance to stay at work. Second, additional research is warranted to further develop the Capability-for-work model on work participation for employees with CMHP. We recommend the use of empirical data to test the newly presented set of capabilities among employees with CMHP in work participation. Besides, to further explore the causal relations presented in the explanatory framework, mean correlations that exist in the study population on group level could be tested but also underlying mechanisms that occur on an individual level. Third, we recommend realist evaluation as an approach to “unpack” underlying mechanisms and contextual factors in order to develop effective organizational interventions. As our research included only one mixed methods study and few qualitative studies, we cannot emphasize enough on the integration of process and outcome evaluation, using novel, mixed methods evaluation designs (12, 100).
In a next step, based on our review results, we will develop and evaluate a multilevel workplace intervention. This intervention aims to improve supervisor’s skills and competence to support employees with CMHP and create a work context that promotes work participation.
Strengths and limitations
This systematic realist review provides a comprehensive overview of mechanisms and contextual factors promoting work participation. By using a realist approach, we succeeded to unravel mechanisms and their causal relationship with the work environment and selected outcomes. The realist data extraction- and data analysis process was time-consuming. However, it seemed valuable as the rigorous understanding of not only what works, but also under what circumstances and how work participation occurs, resulted in more practical contributions. Furthermore, we stimulate the debate among researchers on the understanding of work participation by contributing to theory development of the Capability-for-work model regarding various work participation outcomes.
The present review has a number of limitations that must be addressed. First, it could be argued that the heterogeneity in the type of studies and measures of outcomes led to CMO configurations with different levels of relevance or rigor. To overcome this, two researchers conducted each review step independently, using clearly defined concepts, inclusion and exclusion criteria and assessment tools. Also, the researchers discussed every defined CMO configuration. A second limitation refers to the dichotomous outcome of SAW. Due to the inconsistent definition of SAW in the literature, we screened a plethora of studies using the opposite outcome of SAW, reported as absenteeism or sickness absence. Barriers leading to absenteeism are not automatically facilitators of SAW, so the outcome of absenteeism is not irreversible as such. Therefore we only included studies that compared employees with CMHP who were absent to similar employees who stayed at work. A third limitation is that although we used information regarding context, mechanisms or implementation from the discussion section in publications, the contextual information was only explicitly provided to a certain extent (study population, employment sector). Where information regarding the context of the study was not given, we cannot know under what circumstances certain interventions work. This is a common limitation of realist synthesis and, therefore, is also relevant to our study. For an in-depth discussion on the use of realist research, we refer to our protocol paper (21).
Concluding remarks
This systematic realist review revealed mechanisms and contextual factors that promote both WP and SAW for employees with CMHP. In these situations, the work environment can support employees to participate at work. Program theories using a realist approach reveal how the organizational climate, social support in the work context, and perceived job characteristics enable employees to participate at work. Furthermore, coping styles, severity of mental health symptoms, the personal context and features of interventions enable employees to participate at work. By providing an overview of recent scientific literature, this study provides valuable insights and practical implications for employers, occupational health professionals and researchers in the development and evaluation of evidence-based interventions. Novel explanatory frameworks, based on the Capability-for-Work model, present causal relations between personal- and work factors and a set of capabilities leading to SAW and WP. Finally, the study adds to the debate on using novel methodological research approaches such as realist synthesis, answering what works, for whom, under what circumstances and how.