Musculoskeletal pain is a major cause of morbidity and disability among people of working age, affecting over 40 million workers in western European countries (1). Almost all individuals will experience at least one episode of musculoskeletal pain at some point in their lives and most of them will recover without residual functional loss. Nevertheless, an Australian study of primary care patients found that approximately a third of episodes progressed from acute to chronic and disabling (2). In Spain, it has been estimated that more than 39 million working-days were lost due to musculoskeletal disorders in 2007 (3), and temporary work disability related to such disorders represents 20% of sick leave days (4).
Overall, in the working-age population, the prevalence of musculoskeletal pain is high and appears to be increasing over time (5). However, the main economic impact is attributable to a small proportion of persistent cases with more severe disability (6). Moreover, the economic, social, and functional consequences for an individual who has disabling musculoskeletal pain are greater than for an individual whose pain is not disabling. For example, workers with disabling low-back pain restrict their participation in all aspects of social and family activities, and also find it more difficult to return to work after long periods of sickness absence (7).
Established risk factors for musculoskeletal pain include not only occupational physical activities (8), but also psychological factors such as culturally influenced health beliefs, low mood, and tendency to worry about common somatic symptoms (9–15). However, it is unclear whether these psychological risk factors primarily influence the development and persistence of pain, or whether their impact is more on the disability that it causes. If they relate more to the disability that musculoskeletal pain causes (which was our prior hypothesis), their effects may be underestimated in analyses that do not distinguish disabling from non-disabling pain.
To explore this possibility, we analyzed data from a longitudinal study carried out among Spanish nurses and office workers, in which we assessed the associations of health beliefs, low mood, and somatizing tendency with the development and persistence of disabling as compared to non-disabling musculoskeletal pain. The data were collected as part of the international Cultural and Psychosocial Influences in Disability (CUPID) study (16).
Methods
The methods of data collection have been reported in detail elsewhere (9, 16). In summary, computer-assisted personal interviews were used to collect data in the workplace, both at baseline (between November 2007 and February 2010), and again after a follow-up interval of 12 months. Samples of 716 nurses and 483 office workers from four hospitals and one university in Barcelona were identified from employment records and invited to take part in the study. To be included in the study, participants had to be aged 20–59 years and been in their current job for ≥12 months. Written informed consent was obtained from all who agreed to take part, and the Parc de Salut Mar Ethics Committee of Barcelona and the Health and Safety Committee of each participating centre approved the study. The baseline and follow-up questionnaires were originally drafted in English, translated into Spanish, and then checked by independent back-translation (16).
Ascertainment of musculoskeletal pain
Musculoskeletal pain was ascertained using a similar style of questions to those in the Nordic questionnaire (17). Both at baseline and follow-up, participants were asked whether they had experienced pain during the past month for a day or longer in each of ten anatomical sites (low back, neck, right and left shoulder, right and left elbow, right and left wrist/hand, and right and left knee). Those who answered yes were asked whether during the past month the pain had made it difficult or impossible to do normal jobs around the house or carry out any of a specified list of other everyday activities (for low back: getting dressed or cutting toe nails; for neck: getting dressed; for shoulders: combing/brushing hair, bathing/showering or getting dressed; for elbows: opening bottles/jars/taps or getting dressed; for wrists/hands: writing, locking/unlocking doors, opening bottles/jars/taps or getting dressed; and for knees: walking up and down stairs/on level ground or getting dressed). For each anatomical site, pain was classed as disabling if it had made it difficult or impossible to carry out normal jobs around the house or any of these other activities. Otherwise, it was classed as non-disabling.
Ascertainment of exposures at baseline
Health beliefs about musculoskeletal pain
Baseline health beliefs about musculoskeletal pain were assessed in three domains (relating to the effects of physical activity, work-relatedness, and prognosis), questions being adapted from the Fear-Avoidance Beliefs Questionnaire (18). Health beliefs about physical activity were considered adverse if, either for someone with low-back or upper-limb pain, participants “completely agreed” or “tended to agree” that both physical activity should be avoided as it might cause harm and rest was needed in order to get better. Health beliefs about the work-relatedness of musculoskeletal pain were considered adverse if participants “completely agree” or “tended to agree” that either low-back or upper-limb pain is commonly caused by people’s work. Participants were classed as having adverse health beliefs about prognosis if either they “completely agreed” or “tended to agree” that neglecting such problems could cause permanent health problems, they also “completely disagreed” or “tended to disagree” that such pain usually gets better within three months.
Mental health
Mental health was evaluated at baseline through the relevant section of the SF-36 questionnaire (19). Participants were asked five questions about how they had felt during the month before interview: (i) “Were you a happy person?”, (ii) “Have you felt calm and peaceful?”, (iii) “Have you been a very nervous person?”, (iv) “Have you felt downhearted and low?” and (v) “Have you felt so down that nothing could cheer you up?”. Each item was scored on a 6-point scale (all of the time, most of the time, a good bit of the time, some of the time, a little of the time, none of the time). Scores were then summed (taking into account whether more of the time was better or worse), and grouped in approximate thirds of the overall distribution in the study sample (good, intermediate, and poor).
Somatizing tendency
Somatizing tendency was explored at baseline using a subset of elements from the Brief Symptom Inventory (20). Referencing five common somatic symptoms (faintness or dizziness, pains in the heart or chest, nausea or upset stomach, difficulty breathing, and hot or cold spells), participants were classified into three categories according to the number that had been at least moderately distressing in the week before the baseline interview: (i) “no distressing somatic symptoms”, (ii) “one distressing somatic symptom” and (iii) “two or more distressing somatic symptoms”.
Potentially confounding factors
Among other things, the baseline CUPID questionnaire also asked about sex; age (classified in four ten-year bands); occupation (nurse or office worker); history of musculoskeletal pain for a day or longer in the past year (yes or no) by anatomical site; job satisfaction (overall dissatisfied/very dissatisfied or satisfied/very satisfied with current job); and occupational activities. Participants were asked whether on an average working day, they: (i) used a keyboard or a typewriter for >4 hours in total; (ii) carried out other tasks involving repeated movements of the wrist or fingers for >4 hours in total; (iii) repeatedly bent and straightened the elbow for >1 hour in total; (iv) worked with their hands above shoulder height for >1 hour in total; (v) lifted weights of ≥25 kg by hand; (vi) climbed up or down ≥30 flights of stairs a day; and (vii) knelt or squatted for >1 hour in total. Specific anatomical sites were classed as exposed to relevant work-related physical activity if the participant reported lifting weights of ≥25 kg by hand (low back), work with hands above shoulder height (neck and shoulders), repeated bending of the elbow (elbows), either use of a computer keyboard or other repeated movements of the wrist or fingers for >4 hours (wrists/hands), and either climbing up or down ≥30 flights of stairs a day or kneeling/squatting for >1 hour in total (knees).
Statistical analysis
Analysis was based on anatomical sites. In defining whether pain was incident or persistent, we considered the part of the body affected and the laterality of symptoms. For example, hand/wrist pain (non-disabling or disabling) was considered to be new (at follow-up) if it had not previously been present in the same hand/wrist in the month before baseline, even if the other hand/wrist had been affected.
Multilevel multinomial logistic regression modeling was used to explore the role of health beliefs about musculoskeletal pain, mental health, and somatizing tendency as predictors for: (i) non-disabling pain in the past month at follow-up; and (ii) disabling pain in the past month at follow-up. Anatomical sites that had been pain-free in the month before baseline were “at risk” of having new non-disabling pain and new disabling pain at follow-up. Anatomical sites with non-disabling pain in the month before baseline were “at risk” for persistence of non-disabling pain and development of new disabling pain at follow-up (worsening pain). Anatomical sites with disabling pain in the month before baseline were “at risk” for development of non-disabling pain at follow-up (improving pain) and persistence of disabling pain. In each case, the comparator was having no pain in the past month at follow-up.
To assess the effect of potential confounders, three types of model were fitted. In the first (model 1), each of the exposures was analyzed separately with adjustment for sex, age (in four ten-year bands), and occupation. In the second (model 2), each exposure was analyzed separately, with adjustment for the same variables as in model 1, and also for job satisfaction and exposure to relevant work-related physical activity. In the third (model 3), all risk factors were included in a single model, together with the variables of adjustment from model 2. For anatomical sites that had been pain-free in the month before baseline, history of pain at the same anatomical site in the past year was also considered a potential confounder, and therefore was also included in the three models described above.
For model 1, we used two-level logistic regression with a random intercept, in which anatomical sites were clustered by person. For models 2 and 3, which included work-related physical activities as potential confounders, we employed three-level modeling with clustering of the ten anatomical sites in six anatomical areas (low back, neck, right or left shoulder, right or left elbow, right or left wrist/hand, right or left knee), which in turn were clustered by person. We did this because questions about physical activities did not distinguish which side(s) of the body was involved. Associations were summarized by odds ratios (OR) with their 95% confidence intervals (95% CI). Statistical analysis was carried out using the Generalized Linear Latent and Mixed Models (GLLAMM, 2010) program in Stata 11.1 software (StataCorp, College Station, TX, USA).
Results
A total of 1105 subjects (667 nurses and 438 office workers) completed baseline questionnaires (a participation rate of 96.6%), and usable information was obtained at follow-up for 971 (87.9%) of those initially recruited. Response rates at follow-up according to the characteristics of participants at baseline have been presented in detail elsewhere (9). They were slightly lower among the youngest subjects, but otherwise differed little in relation to the psychological risk factors of interest.
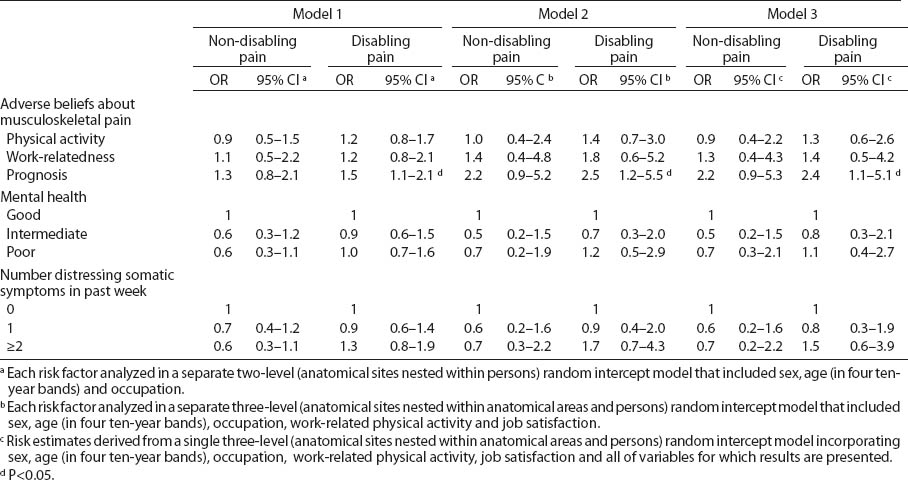
Table 1 sets out the numbers of anatomical sites and percentages in which non-disabling and disabling pain were present at follow-up, according to pain status and exposure to risk factors as assessed at baseline. Among the 8083 anatomical sites that had been free from pain in the past month at baseline, new non-disabling and disabling pain had developed at follow-up among 341 (4.2%) and 412 (5.1%) sites, respectively. Among the 710 anatomical sites at which non-disabling pain was reported in the month before baseline, 292 (41.1%) still had non-disabling pain after 12 months and 92 (13%) had pain that had become disabling. Among the 971 anatomical sites with disabling pain at baseline, 408 (44.5%) still had disabling pain after 12 months and 87 (9.5%) were still painful, but the pain was no longer disabling.
Table 1
Number of anatomical sites and percentages in which non-disabling pain and disabling pain occurred at follow-up, according to baseline pain status and exposure to risk factors at baseline.
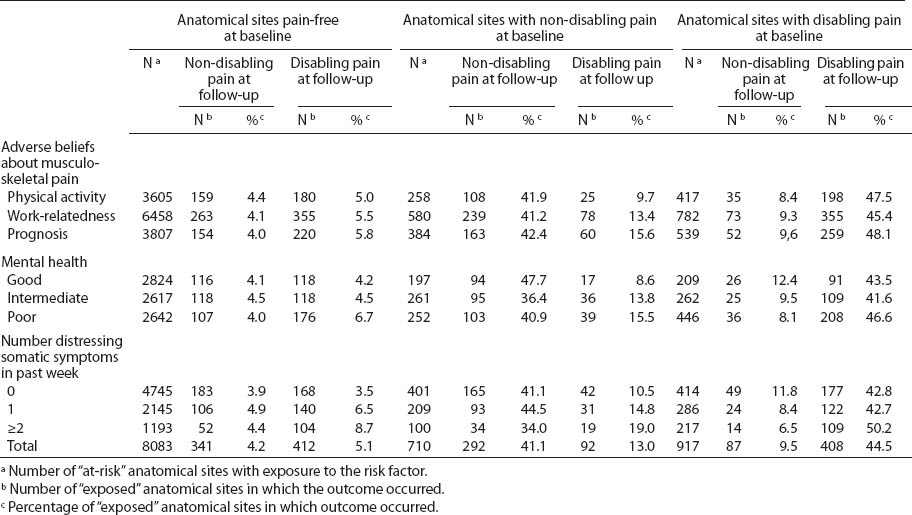
Table 2 presents the associations of new non-disabling and disabling pain with baseline risk factors in an analysis, which was restricted to anatomical sites that were pain-free in the month before baseline. After adjustment for sex, age, occupation, and history of pain at the same anatomical site in the year before baseline (model 1), the risk of developing new disabling pain was associated with adverse health beliefs about pain prognosis (OR 1.4, 95% CI 1.1–1.8), poor mental health (OR 1.7, 95% CI 1.3–2.3, in comparison with good mental health), number of distressing somatic symptoms at baseline (OR 2.7, 95% CI 2.0–3.7, for those reporting two or more distressing somatic symptoms as compared with none), and more weakly with adverse health beliefs about the work-relatedness of pain (OR 1.4, 95% CI 1.0–2.0). These associations persisted after adjustment also for job satisfaction and exposure to relevant work-related physical activity (model 2 in table 2), and with additional mutual adjustment (model 3). In contrast, the only clear association with new non-disabling pain was for multiple distressing somatic symptoms, and the OR was lower than for disabling pain.
Table 2
Baseline risk factors for new non-disabling and new disabling musculoskeletal pain in anatomical sites which were pain-free at baseline: analysis based on anatomical sites. [OR=odds ratio; 95% CI=95% confidence interval]
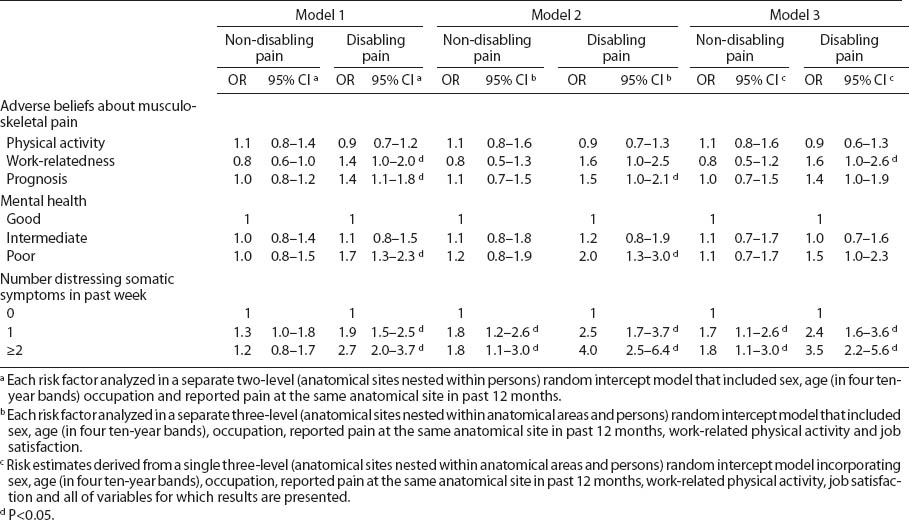
Table 3 shows associations of the same pain outcomes with the same baseline psychological exposures in an analysis restricted to anatomical sites with non-disabling pain in the past month at baseline. Although risk estimates were less precise, their pattern was similar to that of table 2. Risk of disabling pain at follow-up tended to be higher in association with all of the risk factors except adverse beliefs about physical activity, whereas associations with non-disabling pain at follow-up were weaker with no elevation of risk at all for poor mental health.
Table 3
Baseline risk factors for persistence of non-disabling and development of disabling musculoskeletal pain in anatomical sites with non-disabling pain at baseline: analysis based on anatomical sites. [OR=odds ratio; 95% CI=95% confidence interval]
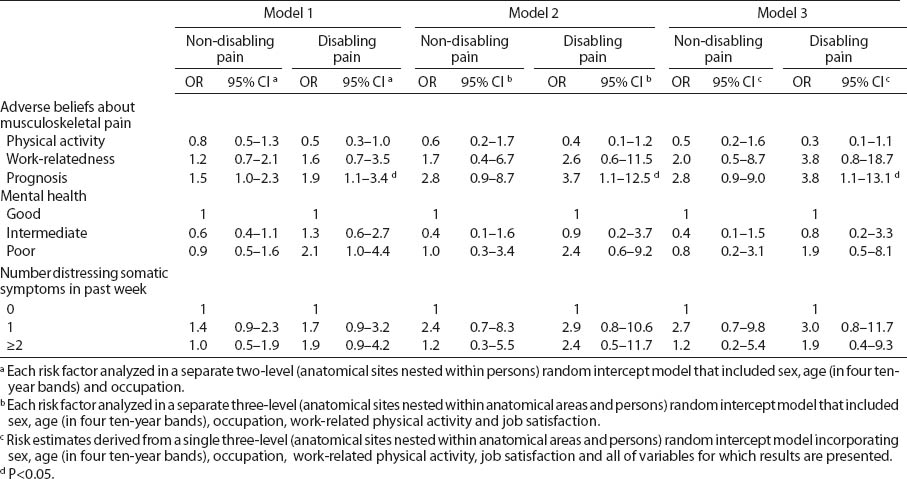
Among the anatomical sites with disabling pain at baseline (table 4), persistence of disabling pain was more common where participants had adverse beliefs about pain prognosis (OR 2.4, 95% CI 1.1–5.1 in the fully adjusted model). However, there were no significant associations with non-disabling pain at follow-up.
Discussion
In this study, the development of disabling musculoskeletal pain was associated with most of the psychological risk factors examined, and its persistence was predicted by adverse beliefs about prognosis. In contrast, associations with the development and persistence of non-disabling pain were weaker. This suggests that the influence of established psychological risk factors is less on occurrence and awareness of symptoms and more on the disability they cause.
The particular strengths of the study were its longitudinal design, the high response rates both at baseline and follow-up (9, 16), and the way that information was collected at baseline, which allowed us to distinguish more reliably incident from persistent pain (for both non-disabling and disabling pain) at each of ten different anatomical sites. In addition, questions on adverse beliefs about pain, mental health, and somatizing tendency were taken from validated instruments (18, 19, 20), and have previously demonstrated predictive validity for incident and persistent musculoskeletal pain in longitudinal studies (9, 11). Furthermore, to avoid possible misunderstanding about pain location, anatomical sites were depicted in diagrams, similar to those of the Nordic questionnaire (17), which has been shown to have acceptable reliability (21).
Against these strengths, several limitations should be considered. It is possible that workers with disabling musculoskeletal pain at baseline were underrepresented due to healthy worker selection, which could have led to an underestimation of the prevalence of persistent disabling pain one year later. However, it is unlikely that this would have caused spurious differential associations of baseline psychological risk factors with disabling pain at follow-up. Sick leave accounted for the loss of only 29 of the 134 participants who failed to answer the follow-up questionnaire, and even if disabling musculoskeletal pain were responsible for the absence among most of these 29 participants, there is no reason to expect that it would be substantially less associated with psychological risk factors than disabling pain that did not cause sickness absence.
Our definition of incident and persistent non-disabling and disabling pain at each anatomical site was based on the occurrence of symptoms during the month before the follow-up interview, according to whether or not they had also been present in the month before baseline. Thus pain that was classed as incident at follow-up represented a new episode, but not necessarily the first occurrence of pain at the anatomical site in question. Moreover, some anatomical sites that were classed as having persistent pain may have been free from pain for part of the interval between baseline and follow-up. Also, our definition of disabling and non-disabling pain at each anatomical site was based on self-reported difficulty or inability to carry out specified everyday activities, and no assessment was made by direct observation or any form of examination. However, there is no reliable standard against which to assess the accuracy of reported pain, and it has been observed that case definitions based only on musculoskeletal symptoms generate similar associations with occupational risk factors to more complex case definitions that include findings from clinical examination (22).
Similarly, the nature of the psychological risk factors was such that they could only be ascertained by self-report. This raises the possibility that the observed associations, even though predictive and not simply cross-sectional, might reflect differences in propensity to report health problems when they occur rather than true differences in the risks of symptoms and disability. We cannot rule this out, but to account for the observed pattern of results, the higher propensity for reporting among, say, somatizers would have to relate specifically to the reporting of disability rather than non-disabling pain. Moreover, cross-sectional analyses have indicated that somatizing tendency is an important risk factor for report not only of disabling pain, but also of prolonged sickness absence (23). It seems unlikely that major differences in propensity to report would extend to a more concrete outcome such as sickness absence.
The threshold that we applied in classifying pain as disabling (making at least one of a specified set of activities difficult or impossible) was the same as has been applied in previous studies (9, 11, 24). In some cases, the disability may have been rather minor, but this would not account for the differences that were observed between disabling and non-disabling pain in associations with risk factors. If anything, it would be expected to obscure differences.
The CUPID study did not collect information about comorbidity. However, to cause a spurious association with disabling as compared with non-disabling pain, comorbid disorders would have to have been associated with a higher prevalence of psychological risk factors at baseline and independently carry a higher risk of new development and persistence of disabling pain at follow-up. It is possible that some progressive diseases of the musculoskeletal system make disability more likely to develop or persist. However, evidence to date suggests that associations with psychological risk factors are stronger for non-specific pain than specific diseases such as osteoarthritis (25) or carpal tunnel syndrome (26). Nor did the questionnaire ask about physical activities outside work, which do not appear to have as much influence on musculoskeletal pain as occupational activities (27, 28).
Most evidence concerning the role of psychological risk factors in the causation and prognosis of musculoskeletal pain comes from studies focused on low-back and, to a lesser extent, upper-limb pain. However, there are reasons to expect similar associations for pain at other anatomical sites. A longitudinal study among working-age subjects found that psychological risk factors, such as adverse beliefs, low mood, and somatizing tendency, were similar for different sites of musculoskeletal pain, including the knee as well as the back and upper limb (29).
Previous epidemiological research has indicated that strong adverse beliefs about the work-relatedness of pain are associated with a higher incidence of disabling low-back pain (9, 30); and that adverse beliefs about prognosis are associated with the persistence of low-back (9, 31) and upper-limb pain (11). Also, low mood has been related to the development of new disabling low-back pain (9, 15), the persistence of both upper-limb (11) and disabling low-back pain (9), the transition from acute to chronic disabling low-back (13, 31) and neck pain (14), and the incidence and persistence of knee pain (29). Furthermore, somatizing tendency has been linked with both the incidence (11, 12) and persistence of upper-limb pain (11), the development of new disabling low-back pain (9), the persistence of shoulder/neck pain (32), and the incidence and persistence of knee pain (29). While some of these longitudinal studies have focused on disabling pain, none has looked at associations specifically with pain that was not disabling.
Our finding that adverse beliefs about pain prognosis were associated with the persistence of disabling musculoskeletal pain and the transition from non-disabling to disabling musculoskeletal pain was not surprising. A theoretical model proposed by Pincus et al (33) postulated that the exposure to a combination of a “microsystem” of individual health beliefs and a “macrosystem” of cultural health beliefs, prevalent in the society in which the individual lives, might produce maladaptive pain-coping behaviors and attitudes to illness in ways that promote chronicity and disability. More difficult to explain is the finding that adverse beliefs about the work-relatedness and prognosis of pain were also associated with the development of disabling musculoskeletal pain in anatomical sites free from pain at baseline. However, it is plausible through a nocebo effect (34) that individuals who strongly believe musculoskelatal disorders are long-term health problems, which carry a poor prognosis and may be caused by work activities, could perceive musculoskeletal pain (triggered perhaps by mechanical exposures) to be more disabling. Against this, however, there was no increased risk of disabling pain in relation to adverse health beliefs about physical activity. This seems to be a fairly consistent finding in cross-sectional data from the CUPID study more widely (35) and accords also with a study of patients from primary care in Spain (36). In the future, it will be possible to check the observation through analysis of longitudinal data from the CUPID study in other countries.
We found that low mood and somatizing tendency were predictors of the occurrence of new disabling pain at anatomical sites that were initially pain-free, and this was not explained by differences in exposure to work-related physical activities and job dissatisfaction. The fact that low mood was more related to disabling than non-disabling pain was not surprising. It has been described that low mood on its own, and not necessarily as a consequence of musculoskeletal pain, can lead to poor pain recovery (33). Furthermore, experimental research has indicated that induction of negative mood has a powerful effect on acute pain, reducing pain tolerance and leading to higher levels of self-reported pain severity (36). Although the association with low mood was reduced after adjustment for somatizing tendency, this does not necessarily argue against it having an independent causal role in the occurrence of new disabling musculoskeletal pain. Both, poor mental health and high somatizing tendency could be considered persistent and disabling syndromes, and, in spite of their psychobiological differences (37), they often coexist. We found only a weak association between low mood and the transition from non-disabling to disabling musculoskeletal pain. This may be because the progression from pain to disability is only partially explained by poor mental health (38), or our study sample may have been unrepresentative simply by chance.
Report of distress from somatic symptoms was more strongly associated with disabling than non-disabling musculoskeletal pain. It is plausible that people who tend to worry about somatic symptoms are more prone to avoid activities that aggravate pain and, therefore, are more disabled by them (39, 40).
In general, the psychological risk factors that we examined showed stronger and more consistent associations with disabling than non-disabling pain. New onset of non-disabling pain was weakly associated with somatizing tendency, and persistence of such pain tended to be more common among people with adverse beliefs about prognosis. Otherwise, however, no notable associations were apparent for pain that was non-disabling.
Our findings suggest that established psychological factors relate more to the disability that musculoskeletal pain causes than to pain per se. Given also that disabling pain has more severe consequences, this suggests that future studies of psychological risk factors should focus particularly on risks for disabling musculoskeletal pain, which may be diluted if non-disabling pain is included in the case definition.