The work of long-distance truck and bus drivers typically consists of long and irregular hours or shift work, and lengthy sitting periods (1, 2). Busy schedules and lack of healthy food choices and opportunity for exercise while on the road may predispose drivers to an unhealthy lifestyle (1, 3, 4). Irregular eating and snacking is common (3). Shift work and night shifts in general have been found to be associated with unhealthy eating habits as well as with weight gain (5–7). Prolonged sitting at work is an independent risk factor for atherosclerosis and diabetes (8). There are also socioeconomic aspects behind drivers’ lifestyles. Truck drivers are often sedentary in their leisure time, and they consume less fruit and vegetables and more sausages and milk fat than recommended (9–11). Most professional drivers are males, who tend to be sedentary more often and have poorer diet than women (12).
Long and irregular work hours predispose drivers to sleep deprivation, which is associated with obesity and other cardiometabolic risk factors (13, 14), as well as increased risk of road accidents (15, 16). Based on studies about actual sleeping time, truck drivers often suffer from sleep deprivation up to several hours per 24 hours compared to recommendations of 7–8 hours of sleeping time (17–19). Among professional drivers, obesity is associated with increased risk of being fatigued and involved in road traffic accident (15, 20). Among the underlying pathological processes, the central ones are breathing disorders during sleep that are induced by obesity (21).
Obesity is one of the most important health risk factors among professional drivers (15, 22, 23). Worldwide around 57%–87% of truck and bus drivers are overweight or obese (23–26), and obesity comorbidities such as hypertension, dyslipidemia, and type 2 diabetes are common to this profession (23). Overweight and obese truck drivers have substantially greater direct medical costs when compared to drivers of normal weight (23). In a Danish study, hospitalization for obesity or diabetes was more common among truck drivers than among other working populations (22). Additionally, in Europe. obese persons have a 50% higher risk for disability pension when compared to persons who are not overweight (27).
Although unhealthy lifestyle and cardiometabolic risk factors are frequent among professional drivers (22, 28–30), few health education interventions have been targeted at this group. To our knowledge, the only previous randomized trial to prevent obesity was conducted among 1061 overweight transit workers, mostly metropolitan bus drivers, lasting 18 months (25). Participants in the experimental group were encouraged to make healthy food choices and increase physical activity by being offered sports activities and healthy and affordable options in snack vending machines. Dietary habits improved but the modest body weight reduction did not differ from the control group. A Chinese randomized intervention delivered diabetes-related information by mobile messages, which led to a decreased risk of developing diabetes among 104 professional drivers with pre-diabetes symptoms (31).
According to previous studies, the most important factor preventing professional drivers from adopting a lifestyle change is irregular working schedule (3, 25, 32), which disrupt healthy eating habits, as well as sleep, exercise and social life (1). In a US study, almost half of 542 motor freight workers, most of whom were truck drivers, reported that they would not have time to eat right because of their work, although 86% thought it would be especially important to eat right (11). In addition, there are few intervention studies focusing on male workers with the same socioeconomic status as drivers, such as construction and manufacturing industrial workers, with or without shift work. These intervention studies have resulted in clinically meaningful decreases in body weight and cardiovascular risk factors (33, 34). However, males are often less likely than females to participate in lifestyle counseling to improve lifestyle habits, especially to decrease overweight (35–37).
Our primary aim was to study the effects of individual lifestyle counseling (nutrition, physical activity, and sleep) for 12 months on weight reduction and prevalence of cardiometabolic risk factors (especially metabolic syndrome: MeS) among abdominally obese male truck and bus drivers. A secondary aim was to study weight maintenance during a subsequent 12-month follow up (at 24 months).
Methods
Recruitment and randomization of participants
Inclusion criteria included: (i) 30–62-year-old male truck or bus driver, (ii) waist circumference ≥100 cm, (iii) irregular working schedules in long-distance service, (iv) absence of sleep apnea diagnosis or medication for diabetes, and (v) little physical activity during leisure (≤2 times weekly for 30 minutes per session). Voluntary participants were recruited by advertisement in service stations, workplaces, and newspapers and through labor unions. After 1.5 years of recruitment, 209 drivers signed up for the trial (figure 1).
Figure 1
Flow diagram of the study. The lifestyle counseling (LIFE) group participated in 12 months of counseling starting from baseline and the reference (REF) group participated in three months of counseling starting at 12 months. Assessments took place at baseline, 12, and 24 months from baseline.
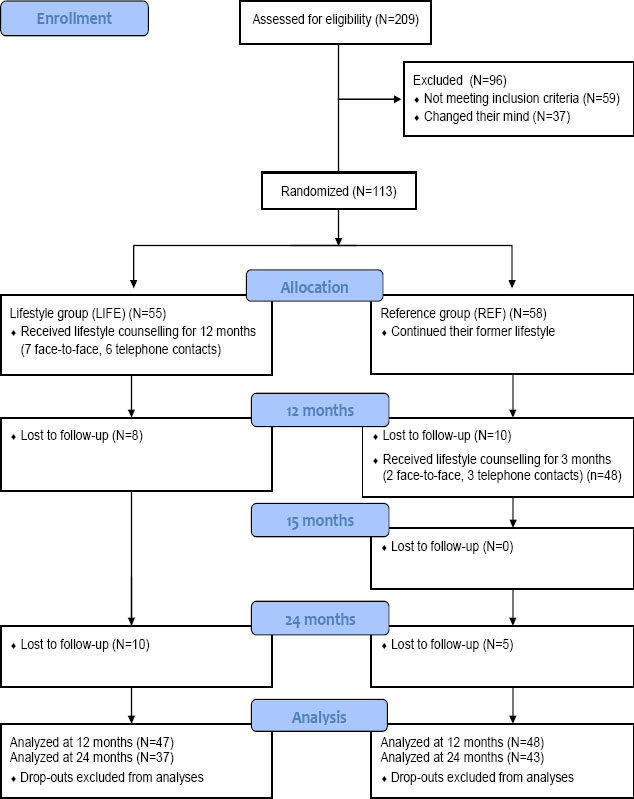
Of these, 113 drivers were eligible for the study and randomized into a lifestyle counseling (LIFE) and a wait-list reference (REF) group. Randomization was performed by a statistician not involved in the study. It was done separately for truck and bus drivers using computerized random numbers in blocks (N=4, with random variation in the block size). The statistician prepared sealed opaque envelopes containing information on the randomization group, and the research secretary delivered the envelopes in consecutive order to eligible participants after a written informed consent was obtained from the participants. Pirkanmaa University Hospital District Ethics Committee approved the study. The research was conducted in accordance with the Declaration of Helsinki (2000). The ultimate aim of the trial, to improve alertness at work and improve sleep through weight loss, will be reported separately.
Lifestyle counseling
The participants in the LIFE group participated in structured monthly lifestyle counseling for 12 months focusing on diet but including also counseling on physical activity and sleep. The contents of the session-specific counseling are described in table 1. Counseling consisted of six individual face-to-face contacts (allocated time 60 minutes) and seven telephone contacts (30 minutes) with trained counselors (two nutritionists and one physiotherapist). The counselors traveled to the participants for the face-to-face meetings. After 12 months, the REF group participated in a shorter 3-month counseling protocol including two face-to-face contacts (at 12 and 15 months after baseline) and three telephone contacts (3, 6, and 9 weeks after 12 months). Counseling was based on the same elements as those used in the LIFE group but in a shortened version. The second year was a follow-up phase (12 months for LIFE, 9 months for REF).
Table 1
The contents of session-specific counseling in the lifestyle counseling group. [F=face-to-face; T=telephone; PA=physical activity]
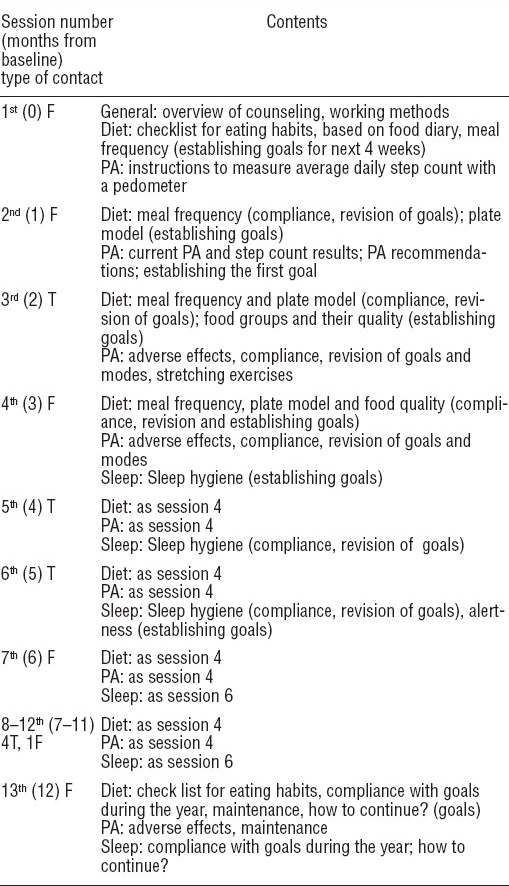
LIFE group counseling aimed at 10% body weight reduction after 12 months. The ultimate dietary targets were to improve meal frequency, increase the consumption of fruit and vegetables (with the help of a “plate model”: half of the portion is filled with vegetables, one fourth with potatoes, rice or pasta, and one fourth with meat or fish), improve fat quality, and reduce low-fiber, rapidly absorbed carbohydrates (38) (table 1). The ultimate goal of physical activity counseling was to add 4000 steps – approximating 30 minutes of moderate-intensity walking (39) – to the daily baseline on five self-selected days of the week. The goal was approached progressively with the help of a pedometer (Omron Walking Style II, HJ-113-E-03-10/05, Omron Healthcare, Kyoto, Japan) by setting smaller goals in a sequence of 2000 steps, which has previously been shown to be achievable (40, 41). The sleep target was ≥6 hours of sleep per 24 hours.
The Health Action Process Approach (42–44) was used as a context to formulate the procedure and contents of the counseling sessions (table 1). The counselors used a manual developed by the research group to follow the intended procedure and content of each counseling session but were also free to emphasize topics most relevant to the participant. At each session, individual goals for diet, physical activity and sleep were set based on participant’s preferences, abilities, and experiences. The participants had a log book of their own to monitor the daily accomplishment of their dietary, physical activity and sleep goals. Feasibility and results of counseling on living habits will be reported separately.
Outcome measurements
Assessments took place at baseline, and at 12- and 24-month follow-up. Body weight was measured by a precision scale (F150S-D2, Sartorius, Goettingen, Germany). Waist circumference was measured three times: (midway between the lowest rib and the iliac crest) and the mean value was used. Dual-energy X-ray absorptiometry (DXA, Lunar Prodigy Advance, GE Lunar, Madison, WI, USA) was used to measure fat and fat-free mass. Blood pressure was measured in duplicate in the morning and afternoon, and the mean value was used. The participants answered a questionnaire on health status and working conditions. At each counseling meeting, weight (Omron HBF-500-E, Omron Healthcare, Kioto, Japan) and waist circumference were measured.
Blood samples were taken for glucose, cholesterol, high-density lipoprotein (HDL) cholesterol and triglyceride analyses after a 12-hour fast. Venous blood was drawn into citric acid/fluoride and ethylenediaminetetraacetic acid (EDTA) tubes. Plasma glucose concentrations were measured fresh, and plasma samples for lipid analyses were stored frozen at -80° C until analyzed. Glucose, total cholesterol, HDL cholesterol and triglyceride concentrations were determined in enzymatic assays in duplicate (Roche Cobas Mira Plus analyzer; Roche Diagnostic Systems, Basel, Switzerland). Low-density lipoprotein (LDL) cholesterol was calculated by Friedewald formula if triglyceride concentration was <4.51 mmol/l. MeS was diagnosed according to the International Diabetes Federation (IDF) guidelines (45), based on five components: waist circumference, blood pressure, fasting glucose, HDL cholesterol and triglycerides. Of these, three pathological values are needed for the diagnosis. Impaired fasting glucose (IFG: fasting plasma glucose ≥5.6 mmol/l) was diagnosed according to the IDF guidelines.
Power calculation
Statistical power calculations were based on the assumption that 25% of LIFE participants and 5% of REF participants had reached the target of losing 10% of their initial body weight after 12 months. Using Fisher’s exact test, it was calculated that with 59 LIFE participants and REF 59 participants, there was a 84% probability (power 84%, type II error 16%) to detect a significant difference between the groups at a two-sided 0.05 significance level (Alfa=0.05, type I error). The drop-out rate was expected to be 15%, and therefore we aimed to recruit 140 persons.
Statistical analysis
Linear regression models adjusted by baseline were used to analyze statistical differences in changes between the groups in body composition and cardiometabolic risk factors in assessments after 12 and 24 months. Fisher’s exact test was used to analyze differences in the proportions of successful weight losers (≥10% of body weight after 12 months) between the LIFE and REF groups. Generalized estimating equations with binary logistic regression using age, time and quadratic time as covariates were used to estimate between-group differences in proportions of participants with MeS or IFG in time (longitudinal data, three measurement points). Interaction of group and time, and group and quadratic time were added to the model to assess linear and non-linear between-group differences in time.
To further evaluate the metabolic risk and its changes, we calculated Z scores for MeS components (waist circumference, blood pressure, glucose, HDL cholesterol and triglycerides). Each component was log-transformed and standardized. The Z score of HDL cholesterol was multiplied by -1 to indicate higher metabolic risk with increasing value. The Z score of blood pressure was calculated as the average of systolic and diastolic blood pressure Z scores. Z scores from the five components were summed up as the metabolic risk score (46). The change in the metabolic risk Z score between the groups was modeled by linear regression using baseline value as a covariate. All results were considered to be statistically significant if P<0.05 or if 95% confidence intervals (95% CI) did not cross zero. All analyses were performed with SPSS software, version 21.0 (IBM Corp, Armonk, NY, USA).
Results
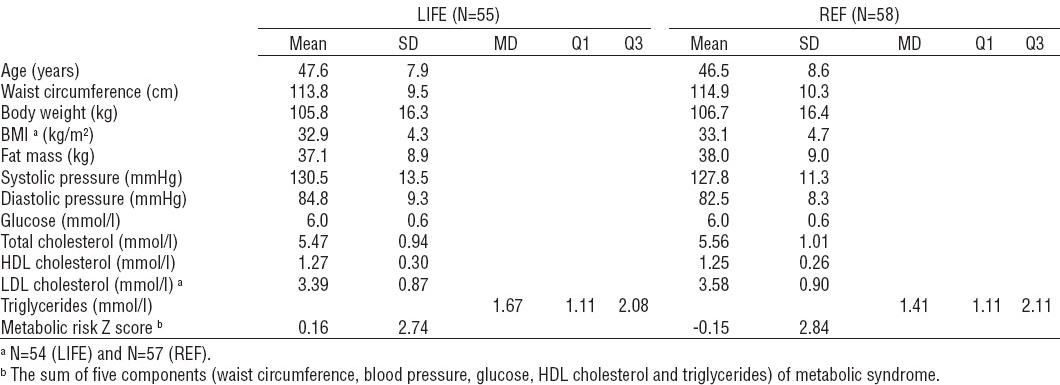
Eighty-three (74%) participants were truck drivers and thirty (26%) were bus drivers. The mean duration of truck or bus driving experience was 24.0 [standard deviation (SD) 14.9] years. Twenty-four (21%) participants used cigarettes or other tobacco products daily. Age, body composition, and components of MeS at baseline are presented in table 2. One fourth (25%, N=28) had a body mass index (BMI) of <30 kg/m2, about half (47%, N=53) of 30–34.9 kg/m2, and about one fourth (28%, N=32) of ≥35 kg/m2. Twenty-five (22%) participants reported use of medication for hypertension, twelve (11%) for dyslipidemia, and one (1%) for type-2 diabetes. One participant had coronary heart disease. More than two out of three (71%, N=80) had MeS at baseline.
Table 2
Characteristics of participants (N=113) at baseline in the lifestyle counseling (LIFE, N=55) group and reference (REF, N=58) group. [SD=standard deviation; MD=median; Q=quartile; BMI=body mass index; HDL=high-density lipoprotein; LDL=low-density lipoprotein]
Of the 113 randomized participants, 95 (84%) participated in 12-month and 80 (71%) in 24-month measurements (figure 1). One LIFE participant died before the 24-month measurements (the cerebrovascular cause of death was not related to the intervention). The mean participation of LIFE (N=47) in allocated monthly counseling sessions was 10.8 sessions (out of 11 allocated sessions) between months 1–11, resulting in participation rate of 98%. The corresponding results in the REF group (N=48) between months 12–15 were 3.97 sessions (out of 4 allocated sessions) and a 99% participation rate.
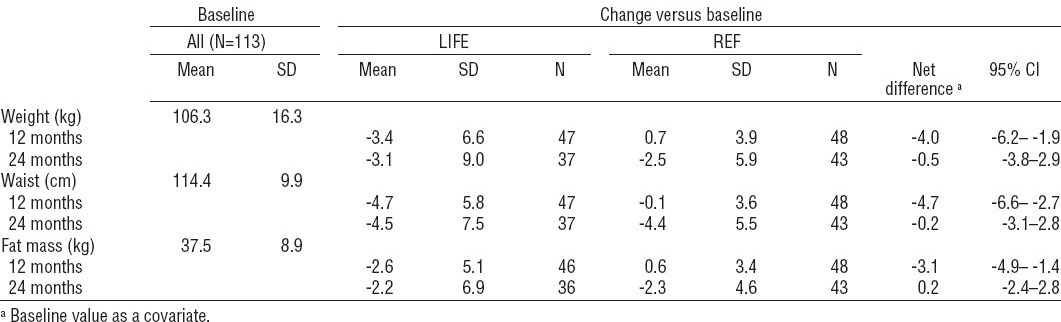
The mean body weight change (versus baseline) after 12 months was -3.4 (P=0.001, range -26.1–9.9) kg in LIFE (N=47) and 0.7 (P=0.214, range -9.5–12.5) kg in REF (N=48), the net difference being -4.0 kg (95% CI -6.2– -1.9) (table 3). The differences of changes in waist circumference and body fat were statistically significant in favor of the LIFE group after 12 months. The change in lean body mass did not differ between the LIFE and REF group (net difference -0.6 kg, 95% CI -1.4– -0.2). Six (13%) LIFE participants (N=47) reduced body weight by ≥10%, and another six (13%) lost 5–9.9% of initial body weight. In the REF group (N=48), the corresponding numbers were zero and three (6%) (P=0.01 and P=0.3 between the groups). Seven (15%) and fifteen (31%) LIFE and REF participants gained body weight by ≥2%, respectively (P=0.09 between the groups).
Table 3
Body weight, waist circumference and fat mass at baseline (N=113) and their changes in assessments after 12 and 24 months versus baseline and net differences of the changes between the lifestyle (LIFE) and reference (REF) group. [SD=standard deviation; N=number of participants; 95% CI=95% confidence interval]
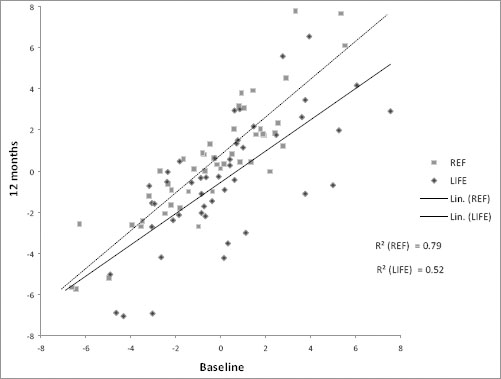
At baseline, 44 (80%) of 55 LIFE participants and 36 (62%) of 58 REF participants had MeS. After 12 months, the prevalence had decreased to 62% (29 of 47 LIFE) and to 60% (29 of 48 REF). The difference in the change of proportions between the groups was not statistically significant (P=0.34, logistic regression analysis). Metabolic risk Z score reduced more in the LIFE compared REF group (net difference -1.2 points, 95% CI -0.6– -2.0, linear regression) (figure 2).
Figure 2
Linear trend and R2 of metabolic risk Z score of the lifestyle counseling (LIFE, N=47) and the reference (REF, N=48) group between baseline and 12 months. [Lin =linear regression]
At baseline, 44 (80%) of 55 LIFE participants and 42 (72%) of 58 REF participants had IFG. After 12 months, the prevalence had decreased to 64% (30 of 47 LIFE) and increased to 77% (37 of 48 REF) (P=0.012 between the groups). Among all LIFE participants, the mean change in glucose concentration after 12 months was -0.15 mmol/l (SD 0.43) and 0.01 mmol/l (SD 0.43) among REF participants, the net difference being -0.15 mmol/l (95% CI -0.33– -0.02). After 12 months, the mean concentration of LIFE group HDL cholesterol increased by 0.02 mmol/l (SD 0.11) and decreased by 0.03 mmol/l (0.26) in the REF group (net difference 0.06 mmol/l, 95% CI 0.02–0.18). Also diastolic blood pressure tended to improve more in the LIFE than REF, group the net difference being -2.7 mmHg (95% CI -5.2–0.1) after 12 months. There were no statistically significant differences in the changes in total and LDL cholesterol, triglycerides, and systolic blood pressure between the groups after 12 months.
The waitlist REF group received 3 months of counseling, starting at 12 months from baseline. After 3 months, they lost 4.0 kg (SD 4.2) of body weight and 4.1 cm (SD 4.1) of waist circumference when compared to the 12-month assessment. Of 48 participants, 3 (6%) reduced body weight by ≥10% and 13 (28%) reduced body weight by 5–9.9% after the counseling.
After 24 months, there were no statistically significant differences in the changes of body weight, waist circumference and fat mass between the LIFE and REF group when compared to baseline (table 2). About one-tenth had reduced body weight by ≥10% from baseline, ie, four (11%) LIFE participants and three (7%) REF participants. The corresponding numbers with body weight loss of 5–9.9% were nine (24%) in the LIFE and 13 (30%) in the REF group. There were 11 (30%) participants in LIFE and 10 (23%) in REF who gained body weight by ≥2%.
After 24 months, the prevalence of MeS had decreased to 60% (22 of 37 LIFE) and 51% (22 of 43 REF). The between-group difference in the prevalence curves during 24 months (assessment at 0, 12, and 24 months from baseline) was not statistically significant (interaction between the group and quadratic time P=0.11). Neither was there a difference in change in metabolic risk Z scores between the groups after 24 months compared to baseline (net difference 0.1, 95% CI -0.8–1.0).
According to drop-out analysis, there were no differences in baseline characteristics (body composition, components of MeS or smoking) between completers and non-completers after 12 months (N=95 versus N=18) or 24 months (N=80 versus N=33). Neither were there differences after 12 months between completers and non-completers after 24 months (N=80 versus N=33).
Discussion
After 12 months of counseling, the mean body weight loss was 3.4 kg in the LIFE group and the net difference of body weight change was 4.0 kg favoring LIFE participants. The results are meaningful from a clinical and public health perspective. Thirteen percent in the LIFE and none in the REF group managed to reduce 10% of initial body weight. There was no difference between the groups in the change in the prevalence of MeS, but the metabolic risk Z score decreased more in the LIFE than REF group after 12 months. Waist circumference and HDL cholesterol improved more and the prevalence of IFG decreased more in the LIFE than REF group after 12 months. At the end of the study, after three months of counseling (months 12–15), REF participants had caught up with the weight loss that LIFE had achieved during 12 months. Thus there were no differences in body composition and metabolic risk factors between the groups after 24 months.
Recruitment of overweight long-distance drivers all over Finland was challenging and took 15 months. This was probably mostly due to their long and irregular working hours and because counseling sessions and measurements were implemented during participants’ leisure time. Thus we suppose that the most motivated and health conscious men participated. This is also reflected by the fact that only 21% of the participants were smokers, while the prevalence of regular smoking is around 27% among Finnish men at the same educational level (47). Internationally, smoking is more common among professional drivers than in other working populations (1, 9, 48).
We aimed at a 10% loss of initial body weight in ≥25% of the LIFE participants after 12 months. Weight loss of at least 5–10% has been found to be related to reduction in cardiovascular risk factors associated with obesity (49–51). In our study, the proportion of the LIFE participants to actually reach the 10% weight loss goal was around half of our assumption (13%). In the REF group, we had assumed 5% of the participants would reach the goal, but none succeeded. In lifestyle counseling interventions the proportion of participants reducing ≥10% of body weight is rarely reported, though this is a common goal in obesity treatment guidelines (51). However, when compared to previous lifestyle counseling interventions aiming at weight reduction, our result after 12 months (net effect -4.0 kg) is in the same magnitude and clinically relevant (52, 53).
According to meta-analyses on treatment of overweight and obese persons, the mean body weight loss in lifestyle interventions varied between 2.3–3.5 kilograms at follow-up for 1–2 years (52, 53). Previous health education interventions have achieved slight to moderate changes in drivers’ health behavior and body weight (25, 32, 54, 55), and only one of them has been a randomized intervention (25). Previous weight reduction studies concentrating only on males or shift workers are heterogenic and few. A randomized 6-month Dutch lifestyle counseling intervention resulted in a -2.2 kg (95% CI -3.1– -1.3) net difference at one year among 372 overweight male construction workers (33). Another randomized intervention by phone and email in a Dutch overweight working population (N=1386, of whom 67% were males) lead to a net weight loss of 1.5 kg (95% CI -2.2– -0.8) (by phone) and 0.6 kg (95% CI -1.3– -0.01) (by email) compared to control group after six months of lifestyle counseling (56). In an Australian randomized study, a three-month workplace-based weight loss program among 110 overweight male shift workers, led to a net difference of -4.4 kg (95% CI -2.6– -6.1) (34). Overall, in addition to more intensive and expensive individual counseling, work-site interventions (with different methods like group classes, leaflets, poster displays, work-shops, improved cafeteria food choices, and community events) have demonstrated promising results in obesity prevention and reducing cardiovascular disease risk (57, 58). However, workplace-bound approaches are not applicable to long-distance drivers.
The body weight regain in the LIFE group from 12 to 24 months was moderate (mean 0.5 kg, SD 4.8 kg). According to systematic reviews, about 50% of weight loss is maintained after one-year follow-up (59, 60). In a Finnish weight maintenance study among abdominally obese men, 37% of achieved body weight loss was maintained for two years after weight reduction by very-low-energy diet followed by exercise training (61).
The body weight decrease of 3.4 kg among LIFE participants after 12 months in the present study did not lead to a clear reduction in the prevalence of MeS. However, in the metabolic risk Z score the mean decrease of 1.2 points (95% CI -0.6– -2.0) was significant. Also fasting glucose and HDL cholesterol improved. According to several studies (62–64) it seems that even a modest body weight reduction (3.5–4.2 kg in 1–2 years) with the aid of diet and exercise is enough for reduction in cardiometabolic risk factors like insulin resistance, impaired glucose tolerance, dyslipidemia, and hypertension. The results of the present study are in line with these studies.
The present study shows that weight reduction with some improvement in cardiometabolic risk factors among long-distance truck and bus drivers is possible through lifestyle counseling, despite challenging working conditions. In addition to the weight loss achieved, an interesting finding was that the shorter three months of counseling in the REF group led to an almost equal body weight loss compared to the more intensive 12 months of counseling in the LIFE group. This may imply that in the short run, lifestyle changes are also achievable with less intensive counseling, which might be more applicable in occupational healthcare. Future studies are, however, needed to support this finding, since the effects of shorter counseling on long-term weight maintenance are not known.
Especially working hours, long absences from home, and dependence on road site food and rest services are substantial barriers to a healthy lifestyle of long-distance drivers. To improve the environment, resting and eating locations should serve healthier food, more showering facilities and possibilities to engage in exercise and rest. Professional drivers have shown interest in eating in a healthier way if there were options for these at the resting places (2, 11, 24). In many countries, including those in EU, Northern America, and some parts of Asia, hours-of-service rules are officially set to control the working and resting times of heavy vehicle professional drivers. In spite of that, economic aspects and international competition may lead to unrealistic delivery schedules and rule violations (65). In our study, we had no possibility to affect drivers’ working schedules or access to occupational healthcare.
Strengths and limits of the study
There are several strengths in the present study. First, our study is the first randomized controlled trial on lifestyle counseling in long-distance drivers. The counseling was planned to be intensive and individually tailored as the group was known to be hard to reach and maintain involvement. As long-distance drivers have no stable working place, participation in each counseling meeting was made as easy as possible for the participants as the counselors traveled to them. The counseling was structured and theory-based, which ensured homogeneity among the three counselors. The duration of the study with follow-up was rather long, namely, two years.
The most important limitation of the study is the number of participants, which makes the study underpowered. We lacked 23 participants from the target of 118 at 12-month measurements, meaning a gap of 19%. As the recruitment was countrywide, the less-than-optimal number of participating volunteers most probably reflects challenging working hours or lack of interest in health issues. However, the participant drop-out (16% after 12 months and 29% after 24 months) was rather low compared to other weight loss studies (37). This probably reflects appreciation of free and easy-to-reach counseling sessions and the attention and advice given by health professionals.



