Occupational accidents are a global problem. Although no effective recording systems for occupational accidents exist at the global level, it is estimated that more than 260 million occupational accidents take place each year (1, 2). A number of different factors, both personal and occupational, have been associated with an increased risk of work-related accidents. Young age, alcohol, smoking, shift work, and overweight are all factors that have been shown to correlate with an increased risk (3–8).
Sleep disturbances are very common in the general population, and it has been estimated that as many as 10–15% of adults suffer from chronic insomnia (9, 10) and that it is more common among women (9, 11–13). Although the exact pathophysiology is yet to be determined, it has been shown that certain precipitating factors contribute to the occurrence of insomnia. These factors include psychiatric disorder, shift work, acute and chronic illnesses and specific sleep disorders, such as obstructive sleep apnea syndrome and restless legs syndrome (14). As primary insomnia only accounts for about 12–15% of patients with chronic insomnia (15), the vast majority of patients suffer from a secondary insomnia that is caused by factors that can potentially be affected or treated. Following the high prevalence of insomnia, the potential association between sleep disturbances and different types of accident has attracted interest due to the possible socioeconomic gain that may be generated by preventive measures. In the US alone, population projections estimate a cost of >$30 billion a year (16) for sleep-related occupational accidents. An Australian study has reported equivalent figures (17).
Based on previous research, it is well known that subjects with obstructive sleep apnea run an increased risk of traffic accidents (18–20), and we have previously reported that symptoms of obstructive sleep apnea syndrome (OSAS) also are an independent risk factor for occupational accidents among men (21). However, our knowledge of the impact of OSAS symptoms on occupational accidents among women as well as the impact of other sleep disturbances, such as insomnia, on accident risk is still limited (22, 23). In addition, most studies within this field have been small scale (24–26) or focused on specific professional groups (27–32).
Some cross-sectional studies have reported that occupational accidents are related to sleep disturbances (33, 34). The few prospective studies within this field are limited by not being population based (35) or only including fatal accidents (36). Furthermore, to our knowledge, no studies have previously focused on sleep disturbances and work injuries solely among women.
This population-based cohort study was performed to assess the association between sleep disturbances and the risk of occupational accidents among women. To achieve this, a population-based cohort study was performed where sleep disturbances both at baseline and at follow-up were taken into account.
Methods
Population
In 2000, the population-based study “Sleep and Health in Women” (SHE-study) was initiated. A questionnaire was sent to randomly selected women aged ≥20 years in the Municipality of Uppsala, Sweden. With a response rate of 71.6%, 7051 completed the baseline questionnaire (37–39). For those 20–67 years, the response rate was 73.1%. Ten years after the baseline questionnaire, 596 women had died or moved abroad. A follow-up questionnaire was sent to the remaining women, of whom 5193 responded, yielding a response rate of 80.5%.
Of those who responded to both questionnaires, subjects aged >67 years in 2000 were excluded from this study, as most Swedish citizens have retired at that age. Of the remainder, subjects who reported working ≥10 hours/week for ≥1 year during the follow-up period were included in the present analysis.
Questionnaires
The baseline questionnaire consisted of 109 questions and included questions about sleep disturbances, tobacco use, physical activity during leisure time, alcohol consumption, height, and weight. The follow-up questionnaire had identical questions on sleep disturbances and also included questions on occupation and occupational accidents during the follow-up period.
In the calculations, data on body mass index (BMI), age, smoking and alcohol dependency were retrieved from the 2000 questionnaire, work-related information was retrieved from the 2010 questionnaire, while information on sleep disturbances was analyzed from both questionnaires.
The questions regarding sleep disturbances were adopted from the Uppsala Sleep Inventory (USI) (40), which has previously been used in several epidemiological studies (41, 42). In both the baseline and follow-up questionnaires, questions on sleep disturbances were given five alternative answers. The participants were asked to assess the severity of their problems with difficulty initiating sleep (DIS), early morning awakening (EMA) and difficulty maintaining sleep (DMS) using a 5-point scale: none (1), small (2), moderate (3), severe (4), and very severe (5). Scores of 4 or 5 classified the subject as suffering from DIS, EMA, or DMS respectively, ie, having insomnia symptoms. The response options regarding the frequency of loud and disturbing snoring were: never (1), rarely (2), sometimes (3), often (4), and very often (5). The question “How often do you fall asleep involuntarily for a short period during the day, for example when there is a pause at work” was used to assess excessive daytime sleepiness (EDS) using the same response options as snoring. Subjects scoring 3–5 on both the snoring and EDS questions were categorized as having symptoms of obstructive sleep apnea syndrome (OSAS). A similar definition was used in a previous study on men (21). Based on their answers regarding symptoms of insomnia and OSAS in 2000 and 2010, the participants were divided into four groups: (i) no disturbances during the period, (ii) disturbances in 2000 but not in 2010, (iii) in 2010 but not in 2000, and (iv) persistent disturbances if reporting disturbances in both 2000 and 2010.
BMI was calculated as weight in kg divided by height in meters squared. The self-reported weight and height from the baseline questionnaire were used.
Subjects were categorized into three groups depending on their physical activity during leisure time: low, medium, or high level. A low level of physical activity was assigned to subjects spending most of their leisure time in sedentary activities such as reading or watching television. The medium group was assigned if subjects reported physical activity such as cycling or walking for ≥4 hours a week. The group with a high level of physical activity comprised subjects participating in activities such as swimming or running for ≥3 hours a week or even more vigorous activities on a weekly basis (39, 43).
Subjects were categorized as “smokers” or “non-smokers” based on their answers regarding tobacco use. The group of “non-smokers” included subjects who had never smoked or had quit smoking >6 months before answering the baseline questionnaire (37).
The CAGE questionnaire was used to categorize subjects as alcohol or non-alcohol dependent. Subjects were defined as being alcohol dependent if they had ≥2 affirmative answers to the CAGE questions in 2000 (“have you tried to cut down on your drinking?”, “have people annoyed you by criticizing your drinking?”, “have you ever felt guilty about your drinking?”, have you ever had a drink first thing in the morning after drinking, as an eye-opener?”) (44, 45).
Occupations and occupational accidents
In the follow-up questionnaire, participants were asked how many years they had been at work during the last ten years and whether they worked full- or part- time. Part-time workers were further asked how many hours/week they worked. They were also asked how many months they had worked in shifts or at night and how many months they had been exposed to noise, solvents, exhaust fumes, and whole-body vibrations.
Based on the responses to the question on occupation during the 10-year period, all participants were categorized as blue- or white-collar using the Swedish classification of occupation (SSYK), which is based on the International Standard Classification of Occupations 1988 (ISCO-88).
In the 2010 questionnaire, the subjects were asked to state whether they had been involved in an occupational accident between 1 January 2000 and the time of the questionnaire in 2010. They were asked to also include mild accidents not leading to sick leave. Information on occupational accidents with sick leave during the same period was obtained from the Occupational Injury Statistics Division (ISA) of the Swedish National Board of Occupational Safety and Health. This is a national register where the Injury Statistics Division compiles statistics on occupational accidents, including commuting accidents, and diseases in Sweden. Employer reporting of serious occupational accidents is mandatory. The injury report form includes information on occupation, the enterprise, working conditions, circumstances of the injury, and number of days of absence from work. Output data from the register is available on the individual level.
The informed consent of all participants was obtained and the Ethics Committee at the Medical Faculty at Uppsala University approved the study.
Statistical analysis
Statistical analyses were performed using Stata 10.1 (StataCorp LP, College Station, TX, USA). The chi-square test was used to analyze subgroups of women in the baseline and follow-up data. The unpaired t-test was used for comparisons of continuous values. Significant variables from the univariate computations were further analyzed with multiple logistic regression analyses adjusting for age, smoking, number of years worked, alcohol dependency, BMI, blue-collar worker, night work, and physical activity during leisure time. Shift work was not added as a confounder due to covariance with night work (r=0.314, P<0.001). The results are presented as adjusted odds ratios (ORadj) with 95% confidence intervals (95% CI). P-values of <0.05 were considered statistically significant.
Results
Of the total of 5193 women who had answered both questionnaires, 378 women were excluded from the study population because they were >67 years old and another 495 due to not having worked during the follow-up period. As a result, the total study population consisted of 4320 women.
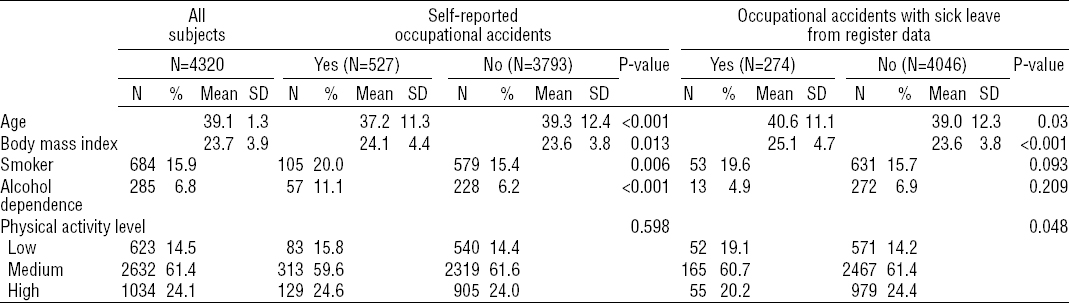
Of the responders, 527 (12.2%) subjects reported ≥1 occupational accident during the 10-year follow-up period. During the same period, 274 accidents with sick leave were reported to the ISA. Only 50% of the accidents with sick leave reported to the ISA-register were also recollected by the subjects in the questionnaire. Of the total number of occupational accidents reported in the questionnaire, 26.0% were also reported to the ISA-register as accidents with sick leave. The women who reported an occupational accident in the questionnaire were younger, had a higher BMI, and were more often smokers and dependent on alcohol. The level of physical activity did not differ significantly between the groups. Women who had been involved in register-reported accident were slightly older, had a higher BMI and also had a lower level of physical activity, while there was no significant difference for smoking or alcohol dependence (table 1).
Table 1
Characteristics of the cohort at baseline (2000), in the whole study group and by involvement in occupational accidents. [SD=standard deviation.]
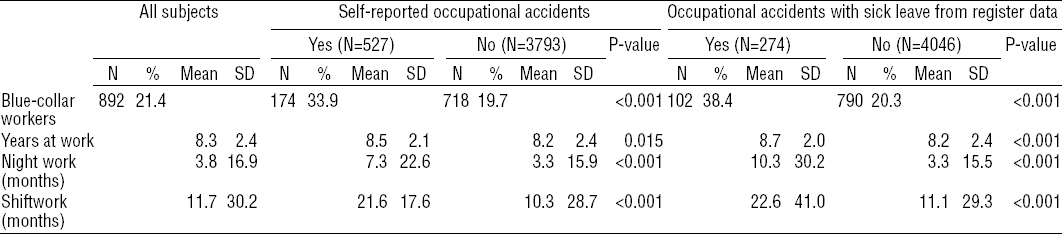
Blue-collar workers were considerably more common in the group with self-reported occupational accidents. The women involved in self-reported occupational accidents had generally been working for a somewhat longer period during the 10 years and both night work and shiftwork were more common in this group. The same relationships were shown for register-reported accidents with sick leave (table 2).
Table 2
Work related characteristics of the study population during the 10-year period, in the whole study group and by involvement in occupational accidents. [SD=standard deviation.]
The 892 blue-collar workers were older than the 3267 white-collar workers [40.3 years (SD 12.2) versus 38.7 years (SD 12.1), P=0.0004] and had a slightly higher BMI [24.7 kg/m2 (SD 4.5) versus 23.4 kg/m2 (SD 3.7), P<0.001]. Smoking was considerably more common among the blue-collar workers (26.3% versus 13.1%, P<0.001), while there was no significant difference in the prevalence of alcohol dependency (6.3% versus 7.1%, P=0.428). Furthermore, the blue-collar workers had generally been working for longer periods on shift and night work compared with the white-collar workers [shiftwork: 37.1 months (SD 43.0) versus 20.3 months (SD 34.4), P<0.001; night work: 23.0 month (SD 38.0) versus 10.6 months (SD 25.0), P<0.001].
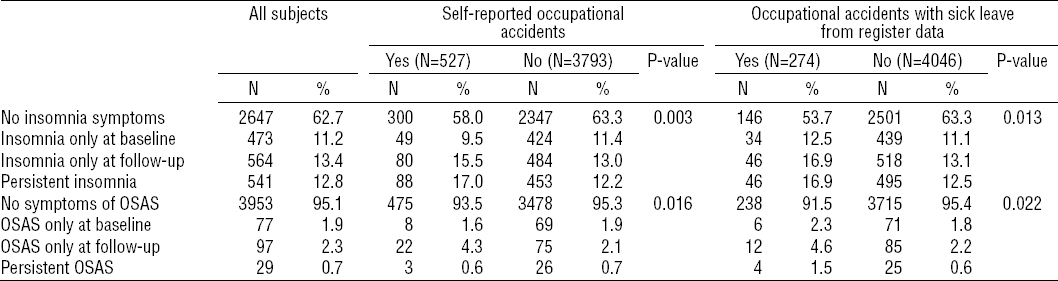
In the univariate analysis, persistent insomnia symptoms were related to the occurrence of both self-reported and register-reported occupational accidents. Symptoms of OSAS at the follow-up were more common among women with either self- or register-reported occupational accidents. Although the number of participants with persistent symptoms of OSAS was low, they were somewhat overrepresented in the group with register-reported accidents (table 3).
Table 3
Prevalence of sleep disturbances at baseline and follow-up. Woman who had been in ≥1 occupational accident, self-reported or from register data, during the 10-year period compared with women with no reported occupational accidents. [OSAS=obstructive sleep apnea syndrome.]
A non-respondent analysis was made comparing the 1262 women who only answered the questionnaire in 2000 with the women who answered both questionnaires. The non-respondents were (i) found to be younger [39.2 years (SD 13.6) versus 40.7 years (SD 13.1), P<0.001], (ii) tended to have a slightly higher BMI [24.1 kg/m2 (SD 4.2) versus 23.9 kg/m2 (SD 4.0), P=0.057] and (iii) smokers considerably more frequently (22.1% versus 15.8%, P<0.0001). However, no significant difference in alcohol dependency was found. There was no significant difference in the prevalence of insomnia between the groups while non-responders had reported OSAS symptoms more often (4.9% versus 3.1%, P=0.002).
Multivariate analyses
Subjects with persistent insomnia symptoms had an ORadj of 1.5 (95% CI 1.2–2.0) for being involved in an self-reported occupational accident after adjustment for white-/blue-collar worker, age, BMI, alcohol dependency, years at work, night work, smoking, and physical activity. Participants reporting symptoms of insomnia only at baseline or the follow-up did not have a significantly increased risk of self-reported occupational accidents. Furthermore, after adjusting for confounders, persistent symptoms of OSAS did not significantly influence the risk of being involved in a self-reported occupational accident (table 4).
Table 4
Results from multiple logistic regression analyses of risk of involvement in an occupational accident by reported sleep disturbances at baseline and follow-up. a [OSAS=obstructive sleep apnea syndrome; ORadj=adjusted odds ratio; 95% CI= 95% confidence interval.]
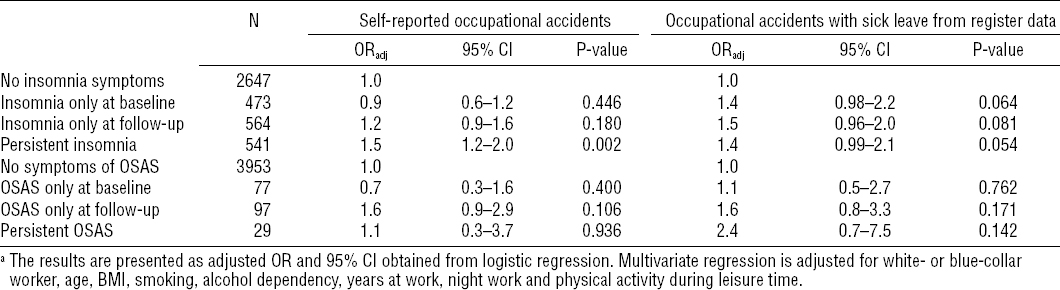
Analyses were also performed from register-reported data on occupational accidents with sick leave. After adjustment for the same variables as above, there was a trend towards a higher risk of occupational accidents in subjects with insomnia symptoms either at baseline (ORadj 1.4, 95% CI 0.98–2.2), at follow-up (ORadj 1.5, 95% CI 0.96–2.0) or persistent insomnia (ORadj 0.99–2.1), but none of the groups reached statistical significance. Symptoms of OSAS did not significantly influence the risk of being involved in a self-reported or register-reported occupational accident.
Discussion
Our main finding was that, among women, persistent insomnia symptoms are an independent risk factor for self-reported occupational accidents, including those not leading to sick leave. Women with insomnia symptoms also had more occupational accidents with sick leave reported to the national register, but after adjusting for confounders the association did not reach statistical significance.
As far as we know, only two prospective studies of sleep disturbances and occupational accidents have previously been conducted. Åkerstedt et al (36) reported an association between disturbed sleep and fatal occupational accidents in a large-scale study. The relative risk was much higher among men compared with women (OR 2.3, 95% CI 1.56–3.38), but no separate analysis of the absolute risk for women was reported. In the cited study, disturbed sleep was defined as responding “Yes” to the question “Have you had difficulty sleeping during the last two weeks”. Salminen et al (35) conducted a large-scale prospective study among public sector workers and found that difficulty initiating sleep was a predictor of occupational accidents with sick leave among women during the following year (OR 1.69, 95% CI 1.26–2.26). However, in contrast to the present study, changes in the occurrence of sleep disturbance during the follow-up period were not taken into account, making the role of the persistence of the sleep disturbance unclear.
An association between sleep disturbance and less severe occupational accidents has been reported in several cross-sectional studies. Nakata et al (27) included minor injuries in their cross-sectional study and found that insomnia symptoms were associated with occupational injuries in both genders. Moreover, in Simpson et al’s community-based, cross-sectional study, an increased number of minor injuries at work were reported among persons with sleep problems (46). Industrial work-related accidents were more common among those with insomnia than good sleepers (26) and similar relationships between sleep and accidents have been found among veterinarians (32), construction workers (29), and railway workers (30, 31). Among white-collar workers, poor sleep was not linked to workplace accidents (28), consistent with our finding that being a blue-collar worker is a risk factor for accidents. A large-scale Canadian cross-sectional, population-based study reported an increased number of work-related accidents serious enough to limit normal activities in both men and women reporting poor sleep “most of the time” (33). The same study showed that, in the case of women, there was also an association between “trouble sleeping sometimes” and work injury (ORadj 1.26, 95% CI 1.03–1.54). An international, cross-sectional study reported that, among patients consulting participating physicians about sleep disorders, those fulfilling the criteria for insomnia reported a large number of occupational accidents related to sleepiness (34). In an earlier study, Leger et al (24) did not observe a significant difference between insomniacs and non-insomniacs regarding the occurrence of occupational accidents, probably due to the small sample size (N=369 matched pairs of workers with insomnia).
There was no significant association between OSAS symptoms and occupational accidents. This is in contrast to a previous study among men, where the occurrence of symptoms of OSAS (snoring and excessive daytime sleepiness) resulted in an increased long-term risk of occupational accidents (ORadj 2.2, 95% CI 1.3–3.8) (21). Even though a gender difference cannot be ruled out, the discrepancy can also be due to a lower power of the present study. In the male cohort, both the prevalence of OSAS symptoms (5.4%) and incidence of register-reported occupational accidents (12.3%) was higher. Furthermore, drawing parallels to motor vehicle accidents, several case-control studies using questionnaire-based classification of obstructive sleep apnea syndrome, have failed to show a significantly increased risk of accidents (47, 48). In contrast, in studies exploring the risk of motor vehicle crash among subjects with obstructive sleep apnea syndrome, as defined by objective measurement of sleep through polysomnography, an increased risk of motor vehicle accident has indeed been found (49). The lack of objective measures in the present study may hence have introduced misclassification of the subjects regarding sleep apnea syndrome. A subsample of 400 women from the population also performed a whole-night polysomnography (50) and the validity of the combination of snoring and EDS, as defined in the present study, to identify subjects with an apnea-hypopnea index of >15 was analyzed. When compared with the group with neither snoring nor EDS, the sensitivity was 85% while the specificity was only 37%. The specificity of the reference variable “no snoring or EDS” to identify subjects without sleep apnea was 91%.
Despite differences in study design, the finding in the present study of an association between insomnia symptoms and occupational accidents is in accordance with the results of previous studies. It is reasonable to assume that this relationship is due to a subsequent lack of concentration and sufficient alertness at work because of disrupted sleep. The lack of a significant association between insomnia symptoms and the register-reported occupational accidents with sick leave among women could be due to more low-risk work and the possible avoidance of high risk-situations.
Hypnotics with long half-lives, such as those used for the treatment of insomnia, can be indicated as a possible culprit in accidents among insomniacs. Widera addresses this issue in a review article of sleep medication and hip fractures among the elderly and concludes that current research in the field is unable to show whether it is in fact the underlying insomnia or the treatment of the insomnia that is at fault (51). Unfortunately, we have no information on the use of hypnotics during the 10-year period in the present study population. However, in the cross-sectional EQUINOX study, subjects who had received treatment in the previous six months were excluded from the study and an association between insomnia and occupational accidents was still found (34). Furthermore, Kling et al did not find a significant association between taking sleeping pills and the occurrence of work accidents (33).
Defining insomnia in large-scale epidemiological study is difficult and wide range of different questionnaires exists. The USI-questionnaire used here is similar to the first three questions in the Insomnia Severity Index (52) although the timeframe is not defined in the USI. It could be criticized that it is a questionnaire based on severity and not frequency of symptoms. However, Mallon et al (42) reported a good correlation between the USI and the Basic Nordic Sleep Questionnaire (BNSQ) that is a frequency-based questionnaire covering the last 3 months on a 5-point scale (ranging from 1=never or less than once a month to 5=daily or almost daily). In Mallon et al’s study, 86.3% of the subjects who reported having severe or very severe problems with DIS in the USI questionnaire also reported DIS at least 3–5 times a week during the last three months in the BSNQ questionnaire. Regarding DMS, 94% of subjects reporting severe or very severe problems in the USI also scored 4 or 5 on the BNSQ. Thus, there is a strong correlation between the severity-based USI-questions and frequency-based BNSQ for those subjects with highest scores. Furthermore, the DIS question from the USI has been compared to polysomnography (53) showing good correlations between the degree of DIS in the USI questionnaire and sleep latency measured by polysomnography (r=0.34, P=0.0002).
The strengths of our study are that it is one of the few prospective studies on the subject, that it is population-based with a large cohort with a high response rate, and the use of both self-reported and data from a national register. It is reasonable to assume that there is more incentive to report more serious accidents that have a higher chance of being claimed as work-related accidents with financial compensation, meaning that mild and minor accidents may be not included in the ISA to the same extent. The Swedish National Board of Occupational Safety and Health have conducted a comparative study between the statistics in the national register and data from a survey study administrated by the governmental agency Statistics Sweden. The comparative study concludes that only 40.8% of occupational accidents without sick leave were reported to the register while 54.8% of the accidents with sick leave and 53.9% of commuting accidents are reported to the register (54). Outcomes with higher degree of severity will often be more specific, and more specific outcomes (if the association is true) often lead to higher risk estimates (55, 56). In this study, we see higher risk estimates when using ÍSA, but without statistical significance. However, due to low power we cannot exclude the possibility of an association between insomnia symptoms and increased risk of register-reported occupational accidents.
There are also other limitations that should be considered when interpreting the results. For subjects who only reported symptoms at baseline or follow-up, we have no information on the timeline for the changes. They most probably constitute a mixture of subjects displaying the respective symptom most of the time, for only a short period, and are also an effect of regression to the mean. The fact that only 50% of the accidents with sick leave were recollected by the subjects illustrates that there is an important recall bias that might weaken the results. The association between persistent insomnia symptoms and occupational accidents reported here might hence be an underestimation. Another limitation is that the cause of the insomnia symptoms are not investigated; potentially treatable psychiatric or somatic disorders may be the indirect cause of the occupational accidents by causing the sleep disturbances. The number of years a subject was at risk for occupational accident was based on the numbers of years the subject stated having worked during the follow-up period, a limitation being that part-time work was not taken into account. Furthermore, a reversed causality may occur in that occupational accidents may increase the risk of developing disturbed sleep; in particular the sleep disturbances reported at follow up may be effects of reversed causality. Finally, work environment exposure was not considered and hence residual confounding may exist.
In conclusion, persistent insomnia symptoms were associated with an increased risk of self-reported occupational accidents, while no significant association was found with occupational accidents with sick leave reported to government register.



