Many employees report problems with poor sleep quality, partial sleep loss, elevated daytime sleepiness and increased stress levels during workdays (1–5). Possible reasons for these complaints may be high workload combined with insufficient time for recovery after work (6, 7). According to the Effort–Recovery Model (8), if recovery is compromised, a development of persistent load reactions might occur that could contribute to chronic conditions such as hypertension, increased heart rate, chronic fatigue, and sleep problems (5, 9–12).
Shortening of work hours is not only a way of diminishing workload, it may also be one way of ameliorating recovery opportunities and enhanced sleep. However, there is an apparent scarcity of longitudinal research and intervention studies in this area. To our knowledge, only one intervention study has evaluated reduced weekly worktime with retained salary and its consequences for perceived stress, sleep, and sleepiness over time (13), where a slight improvement in sleep quality and mental fatigue was observed when work hours were reduced from 8 to 6 hours/day. Moreover, studies on worktime reduction have shown that shorter workdays lead to a reduction of job exhaustion (14) and have a positive impact on work–family interaction (13, 15). The mechanisms behind the beneficial effects of worktime reduction are believed to be extended time for recovery, additional time spent on beneficial health-related behaviors such as exercise, and less conflict between work and other domains in life (13, 15–17).
In earlier studies on worktime reduction and its effects on sleep and stress (13, 14), there has been no randomization and the samples have been small. Thus, there is a need for randomized controlled interventions, with large samples and many workplaces together with long-term follow-up measurements to evaluate the stability of the effects. The present study aims to evaluate an intervention of a 25% reduction of weekly work hours with retained salary through a group randomized trial. Drawing on the Effort–Recovery Model (8), it was hypothesized that worktime reduction would result in longer sleep duration, better subjective sleep quality, less sleepiness, and lower levels of perceived stress, including worries and stress at bedtime on workdays. The study also investigated whether reduced weekly work hours would promote good sleep and lower sleepiness and perceived stress during days off. Because women working fulltime often have a double load of both paid and unpaid work (eg, in the household; 18, 19), the study also explored if women would benefit more than men from reduced weekly work hours. Age, having children living at home, as well as having poorer sleep quality and higher levels of bedtime worries at baseline were also tested as subgroup factors.
Methods
Design and procedure
Data were collected within a longitudinal controlled intervention study evaluating a 25% reduction of weekly work hours and its impact on health. Commissioned by the Government, the Swedish National Institute of Working Life carried out the project in 2005–2006 (20). In the intervention group, participants retained their salaries and the workplaces obtained funding for recruiting more staff in order to avoid an increase in workload for the employees. Participants signed legally binding documents agreeing not to engage in any other paid work in their free time during the intervention period. The Stockholm regional ethical review board approved the study (reference number: 04-1059/5), and all participants gave their written consent.
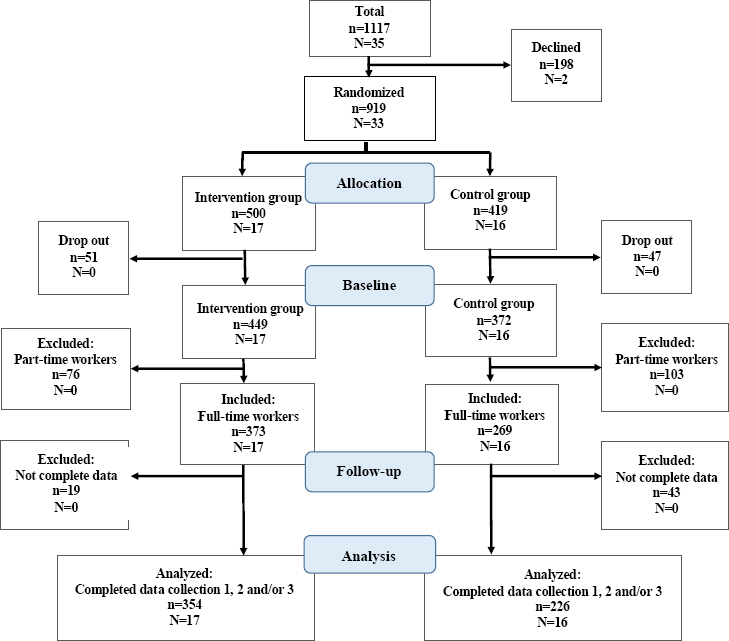
Randomization was made at the workplace level, however balanced on three variables: geographic location, type of work, and gender distribution. In total, 33 workplaces were included and randomized (17 to the intervention group and 16 to the control group). However, one of the 33 units (3%), could only participate if it belonged to the control group due to problems recruiting new staff.
Data collection
Data were collected at baseline (1–2 months before the intervention; February–May 2005) and then approximately 9 and 18 months after the start of the intervention (in January/February and October/November 2006). At each data collection, participants completed a questionnaire including questions on demographic data and work environment exposure, evaluated through job demands (1=low demands to 4=high demands) and job control (1=low control to 4=high control) (21). Participants also completed a sleep and wake diary during one week for each measurement period.
During data collections, each morning, participants were asked to answer questions in the Karolinska Sleep Diary (KSD; 22) on bedtime (hours), time of awakening (hours), and sleep latency (hours), as from which a measure of sleep duration was derived for each day. Furthermore, the diary contained a question of worry and stress at bedtime (1=a lot of worry and stress to 5=no worry or stress) and questions of subjective sleep quality (SSQ), which was based on an index using four questions; “Did you have difficulties falling asleep?” (1=very much to 5=not at all), “How did you sleep?” (1=very poorly to 5=very well), “Did you have a restless sleep?” (1=very much to 5=not at all), and “Did you wake up very early without being able to fall asleep?” (1=very much too early to 5=no). The index, calculated as a mean of the four items (Cronbach’s alpha=0.76–0.82 on workdays and 0.74–0.79 on days off) has previously been validated against physiological sleep parameters and showed significant correlations with objective measures of sleep continuity (23).
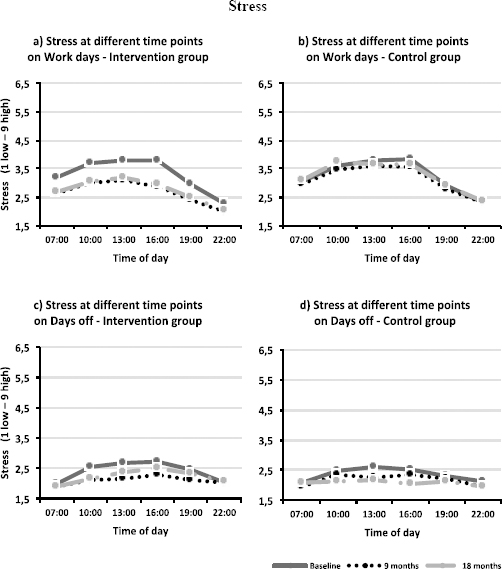
The wake diary was completed during the day or before going to bed and contained questions of workhours (start and finishing times), sleepiness, and perceived stress. Sleepiness was measured at six time points per day (07:00, 10:00, 13:00, 16:00, 19:00, and 22:00 hours) through the Karolinska Sleepiness Scale (KSS; 24, 25); a 9-graded scale with values ranging from 1=very alert to 9=very sleepy, fighting sleep. At the same occasions, perceived stress (26) was rated from 1=very low stress to 9=very high stress.
Study sample
Initially, 33 workplaces with 919 employees within the public sector agreed to participate; 98 employees dropped out after randomization. The main reasons for this were changed job/workplace (N=29), parental leave (N=14), and long-term sickness absence (N=14). Out of the remaining 821 employees, 580 were included in the present study (intervention group: N=354; control group: N=226). They met the inclusion criteria of working full-time, having reduced the worktime by 25% according to the employers’ time recording data over 14 months (intervention group) and having participated in the data collection at baseline as well as the 9-month follow-up and/or the 18-month follow-up (see figure 1). One paper on a subsample of these data has recently been published in 2015 (16), but it was restricted to the first and the last measurement period in a subgroup of social workers.
Participants worked in four different working sectors: social services (managers, social workers or social assistants; N=152, eg, from 8 workplaces), technical services (eg, administrators, airport workers or parking guards; N=214 from 9 workplaces), care and welfare (eg, caregivers at preschools, hospitals or retirement homes; N=143 from 11 workplaces), and call center (eg, managers or administrators; N=70 from 5 workplaces). Almost one third (29%) were shift workers, most of the participants were women (76%) and the age range was 20–65 years [mean 44.6, standard deviation (SD) 10.6 years]. About half of the participants reported they had children living at home. Chi2 tests indicated no differences between groups in background variables presented in table 1 (P=0.062<0.715), except for the number of shift-workers (P=0.000) and educational level (P=0.002). T-tests showed no age difference between groups (P=0.531) but significant differences in level of job control (P=0.037, table 2). Educational level, working shift or not, as well as job control were consequently added as covariates in the statistical models.
Table 1
Descriptive data at baseline.
| Intervention group | Control group | Total | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| N | % | N | % | N | % | |
| Total | 354 | 100 | 226 | 100 | 580 | 100 |
| Gender | ||||||
| Women | 275 | 78 | 166 | 74 | 441 | 76 |
| Men | 79 | 22 | 60 | 27 | 139 | 24 |
| Educational level a | ||||||
| Elementary school | 34 | 10 | 40 | 18 | 74 | 13 |
| Upper-secondary school | 165 | 47 | 111 | 49 | 276 | 48 |
| University courses | 30 | 8 | 15 | 7 | 45 | 8 |
| University exam | 124 | 35 | 59 | 26 | 183 | 32 |
| Having children living at home | 174 | 49 | 111 | 49 | 285 | 49 |
| Working area b | ||||||
| Social services | 102 | 29 | 50 | 22 | 152 | 26 |
| Technical services | 118 | 33 | 96 | 43 | 214 | 37 |
| Care and welfare | 83 | 24 | 60 | 27 | 143 | 25 |
| Call center | 50 | 14 | 20 | 9 | 70 | 12 |
| Shift workers | 86 | 24 | 82 | 36 | 168 | 29 |
Table 2
Mean values and standard deviations (SD) of descriptive data at baseline.
Attrition analysis
A total of 62 participants (19 in intervention group, 43 in control group) did not participate in the data collection during follow-up measurements and were not included in the statistical analyses. No significant differences (through t-test) were observed between those who completed and those who did not complete participation, except for sleep duration on workdays, where completers reported 18 minutes shorter sleep on average as compared to non-completers (t=2.48, P=0.013). In terms of age and gender, the analysis showed that men were more prone to drop out as compared to women (t=2.53, P=0.012) and non-completers were slightly younger than those who completed the study (t=-2.75, P=0.006).
Statistical analysis
A mean value for workdays and days off, respectively, was computed for the outcome variables of the sleep and wake diary. In order to account for the nested structure of data, a value of the intraclass correlation (ICC) of workplace was calculated for each variable at baseline. Although the values of ICC were low (0.005–0.065), they were taken into consideration in the statistical analyses, which were based on multilevel mixed models including random effects for workplace at level 2.
The model included the outcome variable and the fixed effects of the between-group factor “group” (intervention versus control; level 2), the within-group factor “time” (baseline, 9 and 18 months, respectively; level 1) and the group×time interaction. The model was fitted by modeling the autocorrelation. Sensitivity analyses, (eg, excluding the workplace that was not randomized) were made in order to rule out possible bias due to the randomization procedure.
The subgroup analysis of gender was made by adding a second between-group factor (gender) into the model, resulting in several two-way interactions and one three-way interaction of group×time×gender. Additional subgroup analyses of age, having children living at home, and baseline levels of sleep quality and worries and stress at bedtime (weekly mean value dichotomized by median split) were also performed. For the analysis of sleepiness and perceived stress at different time points of the day, an additional within-group factor was entered (“time of day”), resulting in a three-way interaction of group×time×time of day together with several two-way interactions. A two-tailed alpha-level of 0.05 was used when testing for statistical significance. Effect sizes were calculated through Cohen’s f2 evaluated on the threshold levels of 0.02 (small), 0.15 (medium), and 0.35 (large) (27, 28). Descriptives, Cronbach’s alpha, t-tests, Chi2 tests and analyses of variance were carried out in SPSS 21 (SPSS Institute, Cary, NC; USA), whereas multilevel analyses and calculation of ICC and Cohens f2 were made in STATA 14 (StataCorp, College Station, TX, USA).
Results
Implementation of the intervention
Although one criterion for being included in the study was having implemented the 25% worktime reduction according to the employers’ time recording data over 14 months, self-reported hours worked per day (including breaks and reported overtime), and the number of days worked per measurement week have been computed (see table 3). The intervention group (N=354) showed a significant reduction of work hours; on average 1:40 hours/day including breaks (corresponding to a reduction of 20% between the first and last data collection period), as compared to the control group which showed a reduction of 8 minutes/day, resulting in a significant group×time interaction (F=59.88, P<0.0001, f2=0.17). The majority of the participants in both groups worked five days on average per week during all three data collection periods, however, the intervention group decreased the number of worked days over time to a greater extent than did the control group (F=6.44; P=0.002; f2=0.01).
Table 3
Hours of work per day, hours of reported overtime and number of days worked per week, presented by group at the three different measurement weeks. [hh:mm=hours and minutes; SD=standard deviation]
| Hours (hh:mm) worked per day a | Over time (hh:mm) per week | Days worked per week | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||||
| Intervention | Control | Intervention | Control | Intervention | Control | |||||||
|
|
|
|
|
|
|
|||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Baseline | 8:17 | 0:54 | 8:32 | 1:00 | 0:39 | 1:42 | 1:11 | 3:00 | 4.80 | 0.7 | 4.64 | 1.2 |
| 9 months | 6:38 | 0:54 | 8:26 | 1:06 | 0:28 | 1:12 | 0:48 | 1:42 | 4.55 | 1.1 | 4.85 | 0.9 |
| 18 months | 6:37 | 0:54 | 8:25 | 1:00 | 0:41 | 1:42 | 0:50 | 1:48 | 4.52 | 1.1 | 4.34 | 1.3 |
Intervention effects on sleep, sleepiness and stress
Levels of SSQ, sleep duration, sleepiness, and perceived stress on workdays and days off did not differ significantly between the groups at baseline (through t-test; P=0.055<0.905). Data for the outcome variables and the results of the interactions between group and time are presented in table 4. On workdays, the intervention group displayed improved SSQ, 23 minutes extended sleep duration (over the whole period of 18 months), decreased sleepiness and perceived stress and less feelings of worries and stress at bedtime when work hours were reduced. Similarly, the intervention showed positive effects on days off, except for sleep duration. The range of the effect size (Cohen’s f2) was 0.03–0.08 on workdays and 0.03–0.04 on days off. The range of internal response rates for the outcomes in diary data were 73–93%.
Table 4
Mean values and standard deviations (SD) over the three data collection periods divided on group and gender and results of the group×time interaction from the multilevel mixed model analyses. All three data collection periods are included in the model. [SSQ=subjective sleep quality; I=intervention group; C=control group]
| Group | Baseline | 9 months | 18 months | Multilevel mixed-model analyses | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||||||||||
| Women | Men | Women | Men | Women | Men | Estimate | 95% CI | |||||||||
|
|
|
|
|
|
|
|||||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||||
| SSQ work (1–5 good) | I | 4.03 | 0.5 | 4.27 | 0.5 | 4.18 | 0.5 | 4.35 | 0.4 | 4.28 | 0.5 | 4.44 | 0.4 | 0.086 a | 0.036 | 0.135 |
| C | 4.12 | 0.5 | 4.20 | 0.6 | 4.10 | 0.6 | 4.25 | 0.5 | 4.19 | 0.5 | 4.24 | 0.5 | ||||
| SSQ days off (1–5 good) | I | 4.21 | 0.8 | 4.47 | 0.5 | 4.37 | 0.7 | 4.49 | 0.6 | 4.46 | 0.6 | 4.50 | 0.6 | 0.109 a | 0.040 | 0.179 |
| C | 4.32 | 0.6 | 4.25 | 0.8 | 4.32 | 0.7 | 4.43 | 0.7 | 4.30 | 0.7 | 4.25 | 0.7 | ||||
| Sleep length work (hh:min) | I | 7:20 | 0:42 | 7:09 | 0:42 | 7:40 | 0:42 | 7:28 | 0:48 | 7:40 | 0:42 | 7:33 | 0:42 | 0.196 a | 0.130 | 0.263 |
| C | 7:20 | 0:42 | 7:19 | 0:42 | 7:18 | 0:48 | 7:13 | 0:54 | 7:19 | 0:48 | 7:20 | 0:48 | ||||
| Sleep length days off (hh:min) | I | 8:32 | 1:06 | 8:16 | 1:00 | 8:40 | 1:00 | 8:23 | 1:06 | 8:37 | 1:06 | 8:20 | 1:06 | -0.042 | -0.159 | 0.074 |
| C | 8:34 | 1:06 | 8:16 | 1:06 | 8:41 | 1:12 | 8:13 | 1:12 | 8:41 | 1:06 | 8:40 | 1:06 | ||||
| Sleepiness work (1–9 very sleepy) | I | 4.58 | 1.0 | 4.01 | 1.0 | 4.10 | 1.0 | 3.69 | 1.0 | 3.94 | 0.9 | 3.54 | 1.1 | -0.206 a | -0.295 | -0.117 |
| C | 4.60 | 0.9 | 3.95 | 1.3 | 4.41 | 1.0 | 4.03 | 1.2 | 4.25 | 1.0 | 4.19 | 1.1 | ||||
| Sleepiness days off (1–9 very sleepy) | I | 4.04 | 1.2 | 3.84 | 1.3 | 3.82 | 1.2 | 3.36 | 1.2 | 3.67 | 1.1 | 3.26 | 1.3 | -0.224 a | -0.337 | -0.111 |
| C | 3.98 | 1.1 | 3.32 | 1.3 | 3.90 | 1.2 | 3.44 | 1.3 | 3.90 | 1.1 | 3.77 | 1.4 | ||||
| Stress work (1–9 very high) | I | 3.46 | 1.2 | 2.75 | 1.3 | 2.88 | 1.2 | 2.44 | 1.1 | 2.84 | 1.1 | 2.53 | 1.1 | -0.243 a | -0.356 | -0.130 |
| C | 3.34 | 1.3 | 2.76 | 1.1 | 3.20 | 1.4 | 2.93 | 1.0 | 3.29 | 1.3 | 3.02 | 1.1 | ||||
| Stress days off (1–9 very high) | I | 2.42 | 1.2 | 2.21 | 1.3 | 2.15 | 1.2 | 1.85 | 0.9 | 2.06 | 1.0 | 2.00 | 1.1 | -0.224 a | -0.338 | -0.110 |
| C | 2.24 | 1.2 | 1.87 | 0.9 | 2.23 | 1.3 | 2.01 | 0.8 | 2.39 | 1.3 | 1.91 | 0.8 | ||||
| Worries/stress at bedtime work (1–5 no worry/stress) | I | 4.24 | 0.7 | 4.52 | 0.6 | 4.44 | 0.7 | 4.59 | 0.5 | 4.50 | 0.6 | 4.72 | 0.5 | 0.089 a | 0.026 | 0.151 |
| C | 4.41 | 0.6 | 4.43 | 0.7 | 4.44 | 0.7 | 4.50 | 0.6 | 4.46 | 0.6 | 4.60 | 0.6 | ||||
| Worries/stress at bedtime days off (1–5 no worry/stress) | I | 4.57 | 0.7 | 4.67 | 0.6 | 4.66 | 0.7 | 4.81 | 0.5 | 4.76 | 0.5 | 4.84 | 0.4 | 0.098 a | 0.032 | 0.164 |
| C | 4.69 | 0.6 | 4.63 | 0.7 | 4.72 | 0.5 | 4.72 | 0.5 | 4.65 | 0.7 | 4.73 | 0.6 | ||||
Sensitivity analyses through exclusion of the workplace (with N=17 employees) that could not be part of the randomization showed no differences in comparison with the original analyses (see table A in the supplementary material, www.sjweh.fi/index.php?page=data-repository). Furthermore, adding age, educational level and level of job control at baseline as covariates did not impact on the results of the unadjusted models (see table A in supplement).
The analyses of subjective sleepiness (measured by KSS) and perceived stress for the different time points of the day showed no significant three-way interactions, neither for workdays nor days off (see figure 2 and 3).
Subgroup analysis
Subgroup analyses were made on gender, age, and having children living at home, as well as on baseline levels of sleep quality and worries and stress at bedtime. Mean values and effects of the three-way interactions are presented as supplementary material in tables B–F (www.sjweh.fi/index.php?page=data-repository). The results showed that women, older employees, and employees having children living at home did not benefit more from the worktime reduction, except for women reporting marginally less improvement in sleepiness during days off after the introduction of worktime reduction as compared to men. Moreover, those who had poorer sleep quality at baseline benefited more from the intervention in terms of less feelings of worries and stress at bedtime on days off. Whereas baseline levels of worries and stress at bedtime did not impact on the effect of worktime reduction.
Discussion
The hypothesis that a 25% worktime reduction from fulltime work during 18 months would result in longer sleep duration on workdays, better subjective sleep quality, lower mean daytime sleepiness and perceived stress, including worries and stress at bedtime, was confirmed. During days off, the intervention also improved subjective sleep quality, sleepiness and stress, as well as worries and stress at bedtime, but not sleep duration. The effect of the intervention on sleepiness and perceived stress was similar across the day. The results support earlier, non-randomized intervention studies on introducing a 6-hour workday, which showed improved subjective sleep quality and reduced mental fatigue (13), and reduced symptoms of job exhaustion (14). In contrast to this relatively substantial reduction in worktime, a minor reduction of work hours (2.5 hours/week) showed no effect on recovery, fatigue, or well-being (17).
The beneficial effects of worktime reduction on days off have not been investigated across occupations before. It is reasonable that the need for recovery was lower during days off when weekly work hours were reduced by 25%, since recovery opportunities were enhanced during workdays. Neither women, participants with children living at home, nor older employees did benefit more from worktime reduction. These results were shown in spite of the fact that women working full-time and parents with children living at home often have a higher workload (18, 19) and that health and sleep problems becomes more prevalent with increasing age (29, 30).
The aim of the present study was to investigate the effects of a worktime reduction in a working population considered to have a relatively high workload (20). However, since participants reported good sleep and did not show severe sleepiness or stress levels at baseline, small effect sizes could be expected. Two recent systematic reviews similarly show small but significant effects on occupational stress and subjective health by interventions aiming at improving general work conditions, sometimes including changed work schedules (31, 32).
Strengths and limitations
This is the first controlled intervention study of a substantial worktime reduction with preserved salary, using a randomized procedure and including a considerable number of workplaces. Attrition rate was low and sample size large, contributing to high statistical power. The diary procedure provided reliable data with low risk for recall bias and allowed for analyses of workdays and days off separately. By employing new staff to cover up for the worktime reduction, a diminishing level of workload could be ensured. An important additional feature of the present study’s design was its relatively long follow-up of 18 months after introduction of the intervention.
Some limitations of the study should be pointed out. Firstly, worktime reduction was smaller than expected, 20% rather than 25% during the measurement weeks, possibly diluting the effects of the intervention. However, on the monthly level, official payroll data shows a 25% reduction in the intervention group. Secondly, the lack of objective measurements for the outcomes could have introduced bias, such as overestimation of the effects of the intervention. However, diary data have previously been shown to be a reliable method of measuring sleep/wake patterns (33, 34). Thirdly, the randomization procedure could not be fully implemented, since one workplace was not able to recruit new staff, and consequently this organization was automatically part of the control group. However, sensitivity analyses showed no differences in comparison with the original analyses. Fourthly, the study sample was relatively healthy and had low prevalence of severe sleep/wake disturbances or high levels of perceived stress. Thus, stronger effects may occur for employees with poorer sleep and higher levels of stress.
Practical implications and future research
The results in this present study should not be generalized to interventions where salary is not retained. Even though retaining salary without doubt increases costs in a worktime reduction intervention, it should be noted that high self-reported stress, sleep disturbances and elevated sleepiness have been linked to higher accident and occupational injury risk, poorer work performance, lower productivity and increased risk of health-related problems (35–37). Thus, it is likely that employees with sufficient sleep, low stress levels and high levels of daytime alertness are positively related to both work productivity and associated costs. In order to develop strategies to ameliorate health and well-being in the working population, future research should investigate worktime reduction as a means to diminish sick leave or as a part of a rehabilitation program for employees suffering from chronic health problems.
In conclusion, our findings indicate that a 25%, fully compensated reduction in work hours for full-time workers can lead to long-term positive effects on sleep duration and sleep quality, as well as reduced sleepiness and levels of perceived stress. Such effects could be beneficial for an employee’s life satisfaction, daily functioning, and health development.