Neck-shoulder pain (NSP) is a common occupational problem imposing a considerable economic burden on society and organizations (1–3). The annual prevalence of NSP among workers ranges from 30–50% (3), with increasing rates with higher age and among females (3, 4). Factors attributed to the physical work environment, eg, manual handling, constrained working postures, and repetitive arm movements, are presumed risk factors for NSP (5). However, it has been difficult to establish consistent determinants for the time course of NSP (6–8).
The course (trajectory) of NSP is often characterized by recurrent episodes and fluctuations in pain across time rather than following a consistent pattern (9–11). About 10% in the general and working population develop chronic NSP (12, 13). However, studies on the course of NSP have mainly assessed pain at relatively few points over time, often at yearly intervals (6, 8). Such study designs are limited to capturing long-term changes in NSP, while neglecting the temporal variability in pain occurring within a year, eg, between days, weeks or months. Thus, frequent repeated measurements of pain are important to obtain precise and accurate estimates of the course of NSP (14), while minimizing potential recall bias (15).
The degree of NSP varies from very mild symptoms to severe persistent pain (9, 16). The long-term prognosis of NSP also shows a considerable variability between individuals (6). This heterogeneity may consist of homogenous subgroups with different trajectories of NSP and unique risk factors and biological mechanisms (17). Identifying such subgroups may be an important component in establishing prognostic factors and improving diagnosis and treatment of NSP (8). Also, this can aid detection of target groups with NSP in need of specific interventions for prevention of pain, sick-leave, and early retirement.
Latent class growth analysis (LCGA) is an established approach to identify homogenous subgroups (classes) based on individual change, ie, growth parameters (18). LCGA has been used in several studies to identify trajectories of low-back pain (19–21), widespread pain (22) as well as disability (23) and sick-leave (24) due to pain in the arm, neck and shoulders. Lövgren et al (17) used LCGA to determine trajectories of NSP among nursing students based on yearly measurements before and after graduation identifying six trajectories ranging from asymptomatic (43%) to chronic NSP (14%). However, only few studies using frequent (eg, monthly) measurements of pain have been conducted in occupational samples, and to our knowledge, studies using LCGA to identify trajectories of NSP among workers are lacking.
The aims of the present longitudinal study are to (i) identify and characterize subgroups of workers with different trajectories of NSP (assessed every four weeks over one year), and (ii) investigate the extent to which these pain trajectories are predicted by NSP characteristics, personal and occupational factors at baseline.
Methods
Design and study population
This longitudinal study was conducted on data from the Danish PHysical ACTivity cohort with Objective measurements (DPhacto). The study is reported according to STROBE (25). The study protocol is presented in detail elsewhere (26). In brief, data collection was conducted from April 2012 to May 2014 at 15 Danish workplaces in four occupational sectors (cleaning, transportation, manufacturing, and administration in these companies).
Assessment during baseline consisted of a brief questionnaire and a standardized health examination, followed by objective assessment of physical activities in free living conditions. Data on physical activity are presented elsewhere (27, 28). Immediately following baseline, frequent longitudinal data of NSP were collected over the following 12 months, as previously described (26).
The workplaces were initially contacted and recruited in collaboration with a large Danish workers’ union. The workers were recruited to the study at their convenience. The only inclusion criterion was current employment. Exclusion criteria were having a managing position, being pregnant, or being a student/trainee.
In total, 2107 employees were invited to participate in the study, and 1119 accepted. Of these, 32 were excluded due to having a managing position (N=17), being pregnant (N=2), or being a student/trainee (N=13). Of the remaining 1087 workers, 782 responded to a questionnaire and took part in longitudinal measurements of NSP. Finally, longitudinal data of NSP were obtained from 748 workers, comprising the analyzed study population.
All participants provided their written informed consent prior to participation. The present study was conducted according to the Helsinki Declaration, approved by the Danish Data Protection Agency, and evaluated by the Regional Ethics Committee in Copenhagen (H-2-2012-011).
Baseline assessment
Baseline characteristics included personal (ie, age, gender and BMI) and occupational (ie, job seniority, sector and physical strain at work) factors, and NSP characteristics (eg, intensity, frequency and localization of pain), which were primarily obtained from the questionnaire. These factors were selected based on previous studies and theoretical assumptions to account for a broad range of potentially relevant predictors of NSP.
Personal factors
Age was determined from the workers’ Danish civil registration numbers. Gender was determined by the question “Are you male or female?”. Body mass index (BMI, kg/m2) was calculated from objectively measured height and body weight.
Occupational factors
Job seniority (in years) was determined using the question “For how long have you had the kind of occupation that you have currently?”. Occupational sector with four categories (cleaning, manufacturing, transportation, and administration) was determined using information from the company about occupational sector (cleaning, manufacturing, or transportation), combined with the question “Where do you predominantly work?” with two alternatives (“administration” and “production”). Physical strain at work was determined using the question “How physically demanding do you normally consider your present work?” using a 10-point (1–10) scale (modified CR10 based on Borg) (29) with higher values indicating increasing physical demands.
Musculoskeletal pain
The intensity and frequency of pain in different body sites were assessed based on the standardized Nordic questionnaire for the analysis of musculoskeletal symptoms (30). Peak pain intensity was rated in different body sites (ie, neck/shoulders, elbows, hands/wrists, lower back, hips, knees, and feet/ankles) using the question “State the worst pain you have experienced during the past month?”, using an 11-point scale ranging from 0 (“no pain”) to 10 (“worst pain imaginable”). Frequency of NSP was determined using the question “In the past 12 months, how many days in all have you had pain or discomfort in the neck/shoulders?” using six response categories, which were merged into three categories (ie, “0–7 days”, “8–90 days” and “>90 days). Comorbidity of pain in other body sites was defined as a pain intensity score >2 for NSP (scale 0–10) and a score of >2 in at least one more body site (as listed above). Pain medication was determined using the question “In the past three months, how many days have you been taking analgesics due to pain in muscles and joints?”, with seven response categories, which were merged into four categories (ie, “0 days”, “1–7 days”, “8–30 days” and “>30 days”).
Interference of pain in performing daily activities were determined using three modified items from the SF-36 survey (31). Interference in daily work was determined using the question “In the past three months, how much has pain interfered with your daily work (including both work outside and inside the home and housework)?” with five categories ranging from 1 (“very little”) to 5 (“to a very large extent”). Interference in social activities was determined using the question “In the past three months, has pain in muscles or joints interfered with your social activities?” with an 11-point scale from 0 (“no impact”) to 10 (“completely prevented it”). Interference in demanding physical work was determined using the question “In the past three months, has pain in muscles and joints interfered with the performance of your most demanding physical work tasks?” with an 11-point scale from 0 (“no impact”) to 10 (“completely prevented it”).
Frequent longitudinal assessment of neck-shoulder pain
Text messages (SMS) were used to collect repeated data on self-reported NSP over 12 months using the commercial software “SMS-Track” (sms-track.com). The participant received one SMS at four week intervals over 12 months, resulting in 14 SMS in total. The SMS were sent on Sundays, with a reminder the following day. The participants rated their peak pain intensity in the neck-shoulder region during the previous month using a single item with an 11-point numeric rating scale (NRS), ranging from 0 (“no pain”) to 10 (“worst pain imaginable”) (30). The NRS is a valid and reliable instrument for assessment of pain severity (32) and is a recommended outcome in clinical trials (33). Overall, compliance to the SMS was very high; that is, 92% of the included workers provided ≥10 valid responses (ie, a pain score between 0–10), and 66% responded to all 14 SMS. Inclusion in this study required a valid pain response to the first SMS (N=748). Of the 748 included workers, 99% provided ≥2 valid responses over the 12 month period.
Statistical analyses
LCGA was used to identify subgroups of workers with different trajectories of NSP over 12 months. In brief, LCGA uses observed variables representing different aspects of change over time (ie, pain trajectories) as indicators for unobserved (latent) variables (18). This method assigns individuals to subgroups (classes) so the pain trajectories for the individuals are homogenous within each class and heterogeneous between classes. Thus, the variance within class is fixed to zero while the variance between classes varies. Each separate class has its unique growth parameters, ie, intercept, residual variance, and (linear) slope, representing its trajectory of NSP across the one-year study period.
The LCGA were performed using time (14-levels across one year) as a continuous predictor and NSP intensity as a continuous dependent variable. The LCGA models were run stepwise with increasing number of classes (34). The initial model was based on a single class solution, and then one class at the time was added in the subsequent models. To determine the optimal number of classes, model fit indices [ie, Bayesian information criterion (BIC), entropy and bootstrap log likelihood ratio (BLRT)] were evaluated and compared to the previous model, as recommended (18, 34). Also, the interpretability of the identified classes was evaluated with respect to differences in growth parameters (ie, intercept, slope, and error variance) and clinical relevance. Missing values were considered as missing at random and included in all models without imputations.
Demographic variables at baseline are presented as mean and standard deviation (SD) or frequency and percentages, where appropriate. Differences between trajectory classes in personal, occupational and symptom characteristics at baseline were determined using one-way ANOVA (continuous outcomes) or Chi2 test (frequencies).
Multinomial logistic regression was used to determine associations between personal, occupational and NSP characteristics (predictors) at baseline and trajectory class membership (outcome) based on the LCGA. First, univariate regression models were run for each predictor using trajectory class as a categorical dependent variable referencing those with lower intensities of NSP. Then, two separate multivariate regression models were run for (i) personal and occupational factors, and (ii) symptom characteristics as predictors and trajectory class as the dependent variable to avoid over-adjustment by symptom characteristics. Finally, the second regression model was re-run with additional adjustment for the significant predictors identified in the first multivariate model. Collinearity diagnostics did not indicate any marked multicollinearity among the independent variables (all variance inflation factor values <3.6). Thus all predictors were included in the multivariate regression models. For each model, we determined the odds ratios (OR) with 95% confidence intervals (CI). In the multivariate logistic regression, the explained variance was determined using Nagelkerke´s pseudo R2. The level of significance was set at P<0.05.
LCGA were performed using Latent Gold, version 5.1 (Statistical Innovations Belmont, MA, USA). SPSS software, version 22 (IBM Corp, Armonk, NY, USA) was used to derive descriptive data and to predict class membership.
Results
Baseline characteristics of the study population
Of the 748 participants, 83% were blue-collar workers (cleaning 15%; manufacturing 60%; transportation 8%) and 17% worked in administration in the same workplaces. Both males and females were represented, although with a slight predominance of males (55%). The participants were on average 45 (SD 10) years of age, had been in their current job for 14 (SD 10) years, and had a BMI of 27 (SD 5). The mean intensity of NSP was 3.3 (SD 3.0) on the 0-10 scale, and only 212 (28%) of the workers were asymptomatic during the previous three months (ie, pain intensity <1). During follow-up, the participants responded to, on average, 13 (SD 2.3) text messages (14 in total).
Table 1 shows baseline characteristics of the study population stratified on physical strain at work. The stratum with high physical strain contained a larger proportion of females and blue-collar workers, had a slightly higher BMI, and reported more pain-related symptoms.
Table 1
Baseline characteristics of the study population stratified on physical strain at work. Symptom characteristics were obtained from the questionnaire at baseline. [SD=standard deviation; BMI=body mass index; NSP=neck-shoulder pain].
| Baseline characteristics | Low physical strain (N=346) a | High physical strain (N=377) a | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Mean | SD | % | Mean | SD | % | |
| Age (years) | 45.3 | 8.6 | 44.2 | 10.6 | ||
| Gender (female) | 41.6 | 48.3 | ||||
| BMI (kg/m2) | 26.9 | 4.3 | 27.8 | 5.2 | ||
| Seniority (years) | 13.9 | 10.6 | 13.2 | 10.1 | ||
| Sector | ||||||
| Cleaning | 6.4 | 22.3 | ||||
| Manufacturing | 53.2 | 66.8 | ||||
| Transportation | 5.5 | 9.5 | ||||
| Administration/office | 35.0 | 1.3 | ||||
| Physical strain at work (scale 1–10) | 3.2 | 1.4 | 7.3 | 1.0 | ||
| NSP intensity in past 3 months (scale 0–10) | 2.9 | 2.8 | 3.8 | 3.0 | ||
| NSP frequency (days during previous year) | ||||||
| 0–7 | 62.0 | 51.2 | ||||
| 8–90 | 26.7 | 29.3 | ||||
| >90 | 11.3 | 19.5 | ||||
| NSP comorbidity | ||||||
| No | 61.7 | 45.9 | ||||
| Yes | 38.3 | 54.1 | ||||
| Pain medication (days) | ||||||
| 0 | 48.4 | 45.1 | ||||
| 1–7 | 33.3 | 33.1 | ||||
| 8–30 | 12.2 | 15.2 | ||||
| >30 | 6.1 | 6.7 | ||||
| Pain interference | ||||||
| Daily work (scale 1–5) | 1.9 | 0.9 | 2.4 | 1.0 | ||
| Demanding physical-work tasks (scale 0–10) | 1.7 | 2.5 | 3.2 | 3.0 | ||
| Social activities (scale 0–10) | 1.0 | 2.0 | 1.8 | 2.6 | ||
| Number of valid responses to text messages (max 14) | 13.0 | 2.3 | 12.7 | 2.8 | ||
Trajectory classes of neck-shoulder pain
Consecutive LCGA models with 1–10 classes were evaluated based on model fit indices, distinction between classes and clinical relevance (see supplementary tables S1 and S2, www.sjweh.fi/show_abstract.php?abstract_id=3690). Increasing the number of classes improved model fit, as indicated by decreased BIC values and significant (P<0.001) BLRT, while entropy was reduced (table S1). The distinction between classes in growth parameters and clinical relevance was less obvious in the models with >6 classes (table S2). Thus, the LCGA with six classes was considered the optimal solution and used in further analyses. The identified trajectory classes of NSP (sorted by pain intensity) are characterized as follows (table 2 and figure 1): (i) (class 1) “asymptomatic”: zero pain throughout the study; (ii) (class 2) “very low pain”: very low initial pain level and an early decline toward an asymptomatic state; (class 3) “low recovering pain”: low initial pain level with a slow linear decline over time; (class 4) “moderate fluctuating pain”: moderate initial pain level with a fluctuating pattern and a slow linear decline over time; (class 5) “strong fluctuating pain”: strong initial pain with a fluctuating pattern and a slow linear decline over time; (class 6) “severe persistent pain”: very strong initial pain which persisted over time.
Table 2
Model-fit indices and class-specific growth parameters obtained from the 6-class latent class growth analysis (LCGA). [BIC=Bayesian information criterion BLRT=bootstrap likelihood ratio test.]
| Total | Class 1 | Class 2 | Class 3 | Class 4 | Class 5 | Class 6 | |
|---|---|---|---|---|---|---|---|
| Number | 748 | 81 | 73 | 138 | 208 | 178 | 70 |
| Percent | 100 | 11 | 10 | 18 | 28 | 24 | 9 |
| Growth parameters | |||||||
| Intercept | 2.84 | 0.00 | 0.46 | 1.05 | 2.63 | 5.04 | 6.97 |
| Slope | -0.04 | 0.00 | -0.03 | -0.03 | -0.06 | -0.07 | 0.02 |
| Error variance | 2.55 | 0.00 | 0.26 | 1.18 | 3.95 | 3.99 | 2.58 |
| Model fit indices | |||||||
| BIC | 29262.6 | ||||||
| Entropy | 0.9176 | ||||||
| BLRT a | <0.0001 |
Figure 1
Identified trajectories of neck-shoulder pain (NSP) sorted by pain intensity. The y-axis represents mean values of NSP intensity (scale 0–10) based on the 6-class latent class growth model. The x-axis represents the 14 measurements over one year.
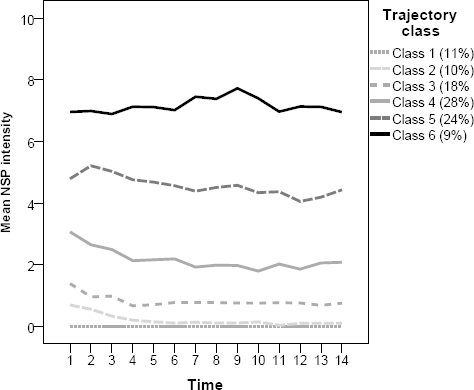
Growth parameters from the 6-class LCGA are shown in table 2. The intercept indicated different intensities of NSP between all trajectory classes (all P<0.001), ranging from zero pain (class 1) to very strong pain (class 6). The negative slope indicated a slow decline in pain intensity over time among classes 2–5 (all P<0.001), which was not the case in the trajectory with “severe persistent pain” (class 6), or in the “asymptomatic” trajectory (class 1). None of the classes showed significantly increased pain intensity over time. Residual variance denoted larger monthly fluctuations in pain intensity for classes 4 and 5 compared to the other classes (table 2). (See also supplementary figure S1, www.sjweh.fi/show_abstract.php?abstract_id=3690.)
Differences between trajectory classes in baseline characteristics
The six trajectories of NSP differed in most personal, occupational and pain-related factors during baseline (table 3). For instance, higher NSP trajectory class modality was linearly associated with female gender, higher BMI, less administration workers, higher physical strain at work, higher pain severity, multisite pain, more days on pain medication, and more pain interference in daily life.
Table 3
Baseline characteristics in each of the six identified trajectory classes of neck-shoulder pain (NSP) in the DPhacto cohort (N=748). [BMI=body mass index; NSP=neck-shoulder pain; SD=standard deviation].
| Baseline characteristics | N | Class 1 (N=81) | Class 2 (N=73) | Class 3 (N=138) | Class 4 (N=208) | Class 5 (N=178) | Class 6 (N=70) | P-value | P-value (linear trend) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
|
||||||||||||||||
| Mean | SD | % | Mean | SD | % | Mean | SD | % | Mean | SD | % | Mean | SD | % | Mean | SD | % | ||||
| Age (years) | 748 | 45.8 | 9.5 | 43.5 | 9.8 | 43.5 | 10.9 | 43.9 | 9.2 | 45.9 | 9.8 | 47.6 | 8.9 | 0.012 | 0.059 | ||||||
| Gender (female) | 748 | 43.2 | 26.0 | 43.5 | 39.9 | 57.3 | 54.3 | <0.001 | <0.001 | ||||||||||||
| BMI (kg/m2) | 732 | 26.4 | 3.8 | 26.6 | 5.2 | 26.9 | 4.6 | 27.8 | 5.2 | 27.5 | 4.4 | 28.1 | 5.3 | 0.068 | 0.005 | ||||||
| Seniority (years) | 722 | 14.3 | 10.9 | 11.3 | 8.7 | 14.5 | 10.6 | 12.4 | 9.9 | 13.5 | 10.2 | 15.6 | 11.4 | 0.046 | 0.256 | ||||||
| Sector | 748 | <0.001 | <0.001 | ||||||||||||||||||
| Administration | 128 | 21.0 | 12.3 | 25.4 | 22.1 | 8.4 | 8.6 | ||||||||||||||
| Cleaning | 115 | 9.9 | 9.6 | 11.6 | 13.0 | 23.0 | 22.9 | ||||||||||||||
| Manufacturing | 448 | 61.7 | 63.0 | 58.0 | 53.8 | 64.0 | 65.7 | ||||||||||||||
| Transportation | 57 | 7.4 | 15.1 | 5.1 | 11.1 | 4.5 | 2.9 | ||||||||||||||
| Physical strain at work (scale 1–10) | 723 | 4.7 | 2.5 | 4.7 | 2.2 | 5.0 | 2.4 | 5.0 | 2.5 | 6.1 | 2.2 | 6.3 | 2.3 | <0.001 | <0.001 | ||||||
| NSP intensity past 3 months (scale 0–10) | 745 | 0.5 | 1.3 | 1.4 | 2.0 | 2.0 | 2.6 | 3.2 | 2.6 | 5.1 | 2.6 | 7.1 | 3.0 | <0.001 | <0.001 | ||||||
| NSP frequency (days/previous year) | 745 | <0.001 | <0.001 | ||||||||||||||||||
| 0–7 | 420 | 98.8 | 84.9 | 78.8 | 57.0 | 24.7 | 12.9 | ||||||||||||||
| 8–90 | 209 | 1.3 | 13.7 | 18.2 | 37.2 | 47.2 | 17.1 | ||||||||||||||
| >90 | 116 | 0.0 | 1.4 | 2.9 | 5.8 | 28.1 | 70.0 | ||||||||||||||
| NSP comorbidity | 745 | <0.001 | <0.001 | ||||||||||||||||||
| No | 399 | 90.0 | 86.3 | 74.5 | 54.1 | 23.0 | 12.9 | ||||||||||||||
| Yes | 346 | 10.0 | 13.7 | 25.5 | 45.9 | 77.0 | 87.1 | ||||||||||||||
| Pain medication (days/previous 3 months) | 745 | <0.001a | <0.001a | ||||||||||||||||||
| 0 | 347 | 73.8 | 71.2 | 64.2 | 42.5 | 26.4 | 18.6 | ||||||||||||||
| 1–7 | 247 | 20.0 | 27.4 | 27.0 | 40.6 | 37.1 | 34.3 | ||||||||||||||
| 8–30 | 103 | 5.0 | 0.0 | 8.0 | 12.6 | 25.8 | 22.9 | ||||||||||||||
| >30 | 48 | 1.3 | 1.4 | 0.7 | 4.3 | 10.7 | 24.3 | ||||||||||||||
| Pain interference | 745 | ||||||||||||||||||||
| Daily work (scale 1–5) | 745 | 1.6 | 0.8 | 1.4 | 0.7 | 1.8 | 0.8 | 2.2 | 1.0 | 2.7 | 0.9 | 3.1 | 1.0 | <0.001 | <0.001 | ||||||
| Demanding physical work (scale 0–10) | 745 | 0.8 | 1.7 | 1.0 | 2.0 | 1.7 | 2.5 | 2.3 | 2.7 | 3.6 | 2.9 | 4.7 | 3.2 | <0.001 | <0.001 | ||||||
| Social activities (scale 0–10) | 745 | 0.4 | 1.3 | 0.4 | 1.3 | 0.8 | 1.7 | 1.3 | 2.4 | 2.2 | 2.6 | 3.2 | 3.0 | <0.001 | <0.001 | ||||||
| Valid responses to text messages (max 14) | 748 | 12.6 | 2.9 | 13.2 | 2.0 | 13.0 | 2.1 | 13.0 | 2.6 | 12.7 | 2.9 | 12.2 | 3.4 | 0.191 | 0.138 | ||||||
Prediction of NSP trajectory classes
Univariate associations between baseline characteristics and trajectory classes of NSP are shown in table 4. The trajectory class “moderate fluctuating pain” (class 4) was positively associated with BMI and all pain characteristics, while none of the occupational factors was significant. The trajectory “strong fluctuating” NSP (class 5) was positively associated with age, female gender, cleaning or manufacturing work (referencing administration), physical strain at work, and all pain characteristics (table 4). The trajectory “severe persistent NSP” (class 6) was associated with the same factors during baseline as strong NSP.
Table 4
Univariate associations between baseline predictors and trajectory classes of neck-shoulder pain (NSP), referencing classes 1–3. [OR=odds ratio; CI=confidence interval; BMI=body mass index; NSP=neck-shoulder pain].
| Multinomial regression, predictors | N | Moderate fluctuating (Class 4) | Strong fluctuating (Class 5) | Severe persistent (Class 6) | |||
|---|---|---|---|---|---|---|---|
|
|
|
|
|||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | ||
| Personal factors | |||||||
| Age a (years) | 748 | 1.00 | 0.98–1.02 | 1.02 | 1.0–1.04 | 1.04 | 1.01–1.07 |
| Gender | |||||||
| Female (reference) | 337 | 1 | 1 | 1 | |||
| Male | 411 | 0.96 | 0.67–1.39 | 0.48 | 0.33–0.70 | 0.54 | 0.32–0.91 |
| BMI a (kg/m2) | 732 | 1.05 | 1.01–1.09 | 1.04 | 1.0–1.08 | 1.07 | 1.01–1.13 |
| Occupational factors | |||||||
| Seniority a (years) | 722 | 0.99 | 0.97–1.01 | 1.00 | 0.98–1.02 | 1.02 | 0.99–1.04 |
| Sector | |||||||
| Administration (reference) | 128 | 1 | 1 | 1 | |||
| Cleaning | 115 | 1.15 | 0.61–2.20 | 5.38 | 2.59–11.19 | 5.25 | 1.87–14.74 |
| Manufacturing | 448 | 0.84 | 0.54–1.32 | 2.63 | 1.43–4.86 | 2.66 | 1.08–6.53 |
| Transportation | 57 | 1.27 | 0.64–2.53 | 1.36 | 0.51–3.61 | 0.85 | 0.16–4.49 |
| Physical strain at work a (scale 1–10) | 723 | 1.03 | 0.96–1.11 | 1.25 | 1.15–1.36 | 1.31 | 1.16–1.49 |
| Pain characteristics | |||||||
| NSP intensity a (scale 0–10) | 745 | 1.42 | 1.30–1.55 | 1.81 | 1.65–2.0 | 2.49 | 2.15–2.88 |
| NSP frequency (days/previous year) | |||||||
| 0–7 (reference) | 420 | 1 | 1 | 1 | |||
| 8–90 | 209 | 4.51 | 2.87–7.09 | 13.20 | 7.97–21.88 | 9.22 | 3.63–23.43 |
| >90 | 116 | 5.06 | 1.74–14.71 | 56.59 | 21.38–149.82 | 271.13 | 87.12–843.81 |
| NSP comorbidity | |||||||
| No (reference) | 399 | 1 | 1 | 1 | |||
| Yes | 346 | 3.79 | 2.53–5.68 | 14.94 | 9.44–23.64 | 30.31 | 14.17–64.85 |
| Pain medication (days/previous 3 months) | |||||||
| 0 (reference) | 347 | 1 | 1 | 1 | |||
| 1–7 | 247 | 2.60 | 1.74–3.89 | 3.83 | 2.42–6.07 | 5.03 | 2.43–10.4 |
| 8–30 | 103 | 3.92 | 1.98–7.76 | 12.98 | 6.69–25.22 | 16.33 | 6.63–40.18 |
| >30 | 48 | 6.78 | 1.79–25.66 | 26.82 | 7.62–94.39 | 86.74 | 22.5–334.45 |
| Pain interference | |||||||
| Daily work a (scale 1–5) | 745 | 2.16 | 1.72–2.71 | 3.68 | 2.88–4.69 | 5.41 | 3.95–7.43 |
| Demanding physical work a (0–10) | 745 | 1.20 | 1.11–1.30 | 1.41 | 1.30–1.52 | 1.57 | 1.42–1.73 |
| Social activities a (scale 0–10) | 745 | 1.27 | 1.14–1.41 | 1.46 | 1.31–1.62 | 1.62 | 1.44–1.82 |
Two multivariate regression models using trajectory classes 4–6 as outcomes were constructed for (i) personal and occupational factors and (ii) pain characteristics (table 5). The model containing personal and occupational characteristics showed an explained variance of 14% (pseudo R2=0.14), while the model containing pain characteristics accounted for 54% of the variance (pseudo R2=0.54). Additional adjustment for gender, age, and physical strain at work revealed similar results for pain characteristics as the model without adjustment (all P<0.05; pseudo R2=0.54).
Table 5
Multivariate associations between baseline predictors and trajectory classes of neck-shoulder pain (NSP), referencing classes 1–3. Two separate models were constructed for (i) personal and occupational factors and (ii) symptom characteristics. [OR=odds ratio; CI=confidence interval; BMI=body mass index; NSP=neck-shoulder pain].
| Multinomial regression, predictors | N | Moderate fluctuating (Class 4) | Strong fluctuating (Class 5) | Severe persistent (Class 6) | |||
|---|---|---|---|---|---|---|---|
|
|
|
|
|||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | ||
| Personal factors | |||||||
| Age a (years) | 748 | 1.00 | 0.98–1.03 | 1.02 | 0.99–1.04 | 1.03 | 1.00–1.07 |
| Gender | |||||||
| Female (reference) | 337 | 1 | 1 | 1 | |||
| Male | 411 | 0.96 | 0.63–1.47 | 0.54 | 0.34–0.85 | 0.67 | 0.37–1.24 |
| BMI a (kg/m2) | 732 | 1.04 | 1.00–1.09 | 1.02 | 0.98–1.07 | 1.05 | 1.00–1.12 |
| Occupational factors | |||||||
| Seniority a (years) | 722 | 0.99 | 0.97–1.01 | 1.00 | 0.98–1.02 | 1.01 | 0.98–1.04 |
| Sector | |||||||
| Administration (reference) | 128 | 1 | 1 | 1 | |||
| Cleaning | 115 | 0.69 | 0.30–1.60 | 1.60 | 0.63–4.06 | 1.11 | 0.30–4.12 |
| Manufacturing | 448 | 0.65 | 0.37–1.15 | 1.40 | 0.66–2.96 | 1.06 | 0.36–3.09 |
| Transportation | 57 | 0.90 | 0.40–2.02 | 0.86 | 0.28–2.62 | 0.18 | 0.02–1.77 |
| Physical strain at work a (scale 1–10) | 723 | 1.07 | 0.97–1.18 | 1.23 | 1.11–1.37 | 1.31 | 1.13–1.52 |
| Pain characteristics | |||||||
| NSP intensity a (scale 0–10) | 745 | 1.29 | 1.12–1.49 | 1.31 | 1.12–1.53 | 1.66 | 1.35–2.03 |
| NSP frequency (days/previous year) | |||||||
| 0–7 (reference) | 420 | 1 | 1 | 1 | |||
| 8–90 | 209 | 2.05 | 1.20–3.51 | 3.91 | 2.11–7.25 | 1.65 | 0.56–4.88 |
| >90 | 116 | 1.40 | 0.43–4.59 | 8.79 | 2.82–27.46 | 16.67 | 4.27–65.14 |
| NSP comorbidity | |||||||
| No (reference) | 399 | 1 | 1 | 1 | |||
| Yes | 346 | 0.91 | 0.48–1.72 | 1.82 | 0.88–3.77 | 1.36 | 0.46–4.04 |
| Pain medication (days/previous 3 months) | |||||||
| 0 (reference) | 347 | 1 | 1 | 1 | |||
| 1–7 | 247 | 1.50 | 0.96–2.35 | 1.75 | 0.99–3.07 | 1.96 | 0.79–4.84 |
| 8–30 | 103 | 1.49 | 0.69–3.22 | 3.02 | 1.33–6.83 | 3.73 | 1.20–11.56 |
| >30 | 48 | 2.35 | 0.53–10.45 | 2.96 | 0.62–14.20 | 3.95 | 0.69–22.59 |
| Pain interference | |||||||
| Daily work a (scale 1–5) | 745 | 1.83 | 1.32–2.53 | 2.47 | 1.70–3.59 | 2.88 | 1.73–4.80 |
| Demanding physical work a (0–10) | 745 | 0.91 | 0.81–1.03 | 0.93 | 0.81–1.06 | 0.91 | 0.77–1.09 |
| Social activities a (scale 0–10) | 745 | 1.10 | 0.96–1.26 | 1.11 | 0.96–1.29 | 1.16 | 0.96–1.39 |
In the multivariate analyses (table 5), “moderate fluctuating pain” (class 4) was positively associated with BMI, days with NSP the previous year, and pain interference in daily work. The trajectory “strong fluctuating pain” (class 5) was negatively associated with male gender, and positively associated with physical strain at work, comorbidity of pain in other body sites, days with NSP, pain medication (8–30 days), and pain interference in daily work. The trajectory “severe persistent pain” (class 6) was positively associated with age, physical strain at work, NSP intensity, >90 days with NSP the previous year, pain medication (8–30 days), and pain interference in daily work.
Discussion
The present longitudinal study used frequent repeated measurements of NSP over one year to identify trajectories of NSP in an occupational sample. Based on LCGA, we identified six distinct trajectories of NSP (asymptomatic 11%, very low NSP 10%, low recovering NSP 18%, moderate recovering NSP 28%, strong fluctuating NSP 24% and severe persistent NSP 9%), with marked differences in NSP and personal and occupational factors at baseline. We found that female gender, age, physical strain at work, NSP severity and comorbidity, pain medication and pain interference in daily work were independent predictors at baseline for severe persistent and/or strong fluctuating NSP in multivariate regression models.
Pain trajectories and occupational and clinical relevance
The monthly prospective measurements of NSP in a relatively large occupational sample are an obvious strength of the study. As far as we know, there are no previous studies using LCGA based on frequent measurements to identify homogenous NSP trajectories in the working population. Relying on frequent text messages, we achieved a considerable compliance and obtained precise estimates of individual pain trajectories (14).
The six identified trajectories of NSP differed markedly in symptom characteristics at baseline. Trajectory class, ranging from asymptomatic (class 1) to severe persistent pain (class 6), was linearly associated with higher pain intensity, more days with pain, comorbidity of pain in other sites, more days on pain medication and more interference of pain in physical and social activities (table 3). This indicates a clinical distinction between the trajectories. It is worth noting that our study was conducted among workers and not in a patient population. Thus, even the trajectory classes with lower pain intensities were considered relevant and potentially reflecting different stages of NSP. However, because of small differences in pain intensity between the subgroups with lower NSP (classes 1–3), their clinical relevance can be questioned (35). On the other hand, it is possible that workers in the asymptomatic trajectory (class 1) are less prone to develop future NSP compared to those with very low NSP (class 2).
Our finding of asymptomatic, decreasing, and persistent NSP trajectories is in accordance with the study by Lövgren et al (17). Interestingly, we did not find any NSP trajectory with increasing pain. This may be caused by the long job-seniority in the present study, ie, 14 years on average; potentially resulting in workers predisposed to increasing NSP trajectories leaving the workplaces prior to the study. Those workers not developing work-related pain prior to the study appear unlikely to develop pain within a 1-year period. Thus, following the progression of NSP among workers entering working life may have yielded different results.
The NSP trajectories with moderate (class 4), strong (class 5), and severe (class 6) pain intensities were characterized by a considerable temporal variability in pain, as indicated by the high residual variance (table 2). This supports the notion of NSP as a fluctuating condition (9, 10); particularly since these two trajectories consisted of >50% of the study population. Still, the determinants of these monthly fluctuations remain unclear and warrant further investigation. This finding underlines the importance of future studies using frequent measurements both of occupational exposure and NSP to determine their relationship.
Using LCGA, two subgroups with more pronounced or chronic NSP were identified; that is, strong fluctuating NSP (class 5, N=178) and severe persistent NSP (class 6, N=70). These two trajectories contained a considerable proportion (33%) of the study population, which is almost twice as high compared to previous studies on chronic NSP (12, 13, 17). Still, the occurrence of severe persistent NSP (9%) is in agreement with some studies using latent class growth modeling of NSP (17) and disabilities due to arm, neck, and shoulder complaints (23). Overall, the high occurrence of NSP may partly be explained by the large proportion (83%) of blue-collar workers in the present study (3). The high risk of NSP among blue-collar workers is presumed to be determined by a combination of occupational, socioeconomic and individual factors (5, 6). The trajectory classes with severe persistent and strong fluctuating NSP may be important as target groups for future workplace interventions; particularly considering that they showed pronounced interference of pain in physical and social activities.
Symptom characteristics and individual predictors of pain trajectory classes
Prognostic studies indicate that current or past symptoms, eg, the occurrence, intensity and duration of NSP and comorbidity of pain in other body sites, predict future NSP (6–8, 36). This was corroborated by the present study showing that the NSP characteristics at baseline accounted for 54% of the variance in explaining NSP trajectories. Specifically, the intensity and frequency of NSP, pain medication and pain interference at baseline were consistent predictors for strong fluctuating and severe persistent NSP in the multivariate model (table 5). Reporting >90 days with NSP the past three months was of particular prognostic value for severe persistent NSP, which is consistent with previous reports (7).
People with NSP often report comorbidity of pain in other body sites, which has been associated with a poor prognosis (36, 37). However, we found that comorbidity of pain at baseline was not a significant predictor for any trajectory class in the multivariate model. Still, it is possible that pain in other body sites occurred during the 12-month follow-up, which might have influenced the results.
None of the personal factors were consistent predictors for NSP trajectories in the multivariate model. Gender (referencing females) showed a moderate negative association with strong fluctuating NSP. Nevertheless, gender is likely confounded by other non-measured factors at work, such as physical work tasks, which usually differ between males and females, even within the same job (38). Systematic reviews indicate no clear gender effect on the prognosis of NSP (7, 11). Age showed a weak positive association with severe persistent NSP, which is in line with other studies (11, 39).
Occupational predictors of pain trajectory classes
Previous studies have failed to determine consistent occupational factors for the prognosis of NSP (6, 7). In a systematic review of prognostic factors for neck pain, white-collar workers had a better prognosis than their blue-collar counterparts (6). This is partly in agreement with our findings. Cleaning and manufacturing workers had larger probabilities for strong fluctuating and severe persistent NSP (referencing administration work), but only in the univariate models. The higher occurrence of more severe pain trajectories among blue-collar workers may be attributed to high physical workload.
Self-reported physical strain at work was a consistent predictor for strong fluctuating and severe persistent NSP, irrespective of personal factors, job-seniority, and occupational sector. This underlines the importance of interventions targeting high physical workload to prevent chronic NSP. Similar findings have been reported in prospective studies on associations between physical work exposures and NSP (5). However, the use of self-reported measurements of both physical strain at work and NSP is a limitation as it could have introduced reporting bias.
Overall, some further limitations should be noted. This study addresses NSP, which usually comprises non-specific disorders of the neck and upper trapezius muscles (40). However, we could not distinguish between pain in the neck and shoulders because it was not feasible to administer pictures on different anatomical regions using text messages. Since the prediction models largely contained self-reported factors, with the exceptions age, BMI and sector, the estimates should be interpreted with caution. Also, some factors were determined using modified questions without additional validation, which could have influenced the results due to measurement error. Another limitation is the lack of repeated measurements of the predictors. This may have yielded important information about changes in work exposure in relation to short-term fluctuations in NSP. Thus, future studies should preferably assess exposure levels repeatedly over time. Further, the prediction models are limited to a selection of personal, occupational and pain-related factors, while other potential prognostic factors were not studied. Thus, further studies should address specific biomechanical factors at work as well as psychosocial working conditions which are presumed to affect the course of NSP (5, 6).
The use of convenience sampling limits the generalizability of the study findings, although we expect that the current findings extend to similar occupational groups. As the response rate to the study was rather low, there is a risk of selection bias. However, comparisons of responders and non-responders indicated no marked difference in any personal, occupational or pain-related factor.
Future studies should address objective measurements of the physical work environment and evaluate whether these pain trajectories are predictive of future sick leave and work ability.
Concluding remarks
In an occupational sample, six distinct trajectories of NSP were identified ranging from asymptomatic to severe persistent pain. Strong fluctuating and severe persistent trajectories of NSP appear strongly determined by past symptoms. Also, our findings suggest that physical strain at work is a pertinent modifiable factor predicting strong fluctuating and severe persistent NSP. The identified pain trajectories can be used as outcomes and possible target groups in future cohorts and worksite interventions on NSP.



