Labor market experiences, such as unemployment or job loss, are an important determinant of health and well-being (1–6). Studies have found a link between unemployment and a variety of health outcomes, including increased risk of mortality (2, 4, 7), cardiovascular disease (8), and depressive symptoms (9). Unemployment has also been consistently linked with lower ratings of self-rated health (SRH) (1, 3, 10), above that which can be explained by potential health-selection into unemployment (1, 2, 10, 11). Moreover, employment has been described as being beneficial for health (6), with studies finding a decreased risk of depression and greater general mental health status among employed individuals. As outlined in Amick and colleagues (5), these individual relationships are embedded within unique social and economic contexts (eg, organization of work, social protections, local and global socioeconomic conditions) that can shape the trajectory of the working life course (1, 3, 5). Thus, not only are there individual-level associations between labor market experiences and health outcomes but also broader social and economic contexts that play a role in attenuating or exacerbating the underlying relationship (1, 4, 5, 12, 13).
Recent methodological frameworks have demonstrated the importance of integrating a life course perspective (5) in order to capture these complex mechanisms operating at the individual, interpersonal, organizational and societal level (1, 4, 5). These are often operationalized as trajectories that depict the labor market or health status of an individual as they progress through the working life course (5, 14). However, only a few studies have attempted to integrate these concepts into concrete analytic measures (5, 10, 14–18). An examination of the dynamic nature of the working life course (versus a static model that focuses on measures from a single point in time) allows us to describe not only the impact of certain end states such as unemployment or labor market exit, but also the distinct labor market patterns associated with better or worsening health trajectories over time.
Given the importance of social and economic factors in shaping individual work-life trajectories (1, 5, 12, 13), it is likely that accounting for additional variation at the contextual-level will provide a deeper understanding of the contexts in which unemployed workers fare better or worse in comparison to individuals with stable employment over time. In 2007, the United States was hit with the largest and deepest economic downturn since World War II, with real GDP declining by 4.3%, unemployment rates increasing to 10%, and repeat spells of joblessness in the post-recession recovery period (19, 20). Recent studies have found a link between the Great Recession and a variety of health outcomes among the general population, including health status, mental health conditions and mortality (12, 21). However, existing models have yet to fully understand the influence of macroeconomic cycles on the unemployment–health relationship, with some authors describing either worse (1, 2, 7, 22–25) or better (13, 26) health and mortality outcomes during periods of economic decline. Variations in the length and severity of recent macroeconomic cycles in the US present a unique opportunity to examine whether the broader economic context exerts a differential impact on the association between labor market experiences and health trajectories (5, 12).
The objectives of this study were to examine the relationship between labor market and self-reported health (LM-H) trajectories among a population-based sample of US individuals drawn from the Panel Study of Income Dynamics (PSID) over the 1988 to 2011 period; and to examine whether the relationship between LM-H trajectories differed across macroeconomic recession or expansion periods. This study hypothesized that trajectories comprised of “worsening” labor market experiences over time would be associated with trajectories comprised of “worsening” health status, when compared to stable employment over time. This study also hypothesized that the length and depth of the Great Recession (compared to earlier recession periods) would exacerbate the association between unemployment and SRH (12, 21, 23).
Methods
Data sources
This study used retrospective cohort data from the PSID, described in detail elsewhere (2). In brief, the PSID contains multigenerational data on employment, economic, demographic and health characteristics, collected from a national probability sample of US households between 1968–2011. Surveys were administered annually until 1997 and then biennially thereafter. Data for this study were obtained from the public-use PSID dataset, produced and distributed by the Survey Research Center at the Institute for Social Research, University of Michigan.
Study sample
Four working-age cohorts were defined using data collected between 1988–2011. Study cohort periods encompass the range of macroeconomic cycles that have occurred in the US in recent decades. The early 1990s recession (20) lasted for only eight months (July to March 1991), and was characterized as mild and brief with relatively small declines in GDP and employment (20). This was followed by a period of economic expansion over the remainder of the decade (1991-2001), although the US was hit again with another mild and brief recession during the early 2000s (20). Most recently, the Great Recession of 2007/2009 represented the largest economic downturn as stated earlier.
Cohorts were defined using data collected over a seven-year period, based on four biennial survey waves. Given the focus on incorporating data from before, during and after the onset of each macroeconomic cycle, this required an overlap in study periods. Study cohorts were restricted to household heads or partners who were aged 20–64 years and in good self-reported health/employed at baseline. We also restricted the cohorts to individuals with a balanced panel of data across all survey waves. A total of 13 585 individuals were included in the final analytic sample, with N=3752 in 1988–1994 (recession period); N=2744 in 1993–1999 (expansion period); N=3387 in 1999–2005 (recession period); and N=3702 in 2005–2011 (recession period). Appendix 1 presents a sample selection flow diagram (www.sjweh.fi/show_abstract.php?abstract_id=3743).
Self-rated health
This study focused on SRH as the key outcome measure, defined as the general health status of the head or partner at the time of survey. SRH has been shown to be a valid overall measure of health, as well as a strong predictor of health morbidity and mortality outcomes (27–29), with systematic reviews and meta-analyses establishing a robust gradient among persons reporting “poor” compared to “excellent” health status (28, 29). We dichotomized SRH as “excellent/very good/good” versus “fair/poor” across each of the four survey waves (per cohort period), resulting in eight unique health trajectories. We then manually clustered the individual trajectories into three distinct patterns: stable good health across all four survey waves; good–poor health; and good–poor–good health. These clusters are similar to latent health trajectories used in previous studies (14, 16, 30). We explored the possibility of using a quantitative method of grouping such as sequence analysis or latent growth modelling, which we did not feel was appropriate given the data structure and limited number of event states.
Labor market status
We used current labor force status, measured across four waves of data (per cohort period), to create labor market trajectories as the key explanatory variable. Current labor force status was defined as employed, unemployed, and labor market inactive (eg, retired, disabled, keeping house, student, other) at the time of survey (31). Based on three event classifications measured across four waves of data, we identified a total of 25 unique trajectories emerging from the baseline condition of employment at start of follow-up.
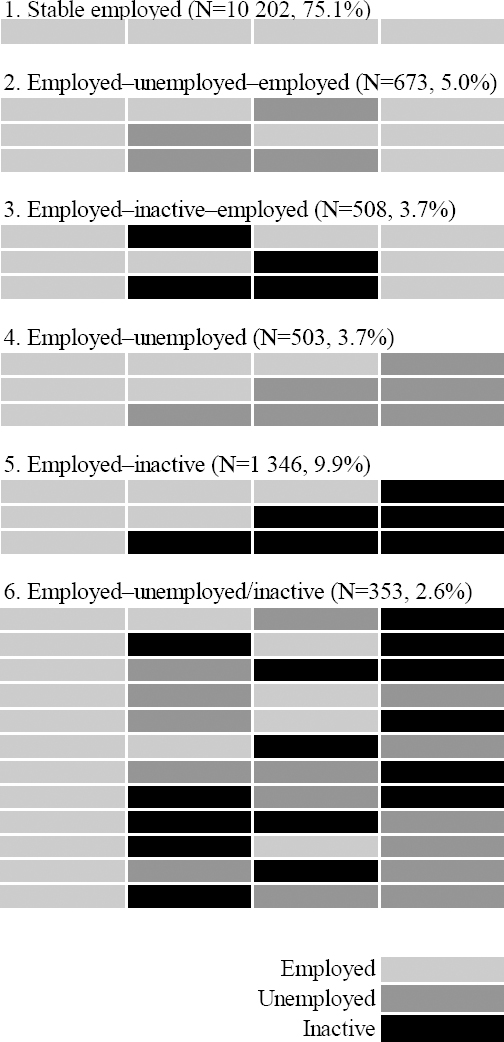
Similar to the construction of health status trajectories, we then manually clustered the individual LM trajectories into six distinct patterns: stable employment across all four survey waves; employed–unemployed; employed–labor market inactivity; employed–unemployed–employed; employed–inactive–employed; and employed to a combination of unemployed and inactivity. We excluded the small proportion of individuals with no discernable pattern of improving or worsening employment over time, given sample size considerations (N=47 total, across all waves). See figure 1 for a graphical depiction of the six clusters of labor market trajectories included in the analyses.
Demographic and socioeconomic variables
Based on a review of the literature examining the relationship between labor market and health outcomes (1, 2, 10, 22), the following variables were included in the analysis (measured at baseline): age; sex; race/ethnicity; marital status; children under 18-years in the family unit; total pre-tax family income for the tax year prior to baseline (adjusted to 2011 USD constant dollars and log transformed); education skill level based on years of education and degree type; and US Census Bureau-designated divisions. Health status in the two years prior to baseline was included as a key covariate given the strong association with subsequent health outcomes (14) and potential for health selection into labor market states (11).
Analysis
Poisson regression with robust error variance (32) was used to examine the relative association (risk ratios [RR] with robust 95% CIs) between labor market trajectories and health trajectories while adjusting for groups of conceptually related covariates, as identified above. Health trajectories were entered into the model as a series of binary contrasts. For the final model, the RR represents the estimated change in risk of experiencing a worsening (good to poor) or recovering (good–poor–good) health trajectory (compared with the reference category of stable good health), for each labor market trajectory (compared with the reference category of stable employment).
Separate models were estimated for each of the four study periods to examine the research question of whether relationships between LM-H trajectories differed across macroeconomic recession or expansion periods. As a sensitivity analysis, we incorporated interaction terms between labor market trajectories and study time period to assess the statistical significance (Wald F-test, P<0.05) of any modified relationships. We also calculated predicted probabilities (Pr) of being in each health trajectory using the coefficients from the final models.
Analyses were completed using Stata/SE 13.1 (College Station, TX). Survey weights were not used for this analysis, as this was a model-based approach (2).
Results
Table 1 provides a description of the baseline characteristics of the four working-age cohorts. Between 1988–2011, there was a shift in the age distribution towards older age groups. There were also increases in median family income in later versus earlier study periods, and increases in the proportion of higher educated respondents. Across study periods, there were differences in the distribution of race/ethnicity, number of children in the family unit, and marital status. There were no differences in the distribution of sex across periods.
Table 1
Descriptive statistics at baseline (column %) by study period: US Panel Study of Income Dynamics, 1988–2011.
| In good health and employed at baseline | 1988–1994 Recession a (N=3752) | 1993–1999 Expansion b (N=2744) | 1999–2005 Recession a (N=3387) | 2005–2011 Recession a (N=3702) |
|---|---|---|---|---|
|
|
|
|
|
|
| % | % | % | % | |
| Sex | ||||
| Female | 50.5 | 50.4 | 51.8 | 52.4 |
| Male | 49.5 | 49.6 | 48.2 | 47.6 |
| Age group (years) | ||||
| 15–24 | 6.8 | 5.1 | 4.8 | 4.3 |
| 25–34 | 36.4 | 31.9 | 24.7 | 27.3 |
| 35–44 | 29.3 | 33.0 | 34.8 | 26.8 |
| 45–54 | 15.9 | 20.3 | 26.0 | 27.8 |
| 55–64 | 11.5 | 9.6 | 9.8 | 13.7 |
| Health status prior to baseline | ||||
| Excellent/very good/good | 95.2 | 96.8 | 96.1 | 95.2 |
| Fair/poor | 4.8 | 3.2 | 3.9 | 4.8 |
| Race/ethnicity | ||||
| White | 67.8 | 72.2 | 67.2 | 65.3 |
| Black | 28.7 | 24.3 | 25.9 | 27.7 |
| Other | 3.5 | 3.6 | 6.9 | 7.1 |
| Children <18 years | ||||
| 0 | 47.5 | 47.6 | 45.7 | 50.6 |
| 1 | 21.1 | 18.8 | 22.1 | 19.7 |
| 2 | 19.8 | 22.0 | 21.1 | 20.0 |
| ≥3 | 11.6 | 11.7 | 11.1 | 9.8 |
| Education skill level | ||||
| Minimum | 13.8 | 9.2 | 10.5 | 9.5 |
| Medium | 59.7 | 61.0 | 57.7 | 57.3 |
| High | 26.5 | 29.8 | 31.8 | 33.2 |
| Marital status | ||||
| Married/cohabitating | 69.6 | 70.3 | 68.4 | 67.3 |
| Single | 13.1 | 14.0 | 15.2 | 17.3 |
| Widowed | 2.0 | 1.5 | 1.4 | 1.1 |
| Divorced | 10.3 | 10.2 | 11.2 | 10.8 |
| Separated | 5.0 | 3.9 | 3.7 | 3.5 |
| Census division | ||||
| New England | 4.1 | 4.0 | 3.8 | 3.2 |
| Middle Atlantic | 12.8 | 12.6 | 11.5 | 10.9 |
| East North Central | 14.8 | 17.3 | 16.9 | 16.4 |
| West North Central | 8.6 | 10.6 | 9.5 | 9.6 |
| South Atlantic | 24.9 | 21.6 | 22.3 | 23.3 |
| East South Central | 8.6 | 8.3 | 7.1 | 6.9 |
| West South Central | 10.1 | 9.4 | 9.2 | 9.8 |
| Mountain | 4.0 | 5.0 | 5.8 | 6.2 |
| Pacific | 12.1 | 11.2 | 13.9 | 13.7 |
| Health status trajectories | ||||
| Stable good | 84.5 | 88.7 | 85.4 | 85.0 |
| Good–poor | 9.6 | 7.2 | 9.1 | 8.6 |
| Good–poor–good | 5.9 | 4.1 | 5.5 | 6.3 |
| Labor market trajectories | ||||
| Stable-employed | 73.6 | 78.6 | 77.7 | 71.5 |
| Employed–unemployed–employed | 4.7 | 4.1 | 4.9 | 5.9 |
| Employed–inactive– employed | 3.9 | 3.8 | 4.1 | 3.3 |
| Employed–unemployed | 3.3 | 2.0 | 2.9 | 6.1 |
| Employed–inactive | 11.6 | 9.7 | 8.1 | 10.0 |
| Employed–unemployed/inactive | 2.8 | 1.8 | 2.3 | 3.2 |
Table 1 also presents the three clusters of health trajectories and six clusters of LM trajectories included in the analyses. The vast majority of individuals in the sample remained in good health across all follow-up waves (ranging from 85–89% across study periods), followed by worsening health trajectories (7–10%) and worsening-to-improving trajectories (4–6%). For LM trajectories, the majority of individuals in the sample reported stable employment across all follow-up waves (72–79%), followed by patterns of worsening labor market trajectories and worsening-to-improving LM trajectories.
Table 2 presents the RR for the association between LM-H trajectories, adjusted for all covariates and health status prior to baseline. Individuals with LM trajectories ending in unemployment (RR 1.73–2.51 across study periods), inactivity (RR 2.34–3.16) or a combination of unemployment and inactivity (RR 2.14–3.00) were more likely to have worsening health trajectories, compared to individuals with stable employment. In contrast, among individuals who became re-employed following an intermediary period of unemployment (ie, employed–unemployed–employed), the estimates for having a worsening health trajectory were attenuated towards a null difference across all periods. Among individuals who became re-employed following an intermediary period of inactivity (ie, employed–inactive–employed), the estimates were also attenuated towards the null, but remained statistically significant for 1988–1994 and 1993–1999 (RR 1.63 and 2.10, respectively).
Table 2
Adjusted risk ratios (RR) for the association between labor force and health status trajectories. Estimates are stratified by the four study periods. US Panel Study of Income Dynamics, 1988–2011. [Obs=observations; CI=confidence interval.]
| 1988–1994 Recession a | 1993–1999 Expansion b | 1999–2005 Recession a | 2005–2011 Recession a | |||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| Obs | RR c (95% CI) | Obs | RR c (95% CI) | Obs | RR c (95% CI) | Obs | RR c (95% CI) | |
| OUTCOME: Good-poor health trajectory d (versus stable good) | 3531 | 2632 | 3200 | 3468 | ||||
| Stable employed (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | ||||
| Employed–unemployed–employed | 1.54 (1.00–2.39) | 1.69 (0.97–2.97) | 1.24 (0.83–1.87) | 0.94 (0.58–1.52) | ||||
| Employed–inactive–employed | 1.63 (1.05–2.53) e | 2.10 (1.11–3.98) e | 1.29 (0.75–2.21) | 1.34 (0.74–2.41) | ||||
| Employed–unemployed | 1.73 (1.08–2.78) e | 2.51 (1.31–4.80) f | 2.49 (1.65–3.75) g | 1.96 (1.41–2.72) g | ||||
| Employed–inactive | 2.34 (1.80–3.03) g | 3.16 (2.20–4.54) g | 2.38 (1.80–3.14) g | 2.39 (1.80–3.19) g | ||||
| Employed–both unemployed/inactive | 2.59 (1.77–3.79) g | 1.78 (0.83–3.82) | 3.00 (1.95–4.59) g | 2.14 (1.49–3.08) g | ||||
| OUTCOME: Good–poor–good health trajectory h (versus stable good) | 3393 | 2546 | 3079 | 3382 | ||||
| Stable employed (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | ||||
| Employed–unemployed–employed | 1.71 (1.07–2.71) e | 2.00 (1.00–4.01) | 1.42 (0.83–2.42) | 1.37 (0.89–2.10) | ||||
| Employed–inactive–employed | 1.41 (0.76–2.61) | 2.32 (1.14–4.70) e | 1.23 (0.63–2.41) | 0.96 (0.48–1.91) | ||||
| Employed–unemployed | 1.12 (0.62–2.02) | 1.88 (0.67–5.30) | 1.04 (0.49–2.21) | 1.40 (0.89–2.18) | ||||
| Employed–inactive | 1.30 (0.87–1.94) | 2.44 (1.39–4.30) f | 1.60 (1.05–2.42) e | 1.51 (1.00–2.28) e | ||||
| Employed–unemployed/inactive | 3.00 (1.82–4.95) g | 1.98 (0.80–4.89) | 1.30 (0.57–2.96) | 1.69 (1.03–2.75) e | ||||
Figure 2 presents the predicted probabilities of being in each health trajectory in association with different LM trajectories. We observed a health gradient across LM trajectories. For example, stable-employed individuals had the highest probability of remaining in good health (ranging from 86–90% across study periods), whereas individuals with an employed–unemployed/inactive trajectory had the lowest probability of remaining in good health (65–79% across periods).
Figure 2
Predicted probabilities (%) of remaining in good health (Panel 1), having a good to poor health trajectory (Panel 2), and having a good–poor–good health trajectory (Panel 3), by labor force trajectories. Models adjusted for sociodemographic, work and economic characteristics, obtained via Poisson regression with robust error variance. Estimates are stratified by the four study periods. US Panel Study of Income Dynamics, 1988–2011.
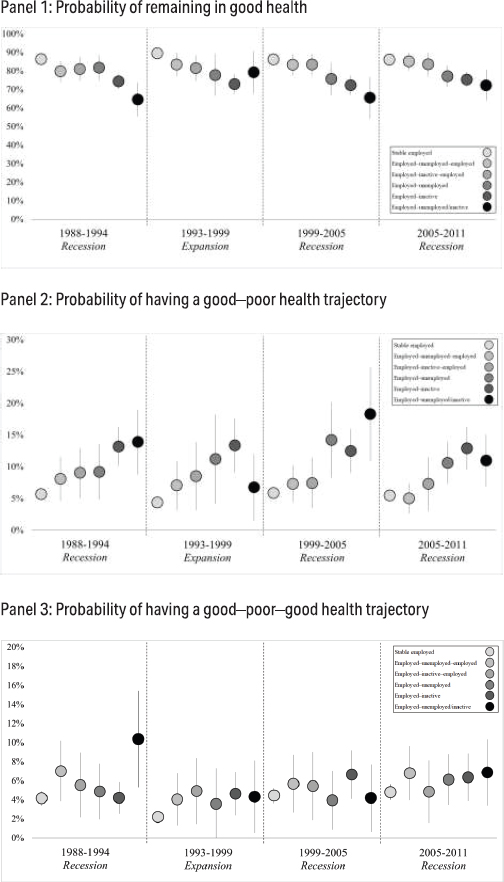
Across the four macroeconomic periods, we observed small differences in health outcomes among stable-employed individuals, with a greater probability of remaining in good health during the expansion study period (Pr 0.90, 95% CI 0.88–0.91) when compared to the recession periods (Pr 0.86 across each of the recession periods). Similarly, among individuals who exited the labor market, there was a greater probability of remaining in good health during the expansion study period (Pr 0.79, 95% CI 0.68–0.91) compared to the recession periods (Pr 0.65 to 0.72 across recession periods). However, in the sensitivity analyses where we tested for interaction between labor market trajectories and study time period, these modified relationships were not statistically significant overall.
Discussion
The objectives of our study were to (i) identify unique patterns of labor market and self-rated health (LM-H) trajectories, (ii) examine associations between these LM-H trajectories, and (iii) examine whether associations differed across macroeconomic recession and expansion periods in the US. Our study found a strong gradient in SRH, with a persistent trend of worsening health for individuals who progressed from employment–unemployment or employment–inactivity by the end of follow-up. We also observed an attenuated association between LM-H trajectories among individuals who returned to work following an intermediary period of unemployment or inactivity. Moreover, these overall relationships were consistent across each of the four working-age cohorts, with no statistically significant modification by contextual macroeconomic period.
Labor market and health trajectories
Similar to previous longitudinal studies that have examined LM-H trajectories (15, 16, 30), we found a strong association between patterns of worsening employment and worsening health. Sacker and colleagues (16) examined latent SRH trajectories using comparable extracts of household survey data from the United States and United Kingdom. The authors found that unemployment and inactivity at the start of follow-up were associated with worse health trajectories over time. Similarly, Virtanen and colleagues (15) examined the association between labor market trajectories and changes in SRH using data on Finnish public-sector employees between 1998–2002. Trajectories were defined by a combination of labor market status at the end of follow-up and levels of employment instability in the intervening periods. The authors found that trajectories ending in unemployment and/or containing employment instability were associated with poorer health, whereas trajectories consisting of stable employment were associated with better health.
Our finding of an attenuated association among individuals who returned to employment following an intermediary period of unemployment or inactivity (compared to those who remained unemployed or inactive at the end of follow-up) is also consistent with previous studies. Strully (10) examined involuntary job loss and SRH in the US using a similar extract of PSID data between 1999–2003. The author found that individuals who lost their job prior to the study period had worse health status, but that those who were re-employed by the end of the study were not at increased risk compared to individuals with stable employment. Thus, our findings of an attenuated (but not eliminated) risk among those returning to employment suggests that health outcomes are not only dependent on the LM end-state, but also on the distinct pattern over time.
Differences across economic cycles
Our results were supportive of the null hypothesis that there were no differential relationships between LM-H trajectories across macroeconomic cycles, and that individual labor market experiences exert a strong and persistent association with SRH trajectories independent of study periods. This finding is consistent with some (25, 33) but not all (12, 21, 23) studies. For example, studies by Urbanos-Garrido et al (25) and Arroyo et al (33) similarly found that recessions were not associated with worse employment-related declines in SRH compared to non-recession periods. The lack of effect-measure modification by contextual macroeconomic period in our study might be a reflection of our use of a global measure of health status. It is possible that the material impact of macroeconomic cycles may be detected using objective measures of health such as mortality (4, 13, 34). Moreover, our use of sequences of health states over time, rather than a single absolute measure, may have led to different associations (14).
Strengths and limitations
This study is one of the first to examine the health impacts of different labor market trajectories across macroeconomic cycles. The strengths of this study were the focus on creating detailed labor market trajectories using longitudinal data from before, during and after the onset of each macroeconomic cycle. The use of longitudinal data spanning 24-years of combined follow-up maximized our sample size and enabled us to examine whether the relationships between LM-H trajectories were modified across earlier or later economic cycles.
Our findings should also be interpreted in light of potential limitations. Given the complex and reciprocal relationships between unemployment and health (11, 31), health selection into unemployment may represent a source of bias or may account for some of the relationship between unemployment and health (35). Indeed, lagged health status two years prior to baseline was strongly associated with health status trajectories in our study. It may also be possible that the impact of health selection varies depending upon macroeconomic conditions (36) and that the bias may differ during severe recessions. Nevertheless, the relationships between labor market and health status trajectories remained consistent in the adjusted models that controlled for baseline health status. Moreover, previous studies (2, 10, 11, 37) have shown that the relationship between unemployment and health is robust to controls for health selection and that health selection explains only a part of the relationship.
There may also be limitations inherent to the observational design of our study, such as the omission of measured or unmeasured variables (eg, psychosocial work conditions) that may confound the relationships between LM-H trajectories, or concurrent changes over time in other unmeasured confounding factors (such as labor market or health insurance policies) (21). As well, some of the labor market trajectories were rarely observed in the study sample (eg, employed–unemployed/inactive), potentially limiting the precision of our estimates. Finally, this study may have limited generalizability to other health measures or specific dimensions of health given our focus on general health trajectories.
Concluding remarks
We found strong relationships between LM-H trajectories, which remained consistent across periods of economic contraction and expansion. The higher risk of having worsening health trajectories among unemployed or labor market inactive individuals, yet attenuated (but not eliminated) risk among individuals who returned to employment following these intermediary periods, suggests that health outcomes are not only associated with the labor market end-state but also with the distinct pattern of labor market states over time.