Young adults living with episodic disabilities can experience
unpredictable disruptions to their employment as they enter and advance
within the labor market. The most prevalent physical (e.g., juvenile
arthritis, inflammatory bowel disease) and mental health (e.g., anxiety,
depression) chronic conditions are often categorized as episodic, with
periods of good health interrupted by flares of poor health (1). Some estimates suggest one out of six
of working-aged adults with disabilities report fluctuating and
unpredictable limitations (2).
The unpredictability of an episodic disability can be stressful and
impact the health and quality of life of young adults. Finding and
sustaining employment can also be challenging, especially managing
fluctuations in symptoms while also navigating the changing demands of
work (3–5). Many episodic conditions have few visible signs
creating challenges communicating about work support needs (6, 7). Living and working with an episodic disability may
have different impacts at various life stages; difficulties at the early
career phase can have an economic scarring effect that impact both
employment opportunities and health across the life course (8, 9).
To manage their health and well-being, many young adults with episodic
disabilities rely on employment not only for income but also for resources
(e.g., extended health benefits, drug coverage) that may improve or
sustain good health (9). To examine
this further, our study reviewed employment and income support
interventions and their impact on the health and well-being of young
adults living with episodic disabilities.
Methods
A systematic review addressed the study aim (10). To inform the search strategy and synthesize key
findings, consultations with knowledge users were held. The review was
registered with PROSPERO (CRD42021268354) and met 2020 PRISMA
Guidelines.
Literature search
The search strategy captured employment or income support
intervention studies for young adults [i.e., sample mean age 16–35
(range 16–45) years] living with any episodic disability (Table 1). Our search was restricted
to intervention studies conducted in OECD countries, those that used
quantitative methodologies, and were published in the last 20 years in
English, French or Spanish. We examined the effect of employment or
income support inteventions on any health outcome. Medline, Embase,
PsycINFO, CINAHL, Sociological Abstracts, ASSIA, ABI Inform, and Econ
lit were searched using database-specific controlled vocabulary terms
and keywords (Supplementary material, www.sjweh.fi/article/4133,
Table S1).
Table 1
Inclusion and exclusion criteria using PICO
framework
|
PICO category |
Inclusion criteria |
Exclusion criteria |
|
Population |
Young adults (sample mean age 16-35 years and age
range 16 and 45 years)
Living with any episodic health
condition
Study sample located in an OECD labor market
country |
Study sample not classified as a young adult or
with an episodic disability
Study sample located in a
non-OECD context |
|
Intervention |
Any intervention that targeted
employment or income support |
Intervention with no employment
or income support component |
|
Comparison |
Any comparator group (population
not taking part or exposed to the intervention) |
No comparison group |
|
Outcome |
Any physical or mental health outcome, measure of
health-related quality of life or assessment of
well-being |
Studies evaluating the effectiveness of an
intervention which did not assess outcomes of interest |
Relevance screening
Two reviewers independently screened titles and abstracts and
full-texts for relevancy using DistillerSR (11). Disagreements were discussed in meetings.
Reference lists of included articles were checked to identify
additional relevant articles.
Quality appraisal and data extraction
A quality appraisal tool for studies in work and health was used to
assess the internal, external, and statistical validity of eligible
articles (10). The tool
assessed risk of bias in study design and objectives, recruitment
procedures, outcome and exposure measurement and analysis
(Supplementary Table S2). Two reviewers appraised each relevant
article. A final weighted sum score of the quality criteria was
generated, converted to a percentage score, and categorized as high
(≥85% of quality appraisal score), medium (50–84% of total quality
appraisal score) or low quality (<50% of quality appraisal total
score). Consensus on scores was reached in a team meeting.
Evidence synthesis
The limited number of eligible studies identified by the review
coupled with variability in the observation length, intervention type,
sample characteristics, outcomes meant that we were unable to
calculate pooled effect estimates. Instead, a narrative synthesis
described the findings.
Results
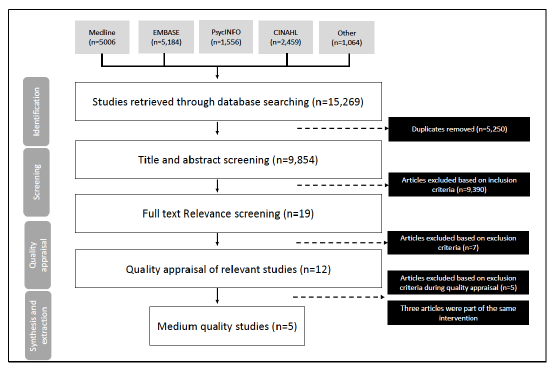
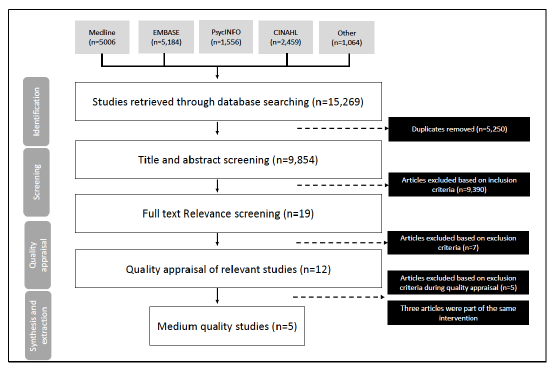
Our search yielded 15,269 articles published between years 2001–2021.
Only five eligible employment interventions focused on young adults with
an episodic disability and assessed health impacts (Figure 1). All
articles were appraised as medium quality. A summary of each study is
provided in Table 2.
Table 2
Description of studies identified in systematic review
examining income and employment interventions on health
Author,
Year,
Country |
Study objectives |
Study design, length of data collection, and
setting |
Sample size description |
Episodic disability group |
Employment and income outcomes (measures
utilized) |
Health and well-being outcomes (measures
utilized) |
Geenen
et al,
2015,
USA |
To examine whether youth who participated in the
Better Future’s project showed improved outcomes when compared
to youth randomized to a control group who were offered standard
services. |
Randomized
controlled trial
16
months
Community setting |
N=67 (36
intervention; 31
control)
Mean age 16.8 ± 0.62 years
52.2%
female |
Youth with mental health challenges in foster
care |
Employment status
Career decision
self-efficacy |
Improvements in mental health (Youth
Efficacy/Empowerment Scale- Mental Health)
Mental health
recovery (Mental Health Recovery Measure)
Hopelessness
(modified Hopelessness Scale for Children)
Quality of
life (Quality of Life Questionnaire) |
Liljeholm et al,
2020,
Sweden |
To determine how the Södertälje
Supported Employment and Education model, an integrated mental
health and vocational support intervention, can impact mental
health among young adults with mood disorders. |
Prospective Longitudinal pre-post
intervention study
12 months
Community
setting |
N=42
Mean age 21 (range
18–28)
years
64.3% female |
Young adults with major depressive
(93%) or bipolar disorder (7%) |
Engagement in everyday life
(Profiles of Occupational Engagement in people with Severe
mental illness [POES]) |
Mental health symptomology and
recovery (Montgomery-Asberg Depression Rating
Scale)
Quality of life (Manchester Short Assessment of
Quality of Life [MANSA]) |
Menrath
et al,
2019
Germany |
To study the efficacy and impact
of the Modular Transition (ModuS-T) patient education program,
designed to support young adults living with chronic conditions
manage their disease and transition to adulthood, when compared
to young adults in usual care. |
Quasi-randomized control
study
4 weeks
Clinical setting |
N=300
Mean age 17.6 ± 1.6
years
47% female |
Young people with chronic
conditions: asthma (5.3%), attention deficit disorder
/hyperactivity disorder (18.7%), type 1 diabetes (19.7%),
phenylketonuria (2.3%), inflammatory bowel disease (16.0%),
cystic fibrosis (2.7%), chronic kidney disease (4.0%), epilepsy
(7.7%), organ transplantation (7.3%), juvenile idiopathic
arthritis (7.7%), esophagus atresia (12.0%), Ehlers-Danlos
syndrome (2.7%) |
Work preparedness (Transition
Competency Scale) |
Health-related quality of life
(DISABKIDS Chronic Generic Measure; SF-8)
Self-reported
health
Engagement in health care (German Patient
Activation Measure for Adolescents)
Health
condition-related knowledge (Transition Competence
Scale)
Health care competence (Transition Competence
Scale) |
Kane et al,
2016
USA
Rosenheck et al,
2017
USA
Rosenheck et al, 2017
USA |
To compare the NAVIGATE
coordinated specialty care program on receipt of disability
income support benefits, employment, treatment and first-episode
psychosis outcomes when compared to usual community care. |
Clustered randomized
trial
24 months
Clinical setting |
N=404 (223 intervention; 181
community care)
Mean age: (intervention) 23.18 ± 5.21
years; (community care) 23.08 ± 4.90 years
27%
female |
Individuals with first episode of
psychosis |
Work participation
Number
of days participating in work
Receipt of disability
income support |
Schizophrenia symptom severity
(Positive and Negative Syndrome Scale)
Depression
symptoms (Calgary Depression Scale for
Schizophrenia)
Mental health illness severity (Clinical
Global Impressions Severity Scale)
Quality of life
(Heinrichs-Carpenter Quality of Life Scale) |
Sveindottir et al,
2020
Norway |
To study the role of the Individual placement and
support (IPS) approach for young adults with mental and
behavioural conditions, at risk of early work disability when
compared to traditional vocational rehabilitation. |
Two-armed randomized control trial
12
months
Community setting |
N=96 (50 intervention group; 46 control
group)
Mean age: (intervention) 23.96 ± 3.46 years
(control) 23.85 ± 3.04
32% female |
Individuals with mental and behavioral
conditions |
Paid competitive employment
Proportion of
participants working ≥20 hours per week
Total number of
hours worked |
Disability (World Health Organization Disability
Assessment Schedule [WHODAS] 2.0)
Psychological distress
(Hopkins Symptom Checklist)
Severity of subjective health
complaints (Subjective Complaints Inventory)
Fatigue
(Chalder Fatigue Questionnaire)
Coping, helplessness, and
hopelessness (Theoretically Originated Measure of the Cognitive
Activation Theory of Stress [TOMCATS])
Alcohol
consumption (Alcohol Use Disorders Identification Test
consumption questions [AUDIT-C])
Drug use (Drug Use
Disorders Identification consumption questions
[DUDIT-C])
Global well-being (Cantril Ladder Scale) |
Figure 1
Systematic review flowchart.
The five employment interventions found improvements in health
outcomes (Table 3). A randomized
controlled trial (RCT) of a personalized coaching initiative in the
United States offered mentorship to young adults with mental health
conditions to meet career and educational goals and build career
self-determination. Although the intervention did not contribute to a
change in employment over the six months following the ten-month
intervention period, it was associated with improved career
self-efficacy. Intervention recipients reported greater mental health
but no difference in quality of life when compared to the control group
(12).
Table 3
Description of study interventions and their impact on income
and employment outcomes and health outcomes
|
Study |
Description of intervention |
Intervention’s impact on income and employment
outcomes |
Intervention’s impact on health and well-being
outcomes |
Quality appraisal |
Geenen
et al, 2015 |
The Better Futures project is a personalized
coaching intervention program that provides foster youth with
mental health challenges to identify and work on their personal,
education or career goals, build self-determination skills
through mentorship workshops with advisory peers who have had
similar experience in foster care and dealing with their mental
health challenges. |
No significant difference in the proportion of
participants who were employed at follow-up when comparing the
intervention group to the control group.
Over the study
period, the intervention group reported significantly greater
career decision self-efficacy when compared to the control group
F (3, 124)=6.06; P=0.0007. |
Over the study period, the intervention group
reported significantly greater efficacy in mental health care
management when compared to the control group F(3, 118)=9.07;
P<0.0001).
While the intervention group reported
greater mental health recovery over the study period when
compared to the control group, the difference was
non-significant F (3, 180)=2.55, P=0.06).
There was no
difference between intervention and control groups in quality of
life over the study period F (3, 118)=2.29,
P=0.82).
There was a significant decline in hopelessness
among the intervention group, when compared to the control group
over the study period F (3, 62)=2.79, P=0.048). |
Moderate |
Lijeholm
et
al, 2020 |
The Södertälje Supported
Employment and Education model is an integrated intervention
targeted towards young adults with major depressive or bipolar
disorders to improve their mental health and support employment.
Intervention included integrated vocational services with mental
health services, personalized benefit counselling and employer
relationship building. All services were delivered by a case
manager and aligned with the client’s preferences and
needs. |
Participants reported
statistically significant improvements to engagement in everyday
life activities at 12-months when compared to baseline
(P=0.002). |
Although depression symptomology
decreased at follow-up when compared to baseline, the
relationship was not statistically significant
(P=0.241).
Participants indicated greater quality of life
at follow-up when compared to baseline (P=0.007).
At 12
months, participants who reported engagement in everyday life
activities were significantly less likely to report depression
severity (r=-0.313, P<0.05) and reported higher quality of
life (r=0.470, P<0.05). |
Moderate |
Menrath
et al,
2019 |
The Modular transition (ModuS-T)
education program aims at empowering patients with chronic
conditions to take responsibility in managing their disease.
Modules on insurance, the health care system, career, social
networking, coping and stress management, health promotion
behaviours, were delivered participants and their
parents/caregivers. Group discussions, role playing, and case
studies were utilized to deliver the training. |
Young adults in the intervention
group observed significantly greater scores for work
preparedness (TC-a) over the duration of the study when compared
to those in the control group F=27.3 (p < 0.001). |
No significant difference existed
when comparing the intervention group to the control group on
health-related quality of life when using the
DISABKIDS.
Young adults in the intervention group showed
significantly higher engagement in health care when compared to
the control group over the study period F=8.1,
P<0.001).
Young adults in the intervention group
showed significantly higher health condition-related knowledge
when compared to the control group over the study period F=22.9,
P<0.001).
Young adults in the intervention group
showed significantly higher health care competence when compared
to the control group over the study period (F=56.9,
P<0.001). |
Moderate |
Kane et al,
2016
Rosenheck et al, 2017
Rosenheck et al,
2017 |
NAVIGATE intervention is a
four-component training approach that includes: 1) customized
medication management training; 2) family psychoeducation 3)
self-management training focused on building resilience and 4)
supported employment and education. |
Compared to community care,
intervention participants were significantly more likely to
report work participation. However, the main effect by time was
most significant for those who participated in >3 supported
employment/education sessions (t=0.16, P<0.05).
No
significant differences between intervention and community care
when comparing number of days
in work (t=0.097,
P=0.16).
No significant differences between intervention
and community care when comparing receipt of disability income
support (t=4.25, P=0.71). |
Intervention participants
experienced significantly greater improvement in quality of life
over the study period than those in community care (t=2.45,
P=0.015).
Intervention participants reported a
significant decrease in schizophrenia symptom severity when
compared to those in community care (t=-2.41,
P=0.02).
Intervention participants indicated a
significant decrease in depressive symptoms when compared to
those in community care (t=-2.15, P=0.032).
No
significant difference in mental health illness severity between
intervention participants when compared to those in community
care over the study period (t=-1.52, P=0.13). |
Moderate |
|
Sveindottir et al, 2020 |
The individual placement and support (IPS) model of
supported employment is an intervention approach that is
targeted towards enhancing competitive employment outcomes for
patients with severe mental health illness through focusing on
patient goals and preferences, providing long-term personalized
support, access to integrated services and counselling. The
intervention was facilitated by a job specialist who matched the
candidate with a job and provided ongoing support following a
job through established IPS principles. |
IPS participants were significantly more likely to
hold competitive employment at 12-month follow-up compared to
the traditional vocational rehabilitation group (OR=10.39, 95%
CI 2.79-38.68).
A significantly higher proportion of IPS
participants reported working ≥20 hours per week at the 12-month
follow-up compared to the traditional vocational rehabilitation
group (OR=8.75, 95% CI 1.83-41.75).
A significantly
higher proportion of IPS participants reported working more
hours at the 12-month follow-up compared to the traditional
vocational rehabilitation group (Cohen’s D=0.70, p=0.002). |
Participants in the intervention group reported
significantly less health complaints (P=0.017), helplessness
(P=0.017) and hopelessness (P=0.006), and drug use (P=0.036)
when compared to the traditional vocational rehabilitation group
at 12-months.
Participants in the intervention group
reported significantly less disability (P=0.038) and greater
perception of future well-being (P=0.038) when compared to the
traditional vocational rehabilitation group at 12-months. |
Moderate |
Three supported employment interventions in community and clinical
settings for young adults with mental health conditions were identified
(13–15). The interventions provided employment placement
services, career counselling and health-related self-management
assistance. Findings highlighted improved occupational engagement,
participation in employment, and hours worked (13–15), as well
as improvements in quality of life and well-being, declines in
depressive symptom severity, fewer health complaints, and less
disability. Supported employment embedded within a specialty health care
program for individuals with psychosis and their families showed a
dose–response relationship such that attending a greater number of
sessions increased the likelihood of participating in employment (16). Intervention participants also
reported greater quality of life and a decrease in mental health
symptoms when compared to the control group.
Finally, a German patient education program within a clinical setting
for young adults with diverse chronic health care conditions (a majority
were episodic) included a specific career development module (17). Intervention participants were
more likely to report greater work-preparedness as well as better
health-related quality of life when compared to the control group.
Discussion
The unpredictable and dynamic nature of an episodic disability in
young adulthood can contribute to early and sustained exclusion from the
labor market and intermittently disrupt the pathway between employment
and health. Past research has highlighted the health-related benefits
attributed to promoting employment (18). This systematic review examined whether employment
or income support interventions could benefit the health and well-being
of young adults with episodic disabilities.
We found an absence of high-quality evidence-based employment or
income support interventions for young adults living with episodic
disability that focuses on health-related impacts. Only five studies
were identified which met our eligibility criteria, despite a large body
of research highlighting the importance of employment as a critical
social determinant of health in young adults with and without
disabilities (19, 20). Results underscore the need to
elaborate on the health and well-being implications of employment
interventions for young adults with different episodic health
conditions. Most interventions identified in our review focused on young
adults with mental health conditions. Findings could reflect a growing
acknowledgment of the relationship between poor mental health and
difficulties participating in employment among young adults (21, 22). Episodic disabilities like juvenile arthritis or
inflammatory bowel disease are among the most prevalent among young
adults and are characterized by variable physical symptoms (e.g., pain,
fatigue, and activity limitations) and can considerably impact
employment (3). Moving forward,
tailored interventions should be designed to account for the employment
challenges of young people living with diverse episodic health
conditions.
Although we uncovered a small body of evidence, our review suggests
that involvement in employment interventions could provide benefits for
the health of young adults with episodic disabilities, all interventions
included employment and disability-specific support components which may
have explained the health-related benefits. Interventions that promote
employment for young adults with episodic disabilities may benefit from
providing specific training on balancing health and work demands.
Additional longer-term research is needed to better understand the
elements of employment interventions that may be valuable to health, as
well as the reciprocal relationship between work and health outcomes
that can emerge over time. Participation in supported employment offers
a promising practice which may foster employment engagement and improve
health. Supported employment interventions aid with finding work and
they offer regular counselling and job-related training which has been
previously shown to be beneficial for the employment of young adults
with disabilities (23). As our
findings suggest, the benefits of supported employment interventions
could extend to health and well-being of young adults with episodic
disabilities at the early career phase.
The fluctuating nature of episodic disabilities represents a unique
challenge to sustaining employment (6). Interventions in our systematic review did not
explicitly address the varying activity limitations and employment
restrictions that can emerge. There is a need to study the unpredictable
employment challenges related to an episodic disability and develop
relevant programing tailored to those at the early career phase.
Additionally, most interventions focused on helping participants find
employment. There was limited focus on employment conditions, including
managing jobs of different quality, access to support and job
accommodations, and health and safety which may shape health outcomes.
For instance, young adults with an episodic health condition may
experience challenges finding full-time permanent employment that offers
income and resources that are beneficial to health (16). There is a need to expand
employment interventions to ensure young adults living with episodic
disabilities can navigate aspects of the work environment which could
pose challenges to sustained employment and also adversely impact
health.
A study strength includes a rigorous systematic review methodology. A
limitation of our systematic review is that we did not include
qualitative studies or grey literature. Capturing broader forms of
evidence can be used to elaborate on the different employment
intervention that can promote health.
Concluding remarks
Our systematic review highlights the need to elaborate on the
impact employment programs can have on the health and well-being of
young adults living with diverse episodic disabilities. Additional
insights are needed to understand how interventions can be designed to
tailor and expand employment services to young adults living with
episodic health conditions to fully optimize the pathways to better
health.
Funding statement
Dr. Jetha’s salary is partially supported by a Stars Career
Development Award (20-0000000014) from the Arthritis Society (Canada).
The funding body had no role in study design, data collection, data
interpretation or manuscript writing. Several members of the authorship
team are employees of the Institute for Work & Health, which is
supported through funding from the Ontario Ministry of Labour,
Immigration, Training and Skills Development (MLITSD). The analyses,
conclusions, opinions, and statements expressed herein are solely those
of the authors and do not reflect those of the MLITSD; no endorsement is
intended or should be inferred.
Competing interest
The authors declare no conflicts of interest.
Ethics approval
No ethics approval is required for the systematic review process.
References
Accommodating and Communicating
about Episodic Disabilities (ACED), Institute for Work & Health
(IWH). Project overview: what are episodic disabilities? [online].
2023 Available from: https://aced.iwh.on.ca/project-overview
Morris S, Fawcett G, Timoney
LR, Hughes J. The dynamics of disability: progressive, recurrent or
fluctuating limitations. Ottawa, ON: Statistics Canada;
2019.
Jetha
A,
Gignac
MA,
Bowring
J,
Tucker
S,
Connelly
CE,
Proulx
Let
al. Supporting arthritis and
employment across the life course: a qualitative
study. Arthritis Care Res (Hoboken)
2018
Oct;70(10):1461–8.
[CrossRef]
[PubMed]
Gmitroski
T,
Bradley
C,
Heinemann
L,
Liu
G,
Blanchard
P,
Beck
Cet
al. Barriers and facilitators to
employment for young adults with mental illness: a scoping
review. BMJ Open 2018
Dec;8(12):e024487.
[CrossRef]
[PubMed]
O’Brien
KK,
Davis
AM,
Strike
C,
Young
NL,
Bayoumi
AM.
Putting episodic disability into context: a qualitative
study exploring factors that influence disability experienced by
adults living with HIV/AIDS. J Int AIDS
Soc 2009
Nov;12(1):5. [CrossRef]
[PubMed]
Gignac
MA,
Jetha
A,
Ginis
KA,
Ibrahim
S.
Does it matter what your reasons are when deciding to
disclose (or not disclose) a disability at work? The association of
workers’ approach and avoidance goals with perceived positive and
negative workplace outcomes. J Occup
Rehabil 2021
Sep;31(3):638–51.
[CrossRef]
[PubMed]
Jetha
A,
Tucker
L,
Backman
C,
Kristman
VL,
Bowring
J,
Hazel
EMet
al. Rheumatic disease disclosure
at the early career phase and its impact on the relationship between
workplace supports and presenteeism. Arthritis
Care Res (Hoboken) 2022
Oct;74(10):1751–60.
[CrossRef]
[PubMed]
Jetha A, Gignac M. Changing
Experiences, Needs, and Supports Across the Life Course for Workers
Living with Disabilities. Handbook of Life Course Occupational Health
Handbook Series in Occupational Health Sciences. New York, N.Y.:
Springer; 2023. p. 1–22.
Strandh
M,
Winefield
A,
Nilsson
K,
Hammarström
A.
Unemployment and mental health scarring during the life
course. Eur J Public Health
2014
Jun;24(3):440–5.
[CrossRef]
[PubMed]
Geenen
S,
Powers
LE,
Phillips
LA,
Nelson
M,
McKenna
J,
Winges-Yanez
Net
al. Better futures: a randomized
field test of a model for supporting young people in foster care with
mental health challenges to participate in higher
education. J Behav Health Serv Res
2015
Apr;42(2):150–71.
[CrossRef]
[PubMed]
Liljeholm
U,
Argentzell
E,
Bejerholm
U.
An integrated mental health and vocational
intervention: A longitudinal study on mental health changes among
young adults. Nurs Open
2020
Jul;7(6):1755–65.
[CrossRef]
[PubMed]
Sveinsdottir
V,
Lie
SA,
Bond
GR,
Eriksen
HR,
Tveito
TH,
Grasdal
ALet
al. Individual placement and
support for young adults at risk of early work disability (the SEED
trial). A randomized controlled trial. Scand J
Work Environ Health 2020
Jan;46(1):50–9.
[CrossRef]
[PubMed]
Kane
JM,
Robinson
DG,
Schooler
NR,
Mueser
KT,
Penn
DL,
Rosenheck
RAet
al. Comprehensive versus usual
community care for first-episode psychosis: 2-year outcomes from the
NIMH RAISE early treatment program. Am J
Psychiatry 2016
Apr;173(4):362–72.
[CrossRef]
[PubMed]
Shahidi
FV,
Jetha
A,
Kristman
V,
Smith
PM,
Gignac
MA.
The Employment Quality of Persons with Disabilities:
Findings from a National Survey. J Occup
Rehabil 2023
Dec;33(4):785–95.
[CrossRef]
[PubMed]
Menrath
I,
Ernst
G,
Szczepanski
R,
Lange
K,
Bomba
F,
Staab
Det
al. Effectiveness of a generic
transition-oriented patient education program in a multicenter,
prospective and controlled study. J Transit
Med
2018;1(1):20180001.
[CrossRef]
Moore
TH,
Kapur
N,
Hawton
K,
Richards
A,
Metcalfe
C,
Gunnell
D.
Interventions to reduce the impact of unemployment and
economic hardship on mental health in the general population: a
systematic review. Psychol Med
2017
Apr;47(6):1062–84.
[CrossRef]
[PubMed]
Norström
F,
Virtanen
P,
Hammarström
A,
Gustafsson
PE,
Janlert
U.
How does unemployment affect self-assessed health? A
systematic review focusing on subgroup effects.
BMC Public Health 2014
Dec;14(1):1310. [CrossRef]
[PubMed]
Vancea
M,
Utzet
M.
How unemployment and precarious employment affect the
health of young people: A scoping study on social
determinants. Scand J Public Health
2017
Feb;45(1):73–84.
[CrossRef]
[PubMed]
Bartelink
VH, Zay
Ya K,
Guldbrandsson
K,
Bremberg
S.
Unemployment among young people and mental health: A
systematic review. Scand J Public
Health 2020
Jul;48(5):544–58.
[CrossRef]
[PubMed]
Fiori
F,
Rinesi
F,
Spizzichino
D, Di
Giorgio
G.
Employment insecurity and mental health during the
economic recession: an analysis of the young adult labour force in
Italy. Soc Sci Med 2016
Mar;153:90–8. [CrossRef]
[PubMed]
Jetha
A,
Shaw
R,
Sinden
AR,
Mahood
Q,
Gignac
MA,
McColl
MAet
al. Work-focused interventions
that promote the labour market transition of young adults with chronic
disabling health conditions: a systematic review.
Occup Environ Med 2019
Mar;76(3):189–98.
[CrossRef]
[PubMed]