Intervention effectiveness research is considered a priority area in occupational health (1). The physical and psychosocial workplace environment offers a crucial setting for improving the health of employed populations (2, 3). Although beneficial for all employees, the need to improve health at work is unequally distributed among employed populations. This is due to the well-established fact of a social gradient of health across the whole of a society. With each step up in the social hierarchy, the better the chances of good health (4, 5). Occupational groups with lower qualifications and occupational positions generally suffer from poorer health than those in higher positions (6, 7). As the quality of work and employment follows the same pattern of social distribution as health, leaving those in lower socioeconomic positions (SEP) in more stressful jobs (8, 9), there is a clear need to prioritize worksite interventions among occupational groups with lower socioeconomic standing and their specific occupational exposures (10).
However, when reviewing worksite intervention trials, this double burden of poorer quality of work and higher risk of ill-health among less-privileged occupational groups is rarely defined as a major challenge. Although several systematic reviews and meta-analyses have been conducted on the effects of workplace interventions (11–25), they fail to deal explicitly with the social gradient of health and poor quality of work.
In this review, we report the results of a meta-analysis of randomized controlled worksite interventions and their effects on health and well-being with a special focus on the social stratification of occupational target groups. Two research questions are addressed: (i) What is the social distribution of occupations included in randomized controlled worksite interventions? (ii) Do effect sizes differ between higher and lower SEP groups? The first objective aims to assess whether lower socioeconomic groups are being prioritized in intervention studies. The second addresses whether intervention effects are being moderated by socioeconomic class.
Methods
The extensive study protocol, search strategy, sensitivity analysis, quality of evidence, and detailed description of studies included in this systematic review are available as supplementary material (http://www.sjweh.fi/data_repository.php). This section is, therefore, restricted to the general selection criteria of the intervention studies and the methodology used to answer the two research questions mentioned above.
In order to achieve robust estimates of effect sizes (26), we aimed to identify only those studies which can be regarded as homogenous with respect to design and outcomes. First, only randomized controlled interventions at the workplace were included to allow the calculation of standardized mean differences (SMD). In order to assess the effect of interventions on healthy working populations, only primary interventions were selected (16). Furthermore, to decrease the small sample bias, studies had to provide a population size >80 (ie, ≥40 employees in each group) in order to be included. Second, we selected those studies whose outcome variables were highly similar or identical. The outcome variables included: (i) body mass index (BMI); (ii) fruit and vegetable consumption (measured in almost all studies by administering a validated screening instrument for daily servings of fruit and vegetables); (iii) musculoskeletal symptoms (self-reported upper-extremity symptoms, shoulder and neck and/or back pain symptoms); and (iv) perceived stress (assessment of operationalizations of self-reported levels of stress).
In line with our first research question, we applied the Erikson-Goldthorp-Portocarrero (EGP) occupational class categories to identify the SEP of the employees in each sample (27). However, due to a lack of specific information regarding the sample characteristics in many studies, only two major groups of SEP categories were defined: (i) EGP classes I–III: higher and lower service occupations, routine clerical, and sales occupations and (ii) EGP classes VI–VII: skilled, and semi- or unskilled manual occupations.
In dealing with differences in the scales of the instruments used for the measurement of outcome variables, SMD were estimated. For publications reporting means and standard errors in the intervention and control groups (26 effect sizes) Hedge’s g (ie, the SMD), was calculated and corrected for small sample size (28). For the remaining publications, appropriate transformation formulae of effect sizes were utilized (29–32).
Due to large heterogeneity, random-effects models were calculated by the restricted maximum-likelihood estimator (33). All models were calculated using the R-package metaphor (34).
Results
After checking for duplicates, the manual search and queries in the databases generated a total of 18 132 initial records. After applying the study selection criteria (briefly mentioned in the Methods section), 104 studies were selected for full analysis. Finally, 36 randomized controlled interventions and 40 reported measurements were considered for the meta-analyses.
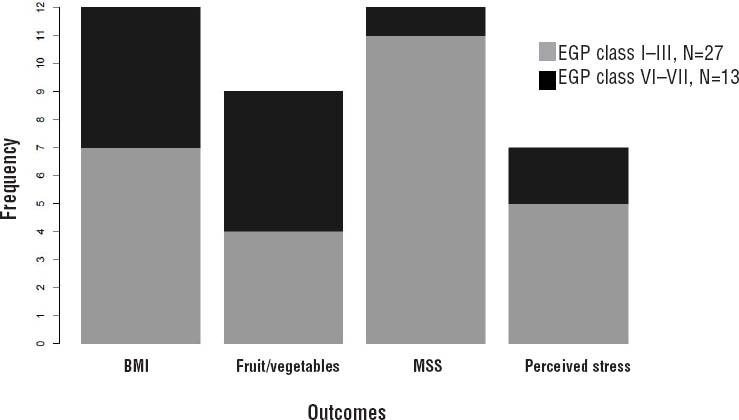
Regarding the first research question, the frequencies of reported outcomes within the different EGP occupational classes are displayed in figure 1. The number of interventions among occupations belonging to EGP classes I–III is twice as high as the number of studies conducted among classes VI–VII. In particular, this difference is due to a larger number of studies dealing with musculoskeletal disorders and perceived stress within EGP classes I–III.
Figure 1
Number of outcomes reported in the 36 intervention studies of the meta-analysis within each Erikson-Goldthorp-Portocarrero (EGP) occupational class. [BMI=body mass index; MSS=musculoskeletal symptoms]
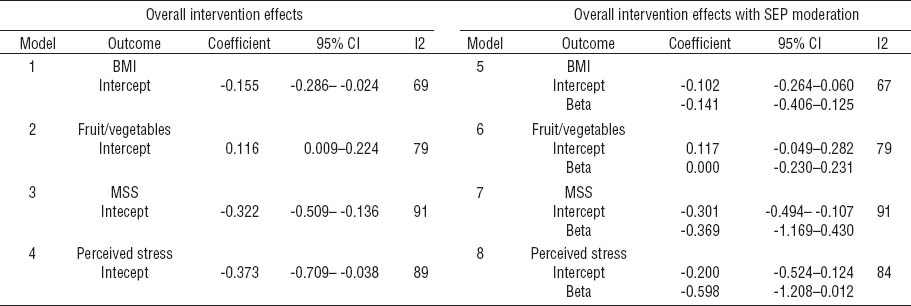
Concerning the second research question, we estimated eight random-effects models that are reproduced in table 1. The first four models did not take SEP into account, whereas the remaining models include SEP as a moderating variable. The intercept is the estimate of the overall effect size (Hedge’s g), and the beta coefficient is an estimate of the effect differences between EGP classes. Workplace interventions in models 1–4 resulted in significantly decreased BMI values, increased intake of fruit and vegetables, decreased level of self-reported musculoskeletal symptoms, and decreased perceived stress. The inclusion of SEP as moderating variable in models 5–8 resulted in a slight decrease of the intercepts [ie, the overall effect sizes, except for musculoskeletal symptoms, even though the proportion of heterogeneity (column I2) remained large]. The results do not show a moderation effect exerted by SEP, as can be seen from the large confidence intervals of the beta coefficients.
Table 1
Eight random-effects models of effect sizes (Hedges g) with and without socioeconomic position (SEP) as moderating variable. The intercept correspond to the overall effect size (Hedges g) for each outcome. The reference category in the moderation models 5–8 consists of Erikson-Goldthorp-Portocarrero (EGP) classes I–III. The coefficient beta corresponds to the average intervention effect differences between EGP classes. [BMI=body mass index; MSS=musculoskeletal symptoms; 95% CI=95% confidence interval]
Discussion
We addressed two questions in this review: (i) What is the social distribution of occupations included in randomized controlled worksite interventions? and (ii) Do effect sizes differ between higher and lower SEP groups? Concerning the first question, the results indicate that more than twice as many intervention trials were conducted among higher than lower skilled occupational groups (EPG classes I–III versus VI– VII), especially for musculoskeletal disorders and perceived stress. Therefore, prioritization of intervention activities according to socially unequal needs has not been a major concern in this area of research. We were unable to find a clear answer to the second research question given the lack of statistical power in our study, which prevented the estimation of occupational class differences.
However, even though the random-effects models controlling for the moderating effect of the EGP classes do not demonstrate statistically significant intervention effects, the corresponding regression coefficients in table 1 suggest lower intervention effects in EGP classes VI–VII in comparison to I–III. For instance, this would imply that for BMI there might be, on average, a 14.1% intervention effect reduction for occupational classes VI–VII.
Finally, some limitations of this analysis need to be mentioned. First, relevant studies may have been omitted as a consequence of the keywords selected in the search strategy. Second, concerning the moderating effect of occupational class, all corresponding random-effects models had low degrees of freedom, especially for the model of perceived stress with only seven studies available, whereby a consistent estimation of mediation effects and corresponding confidence intervals cannot be satisfactorily attained. Third, it should be kept in mind that the sample description in terms of occupational class was very heterogeneous, thus limiting the validity of the applied EPG classification.
In conclusion, the meta-analysis of 36 randomized controlled worksite intervention studies revealed small, but significant effects on four relevant health outcomes: weight reduction, healthy nutrition, reduced musculoskeletal symptoms, and lower levels of perceived stress. As only few studies were conducted among employees with lower socioeconomic standing, the challenge of reducing work-related health inequalities by targeting health-promoting activities at occupational groups with high needs remains largely unmet. Due to lack of statistical power, our study could not confirm a moderation of intervention effects by occupational class. Nonetheless, future research should aim at bridging worksite intervention research with scientific inquiry into social determinants of health.



