Several studies from earlier decades suggest that long working hours and prevalent physical workplace exposures, such as lifting and standing, may increase the risk of adverse pregnancy outcomes, but evidence on this is conflicting (1, 2). Occupational physicians, general practitioners, midwives, and obstetric specialists all need to counsel pregnant workers appropriately when there is concern about such risks (3). This in turn requires an evaluation of current evidence. Recently, we conducted reviews with meta-analysis to assess the evidence on common working conditions and risk of preterm delivery, small-for-gestational-age, low birth weight, and gestational hypertension (4, 5). This paper extends the work by systematically appraising the current evidence on miscarriage.
Miscarriage is defined here as fetal death in-utero, between the time of clinical recognition of pregnancy and the gestational week at which it is presumed that survival outside the uterus is possible (recognized miscarriage) (6). Almost one-third of human embryos surviving the first four weeks after fertilization are lost – some two-thirds before a clinical pregnancy is recognized and one-third during the time window from clinical recognition of pregnancy until the 28th week of pregnancy. This corresponds to a prevalence of miscarriage among humans in the range of 10–14% (7, 8). A large proportion of subclinical embryonal losses arise from chromosomal abnormality, although some 50% of miscarriages have a normal karyotype. Unlike late miscarriage (after the 20th week of gestation) and stillbirths, the frequency of early embryonal loss and early miscarriage has changed little over time (6). Higher maternal age is a strong risk factor that appears, according to evidence from in-vitro fertilization, to be related to the quality of the ovum rather than the woman’s capacity to carry a pregnancy. Miscarriage is prevalent and clustering in workplaces is not uncommon, sometimes raising understandable concerns about known and potential occupational hazards. The aim of this paper is to synthesize current evidence on the risk of miscarriage associated with shift work, long working hours, lifting, standing, and physical workload, and thereby to provide an updated basis for appropriate counseling of pregnant women, employers, and health professionals. We adhere broadly to review and meta-analysis methodologies developed previously in relation to other adverse pregnancy outcomes (4, 5).
Methods
Literature search and selection of papers
We conducted a search in Medline and EMBASE of peer-reviewed papers in English published between January 1966 and June 2012 to identify original research papers providing a risk estimate of miscarriage according to the five occupational activities of interest (shift work, working hours, lifting, standing, and physical workload). We combined medical subject headings and generic terms for the exposures and outcome (defined as miscarriage, spontaneous abortion, fetal death, stillbirth). This yielded 795 hits in all after excluding duplicates. After sifting the titles and further excluding irrelevant hits, we reviewed the abstracts of 90 potentially relevant original articles, of which 57 were retrieved in full. Among these, several reports failed to provide quantitative estimates of risk and a few were reviews: we selected those 22 epidemiological studies that provided ≥1 risk estimate for miscarriage in relation to ≥1 of the 5 reviewed occupational activities. Screening of the bibliographies of retrieved primary reports and reviews resulted in 8 additional papers, so the final database comprised 30 original publications (9–38). (No attempt was made to retrieve papers from the unpublished literature.)
Quality assessment
Reporting
Each publication was evaluated for completeness of reporting by considering the following study characteristics suggested by Bonzini et al (4, 5): (i) study design, (ii) sampling procedure, (iii) inclusion and exclusion criteria, (iv) distribution of age, social class, and induced abortions, (v) numbers and response rates (>70%), (vi) assessment of exposure, (vii) ascertainment of outcome, (viii) statistical analysis, and (viiii) quantitative risk estimates with 95% confidence intervals (95% CI). We evaluated whether each of these study characteristics was described in sufficient detail to allow for independent replication and evaluation of the study and assigned a value of 1 if the criterion was fulfilled and 0 if not. Giving equal weight to each of the 9 characteristics, we considered completeness of reporting as sufficient if the sum of the 0/1 scores for each exposure-outcome combination was ≥7 (4, 5).
Confounding
Surprisingly few determinants of miscarriage are well established besides age, social class, and earlier miscarriage (6). The rate of miscarriage increases dramatically after about 30 years of age (39). While it is not straight forward to account for effects of earlier miscarriage (which may be related to exposure) (6), studies that did not adjust for differences across exposure categories both in maternal age and social class were considered to be at higher risk of confounding. Weak and/or uncertain risk factors such as paternal age, maternal smoking, consumption of coffee and alcoholic beverages, earlier induced abortion, exposure to lead and mercury, infections, malformed uterus, and poorly controlled diabetes were not considered.
Bias
Observational studies addressing risk factors for miscarriage may potentially be biased by several factors. First, differential recall of exposure may inflate the relative risk (RR) if data on exposure are collected by self-report after the miscarriage event has occurred (40, 41). Women experiencing such a serious health event may be more prone to report an exposure than other women, especially if an occupational exposure is suspected to be a hazard (which may be a particular concern of healthcare workers) but also if (i) the time span between exposure and outcome is lengthy (allowing greater time for rumination and biased recall to develop), (ii) there is retrospective recall of exposures that are themselves subjective and less factual (eg, the degree of lifting or workload), and (iii) the outcome is self-reported and based on recall. Inflationary bias (bias that tends to cause an overestimation of risks) can also arise through a form of “unhealthy worker effect”: women who experience an adverse pregnancy outcome, or who are subfertile, may tend to remain in work to a greater extent than women delivering a healthy child and also be at greater risk of future adverse pregnancy events. Risk estimates based upon analyses of subsequent pregnancies may be inflated (42), a problem that is partially avoidable by restricting analysis to first pregnancies. Studies that included non-workers as well as unexposed workers among the referent group were potentially prone to a similar type of bias. By contrast, non-differential misclassification can cause bias to the null when exposure assessment, blinded to outcome, is based upon crude job-exposure matrices or the judgment of third parties (eg, senior nurses and factory physicians) and blurs exposure contrasts. Certain other potential biases were identified, for which we lacked data, and are detailed later in the discussion section.
As most studies identified by this review were retrospective with self-recalled exposures, potential for inflationary bias is of special concern. We rated this on a 4-point scale: likely (++), possible (+), neither likely nor unlikely (+/-), and bias towards the null (-), according to the number of the following criteria present: (i) recall of exposure after the miscarriage event (a) for lifting, standing, or physical workload or (b) with a recall period >2 years (all exposures); (ii) self-reported outcome; (iii) analysis not restricted to first pregnancy (or with no sensitivity/stratified analysis relating to first pregnancies); (iv) reference group included women who were not working; (v) exposure classification based on a job-exposure matrix or a third-party opinion. Criteria (i–iv) were considered to increase the potential for inflationary bias and criterion (v) to cause potential bias to the null. The final score did not reflect a simple sum of each individual item but rather a judgment informed by them, scored independently by reviewers with differences resolved by consensus.
Meta-analysis
We computed a common risk estimate across studies with fairly uniform definition of occupational activity by weighing the RR or equivalent [odds ratios (OR) and hazard ratios (HR)] by the inverse variance. Uniform definition of occupational exposure was the sole criterion we applied in selecting studies for meta-analyses. Completeness of reporting, bias, and confounding was considered, however, in sensitivity analyses. Fixed effects estimates are presented unless a test for heterogeneity was positive, in which case a random effects model was chosen. In sensitivity analyses, for each exposure analyzed, we focused on the subset of studies with high completeness of reporting and lower risk of bias and confounding as defined above. Additionally, in case healthcare professionals, who represented an important proportion of all subjects, were more likely to suspect that work posed potential risks of miscarriage (or, conversely, were more precise in their recall), we conducted a sensitivity analysis in which meta-estimation of risks was repeated after excluding studies of medically qualified healthcare workers.
All statistical analyses were performed using SAS software (SAS Institute, Cary, NC, USA) and the Comprehensive meta-analysis program version 2009 (43, 44). We also used this software to output funnel plots of the standard error by the logarithm of the RR separately for each of the exposures and the higher quality studies, and inspected the plots for evidence of publication bias.
Results
We identified 4 prospective cohort studies, 15 case–control or retrospective cohort studies and 11 cross-sectional studies, altogether 30 original papers that explicitly or implicitly reported the risk of miscarriage according to ≥1 of the 5 occupational activities of interest (table 1). Half of these studies were performed in Nordic or other European countries. Eighteen studies concerned specific occupational groups, such as nurses, physiotherapists, midwifes, textile and agricultural workers, while 12 studies addressed the general population. Sample sizes were >1000–>30 000 women in 18 studies (9–14, 16–17, 19–21, 24–26, 32–35), but <200 in 4 studies (15, 18, 27, 30). Eleven studies included more than one pregnancy per woman in analyses (10–13, 23–26, 29, 34, 38) while others addressed an ongoing, the latest, or a randomly selected pregnancy (30–32). Response rates at baseline or follow-up were >80–90% in ten studies (33%), but <70% in five studies and uncertain in five other studies.
Table 1
Occupational activities and miscarriage. Characteristics of the 29 included studies [gw=gestational week; nd=not defined; ICD=International Classification of Diseases; RR=relative risk; SA=spontaneous abortion]
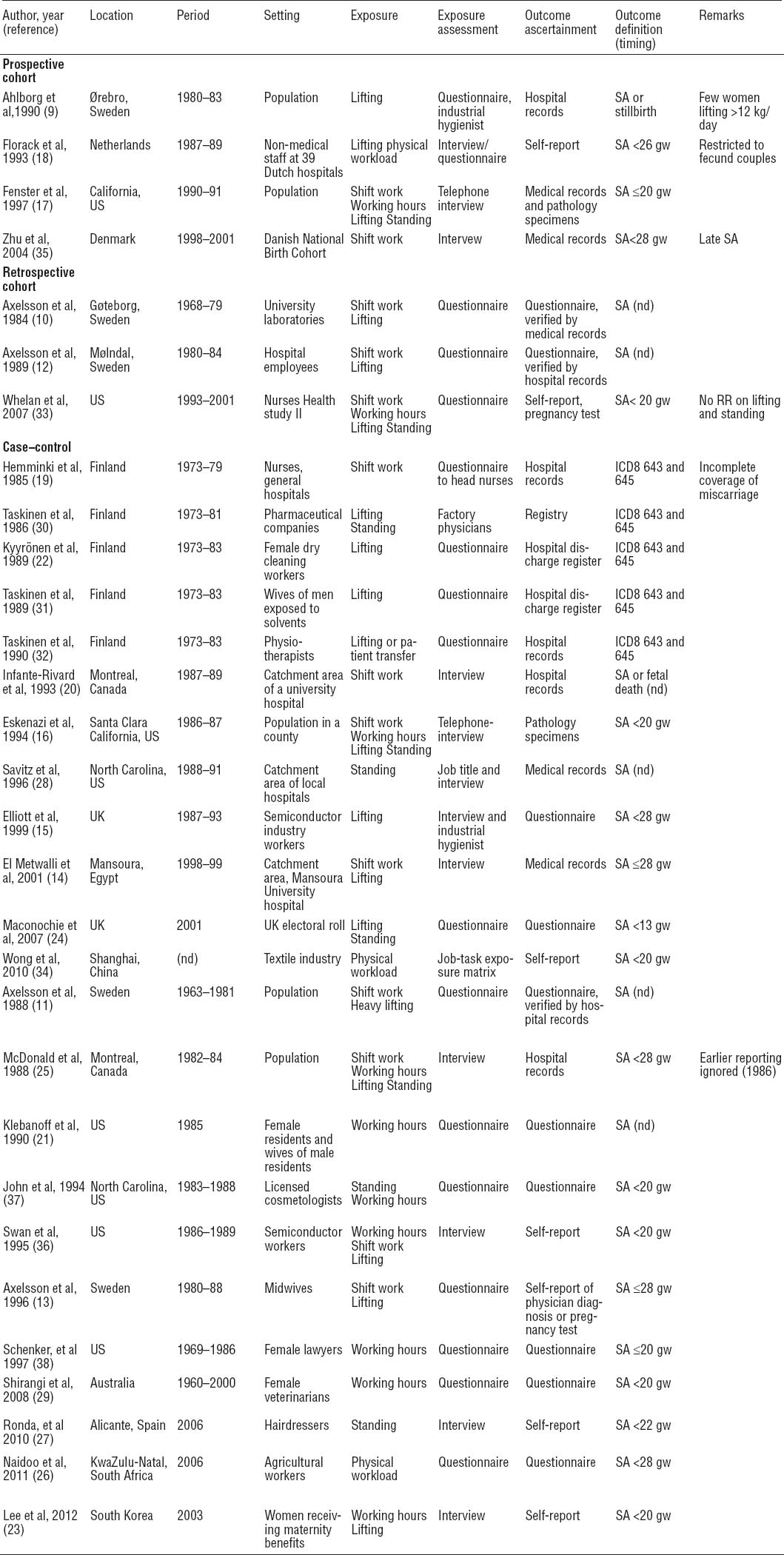
In most studies, miscarriage was defined as spontaneous fetal loss between clinical recognition of pregnancy and the 20–28th gestational week, although seven studies did not specify the timing of miscarriage (table 1). Only six studies provided risk estimates for early and/or late miscarriage, which was too few to allow for separate meta-analyses (13, 24, 31–33, 35). One of these, a large prospective study, preferentially included late spontaneous abortions because most pregnant women were enrolled after the first trimester (35). Miscarriage ascertainment was based upon women’s recall of earlier pregnancies in 13 studies including the 7 published after 2007 (table 1).
Data on occupational activity was obtained by self-reports in 24 studies, from information from managers and/or industrial hygienists in 4 studies, and application of a job-exposure matrix in 2 (table 1). Direct measurements of exposures were applied in only one fairly small prospective study on physical workload (18). Most studies collected data on activity during the first trimester of pregnancy, but seven studies did not provide detailed information on the timing of exposure (14, 20, 21, 23, 25, 26, 29).
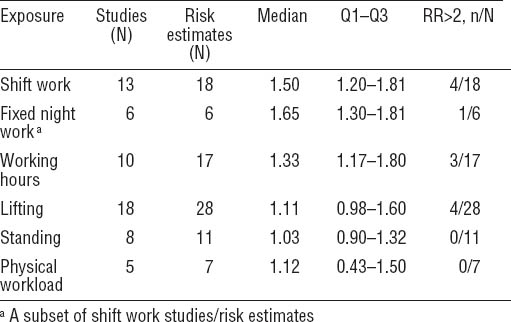
In all, the 30 studies provided 55 estimates of effect relating to the 5 exposures of interest (if a study provided >1 estimate for an exposure, we chose the risk estimate associated with the highest category of exposure). We assessed the potential risk of inflationary bias as low (-, +/-) for 15 (28%), as possible (+) for 17 (31%), and as likely (++) for 22 (41%) of these risk estimates. In subsequent analysis, as few estimated RR per exposure had low potential (+/-) for such bias, we counted those with a bias score of -, +/-, or + as providing the “better” available estimates of effect.
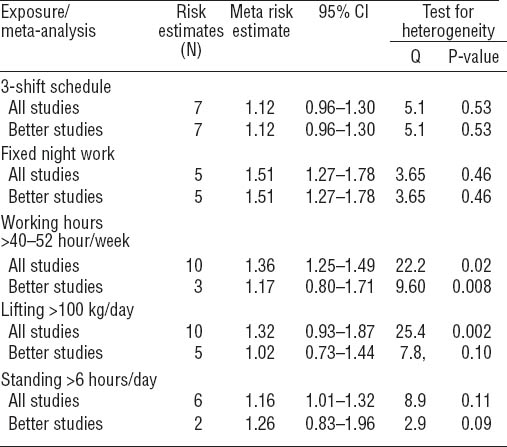
An overview of eligible studies is given in table 1. A summary of risk estimates is given in table 2 (for all studies) and table 3 (for meta-analyses). Finally, in supplementary tables A–E (see Appendix: http://www.sjweh.fi/data_repository.php), we provide detailed risk estimates for each exposure together with our assessment of potential biases.
Table 2
Summary of risk estimates across all identified studies according to type of occupational exposure [RR=relative risk].
Shift work
Thirteen studies (10–14, 16–17, 19–20, 25, 33, 35–36) provide risk estimates for women working shifts (supplementary table 4), with estimates of RR >1 in all but 2 studies (12, 16); a further study reported that RR were not increased but did not provide the associated risk estimate (44) (this was excluded from further consideration). The pooled fixed meta OR for the seven studies reporting risk of miscarriage among women with 3-shift schedules (rotating shifts including night) or evening/night shifts as compared with women not working at night (day workers or 2-shift workers) was slightly increased (OR 1.12, 95% CI 0.96–1.30) without indications of heterogeneity across studies (table 3). The estimated RR was not much altered by excluding the two studies that did not explicitly address 3-shift work (OR 1.19, 95% CI 0.99–1.42). The overall fixed model OR for miscarriage in the subset of five better quality studies reporting RR for fixed night compared with day work was 1.51 (95% CI 1.27 –1.78). Meta-estimates were not sensitive to omitting studies one by one.
Long working hours
Ten studies (16–17, 21, 23, 25, 29, 33, 36–38) examined the risk of miscarriage according to long weekly working hours (supplementary table B). The pooled risk estimate for women working ≥40–52 hours a week versus women working <40–44 hours was 1.36 (95% CI 1.25–1.49), but results were rather heterogeneous and the sensitivity analysis, which involved only three studies of higher quality (16, 17, 33) produced a lower point estimate with widened CI (OR 1.17, 95% CI 0.80–1.71), table 3.
Lifting
Risk estimates for occupational lifting of objects and/or patient transfer operations were available in 18 studies: 14 during the first trimester of pregnancy (9–13, 15, 17–18, 22, 24, 30–32, 36) and 4 during broadly defined or unclear exposure windows (14, 16, 23, 25) (supplementary table C). A further study reported that risks were not increased but did not provide the associated risk estimate (33) (this was excluded from further consideration). Results across studies were highly heterogeneous, with RR ranging from <0.5– >3.5. Studies used widely different definitions of heavy load [varying from >5kg (23) to >20 kg (22)], and frequency of daily lifting (from >6 times per day to >50 times per week). For purposes of meta-analysis, we defined heavy lifting by the product of weight and frequency (total burden lifted during a working day) and identified ten studies that provided risk estimates for lifting ≥100 kg/day in comparison with women with no daily lifting or lifting a smaller amount. The pooled OR, using a random effects model because of heterogeneity, was 1.32 (95% CI 0.93–1.87), but the sensitivity analysis, omitting five studies with highest risk of bias (25, 45–48), produced a pooled RR close to unity (RR 1.02, 95% CI 0.73–1.44) (table 3). The latter was not sensitive to omitting studies from the model one by one.
Standing at work
Eight studies (16–17, 24–25, 27–28, 30, 37) provided risk estimates for prolonged standing at work (supplementary table D). A further excluded study reported that risks were not increased but did not provide the associated risk estimate (33). The pooled RR for those six studies involving standing for ≥6–8 hours a day in comparison with women standing for <6–8 hours was 1.16 (95% CI 1.01–1.32) (table 3). Only two studies were considered of higher methodological quality: a large prospective study with a RR of 1.03 (95% CI 0.73–1.46) for standing >7 hours a day versus <3 hours (17) and a case–control study with a RR of 1.6 (95% CI 1.1–2.3) for standing >8 hours a day versus <3 hours (16).
Physical workload
Five studies (17–18, 25–26, 34) provided seven risk estimates in all for physical workload, with rather heterogeneous findings (supplementary table E). Physical workload is an ill-defined concept and studies applied different measures ranging from crude self-reports to elaborate measures based upon calculated energy expenditure (18). Two prospective studies found a marginally increased risk (17, 18). Pooled analysis was not considered appropriate in view of the different measures of exposure employed in these studies, but the median RR across all risk estimates was 1.12 and 0 of the 7 estimates exceeded 2.0.
Meta-analyses excluding studies of healthcare professionals (12, 13, 19, 21, 29, 32) did not produce systematically lower pooled estimates of miscarriage risk in relation to the four occupational exposures for which meta-analysis was appropriate (data not shown).
Discussion
We computed pooled risk estimates for miscarriage in relation to four prevalent occupational activities and found elevated RR in the range of 1.12 (3-shift schedules) to 1.51 (fixed night work). For long working hours and lifting, the pooled risk estimates fell to lower and statistically non-significant levels when analysis was confined to studies of higher quality. For prolonged standing, the pooled risk estimate was significantly elevated, but only two of five studies were of better quality. For physical workload, too few studies employed similar definitions of exposure to allow for meta-analysis, but the median RR across all studies was only 1.12.
Small risk increments in observational studies, in the range of 10–30%, may arise from uncontrolled bias or residual confounding. It is noteworthy in this respect that only four studies were of prospective design. In the remaining retrospective cohort, case–control and cross-sectional studies, potential existed for asymmetry of recall of occupational activities across exposure groups (41). Such recall bias, although perhaps having a smaller impact than generally supposed (45), could still account for part of all of the small effects observed, especially in studies addressing pregnancies several years back in time. This concern can only be remedied through prospective data collection or independent measurement of exposures in retrospective studies enjoying good response rates. That few studies fulfill these requirements is a major limitation of the current evidence base and one that may have led to some overestimation of risks.
As highlighted in the methods section, RR may also have been overestimated in other ways related to various forms of the “unhealthy worker” effect. Overall, we assessed only 15 of 54 risk estimates as having minimal potential for inflationary bias, and our definition of “better” studies was necessarily predicated on including 17 estimates with some potential for this bias (bias score +), owing to the otherwise small pool of high quality estimates. Additionally, funnel plots presenting RR of studies by their standard errors suggested that larger studies generally had risk estimates closer to unity, with some funnel asymmetry, further indicating potential for overestimation of risks through publication bias.
Certain other biases and errors may have existed that are less easy to evaluate and which further limit the available evidence base. One uncertainty arises from variations in definition of exposures and outcomes. Thus, while studies were generally complete in their essential details of reporting, several failed to provide sufficient information about the occupational exposure(s) of interest. All studies defined miscarriage similarly in relation to clinically recognized pregnancies, omitting early and subclinical fetal death and stillbirth, but case definitions differed at their upper cut-point (from the 20–28th weeks of gestation). The prevalence of miscarriage declines strongly with increasing gestational age. Thus, differences in case definition could hinder comparison between studies, although only to the extent that exposures differ in their effect on late versus early miscarriage.
A second uncertainty arises because only six studies distinguished between early and late miscarriage events, either by study design (35) or by stratified analysis (13, 16, 17, 25, 33). The proportion of chromosomally abnormal fetuses underlying miscarriage falls sharply with gestational age: thus, in theory, stronger associations with environmental exposures may be detectable if analysis is confined to late miscarriages of normal karyotype (assuming effects that are independent of DNA or chromosomal damage). However, the data were too sparse to explore this possibility.
A third limitation was that information on induced abortions (which may be more prevalent than miscarriage in some calendar periods and settings) was typically absent. Although induced abortion does not predict miscarriage in subsequent pregnancies (6), large differences between exposure groups in frequency of induced abortion can still bias risk calculations (46). This phenomenon arises as abortions tend to be induced after the peak risk period for early miscarriage, and thus in pregnancies that would otherwise carry a lower overall risk of miscarriage. This “induced abortion” bias would tend to generate higher estimates of miscarriage risk in a group with more terminations by underestimating the proportion of pregnancies that could otherwise conclude in a live birth. The potential for this inflationary bias can be addressed through prospective studies that record induced abortions, but not in case–control and cross sectional studies that differentiate only between miscarriages and live births.
Finally, no studies accounted for sick leave during pregnancy, which in some countries is substantial relative to sick leave among non-pregnant women (47); and only a few studies specified whether women were in full- or part-time work. These factors may result in less exposure than supposed, with potential bias to the null. Exposure definitions for lifting and physical workload were highly heterogeneous and perhaps difficult for women to recall, and this too may have caused some bias to the null, the extent of which is hard to gauge.
A notable finding of this meta-analysis – albeit based upon only five studies, of which four had potential for inflationary bias (bias grade +) – was a moderately increased risk of miscarriage among fixed night workers (RR 1.51). Night workers may differ from day workers (the main reference category) with respect to lifestyle factors and reproductive health (49), so selection bias may also partly explain this association, despite comprehensive analyses of extraneous factors in several of the studies. As mentioned in various reviews on reproductive health, a major limitation in evaluating shift-work arises because of the differing definitions of shift work across studies (1, 4). For this report, we analyzed risk estimates for 3-shift schedules as these were reported in many studies, but even 3-shift schedules encompass differing work patterns and the frequency of night shift working was not taken into account.
The mechanisms that might underlie a causal link between work at night and miscarriage are speculative at present. Repeated disruption of circadian rhythm among night workers is associated with reduced or changed secretion of melatonin and sleep deprivation, which could interfere with sex hormone homeostasis, implantation, and fetal growth (48). In this regard, the potent estrogen diethylstilbestrol is known to increase the risk of spontaneous abortion when administered during pregnancy (49).
A moderately increased risk of miscarriage was found overall in relation to long working hours, but risk estimates were lower in the three studies of better quality (16, 17, 25). Most investigations encompassed rather limited contrasts of exposure, but that of Klebanoff et al (21) was exceptional in studying women medical residents working an average of about 75 hours per week. In comparison with the wives of male residents, these hard-working newly educated medical doctors did not have an increased risk of miscarriage. Recall bias is unlikely to have played a significant role in this study, while confounding was well addressed by selecting a reference group comparable to exposed women with respect to main demographic and social characteristics. Reassuringly, the findings of Klebanoff et al were corroborated by the only prospective study that addressed long working hours (16).
Findings on the risk of miscarriage and occupational lifting, including patient transfer in healthcare, were divergent, with estimates of RR ranging between 0.4–3.6. However, the pooled estimate for the five studies of higher quality (9, 16–17, 18, 30) indicated no increase in RR, consistent with the three prospective cohort studies on occupational lifting (9, 17, 18). The overall estimate of RR for the latter three studies was 0.80 (95% CI 0.43–1.49). However, heavy lifting was either not defined or defined as lifting objects of 5–20 kg more than few times a day, amounting to a total lifted burden during a work day in the range of 100–200 kilos a day – a modest exposure, rather close to lifting activities encountered in daily life. For this reason, the studies are not informative regarding risks from heavy lifting.
Considering prolonged standing at work, earlier studies reported a moderately increased risk (16, 25, 30) while more recent studies reported a risk below unity (17, 24, 28, 33). This discrepancy is not explained by differences in extent of exposure. In contrast to heavy lifting, exposure levels were close to the highest possible in all studies (6–8 hours standing at work per day). However, the reliability of self-reported standing at work is unknown, possibly inaccurate, and may not encompass breaks taken during the workday. The slightly increased RR in earlier studies may have resulted from recall bias, and the only study with prospective exposure data did not indicate an increased risk (17).
In reviewing the relation of pre-term delivery, low-birth weight, and small-for-gestational-age to shift work, working hours, and occupational lifting, standing, and physical workload, we previously concluded that no compelling case exists for mandatory restrictions (4, 5).
These additional findings on miscarriage support such a view, although the evidence base on miscarriage is substantially more limited, both in terms of amount (especially for extremes of exposure) and methodological quality.
European Union Council Directive 92/85/EEC on the safety and health of pregnant women (50) requires that pregnant women be informed about potential occupational hazards to pregnancy and the fetus and that necessary preventive actions are taken, potentially including their exemption from night working subject to medical certification (Article 7). Advice on such exemptions for women with a healthy uncomplicated pregnancy should recognize the limitations in depth and quality of the existing risk information on miscarriage. Women with at-risk pregnancies should receive tailored individual counseling.
On the research front, there is a pressing need to conduct more and better prospective investigations, with enrolment of women before or during the very early stages of pregnancy. In the meantime, notwithstanding the generally reassuring nature of this review, it may be prudent to advise women against work entailing high levels of such exposures during the first trimester of pregnancy.