There is growing evidence of the negative effects of work stress on sleep (1). Problems with restorative sleep are common: chronic insomnia has a 10% prevalence rate in Western industrialized countries (2–4). Impaired sleep is associated with personal distress, diminished general functioning, increased absenteeism and presenteeism and, in turn, high personal and societal costs (5–7). To effectively target sleep problems in a population of stressed employees, it is important to consider recovery research findings. Recovery from work is regarded as an explanatory mechanism in the relation between acute stress reactions and adverse health. It can be defined as the restoration of depleted resources by psychophysiological unwinding after work (8). Recovery from work is well recognized as an essential daily process to balance the strains of work and prevent general ill health (9–10).
There is evidence that successful recovery from work implies three core components which are closely interrelated: (i) restorative sleep which can be perceived as a particularly important process in recovery from work stress because basic resources are restored during sleep, and fatigue subsequently decreases (11–12); (ii) Cognitive detachment from work is positively associated with general well-being, increased job performance and decreased psychological strain (13) and especially important for restorative sleep (8, 14–15). In fact, a deficient mental detachment has been found to mediate the negative relation between work stress and insomnia complaints (16–17); and (iii) Recreational activities are one way of fostering psychological detachment and restorative sleep by abstracting the mind from work-related thoughts (9, 11). In addition, engaging in leisure activities rebuilds regulatory and affective resources (18).
Evidence-based interventions are available that foster each of these three core components separately. For example cognitive behavioral therapy for insomnia (CBT-I) effectively improves sleep (19–20) and behavior activation interventions increase recreational activities (21). Third, as Querstret and Cropley (22) showed in a meta-analytic review, effective interventions exist for reducing rumination and worrying. An attempt was made to tailor such interventions to employees, and a training mainly focusing on psychological detachment from work was successfully investigated in a controlled but not randomized trial showing moderate effect sizes (23).
To the best of our knowledge, occupational health interventions that aim to promote all three core elements of recovery in an integrated manner have not yet been developed and evaluated. Integrating methods that foster all three components in one intervention and focusing it on the specific target group of stressed employees may increase the potential of inducing effective behavioral change (24–25).
Internet-based interventions for common mental and substance-use disorders as well as insomnia are well-studied in community and clinical samples (eg, 26–27). But less is known regarding their effectiveness in occupational settings among stressed employees (28). Few studies have been effective in reducing stress and depression in workplace settings (eg, 29). Although research on internet-based interventions for workplace settings remains in its infancy, these interventions may offer some advantages to employees such as anonymity and an easy access independent of time and place. Web-based interventions may attract people who do not utilize traditional mental health services (30).
We therefore developed an internet intervention specifically targeted at employees with the aim of overcoming their deficient recovery from work and decreasing their sleep problems. The intervention (GET.ON Recovery) is based on methods to foster the aforementioned three components of successful recovery from work. We hypothesize that GET.ON Recovery will lead to a greater reduction in insomnia complaints at post-test and 6-month follow up compared to a-wait-list control (WLC) condition.
Methods
Design and timeframe
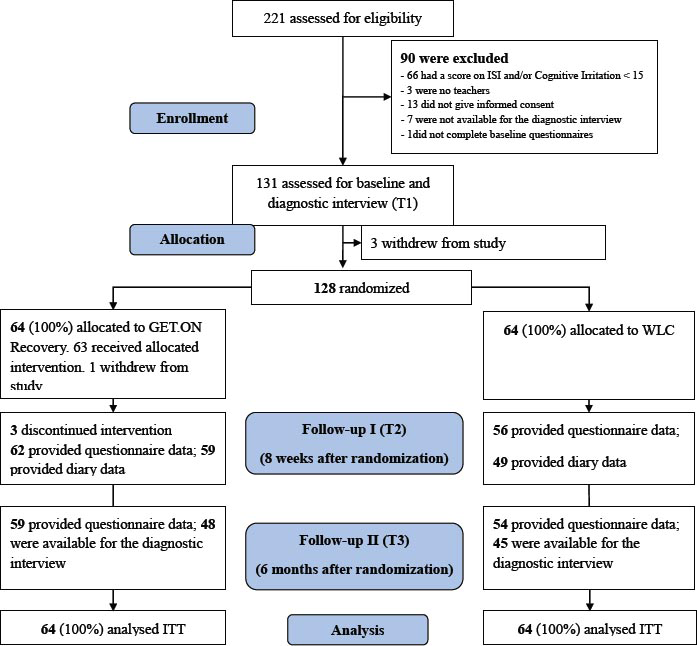
This study was a randomized controlled trial (RCT) comparing an internet-based, guided intervention group (IG) with a WLC group. Outcomes were measured pre-treatment, post-treatment (eight weeks) and at a six-month follow-up (figure 1). The study followed the CONSORT guidelines (31).
Based on the heterogeneous effects observed in the meta-analysis of Cheng (26), and taking into account that the intervention was newly developed, we expected an effect of medium size (Cohen’s d=0.50). Accordingly, a sample size of N=128 was required to detect a difference between the IG and WLC groups at post-test on the primary outcome measure (insomnia severity). This estimate was based on intention-to-treat analyses with α=0.05 and 1-β=0.80 in a two-tailed test.
Interested subjects were included and randomized from March–September 2013. Randomization was performed by an independent researcher using a computer program (randlist) that automatically assigned a 0 or 1 to each ID number, indicating allocation to either IG or WLC group. This random assignment was made at a 1:1 ratio. Randomization was not blinded.
The Psychological Ethics Committee of the Philipps University of Marburg approved the study (Nr. 2013-01K), which was registered as DRKS00004700 in the German Clinical Trial Register. Design and procedure of this study have been described in detail in the study protocol (32).
Procedure
Participants were recruited using email distribution lists to primary, secondary, and vocational schools, provided by the Ministry of Education in the German state of Nordrhein-Westfalen. Interested teachers applied to participate by an email to the primary study investigator (first author). The primary study investigator provided interested teachers with detailed information and a request to complete an online screening questionnaire. Teachers obtained access to the homepage using their email addresses and a self-chosen password. Participants who scored positive on the screening test were provided with an ID number and asked to (i) provide informed consent, (ii) complete baseline questionnaires (including a 7-day sleep diary) and (iii) participate in a diagnostic interview over the telephone. After the diagnostic interview, participants were randomized.
Inclusion and exclusion criteria
Inclusion criteria included (i) currently holding a position as a primary, secondary or vocational school teacher and working; (ii) being over the age of 18; (iii) experiencing significant clinical insomnia symptoms as measured by a score of ≥15 (33) on the Insomnia Severity Index (ISI) (34); (iv) experiencing work-related rumination as measured by a score of ≥15 on the cognitive irritation subscale of the Irritation Scale (IS) (35); and (v) having access to the Internet, an email address and a telephone number.
Exclusion criteria were: (i) receiving psychological help for insomnia and (ii) showing suicidal ideation based on item 9 of the Beck Depression Inventory II (BDI II) (36). Participants with scores of 2 (“I feel I would be better off dead”) and 3 (“I would kill myself if I could”) were excluded and received information via email regarding appropriate help. People taking sleep medication were not excluded from the study but were requested to keep their medication constant during the study period.
Intervention
GET.ON Recovery (32) uses already available and well-established therapeutic techniques combined in order to foster recovery from work. We used CBT-I methods, such as sleep restriction, stimulus control, sleep hygiene and cognitive interventions (37), supplemented by techniques from behavioral activation, metacognitive therapy (MCT) (38), gratitude research (39) and research on boundary management (40).
The intervention comprises six 1-week modules. In the first session, participants learn how sleep, psychological detachment and recreational activities are interconnected, and they make a plan on what sleep hygiene rules and recreational activities they plan to perform in the following week. Also, they are introduced to the 10-item online recovery diary, which is not a standard sleep diary, as recommended by Carney et al (41). The diary is tailored to the intervention and target group while covering important sleep items like time in bed or total sleep time, in order to be able to calculate and monitor sleep efficiency. In session two, participants are introduced to stimulus control and sleep restriction and plan the first steps by rescheduling their sleep for the following week. In session three, participants reflect on their progress and then continue with their sleep restriction plan. Also, they learn about behaviors which help to initiate closing time (‘boundary tactics’) (40) and foster detachment and sleep (gratitude journal) (38). In session four, participants learn how attention works and why worrying and rumination can be so persistent. The fifth session is based on MCT (38), teaching participants how continuous attention on ruminating thoughts can further increase their frequency and intensity.
In every session, homework includes planning of recreational activities into daily life, monitoring sleep efficiency and continuing with sleep hygiene and restriction. Additionally, participants will be asked to choose one exercise from the current session to apply throughout the forthcoming week. The intervention will conclude with a summary session (session six), which aims at preparing for difficult times when sleep gets significantly worse.
Support
The IG participants were supported by trained coaches according to a manual written by the first author to ensure a standardized procedure of coaching. The manual is available upon request. All communication between the coach and study participants occurred via an email messaging system on the secure training homepage. The support comprised brief, motivational, weekly feedback on exercises in completed modules. Additionally, coaches were available for questions that occurred. Coaches also provided reminders if participants did not complete a module within one week. To maximize the comparability of the participants and maintain the guidance at a minimal level, coaches were advised that the total amount of time spent on each participant should not exceed three hours for the duration of the intervention. A clinical psychologist supervised the coaches.
Primary outcome measure
Insomnia severity
Insomnia severity was measured with the German version (Pillmann, F, unpublished) of the ISI (33, 34, 42). This 7-item instrument is answered on a 5-point Likert scale. The total score ranges from 0–28. It has been validated as a web-based measure as well (43) and is frequently used in iCBT-I research [for example (44)]. At screening, we used the cut-off score of ≥15 indicating clinical insomnia (33). Internal consistency was previously reported to be α=0.90 (45). In our sample, internal consistency was α=0.91.
Secondary outcome measures
Recuperation in sleep
We used the recuperation in Sleep subscale, which is part of a well-validated (α=0.90) questionnaire (46) recommended as an outcome measure by the German Society of Sleep Medicine. Seven items (eg, “How relaxed did you feel upon waking up?”) were answered on a 5-point Likert scale. Internal consistency in the present sample was α=0.91
Sleep efficiency
For seven days, at T1 (after the baseline questionnaires and before the telephone interview) and T2, participants completed an online diary. In this diary, participants recorded the time at which they left their beds each morning, their previous evening’s bedtime and their total hours of sleep (41). Sleep efficiency was computed using these data using the formula: (total hours of sleep/time spent in bed).
Diagnoses of primary insomnia, major depression and generalized anxiety disorder
At baseline and 6-month follow up, trained clinical psychologists conducted diagnostic interviews over the telephone. Interviews provided diagnostic data on episodes of primary insomnia according to the Structured Interview for Sleep Disorders (SIS-D) (47). Diagnostic criteria used were: (i) having problems initiating, maintaining or finding restful sleep for ≥1 month and ≥3 nights per week, (ii) which cause clinically significant distress or impaired functioning, (iii) which do not exclusively appear in the context of hyper-, parasomnia or another mental disorder and (iv) cannot be explained by substance use. Because insomnia and depression often coexist and deficient psychological detachment is a core symptom of general anxiety disorder, these disorders were also assessed by employing the according sections of the Structured Clinical Interview for DSM-IV (SKID-I) (48).
Worrying
We measured worrying with a 3-item short version of the Penn State Worry Questionnaire (PSWQ) (49–50). For use as an outcome measure, we adapted a past-week version of the PSWQ according to the three respective German items of the PSWQ-past week (51). Internal consistency of the English ultra-brief version of the PSWQ was previously reported to be α=0.85. In our sample, the scale displayed similar good internal consistency of α=0.88.
Work-related rumination
We measured work-related rumination with the cognitive irritation subscale of the Irritation Scale (IS), a questionnaire which assesses occupational strain (35). We chose a score of >14 as a screening criterion because a score of ≥15 indicates an above-average level of rumination (Stanine ≥7) (35). Responses to the three items (eg, “even at home I have to think about problems at work”) are on a 7-point Likert. The scale has good internal consistency (α=0.86), which also holds for our sample (α=0.87).
Recovery experiences
The 16-item Recovery Experience Questionnaire (REQ) (52) has been validated and includes four factors that represent four different recovery experiences: (i) psychological detachment (eg, “During time after work, I don’t think of my work at all”) (α=0.85), (ii) relaxation (eg, During time after work, I kick back and relax”) (α=0.85), mastery (eg, “During time after work, I do things that are challenging”) (α=0.85), and control (eg, “During time after work, I decide myself what I do”) (α=0.85). The questionnaire is answered on a 5-point Likert scale (not true at all, a little bit true, moderately true, mostly true, true). For our sample, internal consistency ranged from α=0.90 (mastery) to α=0.93 (control).
Recovery activities
The Recreation Experience and Activity Questionnaire (ReaQ) (53) rates participants’ frequency of recreational activities during the past week (0, 1, 2, 3, or ≥4 times) for 21 items (eg, “Over the last week, I calmly enjoyed a coffee/tee”). The internal consistency of the questionnaire was α=0.88 for our sample.
Absenteeism
Absence from work due to sickness was measured at 6-months follow-up as the self-rated amount of total days on sick leave during the past three months.
Presenteeism
Presenteeism was measured at 6-months follow-up as the self-rated amount of total days with impaired productivity due to work-related sleep problems during the past three months.
User satisfaction
We assessed user satisfaction using a self-designed questionnaire with 8 items (eg, “I would recommend this training to a friend in need of similar help”) based on the German version of the Client Satisfaction Questionnaire (CSQ-8) (54–55), answered on a 4-point Likert scale (not true at all, rather untrue, somewhat true, completely true). Internal consistency was α=0.92.
Statistical analysis
We present the results from intention-to-treat (ITT) analyses performed with SPSS, version 21 (IBM Corp, Armonk. NY, USA). Reported P-values are two-sided with a significance level of 0.05.
Missing data
All of the participants completed the baseline assessment. A Markov Chain Monte Carlo multivariate imputation algorithm (SPSS 21) with ten estimations per missing value was used to replace any missing T2 and T3 data (56). In multiple imputation (MI), predictors are defined which lead to estimations for the missing values. We used all pre-, post-, and 6-month follow-up values of all outcome measures as well as age and gender as predictors. At post-treatment, 7.8% (N=8 in the IG and N=2 in the WLC) of the data had to be replaced. At 6-month follow-up, it was 7.2% (N=5 IG and N=10 WLC) for the questionnaires. For the diary data (sleep efficiency), 15% had to be replaced (N=5 and N=15 in the IG and WLC, respectively). Compared to other imputation techniques, MI minimally changes variance of data, thus providing the best estimates of missing data, at least until 50% of missing data (56).
Treatment efficacy
To assess treatment efficacy, the GET.ON Recovery and WLC groups were compared on all self-report outcome measures at T2 using univariate analyses of covariance (ANCOVA) with T1 scores as covariates to prevent bias and increase statistical power (57–59). To assess the stability of treatment efficacy, we also conducted ANCOVA with outcome scores at T3 and baseline scores (T1) as covariates. We report P-values and Cohen’s d for the between-group effect size (60) and corresponding 95% confidence intervals (95% CI).
Reliable change
To enable an interpretation of clinical significance, Jacobson and Truax’s (61) widely used method was employed to detect reliable changes in the primary outcome (insomnia severity) at post-treatment. A reliable change for one participant was defined if the ISI score declined from baseline to post-assessment with a reliable change index >1.96 (5.01 points in the ISI).
Symptom-free status
The number of participants who were free of insomnia symptoms was counted in both conditions. A score <8 on the ISI indicates a symptom-free status as defined by Morin (45).
Reduction of diagnosis of primary insomnia
Participants who fulfilled the diagnostic criteria of primary insomnia according to the SIS-D at baseline were of interest. The numbers of participants were calculated that maintained their diagnostic status or did not meet the criteria of primary insomnia any longer at the 6-month follow-up. We conducted Pearson’s chi² test to compare the WLC and GET.ON Recovery groups with regard to the maintenance or change to diagnose-free status of primary insomnia during the preceding 6 months. The frequency of episodes was omitted; analyses were only processed in terms of whether (=1) or not (=0) an episode occurred during the preceding 6 months.
Additionally, number needed to treat (MI) and corresponding 95% CI were calculated. NNT is an effect size that reflects clinical significance by comparing control and intervention groups on the frequency of a positive outcome (62). We calculated NNT by comparing the intervention and WLC groups with regard to the number of participants with or without (i) reliable change, (ii) symptom-free status and (iii) change from diagnosis of primary insomnia to diagnosis-free status.
Results
Participants
Figure 1 shows the flow of participants including those who were excluded. After screening, 90 participants were excluded: most (N=66) because of a score of <15 on the ISI and/or the cognitive irritation subscale. A total of 128 participants were randomized to either the IG (N=64) or the WLC group (N=64).
Missing data
Baseline data were available for all participants. The study attrition rate was low: 7.8% at post-treatment (N=8 in the IG and N=2 in the WLC) and 7.2% at the 6-month follow-up (N=5 IG and N=10 WLC), for the questionnaires.
Baseline characteristics
The baseline characteristics of the study participants are presented in table 1. The sample comprised 128 teachers, most of whom were female (74.2%), with an average age of 48 (SD=9.9) years. Of these, 59 participants (46.1%) had previous experience with a health training and/or psychotherapy, 100 (78.1%) were diagnosed with primary insomnia, 18 (17.2%) fulfilled the criteria of major depressive disorder, and 12 (9.4%) of generalized anxiety disorder (table 1). Overall, this indicated that participants were highly affected by various mental health symptoms.
Intervention usage and user satisfaction
All of the participants (N=64) in the IG completed the first three modules of GET.ON Recovery. Two subjects dropped out after the third module, and one dropped out after the fourth. Reasons reported were “lack of motivation” and “lack of time”. Overall, 61 (95.3%) participants completed all six sessions. User satisfaction was high: 91% would recommend the training to a friend in need (item 4, answers of “rather yes” or “yes, completely”).
Primary outcome analysis – insomnia severity
Treatment efficacy
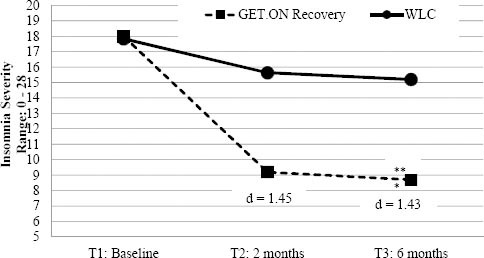
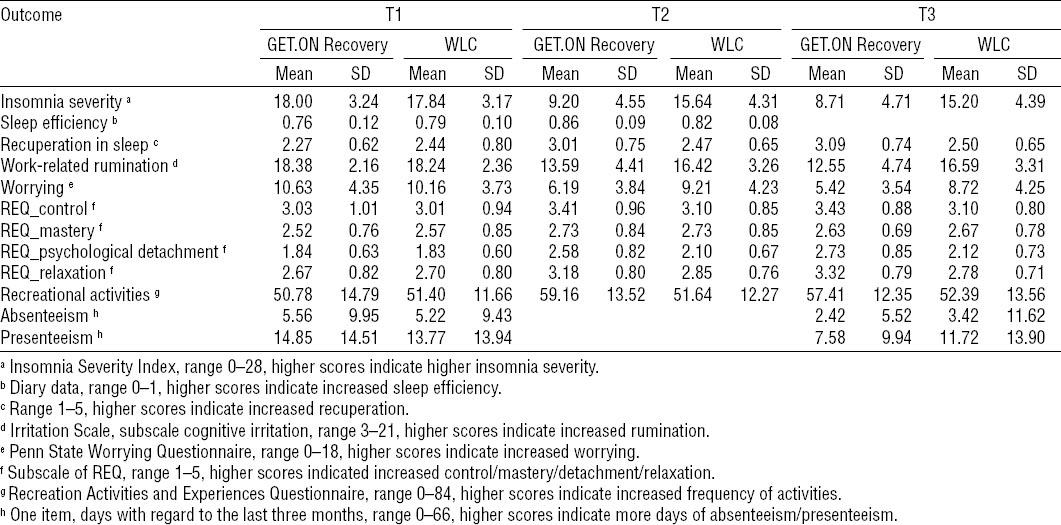
The GET.ON Recovery group reported significantly lower insomnia severity at post-treatment than the WLC group [F=74.11, P<0.001, d=1.45 (95% CI 1.06–1.84)]. Sensitivity analysis (two-way ANOVA, group × time interaction) led to similar results as the ANCOVA (F=63.59, P<0.001). Table 2 shows the means and SD for all outcome measures separately for baseline (T1), post-treatment (T2) and 6-months follow-up (T3). Figure 2 displays the comparison of both groups on the primary outcome. Table 3 displays the results of the ANCOVA for all outcome measures separately for T2 and T3.
Table 2
Means and standard deviations of all outcome variables at baseline, post-treatment and six-month follow-up (intention-to-treat sample, N=128). [WLC=waitlist control; SD=standard deviation; REQ=Recovery Experience Questionnaire]
Reliable change and symptom-free status
There were more participants in the IG [51 (79.7%)] with reliable improvement at post-treatment in insomnia severity than in the WLC group [18 (28.1%)]. This finding corresponds to a NNT to achieve reliable improvement from baseline to post-treatment of 1.73 (95% CI 1.39–2.29). Unlike four participants in the WLC, no IG participant experienced reliable deterioration (T2 score of >5.01 above the T1 score).
In the GET.ON Recovery group, 23 participants (35.9%) were symptom-free at post-treatment as indicated by a score <8 in the ISI. In the WLC group, 4 participants (6.3%) were symptom free. This finding corresponds to a NNT of 3.37 (95% CI 2.33–6.05).
Secondary outcome analysis
As shown in table 3, the ANCOVA of nearly all outcome measures showed significant differences between the two groups. Participants in the IG reported significantly less insomnia severity, rumination, and worrying at post-treatment than WLC participants. In addition, the GET.ON Recovery group showed significantly higher scores with regard to sleep efficiency, restorative sleep, recreational activities, and recovery experiences. The mastery subscale of the REQ was the only measure on which the IG and the WLC group not differ. Effect sizes ranged from d = -0.34 (95% CI -0.69–0.01) (REQ control subscale) to d= -0.77 (95% CI -1.13– -0.41) (recuperation in sleep).
Long-term efficacy
The results at T3 were similar to those at T2. ANCOVA comparing WLC and IG at T3 also showed a large effect size with regard to the primary outcome [d=1.43 (95% CI 1.04–1.82)]. Similarly, for the IG, 27 participants (42.2%) were symptom-free at 6-months follow-up as indicated by a score <8 in the ISI. In the WLC group, 4 participants (6.3%) were symptom free. This finding corresponds to a NNT of 2.78 (95% CI 2.02–4.45).
The effect sizes of the analyses of the secondary outcomes ranged from d= -0.34 (95% CI -0.69–0.01) for recovery activities to d=0.99 (95% CI 0.62–1.36) for work-related rumination (table 3). IG and WLC did not differ in days of absenteeism.
Change to insomnia diagnosis-free status
Of the 128 participants, 93 (72.6%) agreed to a diagnostic telephone interview at 6-months follow-up (figure 1). Missing values were imputed using MI. Divided almost equally between the WLC group and IG, 100 participants fulfilled the diagnostic criteria of primary insomnia at baseline 52 (81.3%) and 48 (75.0%), respectively). At 6-months follow-up, 31 (64,6%) participants in IG and 17 (32,7%) the WLC group were free of primary insomnia. There was a significant greater reduction in the intervention group [χ2 (1, N=100)=10.17, P<0.05] corresponding to a NNT of 3.14 (95% CI 1.98–7.52). Sensitivity analyses led to similar results: When missing T3 diagnoses were imputed using the conservative first observation carried forward (FOCF) approach, the IG also had a significantly greater reduction of primary insomnia [χ2 1, N=100)=5.69, P<0.05; NNT=4.64 (95% CI 2.42–22.10)].
Discussion
The present study evaluated the efficacy of an internet-based guided recovery training for employees with work stress and sleep problems. Results showed that the intervention was more effective in reducing insomnia severity than the WLC condition with a large effect size (d=1.45). The IG also improved significantly more in expert-rated reduction of primary insomnia and self-rated secondary outcomes than the WLC group. In general, we observed small (presenteeism), medium (eg, sleep efficiency) and large (eg, recuperation in sleep) effect sizes for the secondary outcomes. The effects of the intervention on both primary and secondary outcomes were similar at the 6-month follow up. One possible reason for the lack of improvement for absenteeism may be that the reported number of sick days were already small at baseline not leaving much room for improvement.
Notably in this study, nearly 90% of the participants participated in an occupational health training for the first time. This result is consistent with other studies (63) showing that internet-based interventions can reach people not previously reached by traditional training formats. Acceptance can be thus regarded as high. This is additionally supported by the low intervention-dropout rate (5%) and low study attrition. Intervention and study adherence was generally higher than with a traditional group face-to-face training (ie, 23) or guided and un-guided internet-based interventions targeting stress or insomnia (29, 64–65). Our high adherence rates may be due to the guidance in the training in combination with the personal contact in the diagnostic interviews. Both factors are supposed to foster accountability and trust and by that, adherence, (66) and both we share with the studies of Ritterband on iCBT-I (44, 67), which also reported high adherence rates. Another reason could be the high user satisfaction: 90% would recommend the training to a friend. This in turn could be explained by the interactivity of our training and our targeting approach, which might have fostered personal relevance and identification with our program. This is thought to enhance effectiveness as well as adherence to an intervention (24, 68).
Overall, the effects regarding insomnia severity and sleep efficiency are higher than those assessed in Cheng’s meta-analysis (26) on the efficacy on internet-based CBT-I (d=0.86). One reason could be that our intervention included professional guidance while the studies included in Cheng’s meta-analysis did not. It is well established that guidance increases clinical effectiveness (69).
In addition to sleep, a second core process of recovery is psychological detachment from work. Despite the large number of studies on this topic, to our knowledge, there is only one intervention study to date (23). This study showed that psychological detachment from work can be fostered by a face-to-face group training, at least in the short term. Our results add to these findings by showing the effects of an internet-based training in a RCT on recovery experiences like detachment, but also for corresponding recovery activities, for up to 6 months.
The present study has several strengths and limitations. A particular strength is the use of self- and expert-rated health status. Given that studies demonstrating the effects of internet-based CBT-I (26) or interventions for improving detachment have exclusively relied on self-ratings, the use of both self- and expert-ratings in the present study significantly contributes to the present literature by enhancing the validity of the outcome assessment. In addition, this study’s internal validity can be regarded as high since the study sample comprised only schoolteachers.
The strength of high internal validity is simultaneously a limitation with regard to external validity as generalizability is constrained to schoolteachers. Also, women were over-represented in our study, which restricts the validity of the study for male teachers. Plus, objective measures like actigraphy or polysomnography would have made the results stronger. In addition, we cannot draw conclusions regarding the superiority of this intervention over classic CBT-I, which was also found to be effective for a subgroup of stressed individuals (70). In addition, due to our WLC design, blinding was not possible. This and having a more active control group (eg, receiving simple sleep hygiene advice via the internet) in order to investigate if reported improvements are not solely the result of a new delivery mode or attention, would be important perspectives for further research.
In conclusion, the study shows that an internet-based recovery training may help teachers reduce their insomnia symptoms as well as a broad range of related health-outcomes such as rumination and worrying. The results may also be valid for employees with similar working conditions as teachers. Of special interest are those groups of employees who, like teachers, are more likely to face work–home interference (71), which is closely linked to a deficient recovery from work (72). Future research should replicate our findings with teachers, different groups of employees and different control group designs to strengthen the generalizability and robustness of our results.