The menstrual cycle, defined by cyclical patterns of circulating reproductive hormones [luteinizing hormone (LH), follicle-stimulating hormone (FSH), estrogen, and progesterone], is regulated by the hypothalamo – pituitary – ovarian axis (1). Measured by its length and regularity, the menstrual cycle is considered a marker of general reproductive health (2) and has previously been associated with subfertility (3–7). We hypothesize that shifts in the circadian rhythms, either through sleep disturbances or altered melatonin production, may play a role in regulating the reproductive hormones that control the menstrual cycle. Produced in the pineal gland during dark hours, melatonin is thought to regulate several physiologic mechanisms (8, 9).
Shift work is prevalent in the United States; according to the Bureau of Labor Statistics (10), nearly 15 million workers (comprising approximately 15% of full-time US workers) work evenings, nights, or rotating shifts. Shift work is even more prevalent among healthcare workers, 24–28% of whom work evenings, nights, or rotating shifts (11). Long working hours are also commonly reported in the US; approximately 25% of those who are currently employed work >40 hours per week [www.bls.gov/cps/cpsaat19.htm].
Most previous studies examining the relationship between shift work and menstrual cycle characteristics support an association between working at night and menstrual function, though many of these studies were limited by their small sample sizes or small proportion of women exposed to shift work (12–21). The largest of these studies included 71 077 women from the Nurses’ Health Study II (NHS II) and showed dose-dependent associations between the number of months performing rotating shift work in the prior 24-month period and higher risk of irregular cycles, and cycles that were short (<21 days) or long (≥40 days) (18). No previous studies have evaluated whether permanent night work is as disruptive to menstrual function as rotating night shift work.
Nursing can involve physically and emotionally demanding work, yet there are few previous studies of physically demanding work and menstrual function (15, 16, 22–24). In these studies, the study populations, statistical modeling, and results vary to the extent that no clear conclusions can be drawn about what effect, if any, the physically demanding work might have on menstrual function.
We examined the associations between work schedule characteristics and physically demanding work and menstrual cycle length and regularity in the Nurses’ Health Study 3 (NHS3).
Methods
Study population
The NHS3 is a cohort study of US and Canadian female nurses and nursing students born on or after 1 January 1965. Open recruitment started in 2010 and is ongoing. Female registered nurses (RN), licensed practical/vocational nurses (LPN/LVN) and nursing students, ages 18–46 years, are eligible to participate. The NHS3 is an open cohort, and questionnaires are exclusively web-based; participants are asked to complete questionnaires on a regular schedule dating from their study enrollment. The baseline questionnaire includes an assessment of occupational exposures relevant to nurses, including characteristics of current and prior work schedule and physically demanding work. The first follow-up questionnaire (conducted approximately six months after the baseline questionnaire is completed) includes questions on menstrual cycle characteristics.
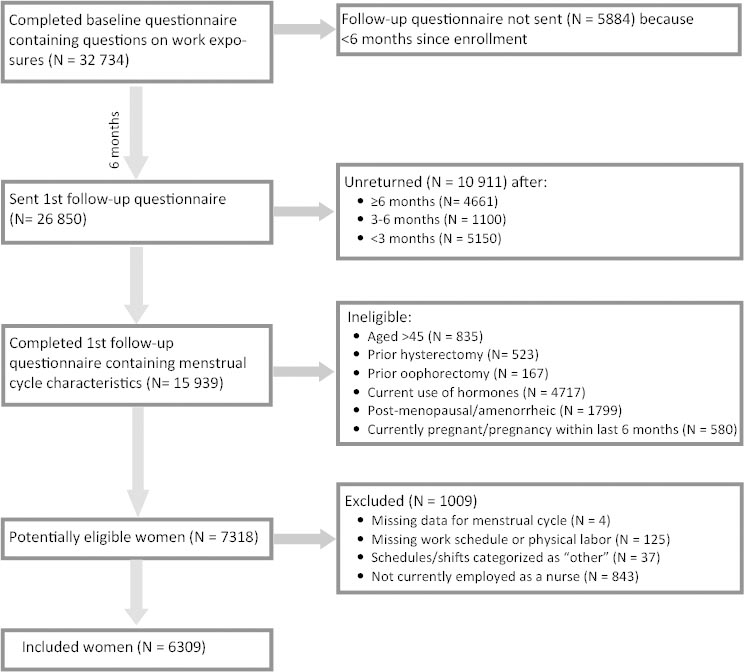
To be eligible for this analysis, participants had to have completed the baseline and first follow-up questionnaires, which, at the time of analysis, included 15 939 participants. Figure 1 describes eligibility and exclusion criteria. After exclusions, 6309 participants were available for analysis.
Data collection
The baseline questionnaire collected information about current and prior work schedules. Average hours worked per week in the past year were collected in the following categories: 0, 1–20, 21–40, 41–60, and >60 hours/week. For analysis, we considered >40 hours/week to be long work hours. Information on current usual work schedule (over the past year) was collected and included days only, evenings only, nights only, rotating with nights, and rotating without nights (ie, rotating between day and evening shifts). For the survey, “night” was defined as most hours worked falling between 24:00–08:00 hours. We also collected data on how many night shifts were worked per month over the past year: 0, 1–2 nights per month, 3–4 nights per month, 2–3 nights per week, and ≥4 nights per week. Women who worked 5–7 nights per month had to choose the closest category (3 –4 nights per month or 2–3 nights per week). To assess the history of night shift work, participants reported the number of years they had worked rotating night shifts (defined as at least three nights per month in addition to days or evenings in the same month) and total number of years they worked non-rotating night shifts.
To collect information on physical demands, we asked how many hours per day, on average over the past month, each participant was on her feet at work (standing or walking): <1, 1–4, 5–8, or ≥9 hours/day. We also asked how many times per day, on average over the past month, she lifted or moved a physical load of ≥25 pounds at work (including repositioning or transferring patients): 0, 1–5, 6–15, or ≥16 times/day.
The data on work schedules and hours were collected at baseline regarding the prior year, and physical demands data (also collected at baseline) concerned the prior month. Approximately six months to a year after baseline, data on menstrual cycle characteristics were collected in the follow-up questionnaire. Participants provided the current regularity of their menstrual cycles in the following categories: “very regular (+/- 3 days), regular, usually irregular, or always irregular”. For analysis, we compared “regular” (very regular or regular) to “irregular” (usually or always irregular).
Participants also reported their current usual menstrual cycle length, defined as the interval from the first day of the period to the first day of the next period. Questionnaire choices included <21, 21–25, 26–31, 32–39, and 40–50 days, and “>50 days or too irregular to estimate.” For analysis, we defined our reference group as 26–31 days, very short cycles as <21 days, moderately short cycles as 21–25 days, and long cycles as 32–50 days. Because 96% of the 316 women who reported that their cycles were “>50 days or too irregular to estimate” also reported “usually or always” having irregular cycles, we excluded these 316 women from the analysis of long cycles.
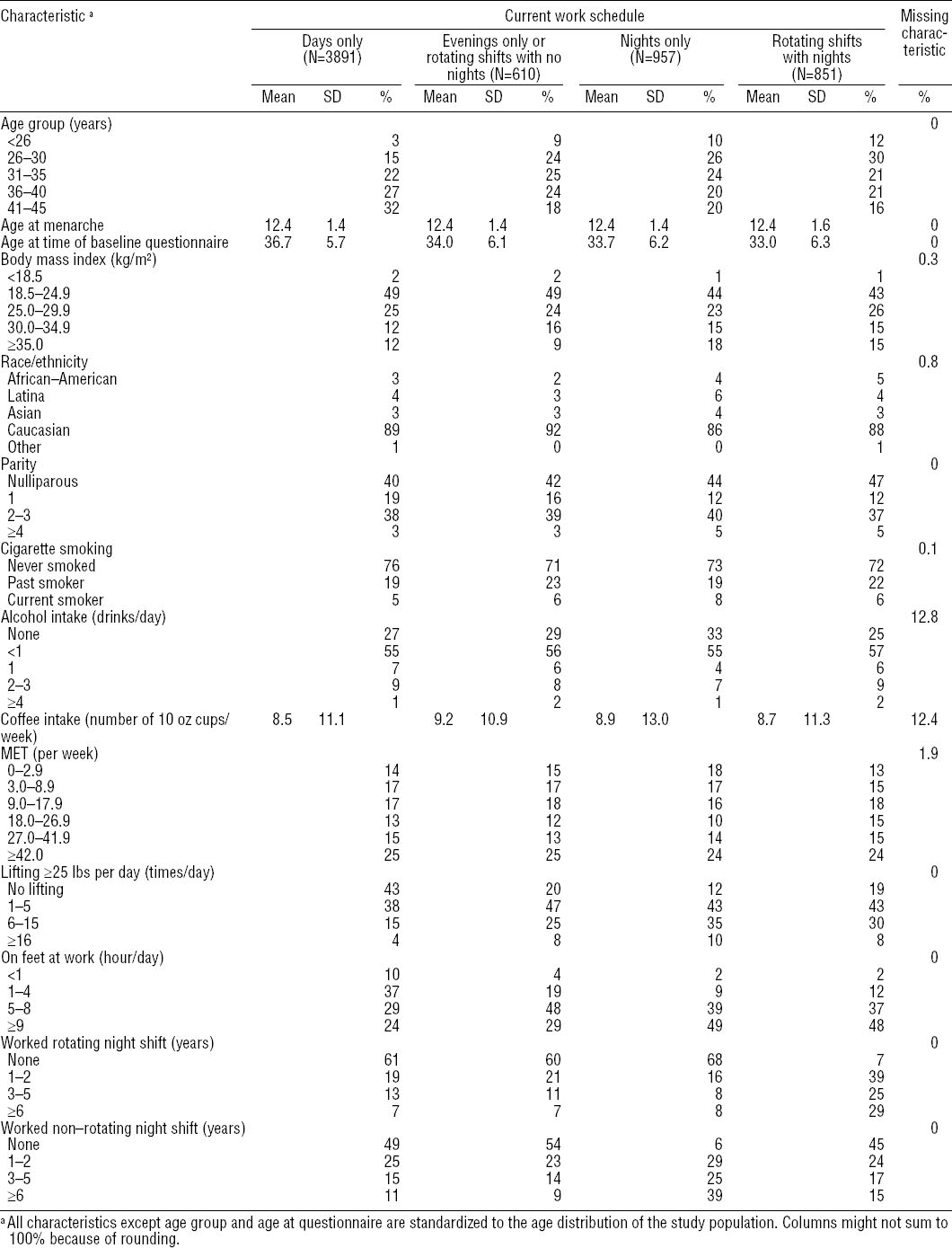
Covariates collected on the questionnaires included age, race/ethnicity, body mass index (BMI), parity, age at menarche, recreational physical activity, smoking status, and caffeine and alcohol consumption (see Table 1 for category definitions).
Statistical analysis
We used SAS statistical software version 9 (SAS Institute, Cary NC, USA) to conduct all analyses. We calculated age-adjusted means and prevalence of selected characteristics. We used log binomial regression analysis to estimate prevalence ratios (PR) of menstrual cycle characteristics in relation to occupational factors. We created separate models for very short (<21 days), moderately short (21–<25 days), or long (32–50 days) cycle length and cycle irregularity. Because the log binomial models did not converge for some of the analyses of very short cycles (due to a small number of cases in some exposure categories), we used logistic regression to estimate prevalence odds ratios (OR) for all analyses of menstrual cycle length. The potential covariates were chosen a priori, based on factors related to menstrual function in previous studies (5, 18, 26). Covariates that changed the estimate by ≥10% for the occupational variables were retained in the final multivariable model; to maintain consistency across models for the same outcome, if a covariate changed an exposure estimate for one exposure (such as, heavy lifting), we retained it in models for all other work exposures (such as, hours worked) for that menstrual outcome. In practice, the additional covariates had minimal if any difference in the other models. Age, smoking, body mass index (BMI), physical activity, parity, age at menarche, and race/ethnicity were retained as covariates. Of the participants, <1% were missing BMI, race/ethnicity, and smoking, and 1.9% were missing physical activity data (table 1). For covariates with missing data, a missing indicator was created. To calculate a dose-response trend for occupational variables, the midpoint of each reporting category was used to create a continuous variable. To separate the effects of current work schedule and number of years of previous shiftwork, we adjusted the analyses of years of shift work for current schedule.
The Institutional Review Boards of the Brigham and Women’s Hospital and the National Institute for Occupational Safety and Health approved the study. Completion of the web-based questionnaires implied informed consent.
Results
The 6309 nurses in our study ranged in age from 21–45 years at the time of the baseline questionnaire [mean 35.2, standard deviation (SD) 6.1 years]. With regard to current work schedule, most participants worked the day shift (61.7%), with the rest working evenings or rotating shifts without nights (9.7%), nights only (15.2%), or rotating shifts with ≥3 nights per month (13.5%). Nurses who worked night shifts or rotating night shifts were – on average – younger, more likely to be overweight or obese, nulliparous, and current or former smokers than nurses working other schedules (table 1). Physically demanding work also varied by current work schedule; nurses working day shifts were half as likely to have heavy-lifting duties and were also less likely to engage in prolonged standing than nurses working other shifts.
Irregular cycles
Of 6309 participants, 1196 nurses reported having irregular menstrual cycles (19.0%). In adjusted models (table 2), working >40 hours per week in the past year was associated with a modestly higher prevalence of irregular cycles [PR 1.16, 95% confidence interval (95% CI) 1.04–1.29] compared to working 21–40 hours/week (P for trend = 0.01). Prevalence of irregular cycles was higher among nurses who worked nights only (PR 1.32, 95% CI 1.15–1.51) or rotating shifts with nights (PR 1.27, 95% CI 1.10–1.47) compared to nurses working days only, and the prevalence increased with the number of nights worked per month (P for trend <0.0001). Though the associations of years of rotating night shifts were attenuated after adjustment for covariates, including current shift schedule, there was still a suggestion of an association between irregular cycles and years of rotating night shift (P for trend = 0.06). An association with years of night shift not involving rotation was eliminated in adjusted models, however, primarily due to adjustments for BMI and current work shift schedule. We also analyzed years of rotating and non-rotating night shift in separate models stratified by whether the current work schedule was days or non-days, and we saw no difference (data not shown).
Table 2
Risk of irregular menstrual pattern with current work schedule, history of shift work, and physically demanding work among 6309 participants of the Nurses’ Health Study 3 (2010–2012). a [PR=prevalence ratio; 95% CI=95% confidence interval]
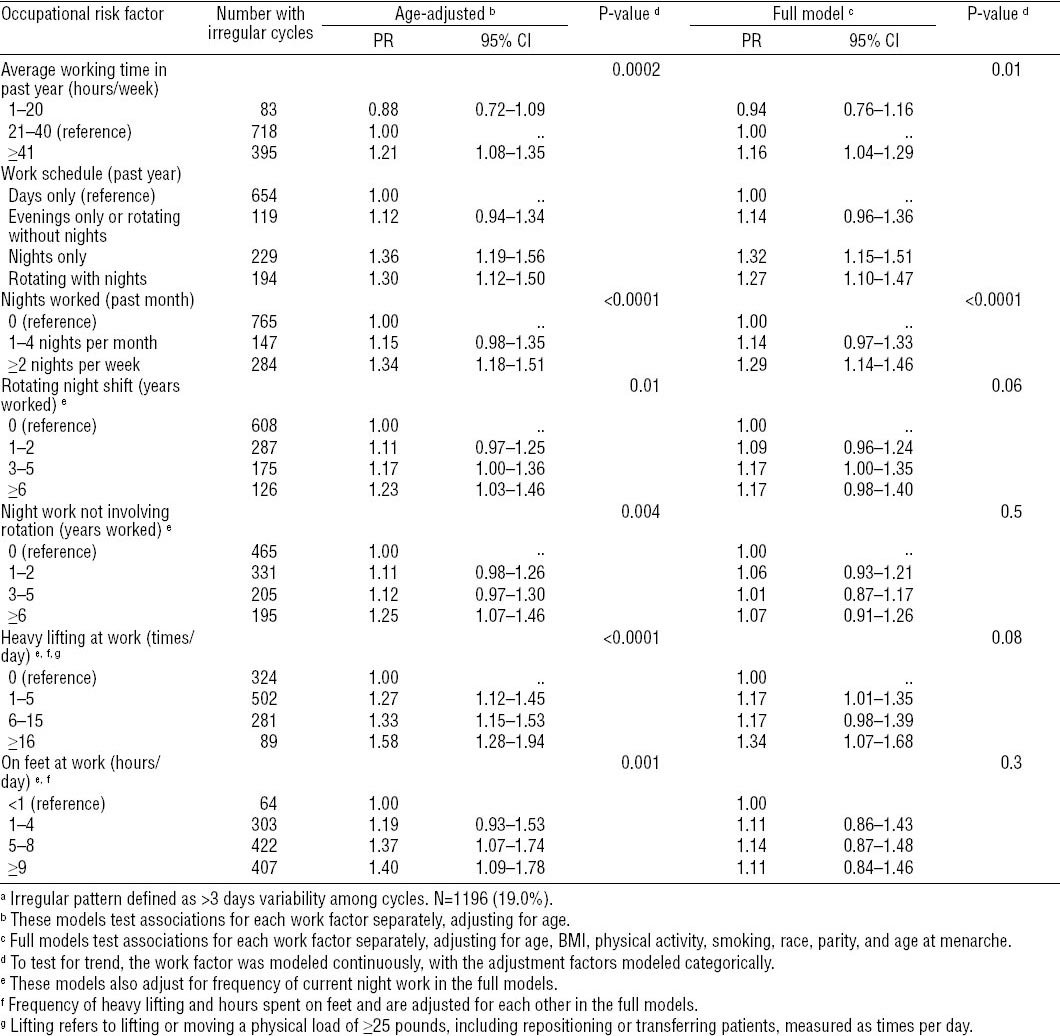
Physically demanding work was also associated with irregular cycles (table 2). A greater amount of heavy lifting was associated with higher prevalence of irregular cycles in the fully adjusted model (PR for lifting ≥16 times/day compared to no lifting: 1.34, 95% CI 1.07–1.68). Although prolonged standing was associated with higher prevalence of irregular cycles in the age-adjusted model, further adjustment — particularly for amount of heavy lifting — attenuated the association of prolonged standing with menstrual irregularity.
Cycle length
Respectively, 92 (1.5%), 935 (15.6%), and 789 (13.2%) participants reported menstrual cycle lengths of <21 (very short), 21–25 (moderately short), and 32–50 (long) days. A majority [4177 (69.7%)] reported cycles lasting 26–31 days (reference category). In age-adjusted models, long working hours were associated with very short cycles, rotating night work was associated with very short and long cycles, and prolonged standing and high amount of heavy lifting were associated with very short and moderately short cycles (table 3).
Table 3
Age-adjusted associations of current work schedule, history of shift work, and physically demanding work with short and long menstrual cycle length among 5 993 a participants of the Nurses’ Health Study 3 (2010–2012). b [OR=odds ratio; 95% CI=95% confidence interval]
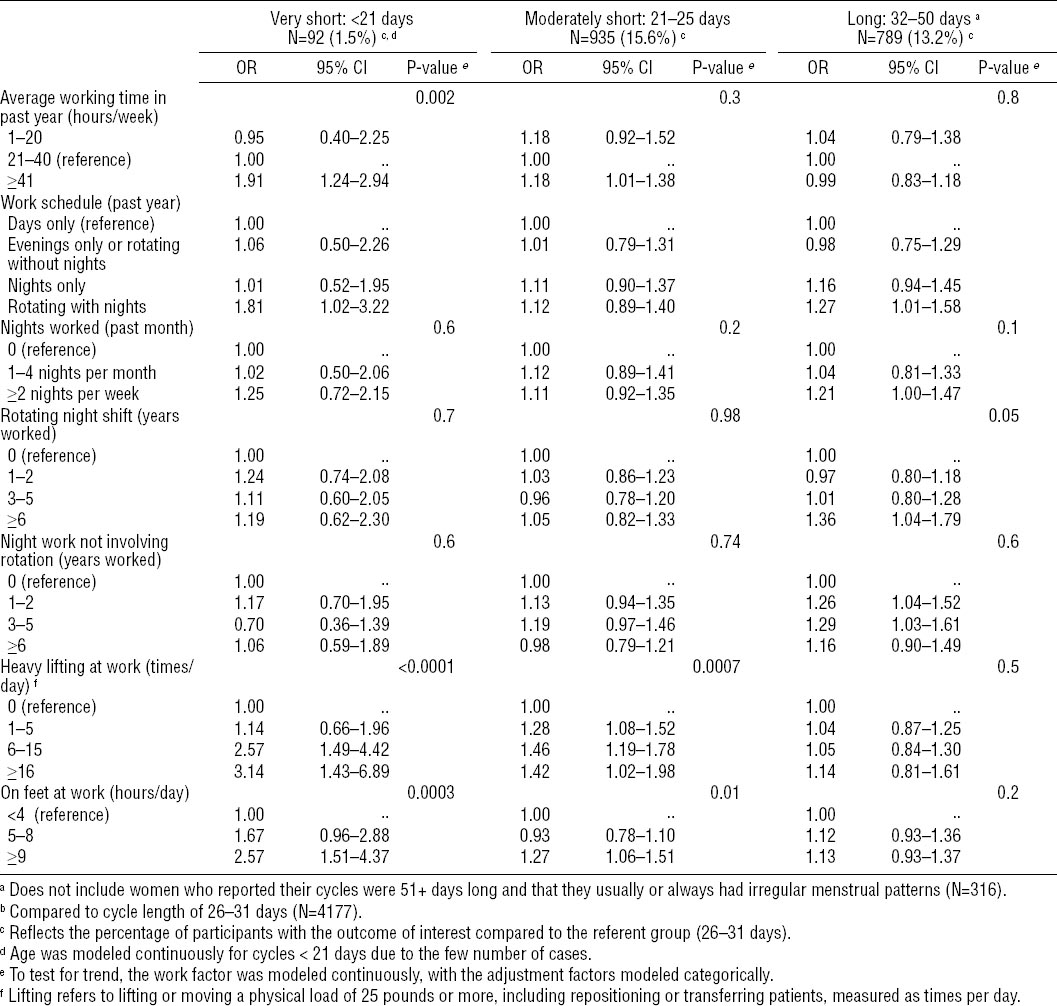
After further adjustment for potential confounders (table 4), long working hours were associated with very short cycles (OR 1.93, 95% CI 1.24–3.01 for ≥41 versus 21–40 hours/week; P for trend = 0.002). Rotating night shift work was associated with very short cycles (OR 1.75, 95% CI 0.98–3.12) and long cycles (OR 1.28, 95% CI 1.03–1.61); however, working nights without rotation was not associated with cycle length. Moreover, neither current amount of nor years of night work showed any clear trend with regard to extremes of cycle length, though confidence intervals were wide.
Table 4
Adjusted models a: Association between work schedule, history of shift work, and physically demanding work with short and long menstrual cycle length among 5993 b participants of the Nurses’ Health Study 3 (2010–2012). [OR=odds ratio; 95% CI=95% confidence interval]
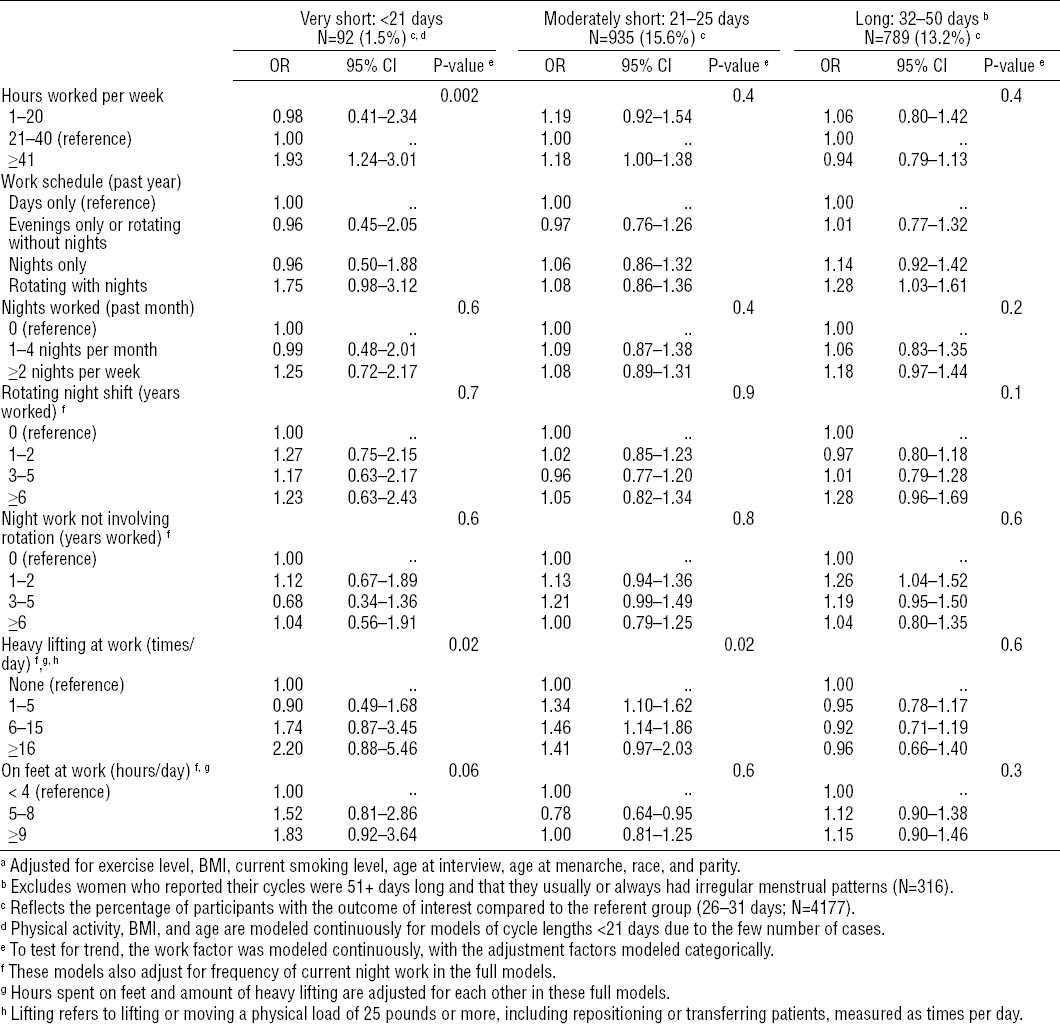
Nurses who reported frequent heavy lifting at work were more likely to experience very short or moderately short cycles (P for trend = 0.02 for each endpoint) (table 4). As was the case for cycle irregularity, the dose–response association of time spent standing with short-cycle length (table 3) was somewhat explained in fully adjusted models (table 4) by its correlation with heavy lifting (correlation coefficient=0.6).
Discussion
The results of our study suggest an association between working at night and menstrual function, including higher prevalence of cycle irregularity, very short cycles, and long cycles. In addition, long working hours were associated with a modestly higher prevalence of irregularity, and a near doubling of prevalence of very short cycles. There were trends towards higher prevalence of irregular cycles and shorter cycle lengths among participants with higher amounts of heavy lifting. The associations of prolonged standing with menstrual function observed in age-adjusted models appeared to be somewhat explained in fully-adjusted models by confounding by heavy lifting; as would be expected, there was a correlation between lifting and standing among nurses.
Most previous studies of work schedule and menstrual function support an effect of night shift work on the menstrual cycle (12–19, 21), though sample sizes were low for some (13, 14, 15, 17, 19), limiting their ability to adjust for confounding factors. Compared to other studies of shift work and menstrual cycle among nurses (13, 14, 15, 18, 19), this is the only study to include nursing students and Canadian nurses, and it has a higher percentage of non-hospital nurses and African-American nurses.
Our previous study of 71 077 participants from the NHS II, the largest study to date, showed that the number of months spent working rotating night shift over the previous two years was modestly related to irregularity, as well as very short (<21 days) or very long (≥40 days) cycle lengths (18). It was unclear in that study, however, if the trends reflected a cumulative dose–response relationship over time, or if women reporting more months of shift work were more likely to have been current shift workers at the time they completed the questionnaire (18).
Our current study shows a suggested trend towards higher prevalence of cycle irregularity with increasing years of rotating night work. A separate analysis of years of rotating night work stratified by current schedule (day versus other) did not show any differences. Thus, our data suggest that there may be a dose–response relationship between number of years working rotating night shift and current menstrual cycle function. Furthermore, it appears that the association does not entirely dissipate when rotating night shift work ceases, at least in the short term. Our measure of current shift work, which includes night work cessation if the participant reported previous night shift but was on a current day shift, was only captured for the prior 12 months. It is possible that effects of night work on menstrual function take >12 months to diminish. In addition, if a participant did cease night work, we do not know when she ceased. Future analyses of NHS3 data may be able to better assess the effects of night work cessation on menstrual function.
In our study, working nights with rotation and without rotation have similar associations with menstrual regularity, though working nights without rotation was not associated with cycle length. Our study also shows a trend towards increasing prevalence of irregularity with higher number of nights worked per month, though the association between number of nights per month and cycle length was less clear, possibly due to lower power among the outcome categories.
More hours of work per week were associated with higher prevalence of irregularity and very short cycle length. Few previous studies have examined working hours and menstrual function. One study reported that working hours among Taiwanese nurses was not related to cycle irregularity (13). Another study reported higher risks of irregularity, amenorrhea, and long cycles with variability in weekly working hours (16), though it did not report the effects of long hours specifically.
Our results showing higher prevalence of irregular cycles and short cycle length with heavy lifting should be interpreted cautiously, because there are few studies of physically demanding work and menstrual function, and the causal relationships between standing, lifting, and other workplace characteristics have not been clearly delineated. A French study of poultry slaughterhouse workers reported that “regularly handling weights” resulted in higher risks of irregular cycles, long cycles, and amenorrhea (16); no effects on menstrual function were noted with prolonged standing. A study of tertiary care nurses showed a higher risk of long cycles among nurses with strenuous job activity (15).
Working during nighttime hours may disturb the reproductive hormones that control the menstrual cycle, possibly through sleep disturbances or altered melatonin production. The mechanisms by which long working hours are related to adverse reproductive outcomes is unclear but, perhaps, are related to stress, mental or physical fatigue, or chronic sleep deprivation, disturbing circadian rhythms (27). Physically demanding work could influence menstrual function via altered circulating androgens (28), or it is possible psychosocial stress or fatigue resulting from repetitive physical demands may result in biochemical responses (eg, increased secretion of cortisol and α-amylase) which may reduce fertility (29).
Our study is limited by a lack of adequate information on sleep behaviors; it is possible that effective sleep hygiene and education may moderate effects of working nights or rotating night shifts (30). In addition, some of our results might have been affected by excluding women who were taking oral contraceptives for irregular cycles. We were also limited by the cross-sectional and self-reported nature of our data collection; however, nurses in the similar NHS I and NHS II were shown to report health data accurately for several medical conditions (31, 32). Previous studies that have investigated the accuracy of self-reported menstrual cycle length by comparing initial self-reported “usual” length with prospective diaries, however, Jukic et al (33) and Small et al (34) reported that 21% of cycle length categories were misclassified. These studies also found that accuracy was better for sexually active women and women with a history of infertility, and that reporting accuracy was lower with irregular cycles and among those with the most extreme lengths. Factors associated with differences in reporting accuracy included parity, BMI, irregular cycles, younger age, single, lower income, and exercise. Misclassification of cycle length is a possibility in the current study, and the direction and magnitude of bias that might arise is difficult to predict. However, it is reassuring that many of the factors that are associated with inaccurate reporting are controlled for in our analyses and that our cohort is comprised of women educated in the medical field. In addition, the fact that we found the expected differences in cycle length with age and BMI suggests that the participants’ self-reported data were adequate. Nevertheless, our study is one of the largest studies to examine work schedule, working hours, and physically demanding work with menstrual function. Thus, we were able to assess a more extreme definition of short cycles than other studies and strengthen our results by adjusting for confounding factors such as age, BMI, and recreational physical activity.
In summary, our results indicate a possible role for night work, long working hours, and physically demanding work in menstrual function disturbances, which may have implications for subfertility (3, 5, 6) and overall health (2). Our study suggests that working rotating nights may have similar effects as working nonrotating nights, and that there may be a dose–response effect with the number of nights worked per month. Questions remain regarding whether the effects from working nights may dissipate once shift work ends. Future research could also assess whether interventions to reduce heavy lifting would improve menstrual function or subfertility.