Established in 2008 and comprising over 60 researchers, the IPD-Work (individual-participant data meta-analysis in working populations) consortium is a collaborative research project that uses pre-defined meta-analyses of individual-participant data from multiple cohort studies representing a range of countries. The aim of the consortium is to estimate reliably the associations of work-related psychosocial factors with chronic diseases, disability, and mortality. Our findings are highly cited by the occupational health, epidemiology, and clinical medicine research community. However, some of the IPD-Work’s findings have also generated disagreement as they challenge the importance of job strain as a major target for coronary heart disease (CHD) prevention, this is reflected in the critical discussion paper by Choi et al (1).
In this invited reply to Choi et al, we aim to (i) describe how IPD-Work seeks to advance research on associations between work-related psychosocial risk factors and health; (ii) demonstrate as unfounded Choi et al’s assertion that IPD-Work has underestimated associations between job strain and health endpoints; these include the dichotomous measurement of job strain, potential underestimation of the population attributable risk (PAR) of job strain for CHD, and policy implications arising from the findings of the IPD-Work consortium; and (iii) outline general principles for designing evidence-based policy and prevention from good-quality evidence, including future directions for research on psychosocial factors at work and health. In addition, we highlight some problems with Choi et al’s approach.
What is the IPD-Work consortium?
The IPD-Work consortium was established at a meeting of principal investigators and researchers working on European occupational cohort studies in London in 2008. In 2010, we obtained funding from the European Union (new OSH-ERA research program) to cover core activities, harmonization of the data across studies, and statistical analysis. Originally, 17 independent cohort studies from Finland, Sweden, Denmark, the Netherlands, Belgium, France, Germany, and the UK were included (2). This number currently stands at 26 studies, including those from the United States and Australia.
Our motivation for establishing the consortium was to advance research on work-related psychosocial factors and health. The most widely studied of these, “job strain”, dates back to 1979 (3). The original hypothesis posits that a combination of high psychological demands at work and low job control (ie, job strain) increases the risk of health problems of public health importance, such as CHD (4). Although the concept was well received by both stress researchers and occupational health specialists, for decades, unresolved debates have hampered interpretation of results and research progress. These include the magnitude of the association, the relative importance of high psychological demands versus low job control (whether one is more toxic than the other), and differences in effect by age and sex (5, 6). Some critics have suggested that observed associations with health are spurious in that job strain is merely a marker of other causal risk factors, in particular socioeconomic disadvantage (7).
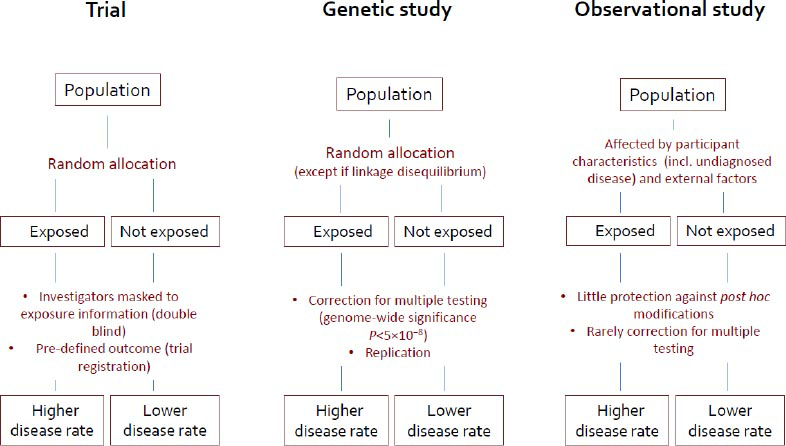
In addition to confounding and bias, a perennial problem in observational studies is the use of post hoc comparisons and selective reporting of findings after multiple testing (figure 1) (8, 9). To address this issue in IPD-Work, we have adopted principles from randomized controlled trials (RCT), one of which is to set out hypotheses and definitions of exposures and outcomes prior to commencing analyses (8, 9). In accordance with these principles, we examined the hypothesized link between job strain and CHD by extracting data from participating cohort studies in two stages: first, the exposure was harmonized across cohorts in a validation study, with investigators masked to outcome information; then, the endpoint of interest, here CHD, was harmonized. To reduce random error, we used the largest available databases to date (197 000 study members contributing 2350 events in the analyses of the job strain-incident CHD relationship, for instance). To test whether observed associations could be replicated across sub-populations, we performed stratified analyses. We excluded disease events that occurred in the first years of follow-up (left-censoring) from the analyses to reduce reverse causation bias. Finally, to evaluate publication bias, we used both published and unpublished data.
Figure 1
Evidence of a risk factor–disease association from a randomized controlled trial (gold standard), a genetic study and a conventional cohort study. This figure has been modified from an earlier version (8).
The IPD-Work consortium has provided new insights into three longstanding debates on job strain and CHD (10). First, the combination of high demands and low control is a more robust risk factor than either component alone, supporting the original job strain theory. Second, there are no important differences in the association of job strain and CHD between men and women, between the young and the old, or between socioeconomic groups. Lastly, there was some suggestion of publication bias: in three studies included in IPD-Work that had been published previously, the hazard ratio (HR) for CHD in those reporting job strain relative to those who did not was 1.43 [95% confidence interval (95% CI) 1.15–1.77]. The HR based on ten studies that had not been published before was smaller although still statistically significant, 1.16 (95% CI 1.02–1.32). The combined HR was 1.23 (95% CI 1.10–1.37).
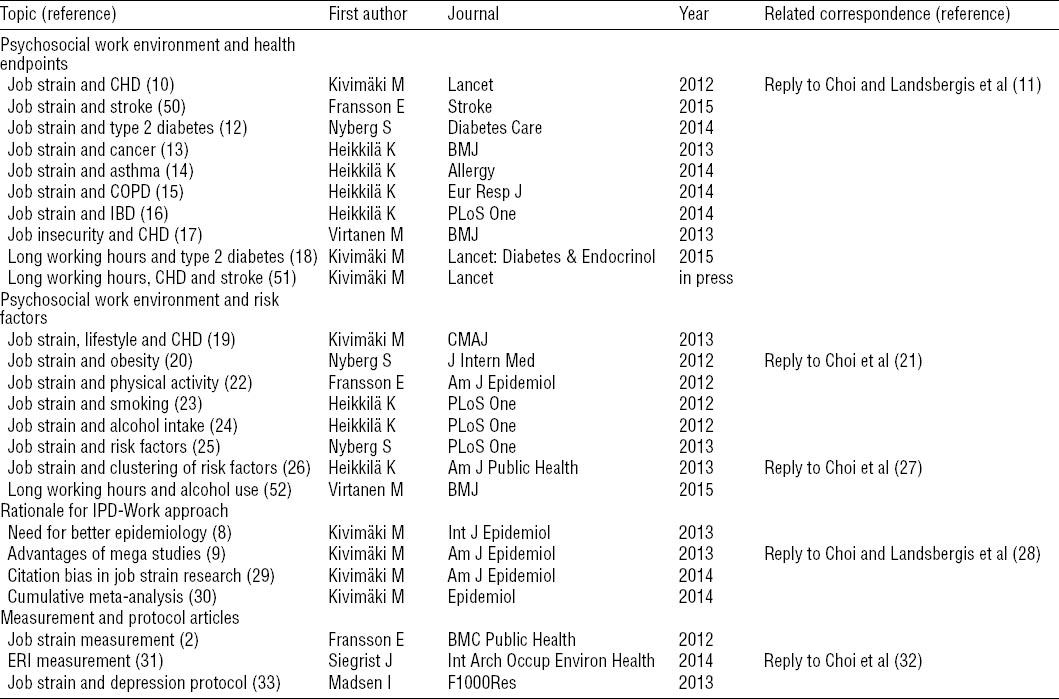
Table 1 provides an overview of the output from the IPD-Work collaboration (2, 8–33). We also include our published replies to the comments received previously by Choi and others, which were not provided in their most discussion paper (1). Our published meta-analyses have been through the rigorous editorial and peer review processes characteristic of high-impact journals and cover a range of prospective associations of job strain with cardiovascular disease risk factors (smoking, obesity, alcohol intake, hypertension, and so on) and disease endpoints, such as CHD, stroke, type 2 diabetes, cancer presentations, chronic obstructive pulmonary disease (COPD), asthma, and inflammatory bowel disease. Recognizing that job strain is only one of many aspects of the psychosocial work environment, we are also studying other potential predictors including job insecurity, long working hours, and effort–reward imbalance (ERI).
Do IPD-Work findings underestimate the associations between job strain and health?
Choi et al (1) argue that findings from IPD-Work underestimate the association between job strain and health. In responding to this point, we compare our results to those from other collections of studies.
Coronary heart disease
The summary relative risk (RR)for job strain from a meta-analysis of the 16 cohort studies published before IPD-Work is 1.39 (95% CI 1.23–1.59) (table 2) (10, 30). This is in agreement with the summary RR of 1.43 (95% CI 1.15–2.17) from the three studies in IPD-Work, which had also previously published findings on job strain and CHD (10). In the only study published after IPD-Work, of which we are aware, a similar RR was reported: 1.31 (95% CI 1.01–1.70) (34).
Table 2
Summary estimates for job strain and risk of coronary heart disease in IPD-Work and related studies
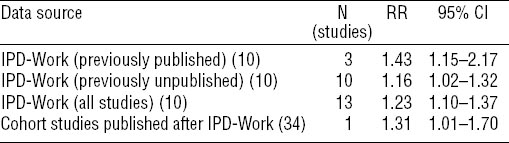
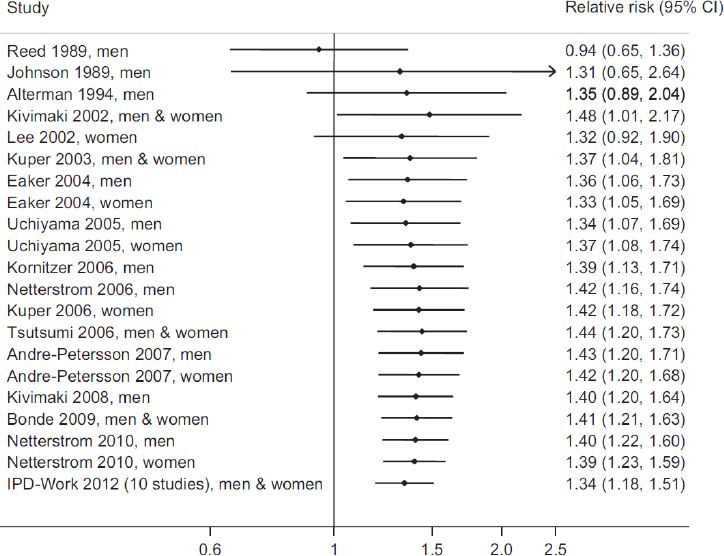
In figure 2, to illustrate chronological changes in the summary HR, we have recomputed the aggregate effect estimate for job strain and CHD with the addition of each new study (30). For the first time, a stable and statistically significant association between job strain and CHD was apparent in 2003 after the first six cohort studies had been published. The summary RR for job strain was 1.37 (95% CI 1.04–1.81). Although reports from an additional 20 cohort studies on the same topic have been published (including the 10 previously unpublished IPD-Work cohorts), the summary estimate is essentially unchanged at 1.34. Using 95% CI rather than point estimates to ensure a cautious interpretation, overall the evidence from cohort studies suggests that the RR of CHD associated with job strain is somewhere between 1.2–1.5.
Figure 2
Cumulative meta-analysis of cohort studies on job strain and incident coronary heart disease for studies identified in the most recent systematic review. Reproduced with permission from Kivimäki M, Batty GD, Ferrie JE, Kawachi I. Epidemiol 2014; 25(3): 464–5 (30).
Type 2 diabetes
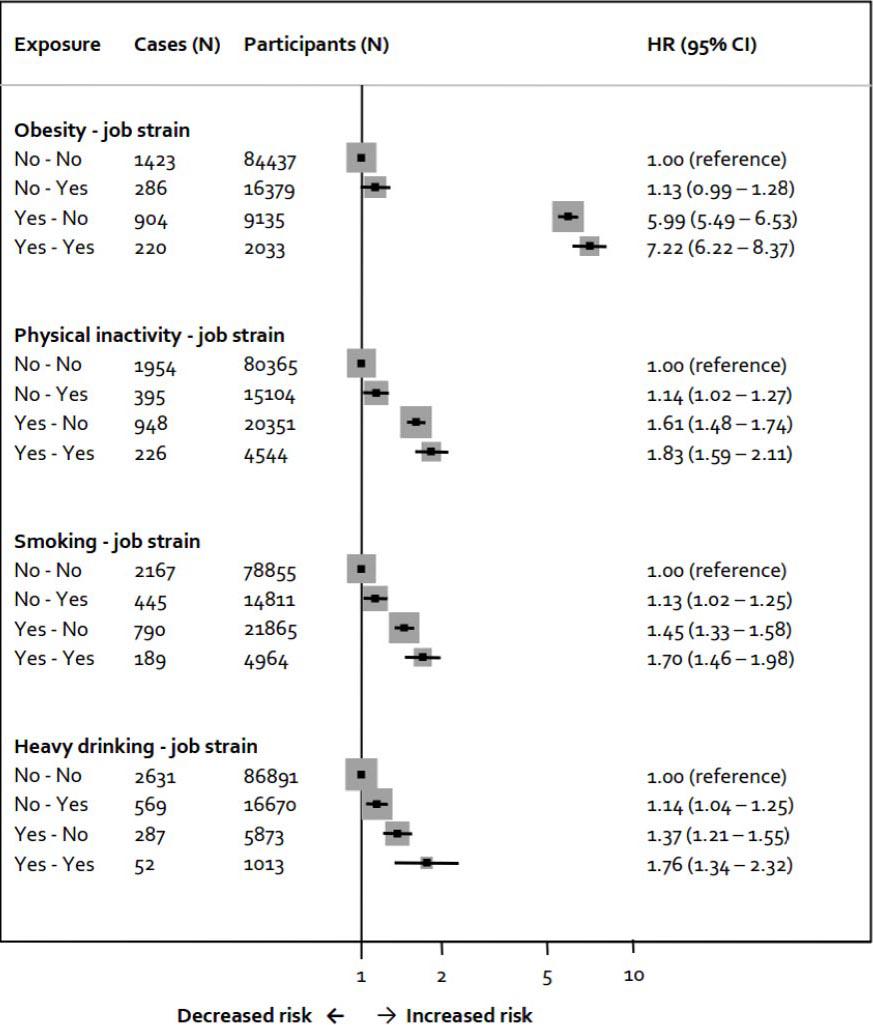
The most recent systematic review and meta-analysis published before IPD-Work on job strain and the risk of type 2 diabetes identified only four relevant cohort studies, with a summary RR from these studies that suggested a weak association, if any (1.08, 95% CI 0.84–1.32) (35). In IPD-Work, harmonized data from 13 cohort studies allowed us to examine this association. The HR for job strain compared with no job strain in relation to type 2 diabetes risk was statistically significant, 1.15 (95% CI 1.06–1.25), with no apparent difference between men (1.19, 95% CI 1.06–1.34) and women (1.13, 95% CI 1.00–1.28) nor according to lifestyle status, characterized in different ways (figure 3) (12).
Figure 3
Association of job strain with type 2 diabetes in healthy and unhealthy lifestyle subgroups. Reproduced with permission from Nyberg ST et al. Diabetes Care 2014;37:2268–75. (12)
Other chronic diseases
Evidence regarding the associations of job strain with cancer (all sites combined and individual presentations), asthma, inflammatory bowel disease and COPD is lacking or, if sparse, reveal discordant results. Analyses from IPD-Work suggest that job strain is unlikely to be an important risk factor for colorectal, lung, breast, or prostate cancers (13), inflammatory bowel disease (16), severe asthma exacerbations (14), and COPD exacerbations (15) leading to hospitalization or death. We cannot exclude the possibility that, despite the large IPD-Work datasets, we missed small effects due to limited statistical power for selected health outcomes (such as less common malignancies), imprecise exposure measurement, or residual confounding. Nevertheless, we strongly believe it is important to publish these null findings, both to address the problem of publication bias and contribute to the evidence base.
Taken together, we find no evidence to support the assertion that the associations observed between job strain and health endpoints in IPD-Work have been underestimated.
Measuring job strain – problems with Choi et al’s approach
In our paper on job strain and CHD, we include the following caveat “we measured exposure to job strain on the basis of one baseline assessment; however, some studies have suggested that cumulative exposure to job strain, ascertained by several assessments repeated in time, could be a stronger predictor of coronary heart disease.” (10, p1495). In the latter context, we make reference to analyses from the Whitehall II study (36). Repeat measures of conventional risk factors and potential confounding factors, compared to one-off baseline measurements, are similarly likely to be stronger predictors of disease, so it is vital also to include repeat assessments of these in the analyses to ensure equivalent treatment (37, 38). Presumably in an unintentional oversight, Choi et al urge us to use repeat assessments of work stress but neglect to suggest we apply this approach to other risk factors or putative confounders, an omission that is likely to lead to an overestimation of the effect of job strain.
Choi et al offer several post hoc justifications for excluding cohorts from our meta-analysis that will have the effect of increasing the RR of CHD in relation job strain. They claim that 4 of 13 cohorts did not meet the quality criteria set out in our paper describing the harmonization process (2). This is not correct. In that paper, we conclude that: “a high agreement for partial scales with at least half of the items of the complete scales, and an accurate classification of job strain when at least one of the scales has no missing items, suggest that these abbreviated scales assess the same underlying concept as the complete survey instrument. However, all the partial scales in the present study (including the subscales comprising only two items), showed high to reasonable agreement with the complete scales.” (2, p7). While harmonization of existing data is often imperfect, this does not mean that studies with less-than-perfect measures should be excluded. Post hoc decisions to exclude studies from a meta-analysis for the purpose increasing the effect size are precisely the kind of practice IPD-Work was established to combat.
Although the job strain concept was launched 35 years ago, there is still no consensus on the best measure. In response to IPD-Work publications, Choi and colleagues have suggested post hoc modifications to our measure, as well as alternative operationalizations. In their commentary (1), they recommend a quartile-based definition of job strain which they say is “theoretically” promising as evidenced by a solitary cross-sectional study in which an association was seen between job strain and leisure-time physical activity, which varied by sex and education level (39), and a methodological paper comparing the original and modified scales in a sample of 682 Swedish adults (4). Their request is not new: Choi’s colleagues have previously proposed multiple operationalizations of job strain, such as the quotient, the quadrant term, the quadrant term using national means, and linear term formulations (41).
Multiple and changing exposure definitions not only hinder comparison and pooling of evidence but also limit conclusions from being drawn as they makes it impossible to determine whether differences between studies are real or attributable to data handling. Availability of alternative exposure definitions may also encourage researchers to selectively report results that best support their own hypothesis, contributing to publication bias and false positive findings. It is particularly notable that despite promoting the use of multiple indicators, Choi and colleagues do not recommend external criteria for measurement validation or, crucially, corrections for multiple testing, given the known propensity of multiple testing, which they propose, to increase false positives.
What is the PAR of job strain for CHD?
Based on the results of our analysis, we previously suggested that prevention of workplace stress might decrease CHD incidence, albeit to a lesser extent than that achieved by tackling standard CHD risk factors (10). Choi et al do not agree with this interpretation based on the argument that our population attributable risk (PAR) evaluations are underestimates. They claim that exclusion of data from the four cohort studies that fail to meet their interpretation of the eligibility criteria increases the PAR% of job strain for CHD from the reported 3.4% to 4.9%. To contextualize this estimate, we report PAR for job strain alongside those for standard cardiovascular risk factors, including unhealthy lifestyle, obesity, high blood pressure, dyslipidaemia, and diabetes. PAR is a tool used to assess the extent to which removing a risk factor might reduce disease events.
The PAR of job strain for incident CHD needs to be interpreted cautiously (10, 19) since we do not know the extent to which the association observed between job strain and CHD is truly causal (an underlying assumption in the PAR calculation) and whether it is accurate. With the same reservations, the PAR of smoking, heavy alcohol use, physical inactivity, and obesity combined was much higher: 26% in IPD-Work (19). We have not evaluated PAR for other established risk factors due to lack of harmonized data, but in the US Atherosclerosis Risk in Communities (ARIC) study (42), the PAR of smoking (11% and 14% in men and women, respectively), obesity (4%; 8%), high blood pressure (19%; 23%), high cholesterol (13%; 3%) and diabetes (14%; 21%), in combination, was 50% for men and 60% for women. In this context, it makes little difference whether the PAR of job strain is 3.4 % or 4.9%. The combination of several work-related psychosocial factors, which may represent overlapping constructs, may yield a PAR that is higher than the one that we found for job strain alone, although without evidence from prospective studies on multiple psychosocial factors and CHD this remains speculative.
As Choi et al note, the cost of cardiovascular disease prevention and treatment is very high. This is mainly because of shifts in the age-structure of most populations towards older ages, leading to increase in the absolute number of people with age-related diseases, such as CHD. However, favorable changes in cardiovascular disease rates is one of the great successes of modern public health: age-adjusted rates of cardiovascular disease mortality have decreased by over 70% since the 1950s in the United States, with similar age-adjusted reductions apparent in many other high-income countries (43). Modeling studies suggest that improvements in treatment and reduction of standard risk factors (obesity and diabetes being exceptions to this general rule) explain most of this age-adjusted decline in CHD mortality (43).
Policies that enable individuals to make and maintain healthy living choices are needed if prevention strategies including early detection and cost-effective management of CHD and their risk factors are to be comprehensive. In this context, tackling the psychosocial work environment might have an important role in working populations (43). It is possible that job strain and other psychosocial factors represent “causes of the causes”. Identifying and tackling such upstream factors is a key aim for public health research and policy, as it is believed that this approach may provide greater benefits for population health than addressing individual health behaviors or risk factors (44).
IPD-Work’s findings on job strain as a “cause of the causes” is mixed. We found that those experiencing job strain were more likely to become physically inactive as assessed via questions on leisure time activity, compared to those free of job strain (22). Using cross-sectional data, we also found a link between job strain and obesity, however, in longitudinal analyses a temporal sequence from job strain to obesity was not confirmed (20). Importantly, persons reporting a reduction over time in job strain did not experience a reduction in obesity risk. This suggests that job strain interventions alone are unlikely to alleviate the obesity epidemic, even in the working population. Associations of job strain with smoking and alcohol intake were similarly modest (23, 24). Taken together, our results indicate that if job strain is indeed a cause of the causes, its impact is relatively modest. Consequently, we feel it is unlikely that a reduction in job strain would have a large effect on CHD via effects on conventional risk factors.
There are other weaknesses in Choi’s et al arguments regarding the PAR of job strain. Contrary to their assertion, under-representation of low socioeconomic status (SES) groups in several IPD-Work cohorts is unlikely to introduce significant underestimation of the PAR of job strain. The PAR estimate is a function of two components: prevalence of job strain and its association (RR) with CHD. The proportion of low SES participants in a cohort study has no effect on the prevalence of job strain because job strain is defined using the distribution of job demand and job control values in each cohort (above-median demand scores combined with below-median control scores defined job strain) (10). Furthermore, the relative risk of CHD in study participants reporting job strain did not differ between high and low SES groups (10).
Choi et al suggest that loss to follow-up over the course of the study (sample attrition) biased our associations towards the null in our studies as those with job strain were perhaps also more likely to drop out of the study. They refer to a report on job strain and self-reported depressive symptoms based on data from the Belstress study (45), a contributor to IPD-Work, to support their claim. Choi et al appear not to have realized that our outcome, CHD, was not taken from self-reports and hence not dependent on participation in follow-up examinations. Incident CHD cases in IPD-Work were identified using linkage to hospitalization and mortality records in all the cohort studies included in our meta-analyses. Hence our PAR estimates were unaffected by attrition. Choi et al also raise concerns about the choice of reference group used in IPD-Work, that is, those free of job strain. Their preference would be to use more extreme low job strain groups, such as the bottom third or fourth based on a continuous job strain score. The policy implications of such extreme reference groups are perhaps unrealistic as they would require a reduction in job strain to the extent that all employees have low job demands and high job control (ie, low job strain).
Choi’s and colleagues’ presentation of the evidence for higher PAR for work stress is misleading. They cite a paper by Niedhammer et al (46) that indeed reported a PAR of 18.2% for effort–reward imbalance with CVD as the outcome using data from 31 European countries participating in the 2005 European Working Conditions Survey. However, Choi et al fail to acknowledge that (i) the PAR was statistically non-significant (95% CI -2.6–39.0%), (ii) the 31 European studies did not have data on CVD, and (iii) the PAR was simply calculated using a statistically non-significant RR estimate from another study (2.05, 95% CI 0.97-4.32 based on a meta-analysis of three cohort studies). Thus, the evidence for a PAR of 18.2% is uncertain and indirect. Choi’s et al suggestion of a PAR of 10–20% appears to be taken from a declaration resulting from an occupational health conference in Japan (unhealthywork.org/news/hot-topic-the-tokyo-declaration-on-prevention-and-management-of-work-related-cardiovascular-disorders/) which has no reference to empirical evidence and refers to work exposures in general, including physical and chemical, not just psychosocial exposures.
Policy implications and the GRADE system
In many countries, preventing excessive work stress, including job strain, is a legal obligation. We fully support the view that exposure to adverse working conditions, such as job strain, is unethical. However, this is a separate issue from whether job strain ought to be considered as a major target for CHD prevention.
Prevention strategies are based on an evaluation of the evidence on benefits and harms using systematic and transparent approaches, such as GRADE (Grades of Recommendation Assessment, Development and Evaluation) (47). In GRADE, evaluation for scientific quality begins with a systematic review of the best available evidence for a given risk factor. The evidence is initially graded on the basis of the strength of the study design with randomized trials representing “high quality”, observational studies denoted as being “low quality” and all other data, such as expert opinions, described as “very low quality”. The initial grade can be downgraded if there are serious limitations in the evidence or important inconsistencies between studies, if the data are sparse or imprecise, the outcomes are measured only indirectly, or if there is a high probability of publication bias. There are also issues that can lead the quality grade to be upgraded, such as a particularly strong association by the standards of modern epidemiology (ie, RR >2 or <0.5) confirmed by consistent observational evidence with no plausible confounding or major threats to validity. However, speculations regarding factors that might have led to underestimations in observed associations, such as those presented by Choi et al are not regarded as a reason to upgrade quality ratings.
The aim of IPD-Work is to conduct rigorous analysis to achieve the strongest possible evidence within the limitations of observational research. We believe that this is of greater relevance to policy than the approach by Choi et al, which appears to be based on weak evidence. Endorsements of our approach come from various sources. According to Thompson Reuters Web of Science, our paper on job strain and CHD (10) is in the top 1% in the field of Clinical Medicine based on a highly cited threshold for the field and year. Use of the individual-participant meta-analysis approach in relation to work-related psychosocial stressors was a major reason for the American Heart Association Spotlight Scientist in Cardiology award for the lead investigator of IPD-Work in 2012 (circ.ahajournals.org/content/126/17/f97) (48). Our findings on job strain and CHD (10) and on long working hours and type 2 diabetes (18) have also attracted considerable interest in media, as evidenced by news stories world-wide (Appendix, www.sjweh.fi/data_repository.php).
This notwithstanding, we acknowledge that, according to GRADE, a major limitation to research on the effects of job strain on CHD, including our own research, is a lack of RCT: the gold standard study design. This limits researchers’ ability to confirm the causal nature of the association between job strain and CHD and evaluate the extent to which interventions to reduce job strain would reduce disease risk. Choi et al list a number of workplace intervention studies, but none of these in fact featured CHD as the endpoint of interest (1). Evidence that job strain interventions reduce sickness absence is insufficiently disease-specific to justify the inclusion of job strain as a target for CHD prevention. Without evidence from intervention studies, the GRADE conclusion that applies to the evidence to date on job strain, and one that seems most reasonable to us, is that “the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different” (49, p404).
Research on psychosocial work environment and health: Where do we go from here?
As shown in figure 2, the RR of 1.2–1.5 for job strain and CHD ascertained by 2003 has remained unchanged despite the inclusion of numerous subsequent studies and considerable associated research costs. As the addition of further studies with similar designs is unlikely to change this estimate, we must now seek improved designs and alternative approaches to gain new information on the link between work-related psychosocial factors and CHD. In IPD-Work, we plan to examine the little-examined links between psychosocial factors other than job strain (eg, ERI, job insecurity and long working hours), including their combined effects, and other health outcomes (table 3). Choi et al have repeatedly expressed their unhappiness with our approach and provided recommendations on how meta-analysis on work-related psychosocial factors and health should be undertaken. We respectfully suggest that it is time for them to put their suggestions into practice. Their results, if published in peer-reviewed journals, will allow comparison with our own and move the field more forward than unmoderated web-based postings or rarely-reviewed repeat letters of criticism that provide no new empirical data.
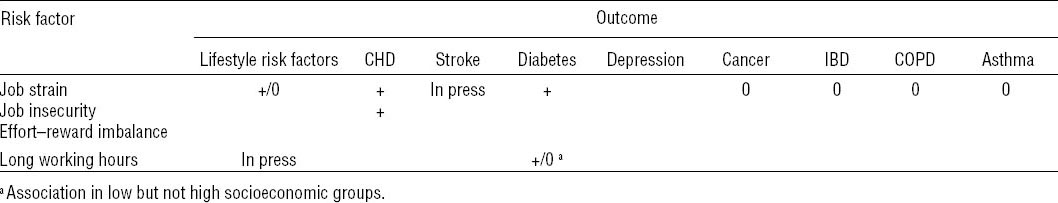
Table 3
Summary of associations examined in IPD-Work ( + = association, 0 = no association, - = inverse association, empty = not studied yet) [CHD=coronary heart disease; COPD=chronic obstructive pulmonary disease; IBD=inflammatory bowel disease].
We encourage researchers in the field to conduct intervention studies designed to determine whether the associations observed between work-related psychosocial factors and disease endpoints can be confirmed in experimental designs, such as individual RCT, cluster-randomized trials, or natural experiments. Obviously, such studies come with great challenges, but they are needed to advance research in a field which hitherto has been dominated by observational evidence. One way to support such developments is to encourage journals, such as Scand J Work Environ Health, to publish even small and underpowered pre-registered RCT on work-related psychosocial factors and health. This will lead, over time, to the accumulation of an evidence base sufficient, when pooled, to evaluate the extent to which psychosocial factors are causally related to disease outcomes and amenable to change.