The aging of the working population and intensification of work are structural trends tending to increase the incidence of musculoskeletal pain and disability (1). Interventions in the workplace have been developed to facilitate return to and maintenance of work (2). The Sherbrooke model has proved more effective than conventional care in facilitating return to work (RTW) after low-back-pain disability (3). It is characterized by its early time frame (four weeks of work absence), and its change of paradigm in rehabilitation. Its first component is not a medical but a participatory ergonomic intervention in the workplace to facilitate work accommodation and the RTW of the worker with low-back pain. Its second step is implemented only if necessary after 12 weeks of work absence, with the so-called “therapeutic” approach with a progressive and adapted RTW under the supervision of a facilitator (ergonomist or occupational therapist) (4). Despite demonstrations of its good internal validity and cost-effectiveness (5) and an implementation plan (6), the model failed to be included in the healthcare system in Québec (7). Other failures of implementation and sustainability of work disability prevention interventions have been reported (7).
Work disability prevention interventions show all the criteria of complex health interventions (8). They require change in representations and behavior at different levels in categories of agents with conflicting interests (7). Designing RTW programs in the form of such complex interventions requires careful attention to conditions of implementation and their sustainability beyond the clinical trial stage, which assesses efficacy in experimental conditions (9).
It has been found that the spread of innovations and the implementation of health programs run up against many barriers at the individual, organizational, and contextual (economic, legal, political, social and cultural) level (9, 10). For this reason, it has been recommended that the context in which a new intervention is to be implemented be analyzed and barriers and facilitators be identified in order to guide strategy (9). However, there is no clear indication as to how these barriers and facilitators should be identified (11).
In France, reducing low-back pain disability has been made a public health priority. A scientific task force on low-back pain recommended the assessment of the Sherbrooke therapeutic RTW approach (12), and the Workers Compensation Board (Assurance Maladie, Direction des Risques Professionnels) funded a research project to evaluate the feasibility of the Sherbrooke model in France. This study was deemed necessary due to some characteristics of the French context which contrast with the Sherbrooke model, namely an over-medicalization of low-back pain and the predominance of a hospital-based approach to rehabilitation (13). Therefore, a specific conceptual framework was developed to analyze the feasibility of a RTW intervention for workers with low-back pain (14). Using this framework, the present study sought to identify barriers and facilitators in implementing the Sherbrooke model in two regions of the French health system at individual, organizational and contextual levels for three categories of agent: workplace actors, healthcare professionals, and health insurance agents.
Methods
A multiple case study with nested levels of analysis was performed (15). This method of qualitative research is commonly used in health service research (16). The cases were two geographical health system regions; the analysis levels were individuals, organizations, and general contexts.
Participant sampling
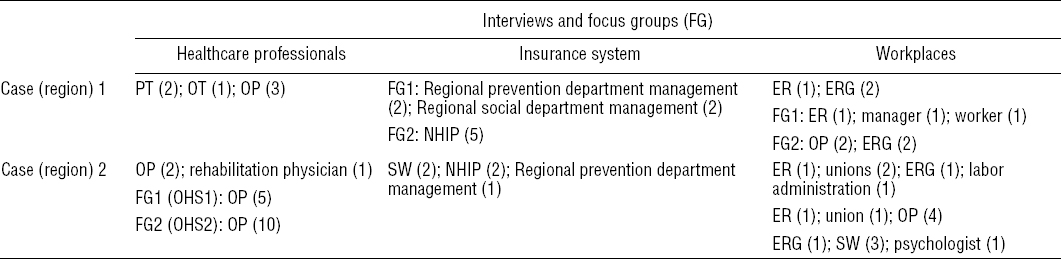
Two regions of France were selected for their high prevalence of musculoskeletal disorders. In each one, a theoretical sampling strategy (17) was drawn up based on the categories of the “arena” model in work disability prevention (7). First, purposeful sampling included three key informants per region for each category of actor. Then snowball sampling per region identified participants in each category. Table 1 presents participant characteristics and the means of data gathering.
Table 1
Respondent characteristics per region. Some respondents were involved in both the interview and focus group. [ER=employer; ERG=ergonomist; NHIP=national health insurance physician; OHS=occupational health service; OP=occupational physician; OT=occupational therapist; PT=physical therapist; SW=social worker.]
Data collection
The participants were involved in a structured transfer of knowledge of Sherbrooke model theory and practice. After this 3-hour training session, data were collected by semi-structured individual interview (N=22) and focus groups (N=7) led by an investigator. Focus groups were homogeneous in terms of background and occupation with no primary intention to explore divergences or reach consensus among the participants. The questions were based on the conceptual framework (14) and concerned perceived needs for a Sherbrooke-type intervention, perceived difficulties of understanding and use, perceived pros and cons, perceived usefulness, and compatibility with the participants’ values and practices. In two rehabilitation centers, triangulation of data collection modes was used to improve accuracy. Participant observation (inclusion of low-back pain patients in functional restoration programs) provided a description of individual and organizational practices. Gray literature (annual activity reports, internal procedures) was used to triangulate these observations and participants’ responses. The questions used with each data collection mode were the same: who does what, how, when, where and why? The findings obtained by these different means were concordent.
Study context
Data were collected in two rehabilitation centers, two national health insurance offices, three occupational health services, and four workplaces with high rates of absenteeism for low-back pain (a car maker, one association providing home services for the dependent, and two university hospitals). Data collection was performed between March 2006 and May 2007.
Data analysis
All interviews and focus group meetings were recorded, transcribed, and collated in a single database. Mean interview time was 59 minutes (range, 22–180 minutes). The ATLAS.ti v5.2 (Berlin) thematic qualitative content analysis software was used to analyze and compare content from each region (15). Coding reliability was checked by a second investigator using co-coding, and disagreements were resolved by discussion. The eight dimensions of the initial conceptual framework were used as core categories of analysis in a deductive fashion. Some categories were modified and/or refined in an inductive way (such as “top and frontline management” included in organizational practices) so as to be able to take into account all the data. The rationale for the modifications and the final conceptual framework are detailed in a previous publication (14). Analytical categories were deemed saturated when further interviews provided no new input.
For accuracy considerations, a preliminary report was sent to the participants who were requested to precise, correct, or confirm its content as far as necessary. Eight participants answered they had no comment. Four participants had minor changes. No disagreement was expressed. All answers were appended to the final research report.
The principal investigator kept a log-book during the research project. Pro-innovation biases favoring the Sherbrooke model were identified and taken into account to analyze discordant values expressed by some respondents.
The research review board of Charles LeMoyne Hospital, Longueuil, Quebec, approved the research protocol. All participants signed an informed consent form.
Results
Healthcare system (table 2)
Table 2
Barriers and facilitators in the healthcare system. [GL=gray literature; GP=general practitioner; LE=legislation; OB=observation; RTW=return to work; SV=stakeholder views.] Content in italic font refers to the data collected.

External context: barriers
At the legal level, medical confidentiality was identified as a barrier to collaboration between general practitioners (GP), national health insurance physicians (NHIP) and occupational physicians (OP). GP cited the complexity of administrative procedures as discouraging. The “payment by act” system was seen as a source of over-medicalization (table 2).
External context: facilitators
At the legal level, one facilitator was the possibility of structuring care in a network associating primary/secondary care, public/private sector and occupational medicine/rehabilitation. Certain legal provisions allow gradual RTW, in line with the Sherbrooke model.
Organizations (rehabilitation center, occupational medicine department, community physician): barriers
Lack of interest in RTW on the part of certain rehabilitation structures and GP was cited as a barrier, with treatment objectives unrelated to work. Lack of human and financial resources to enable workplace interventions was highlighted. Lack of structured collaboration was another barrier, whether between healthcare professionals or with other sectors (workplace, health insurance).
Organizations: facilitators
An organizational culture integrating work disability prevention was identified as a facilitator, as was a policy of screening at the sub-acute low-back pain stage with resources allocated for workplace intervention (ergonomist). Certain rehabilitation centers set up collaborations with occupational health services and community physiotherapists.
Individuals (health professional, patient): barriers
Physicians’ lack of knowledge of work and the relevant legislation was clearly identified as a barrier. A strictly biomedical vision of low-back pain was associated with objectives centered on cure without concern for RTW. Some practices amounted to over-medicalization, with lack of collaboration and mutual distrust between physicians. Healthcare professionals’ reticence regarding movement was identified as a barrier. Finally, overwork and lack of time were unanimously cited as a barrier to involvement in this type of model.
Individuals: facilitators
Conversely, some healthcare professionals had a clear understanding of the legal bases and issues in RTW. They had a biopsychosocial vision of low-back pain. Their perception of their professional role included the social dimension over and above healthcare as such. These people were more used to teamwork with others.
National health insurance system (table 3)
Table 3
Barriers and facilitators in the national health insurance (NHI) system. [GL=gray literature; GP=general practitioner; LE=legislation; OB=observation; RTW=return to work; SV=stakeholder views.] Content in italic font refers to the data collected.
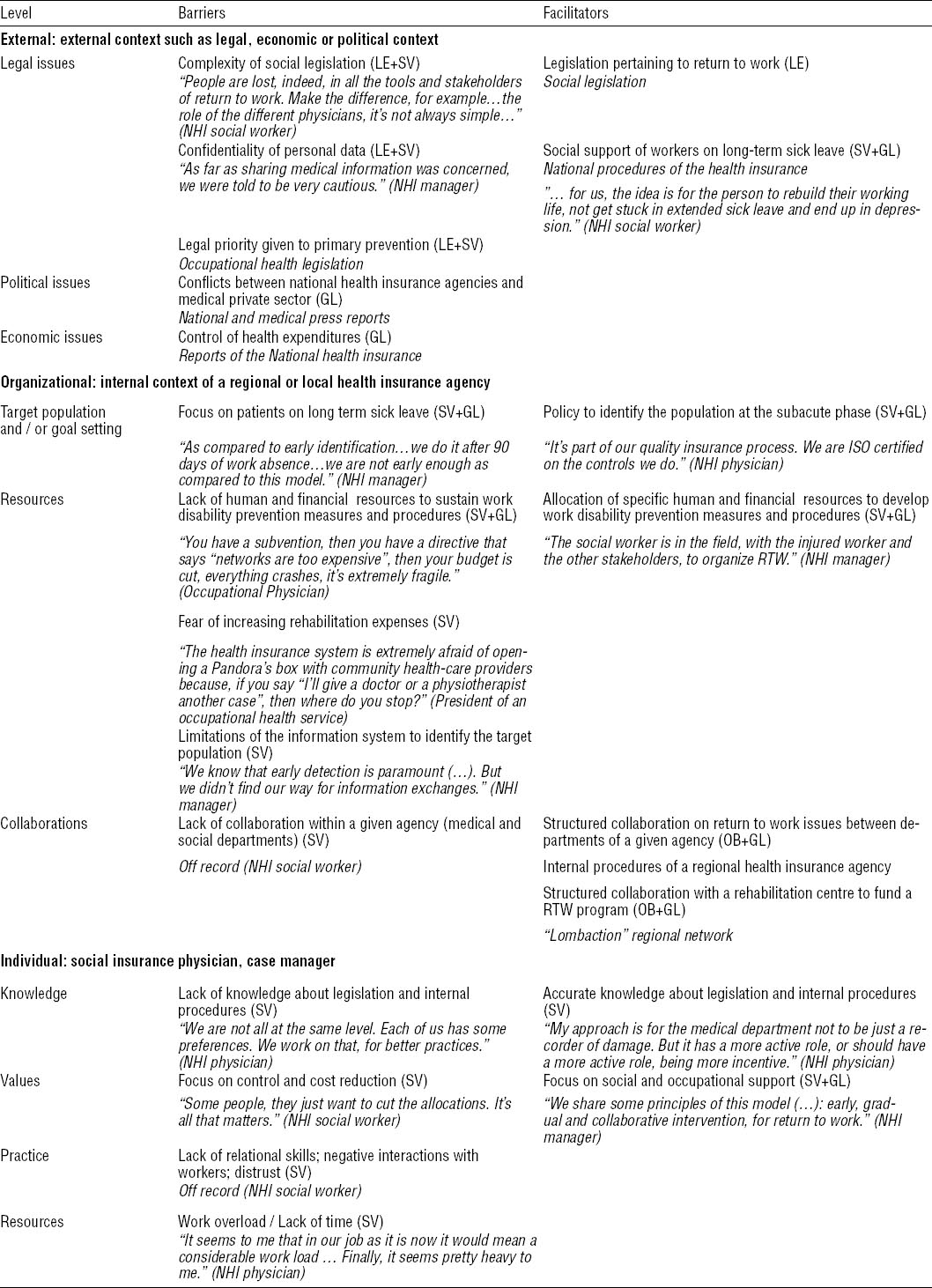
External context: barriers
Respondents working in the national health insurance system itself underlined the complexity of health insurance law as a barrier. Legal barriers to sharing personal data were cited as a barrier to identifying workers at the sub-acute phase. The priority given in the legislation to primary prevention was seen as a barrier to developing solutions in tertiary prevention. Economically, limitations of health expenditure were cited as a barrier.
External context: facilitators
Health insurance procedures for accompanying workers on sick leave for >3 months were identified as a possible facilitator, as was the legislation on therapeutic part-time work.
Organizations (health insurance agencies): barriers
The priority given to workers on >6 months’ sick leave was cited as a barrier to early interventions. Lack of resources to develop more interventions was underlined. Fear or refusal of increased rehabilitation expenditure was reported as hindering the development of ergonomic intervention in favor of RTW. Some health insurance agencies showed a lack of collaboration between departments: administrative, medical and social.
Organizations: facilitators
Dedicated procedures for identifying low-back pain patients as of 3-months’ sick leave were seen as a facilitator in some national health insurance agencies. At a regional level, setting up structured collaboration with a rehabilitation center to finance a RTW program was cited. At a local level, teamwork between the administrative, medical and social departments of one agency was mentioned as facilitating.
Individuals (national health insurance physicians, case managers): barriers
Lack of knowledge of the relevant legislation and internal procedures of the national health insurance system was cited. The priority given to limiting health expenditure was also stressed, associated with mistrust of workers and other actors. Lack of time and overwork were unanimously identified as barriers.
Workplace system (table 4)
Table 4
Barriers and facilitators in the workplace system. [GL=gray literative; GP=general practitioner; LE=legislation; OB=observation; RTW=return to work; SV=stakeholder views.] Content in italic font refers to the data collected.
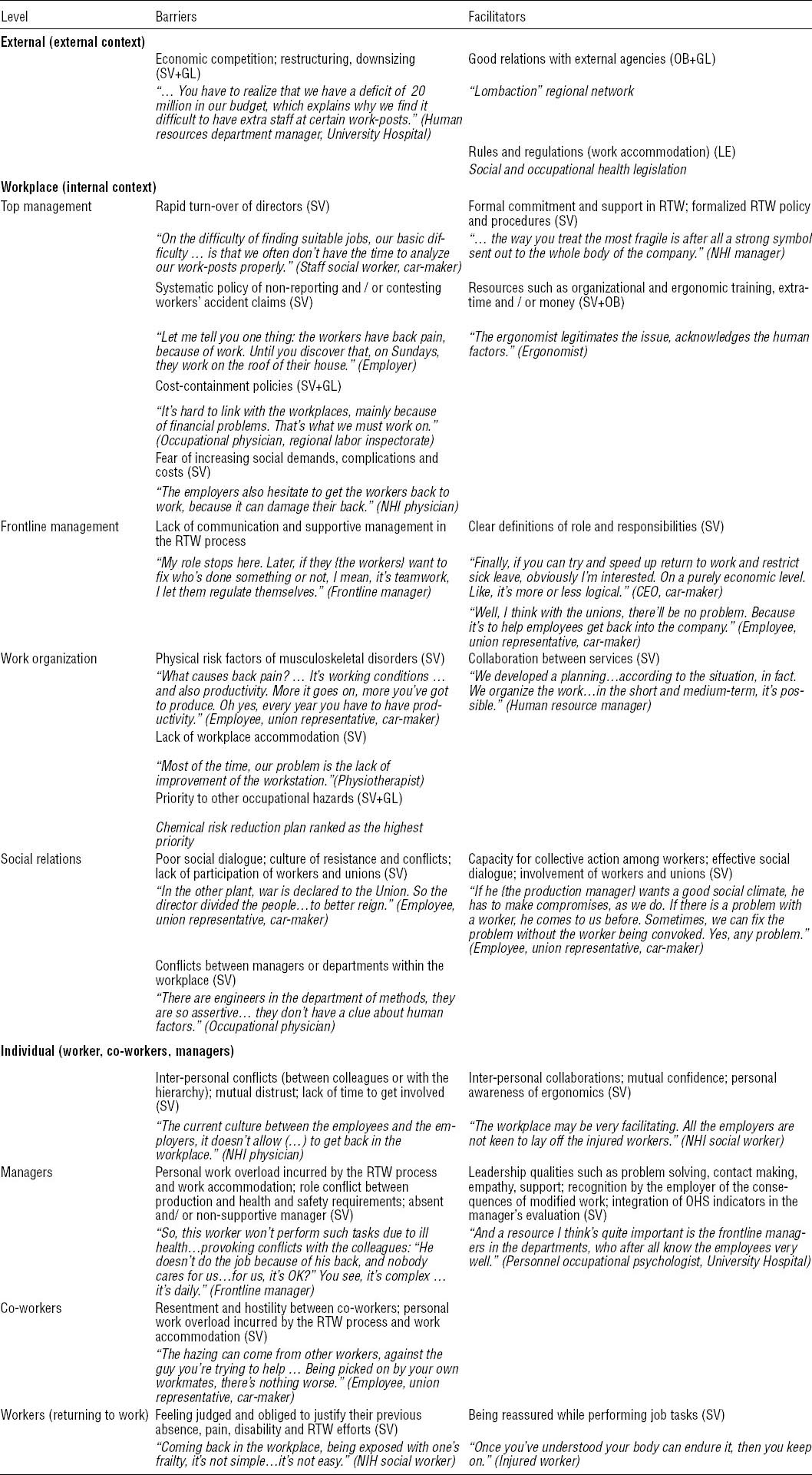
External context: barriers
A competitive economic context, with restructuring and workforce reduction, was cited as a barrier to the feasibility of the Sherbrooke model.
External context: facilitators
Legally, the regulations concerning job accommodation for disabled workers and the prevention of occupational risk (French Employment Code) were mentioned. Good company relations with the occupational health and safety departments and national health insurances agencies (prevention department) were cited.
Workplace: barriers
At management level, fast managerial turnover, lack of latitude in decision-making and the fear of increasing costs and claims for better working conditions were cited as barriers. At the frontline management level, lack of communication between the manager and the team about RTW and lack of support to injured workers were highlighted. In work organization, production rates, workforce downsizing, use of temporary staff, failure to accommodate work posts and the priority given to other occupational risks were identified as possible barriers. In terms of social relations, a culture of contestation, with conflicts between branches of management and/or departments within a given establishment was mentioned as a barrier.
Workplace: facilitators
At management level, official commitments on RTW issues, with formalized procedures and ear-marked resources (job accommodation, extra temporary workers), were mentioned as possible facilitators. A perception of the Sherbrooke model as able to improve working conditions and corporate public image, reducing sick-leave duration and costs, was seen as a facilitator. The possibility of financing ergonomic intervention from outside budgets was mentioned as a possible facilitator. The personal involvement of the OP was underlined as a positive factor. In terms of social relations, the involvement of workers and unions in occupational health issues was underlined as a facilitator. At frontline management level, clear definition of roles and responsibilities in occupational health issues was considered positive.
Individuals (workers; colleagues; managers): barriers
The existence of interpersonal conflict with colleagues or managers was mentioned as a barrier, as was mutual mistrust. For managers, overwork, role conflict between production targets and occupational health and a lack of hierarchic support were possible barriers. With colleagues, overwork and skepticism about medical problems could induce hostility and rejection. For workers with LBP, the feeling of being judged and having to justify absence, pain and limitations was perceived as a barrier.
Individuals: facilitators
Conversely, collaboration with colleagues and superiors and mutual trust were underlined as facilitators. Qualities of leadership such as problem solving, and relationship capabilities such as empathy and support were mentioned. The perceived benefit of the Sherbrooke model, recognition by the employer of the consequences of job changes, and the inclusion of occupational health indicators in management assessment were cited positively.
Discussion
The present results confirm the variety of barriers to implementation of RTW interventions, in agreement with other literature reports (7, 18–21). The notable feature of the study is the ability of the conceptual framework (14) to identify barriers ahead of implementation. This confirms the special attention which needs to be paid when implementing this type of program, to avoid the repeated failures previously reported (7).
Implementation science
Implementation science has been the focus of many studies, to the point of leading to a certain confusion of definitions and theoretical frameworks (22, 23). Some authors have sought to bring these together in integrative frameworks and clarify the concepts used (9, 10, 22, 23). Despite the efficacy of implementation strategies adapted to identified barriers (11), it remains unknown which implementation interventions are most effective, in what context, with what mechanisms and means of administration (23).
Implementation strategies adapted to identified barriers
The present results have two important consequences for implementation. The existence of barriers in each category of agent suggests that implementation interventions limited to one particular category have little chance of success. Rather, an inter-sector strategy, associating healthcare, health insurance and the workplace, should be adopted. The existence of barriers at each level suggests that implementation interventions limited to one particular level (external context, organizations, or individuals) have less chance of success than a strategy aimed at changes at different levels. Given the number of barriers identified, they need ranking in terms of importance and ease of change. A pragmatic approach would be to consider first of all barriers common to the different categories of agent.
A change in the law to overcome medical and health-data confidentiality may not be realistic. However, these barriers can be overcome by reminding those concerned that the French law allows the sharing of information for multidisciplinary patient management, in the interest and with the consent of the patient. Thus this barrier is to be got around not by legislation so much as by changing representations and through professional collaboration. A strategy to deal with the complexity of the legal framework could be founded on ongoing training with information supports shared by the different types of agent, including the low-back pain sufferers themselves.
The perceived legal risk could be changed by better knowledge and perception of the benefits of the Sherbrooke model. Implementation interventions should thus include well thought-out information on benefits according to category of agent. One strategy would be to develop the Sherbrooke model progressively on a limited basis in a few volunteer firms, so as to test out implementation in a favorable environment, thus visibly demonstrating its feasibility and benefits to other agents. Lack of human and financial resources is obviously a common barrier needing to be overcome; a solution would consist of training and financing resource persons such as “case managers” or “RTW coordinators”. These agents certainly constitute one of the active ingredients of the Sherbrooke model (3). Their skills have been described in the literature (24) and are presently lacking in the French health system on a large scale.
At the individual level, common barriers were personal overwork (lack of time), lack of trust between other agents, and individualistic professional practices. The first of these could be overcome by case managers taking some of the workload from the other agents. Mistrust can also be overcome by a communication campaign targeting the shared benefits of the Sherbrooke model and visible pilots demonstrating its benefit. There is no easy solution to the problem of individualistic professional practices, but it may be hoped that the above solutions will have some impact here too.
Barriers specific to healthcare professionals (over-medicalization and over-functional approach) require improved link-up between first-line care and rehabilitation and occupational medicine. This could be achieved by in-service medical training and health networks. Barriers specific to the workplace require dialog on RTW for employees with health problems; this could involve interventions specifically targeting certain occupational sectors.
Strong and weak points of the study
The multiple case study design (15) allowed a complex notion to be dealt with in a real life setting. Several measures were taken to ensure the validity of the results (16). Drawing up an eclectic conceptual framework allowed barriers and facilitators to be identified in the various agents and at the various levels. Triangulation of data collection and investigators at the time of analysis was performed. The investigators’ interpretation of the results was fed back to the participants. Use of a single database and software package ensured process traceability. Analytical categories were saturated at the end of the analysis. A log-book kept during data collection enabled results to be contextualized and investigator subjectivity to be included. For all these reasons, the results can be presumed to have good construct validity and reliability.
The study also involved several limitations. The maximum number of study cases was originally chosen for logistic reasons. Although including extra cases might have identified other results, the saturation observed at end of analysis suggests otherwise. Workplace sampling led to over-representation of the healthcare sector. However, input from two occupational health services (15 OP) allowed experience to be included from a broad economic sector. Involving GP in the study was very difficult – which is in itself an interesting finding, reflecting the difficulty of getting these agents to participate in this kind of project. Only one disabled worker and two co-workers could be interviewed in the participating workplaces. This limitation is partially compensated by the accounts of injured workers in the voice of other respondents (social workers, occupational physicians).
Generalizability of the results
The barriers and facilitators identified in this study, although identified in the French context, are believed to apply in other countries. The occupational health and safety legislation presents common features in many European countries. Issues identified within the (occupational) health system, in the workplace and within the insurance system have been reported in several other countries (18–21, 25, 26).
Future research
The next stages will consist of discussing the implementation strategy drawn up here between the stakeholders and implementation scientists, applying this strategy and monitoring the process and results of implementation. The effects of the Sherbrooke model should not be assessed until implementation is such as to guarantee its lasting and routine use. Only then can effectiveness at a population level be established for this new intervention to be integrated into healthcare provisions, in contrast to an experimental trial in a controlled context.
Concluding remarks
Facilitating RTW for low-back pain sufferers requires several barriers to be overcome among healthcare professionals, workplaces and the health insurance system. Implementing a RTW intervention should be considered as a process at high risk of failure, requiring a strategy painstakingly adapted to the barriers and facilitators identified in the field. Such strategies are presently drawn up in a more pragmatic than scientific manner. Implementation process assessment is essential to guarantee that the implemented intervention is sustainable before attempting to assess its effectiveness.



