Employees experiencing workplace bullying are more likely to report both concurrent and subsequent sleep problems (1–3), as well as a higher use of sleep inducing drugs and sedatives compared to non-bullied employees (4). Workplace bullying may affect both men and women. It is often assessed by the so called “self-labelling method”, which entails asking the respondents directly whether they think they have been subjected to bullying or not, generally after having been presented to a definition of the term bullying (5). Depending on the assessment method, the prevalence of workplace bullying varies from approximately 2–14% (6). A recent study showed that workplace bullying may pose a threat to mental health five years after it occurs for men (7). The authors also found a reverse relationship between mental health symptoms and bullying after five years for men. This may indicate the existence of a vicious circle where bullying and mental health symptoms reinforce the negative effects of each other. Accordingly, bullying may lead to mental health symptoms, which in turn may worsen the situation for the target or the perception of the work situation. Provided that sufficient rest and recovery follow stressful episodes (or serve to divide longer stress episodes into shorter periods), it is generally presumed that humans may endure quite severe stress without developing poor health or long lasting mental health problems (8). However, rest and recovery is not necessarily equal to physical inactivity. For example, a recent study showed that leisure-time physical activity (LTPA), relaxation and detachment after work all reduced the need for recovery (9). Indeed, physical activity (eg, various sports activities) may have a recreational value as well as a general fitness enhancing effect that increases an individual’s resilience. It seems plausible that being physically active during leisure time may serve to reduce the hazardous effect of bullying on sleep.
The aims of this study were to examine prospectively whether (i) bullying increases the risk of sleep problems, and (ii) the association between bullying and sleep problems is moderated by LTPA (figure 1). To our knowledge, no studies seem to have evaluated the moderating role of LTPA in relation to the association between workplace bullying and sleep problems. Thus the research questions of the present study are: (i) Does exposure to bullying increase the risk of developing sleep problems? (ii) Does high LTPA buffer the potential effect of workplace bullying on risk of sleep problems?
Figure 1
Model of the association of the moderation role of leisure-time physical activity in the association between workplace bullying and sleep problems.
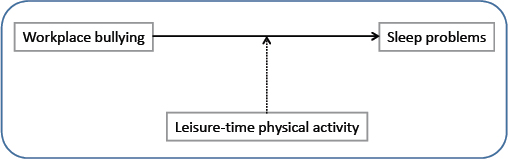
We expect that, among individuals with high LTPA levels, the association between bullying and sleep problems will be weaker compared to individuals who are less physical active during leisure-time.
Methods
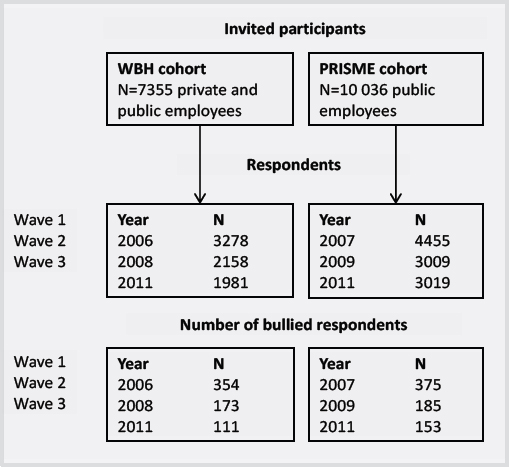
The study population (figure 2) consists of two cohorts. The Workplace Bullying and Harassment (WBH) cohort consisted of public and private employees [N=3278 (2006) (2) and new respondents in 2008, N=595]. The Psychosocial Risk Factors for Stress and Mental Disease (PRISME) cohort consisted of civil servants (N=4455 in 2007) (10, 11).
The WBH cohort consisted of public (63%) and private employees (37%). The cohort was established with the aim to study workplace bullying and health effects. From September–November 2006, 7355 employees were invited and 45.7% responded to a baseline questionnaire (67% women). The second wave was performed in September–November 2008 [for more details see (2)] and 2158 of those who were invited at baseline and new employees from 2006–2008 responded to the questionnaire (response rate at follow-up 62%). Respondents were excluded if they did not respond to the question on bullying at wave 1 and wave 2.
The PRISME cohort consisted of civil servants employed in the central region of Denmark and was established with the aim of studying mechanisms linking psychosocial factors at work with stress, burnout, and depression. From January–March 2007, 10 036 employees were invited and 44.7% responded to a baseline questionnaire (78% women) [for more details see (12)]. A total of 4455 respondents were included from wave 1. The second wave was performed in January–March in 2009, a total of 3009 responded (71%).
Wave 3 (13) was conducted in 2011 among all invited from the previous waves of both the PRISME and the WBH cohorts. Of those who were invited, 5000 responded to items in the questionnaire (response rate 67%).
We combined the two cohorts and the three waves into a panel study and established 2-year follow-up courses from wave 1 to 2 (course 1) and from wave 2 and 3 (course 2) (figure 2). We use T1 for baseline (ie, wave 1 in course 1 and wave 2 in course 2) and T2 for follow-up (ie, wave 2 in course 1 and wave 3 in course 2). In the combined data, we had 11 813 2-year courses of not bullied respondents at baseline, where 6904 participated in 2006/2007–2008/2009 (course 1) and 4909 participated in 2008/2009–2011 (course 2). In courses 1 and 2, we had 729 and 358 bullied, respectively, totaling 1087 2-year courses among bullied respondents (figure 2).
Measures
Bullying
The determination and classification of targets to bullying were based on one question. To calibrate the responses, a definition of bullying was presented before the questions: “Bullying takes place when one or more persons are exposed to unpleasant or negative behavior at work, repeatedly over a longer period of time, which it is difficult to defend oneself against”. The question that followed read “Have you been subjected to bullying at work within the past 6 months?” with responses on a 5-step scale: 1=never, 2=now and then, 3=monthly, 4=weekly, 5=daily. The reference group comprised respondents who were not bullied and without missing data in the item.
Sleep problems
Sleep problems during the past four weeks were assessed with six items from a modified version of the Karolinska Sleep Questionnaire (KSQ) (14). Disturbed sleep and the items on awakening problems have previously been used by the inventors of the instrument (15) and in previous research (16). Disturbed sleep reflects lack of sleep continuity and awakening problems illustrate feelings of unsatisfactory awakening and being insufficiently restored (17). In both cohorts and across all three waves, the disturbed sleep score (range 1–5) was calculated as the mean score of four items: (i) “How often was your sleep poor and disturbed?”, (ii) “How often did you have problems falling asleep?”, (iii) “How often did you wake up too early and could not fall asleep again?”, and (iv) “How often did you wake up several times and were not able to fall asleep again?”. Awakening problems in the WBH cohort was assessed with one item: (v) “How often did you have difficulties waking up?” and lack of restful sleep with one item: (vi) “How often did you get enough sleep?”. In waves 1 and 2 in WBH cohort, responses were on a 5-point Likert scale ranging from 1=at no time, 2=some of the time, 3=a part of the time, 4=a large part of the time, and 5=all the time. Awakening problems in the PRISME cohort and in the third wave were measured using one item: (v) “How often did you have difficulties waking up?” and lack of restful sleep with one item (vi) “How often didn’t you feel rested when you woke up?”. In waves 1 and 2 in the PRISME cohort and in wave 3 of both cohorts, all the items were responded to on a 5-point Likert scale ranging from 1=never, 2=seldom, 3=occasionally, 4=most of the time, and 5=all the time. High scores represent poorer sleep. A correlation analysis showed poor correlations between disturbed sleep and items of awakening problems and lack of restful sleep (Pearson’s correlations <0.4). As the different items reflect different types of impairment of sleep, we decided to analyze disturbed sleep, awakening problems and lack of restful sleep separately. However, as different individuals may perceive different ways of impaired sleep, we also included an overall 8-item sleep problem scale. An overall sleep problems score was established as a mean score for each cohort and wave based on the six items in the disturbed sleep scale as well as the items on awakening problems and lack of restful sleep. The Cronbachs α’s were >0.7 for the scales on overall sleep problems for both cohorts and waves.
Leisure-time physical activity
The participants were asked how many hours per week they were physically active during their leisure-time. The response categories were: 1=<2 hours/week; 2=2–4 hours/week of light physical activity, 3=>4 hours/week light physical activity or 2–4 hours/week intense physical activity; and 4=>4 hours/week intense physical activity. The validity of items on physical activity was validated to a metabolic equivalent (MET) activity scale with a correlation of 0.74 by Aadahl & Jorgensen in 2003 (18).
Covariates
Information on age, gender, and body mass index (BMI) (kg/m2) based on self-reported weight and height, were obtained at baseline. We adjusted for age, gender, BMI, alcohol (drinks per week) and smoking at baseline since previous studies have shown differences in sleep patterns among men and women, with age, BMI and with alcohol intake (19–21). We also adjusted for working time, as working at night might affect sleep, education beyond primary and high school (three groups: <3 years; 3–4 years; >4 years) as used before in a study of workplace bullying, and T1-sleep problems (1, 3). We identified respondents with depression estimated in the PRISME cohort from Schedules for Clinical Assessment in Neuropsychiatry (SCAN) interviews (12). In the WBH cohort, we identified respondents with depression using the Major Depression Inventory (MDI) to assess symptoms of depression during the past two weeks with an algorithm that equals the ICD-10 categories of “moderate” to “severe” depression. The MDI includes 12 questions measured on a scale ranging from 0–5 (symptom present all the time) (22). According to the ICD-10 definition scoring, >19 was classified as having depression.
Statistical analysis
All statistical analyses were performed on the data set with and without imputed data on all variables. We used multiple imputation in STATA 14.0 (IBM Corp, Armonk, NY, USA) for imputing data on missing values on workplace bullying, sleep variables, LTPA, as well as covariates using multiple imputations of missing data on covariates missing at random as described in Sterne et al 2009 (23). Since data was collected in three waves, a participant could have imputed data in two waves. The imputation procedure increased the number of eligible 2-year courses from 11 802 to 15 095. We imputed data for missing values on responses to: workplace bullying (N=2206); sleep quality (N=4256); awakening problems (N=4238); restful sleep (N=4232); disturbed sleep (N=4211); and LTPA (N=1893). With respect to missing values in covariates, we imputed data for missing values on smoking (N=1861), alcohol (N=2535), working hours (N=4968), BMI (N=1966), and education (N=1882). We had no missing values in gender, age, or cohort.
We analyzed the association between T1-workplace bullying (T1-WB) and T2-sleep (research question 1/model 1) using multilevel mixed-effect linear regression models to examine associations between workplace bullying and sleep problems. In models 2 and 3, we adjusted for T1-sleep problems, gender (men, women), age (continuous), T1-BMI continuous), T1-smoking (never smoker, former smoker, and current smoker) T1-alcohol intake (continuous drinks per week), T1-working time (three levels: day and evening work; mixed shifts; fixed night work), T1-education (three levels: ≤2 years of education; 3–4 years of education; ≥5 years of education), cohort (two levels WBH and PRISME). Finally we excluded depressed respondents at T1 in model 3. Sensitivity analyses were conducted stratified by cohorts (levels WBH and PRISME) and courses 1 and 2.
We estimated the moderating effect of T1-LTPA (continuous) on T2-sleep problems among bullied respondents in multilevel mixed-effect linear regression models testing for multiplicative interaction (ie, T1-WB×T1-LTPA/ research question 2). In models 2 and 3, we adjusted for the same variables as mentioned above and finally, in model 3, we excluded depressed respondents at T1. All analyses used a random effects model to account for most participants providing more than one set of observations.
Lastly, we tested four subgroups based on T1-and T2-WB with T2-sleep problems to investigate across time developments (supplementary analyses for research question 1). For these analyses the respondents were classified as bullied if they answered ≥2. STATA 14.0 was used for the statistical analyses. P-values <0.05 were considered statistically significant.
Results
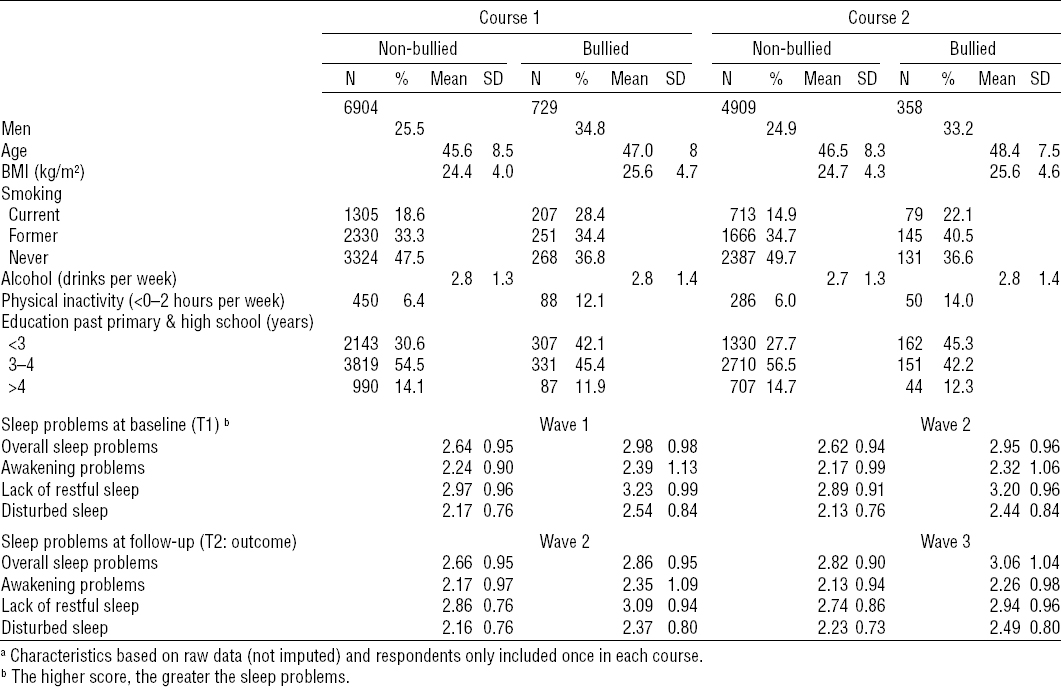
Table 1 describes the characteristics of the respondents in the two first waves of bullied and non-bullied respondents. In total, we had 1087 bullied respondents and 11 802 non-bullied respondents in all. The mean age of the non-bullied respondents were 45.6 years [standard deviation (SD) 8.5] in the first course, and the bullied respondents were approximately one year older. Bullied respondent had a higher T1-BMI than non-bullied respondents (25.6 versus 24.4 kg/m2) and the same pattern was observed at T2. Bullied respondents also reported more T1-current smokers. More bullied respondents had <3 years of education beyond primary and high school. Mean scores (SD) on overall sleep problems, awakening problems, lack of restful sleep and disturbed sleep at T1 and T2 among bullied and non-bullied in the two courses are also presented in table 1. Bullied respondents scored in general higher on sleep problems.
Table 1
Characteristics of the bullied and non-bullied respondents in course 1 and 2. a [BMI=body mass index; SD=standard deviation.]
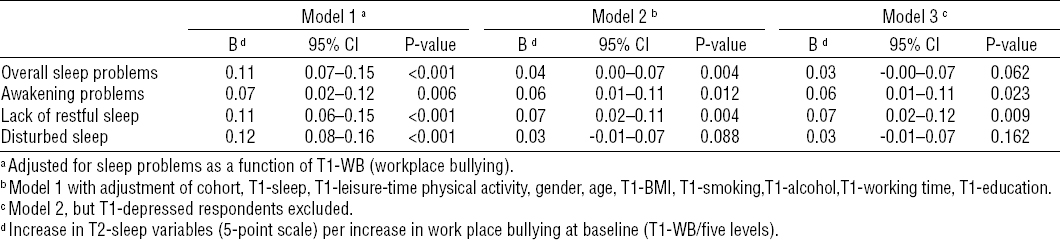
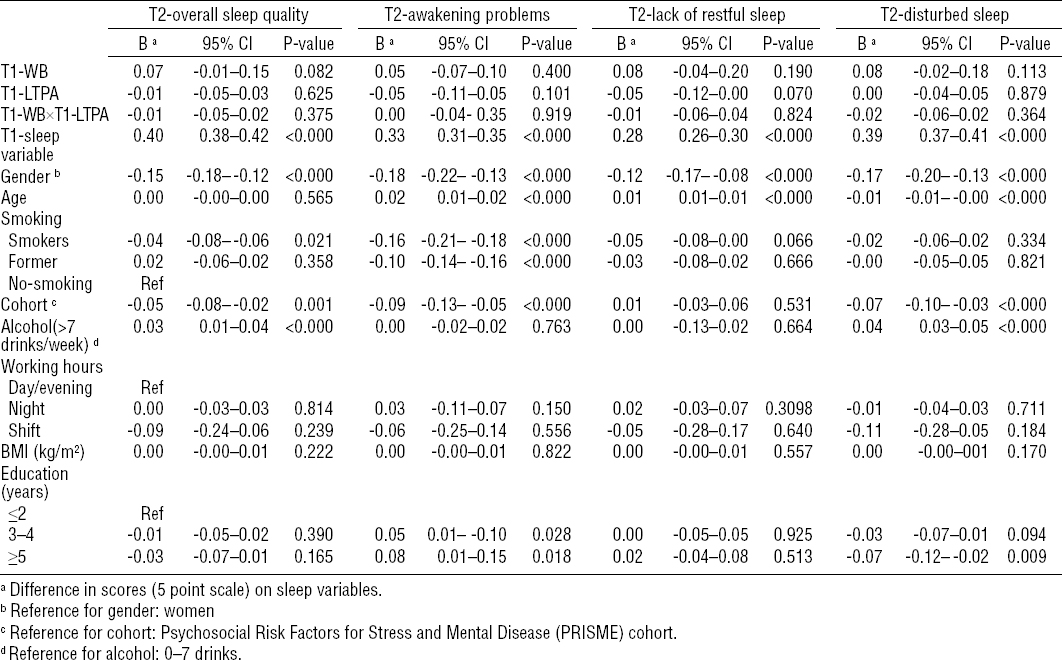
T1-WB was associated with overall sleep problems, awakening problems, lack of restful sleep, and disturbed sleep at T2 (model 1). When adjusting for the sleep variables at T1, gender, age, physical activity, smoking, alcohol, working time, and education at T1 as well as cohort, overall sleep problems (B=0.04, 95% CI 0.00–0.07), awakening problems (B=0.06, 95% CI 0.01–0.11), and lack of restful sleep (B=0.07, 95% CI 0.02–0.11) remained significant (table 2) but not disturbed sleep. When excluding T1-depressed respondents, the effect stayed significant with respect to awakening problems and lack of restful sleep.
Table 2
Difference in sleep problems at follow-up among 629 bullied participants at baseline compared to 8057 non-bullied participants.
The results of the moderation analyses (research question 2) are presented in table 3. T1-sleep variables had a significant influence on the association between workplace bullying and T2-sleep variables. Further, gender, T1-smoking, T1-alcohol and education affected the models. LTPA did not moderate the association between workplace bullying (T1) and sleep problems (T2).
Table 3
Difference in sleep problems at follow-up and being bullied at baseline stratified by physical activity. [T1-LTPA=leisure-time physical activity at baseline; T1-WB=workplace bullying at baseline.]
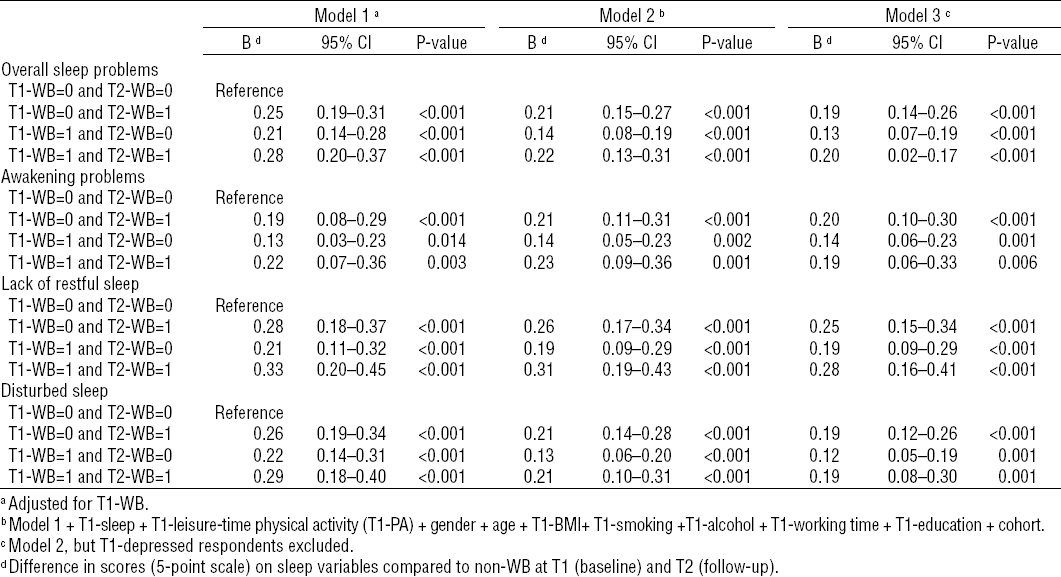
In table 4, we present supplementary analyses for research question 1 on sleep problems at T2 among four subgroups of workplace bullying at T1 and T2 [ie, WB-T1=0 and WB-T2=0 (reference)]; WB-T1=0 and WB-T2=1; WB-T1=1 and WB-T2=0; and WB-T1=1 and WB-T2=1. In model 1, the participants reported more sleep problems at T2 if bullied at T1, at T2 and at both T1 and T2. We found associations between T1-WB and T2-sleep problems. The effects stayed significant if bullied at T1, T2 and both T1 and T2 when adjusting for T1-sleep problems, T1-LTPA, gender, age, T1-BMI, T1-smoking, T1-alcohol, T1-working time, education, and cohort (model 2). Excluding respondents with depression at T1 did not change the result.
Table 4
Differences in sleep problems among participants bullied at baseline and/ or follow-up compared to non-bullied participants. [WB=workplace bullying; 96% CI=95% confidence interval.]
We did not have sufficient statistical power to test for moderation in the subgroup analyses. Results are presented on the data set with imputed data. Interested readers can obtain detailed results of the analysis on not imputed data and sensitivity analyses on request from the first author.
Discussion
The main findings in the present study among occupationally active Danish men and women were that workplace bullying was associated with awakening problems, lack of restful sleep, but not with disturbed sleep and overall sleep problems two years later. In addition, we found no indication that LTPA at baseline moderated these associations. Thus, our research question that high LTPA would reduce the hazardous effect of bullying on sleep did not receive support.
As to our first research question, and in line with previous longitudinal studies on workplace bullying and sleep problems (2, 3), we found evidence to support that exposure to workplace bullying increases the risk for sleep problems. In Lallukka et al’s prospective study (3), excluding respondents with mental health problems and adjusting for sleep problems at baseline resulted in attenuation of the observed association between bullying and sleep problems. We had similar findings with adjustment of T1-sleep problems and excluding respondents with depression. Hence our results supported Lallukka et al’s findings (3). We also investigated across time developments and observed that bullied respondents at T1 had overall sleep problems, awakening problems, lack of restful sleep, and disturbed sleep at T2, irrespective of whether workplace bullying was reported at T2 (table 4). Whether an increase of 0.04 to 0.07 more sleep problems with an increase in frequency of bullying constitute clinical relevance is at this point difficult to assess. However, the results indicated that workplace bullying has an impact on the respondents’ perceived sleep quality. We studied associations in the working populations and do not expect to find severely poor sleepers.
Hence, in relation to our second research question we did not find supportive evidence. As we did not find support for such a buffering effect, this may indicate that being physically active does not prevent bullying from having an impact on sleep. Results from other empirical studies suggest that some victims of bullying at work may suffer from post-traumatic stress disorder (PTSD) symptoms (24). PTSD include symptoms of increased arousal such as difficulty falling or staying asleep and according to the ICD-10 classification of the disease, the symptoms must have lasted ≥1 month, causing significant impairment in functioning in various spheres of the victims’ lives (25). Although, it is a matter of debate to what extent the diagnostic characteristics of PTSD are present among bullied victims (24), our results show that many of the bullied participants exhibited symptoms of increased arousal such as difficulty falling and/or staying asleep. Since these sleep symptoms were lasting and that sleep is central for restitution, it can be concluded that the complaints are severe enough to be taken seriously.
The association between workplace bullying and sleep problems showed that the effect were higher among those who were bullied at T2 independently of bullying at T1, which may indicate that being bullied during the past 6–12 months was associated with sleep problems. If bullied at T1 and not at T2, the effects tend to be lower than being bullied at T2. The results may indicate that discontinuance of workplace bullying tend to be associated with slightly better sleep. According to Einarsen & Nielsen (7), a bullying episode may last up to two years. Hence a 2-year follow-up period may blur the results.
Strengths and limitations
The study comprised two large cohorts including many different workplaces from both private and public sectors. This increases the external validity as it allows us to observe the prospective relationships across different settings and occupations.
We used the self-labelling method to assess workplace bullying, which may have affected the reports of the outcome variables. The self-labelling method does not provide information on the nature and content of workplace bullying (26). Furthermore, items regarding workplace bullying may be sensitive to personality (27), eg, bullied persons with high scores on neuroticism might interpret acts that they are exposed to as negative and threatening in cases where others would not. Also scoring of sleep problems may be sensitive to personality (28), which may result in unadjusted confounding. Another limitation was that the response rates were relatively low in the two cohorts. Low participation in population-based follow-up studies addressing psychosocial risk factors may cause a biased estimation of the occurrence of depression (29). However, in the PRISME study, very little indication of biased risk estimates due to low participation was found at baseline (10). A dropout analysis showed that more bullied respondents refrained from responding to the questionnaire at follow-up. Hence we may underestimate the effects on sleep problems of workplace bullying.
In conclusion, results showed that workplace bullying is related to development of T2-sleep problems but this association seems not to be modified by LTPA.