Low-back pain (LBP) is both a common and recurrent condition, for which estimates of recurrence at one year range from 24–80% (1). In France, over a one year period more than half the population reported LBP (2), and it is the first condition that contributes to disability (3). Preventing work disability due to LBP has been acknowledged as a public and occupational health priority in many countries. Given the prevalence of LBP, it has been argued that a focus on secondary prevention might be worthwhile, aiming at reducing recurrence of LBP episodes and/or at reducing chronic pain and work disability due to LBP (4, 5).
In contrast to the available evidence about LBP prognosis (6), screening instruments (7, 8), interventions at the chronic phase (9), work-directed (10) and workplace-based interventions (11) for disabled workers, evidence is remarkably scarce about effective strategies to prevent LBP recurrence. A review of exercises for the prevention of LBP recurrence (12) identified only four studies evaluating so-called post-treatment interventions, delivered after the resolution of an LBP episode in order to prevent new episodes. Based on two studies, there was very low quality evidence that post-treatment exercises could reduce the number of days on sick leave at mid-term follow-up (13, 14). This positive effect was lacking at long-term follow-up (13), and new trials were deemed necessary to figure out which strategies could prevent LBP recurrence and related work disability in the long term (12).
Healthcare workers are particularly exposed to LBP biomechanical risk factors such as bending and manual handling of loads and patients (15, 16). In France, nurse auxiliaries are the first occupational category exposed to manual handling, with an estimate of 169 000 workers exposed (17). As a consequence, the healthcare sector is one of the most badly affected by LBP. The main goal of the PRESLO study (French acronym for “secondary prevention of LBP”) was to evaluate the long-term effectiveness of a secondary prevention program based on education and exercise therapy to prevent LBP recurrence and related work disability among hospital workers. We wanted to test the hypothesis that a light exercise program, initiated in the workplace and continued at home, is effective in the long-term to reduce LBP recurrence episodes (and thus sick leaves related to LBP) among workers with a previous history of LBP compared to a control group with usual care.
Methods
Study design
A 2-arm single blinded randomized controlled study was conducted among healthcare workers recruited from ten hospitals of a large public consortium employing 16 000 workers (Hospices Civils de Lyon) in Lyon, France, from October 2008 to July 2011. The participants were randomly allocated to the intervention or control groups. The relevant authorities (Ethics Committee, Directorate-General for Health and Consumers, National Commission for Data Protection and Liberties – CNIL France) approved the study, which was authorized by the direction of the Hospices Civils de Lyon, and the Committees for Health, Safety and Working Conditions (CHSCT) of each participating hospital. The study was registered in ClinicalTrials.gov (NCT00782925) and its protocol has been published elsewhere (18).
Recruitment and flow of participants
Participants were recruited by their occupational physician (OP), either during their annual follow-up visit or on their own request following communication campaigns that were regularly carried out in the Hospices Civils de Lyon (electronic newsletters and other hospital newspapers).
The inclusion criteria were presenting, over the previous three years, ≥1 episode(s) of LBP of <3 months’ duration, with or without sick leave (LBP, lumbosciatica or acute or sub-acute cruralgia were considered). The exclusion criteria were previous history of back surgery (for spine fractures, discal hernia in two or more locations, lumbar or lumbosacral arthrodesis in three or more locations), radiculalgia with sequelary motor deficiencies or pure radiculalgia, chronic LBP for >3 months, current episode of LBP, psychiatric and/or behavioral disorders, unstable cardiac pathology, insufficient mastery of the French language, and pregnancy.
Randomization and blinding
Following the inclusion visit, participants were randomly assigned in permuted blocks of four, stratified by participating hospitals. The randomization lists were computed by an independent service operating outside the workplace using SAS® statistical analysis software (version 9.1, SAS Institute Inc, Cary, NC, USA). Each participant was informed by mail of his assignment and, where appropriate, the timetable for the program sessions was included. Participants were carefully instructed to conceal their allocation from the OP who performed their 1- and 2-year follow-up evaluation. The OP had no contact with the physiotherapists who carried out the intervention and thus remained blinded to the allocation of the participants during the intervention and at 1- and 2-year follow-up visits. For obvious reasons, the participants and the program providers (physiotherapists) could not be blinded. Participants were informed prior to the study that people allocated to the control group would receive the program after the trial if it was proven effective.
Intervention
The exercise therapy program comprised three steps (18). First, a 2-hour education session was delivered to the participants about LBP, pain pathways, fear-avoidance beliefs and coping. Key messages focused on pain management, staying active and adaptive coping during LBP episodes. Second, coaching 8–10 participants, one physiotherapist delivered five weekly 90-minute training sessions. The sessions were based in the workplace, and considered as working time. Each exercise session was composed of a 15-minute warm-up with rhythmic exercises, followed by 60 minutes of stretching and mobilizing the spine (including relaxation of the lumbar spine and stretching of the hamstrings, gluteals, quadriceps, psoas and adductors, as well as pelvic tilt awareness exercises) and finally, 15 minutes involving respiratory and postural work. The last step of the program was home-based with a booklet for self-managed home exercising and the French version of the Back Book (19). The participants were instructed to perform the exercises at home daily for approximately ten minutes. Control group members did not benefit from specific treatment of LBP aside from their usual care.
Outcomes
LBP recurrence
The OP measured LBP recurrence outcomes among participants at two years follow-up after the completion of the training sessions, with an intermediate data collection point at one year. The primary outcome was the percentage of participants with ≥1 recurrence of LBP with sick leave. Other outcomes were the average time to recurrence of LBP, the percentage of participants with sick leave related to chronic LBP (pain for >3 months), the participant’s compliance with the program, and their satisfaction. All other outcomes were measured by physiotherapists at 18-month follow-up after completion of the training sessions.
Psychological outcomes
Pain was assessed using the Saint-Antoine pain questionnaire (QDSA) (20) and visual analog scale (VAS). Anxiety and depression were measured with the hospital anxiety and depression (HAD) questionnaire (21). Coping strategies and fear-avoidance were measured with the French versions of the coping strategy questionnaire (CSQ) (22) and fear avoidance beliefs questionnaire (FABQ) (23). Health related quality of life was evaluated with the 12-item short form (SF-12) questionnaire (24).
Functional and physical outcomes
Functional disability was assessed by the French version of the Quebec back pain disability scale (QBPDS) (25). Lumbar flexibility was tested using the Schöber Mac Rae test. Pelvic flexibility was tested by the finger-to-ground distance. Muscle endurance was tested by the Shirado test (abdominal wall) and Sorensen test (lumbar extensors).
Healthcare utilization
We assessed for painkillers, visits to the general practitioner and/or specialists, imaging and outpatient physiotherapy.
Process evaluation
Attendance of the training sessions and observance of the home-based exercises at 6, 12 and 24 months were measured. The participant’s appreciation of the program was explored by a satisfaction questionnaire and by means of semi-structured interviews conducted one year after the completion of the training sessions with 21 participants identified by purposive sampling to represent a variety of jobs and hospitals. The interview guide was drawn to explore the workers’ representations of LBP and their initial expectations about and personal experience with the program. All interviews were transcribed to perform a qualitative thematic content analysis with Atlas.ti software, the results of which results have been published elsewhere (26).
Statistical analysis
Assuming a recurrence rate of LBP episodes of 45% after two years of follow-up, a population of 310 healthcare workers in each group was required to detect a 25% reduction in the risk of LBP recurrence with sick leave between the intervention and control groups with a power of 80% and alpha risk of 5%. With an estimation of 5% dropouts, 325 healthcare workers per group were needed.
Baseline characteristics of healthcare workers were compared between the study groups with the two-sample t-tests or Wilcoxon’s test, where appropriate, for quantitative data and the Pearson Chi2 test or Fisher’s exact for categorical data. The intervention effect on outcomes (LBP recurrence with and without sick leave or number of LBP recurrences over the 2-year follow-up) was assessed using logistic model or Poisson model adjusted for baseline characteristics (age, LBP history 3 years prior to inclusion, FABQ-W). A Wald statistic was used to test the significance of each coefficient in the model. The intervention effect was given as adjusted odds ratio (ORadj) or relative risk (RR) with its 95% confidence interval (95% CI). The time to first recurrence of LBP episode was compared between the study groups with Kaplan and Meier plot. The duration of sick leaves caused by LBP at 2-year follow-up was compared between the study groups with the Wilcoxon test. Additionally, a sensitivity analysis was performed for the main outcome by excluding workers with ≥2 previous sick leaves for LBP over the three years prior to inclusion.
Changes in physical and psychosocial outcomes were analyzed according to the difference-in-difference (DID) approach (27) by testing for the effects of group (intervention versus control), time (baseline versus 18 month) and interaction between group and time. We used the interaction between group and time and its 95% CI to estimate the mean of improvement in the intervention group compared with the control group. DID estimate captures the program effect in the intervention group, controlling for the effects of change over time in physical and psychosocial outcomes owing to factors other than the intervention itself. Compliance with the program and home-based exercises was compared between surveys at 6 and 24 months using the Wilcoxon signed rank test. Analyses were carried out in accordance with the principle of intention-to-treat. A per-protocol analysis was also performed, excluding all health workers who had failed to complete the intervention (<5 sessions). Statistical analyses were performed using SAS® 9.3 (SAS Institute Inc, Cary, NC, USA). P<0.05 was considered to be statistically significant.
Results
Study population
A total of 353 healthcare workers were enrolled between October 2008 and July 2011. Figure 1 presents the patient flow over the course of the study. After exclusion of 11 subjects, 342 participants were randomized to either the control or intervention group. Table 1 shows the baseline characteristics of the participants, without significant differences between groups. At 2-year follow-up, a total of 44 (13%) participants had dropped out. More than half of the dropouts were due to uncontrollable reasons (retirement, lay-off, and job transfer). Finally, a total of 298 participants (87%) had complete data for the analysis of the primary outcome.
Figure 1
Participant recruitment flowchart. *Lost to follow-up: retirement, job transfer, laid-off, no news; **Number of patients with data for the primary outcome (≥1 recurrence of low-back pain with sick leave over the 2-year period). [OP=occupational physician; PT=physiotherapist]
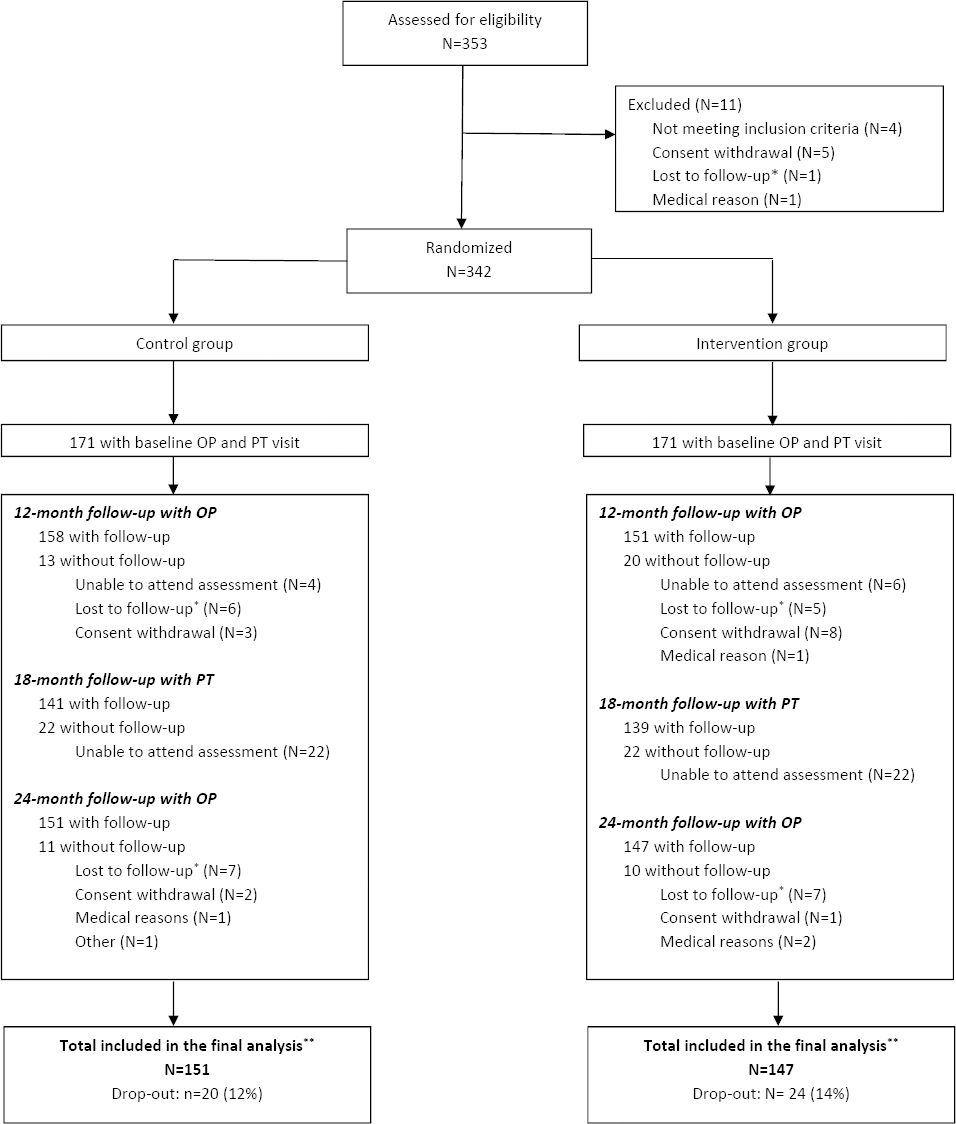
Table 1
Baseline characteristics of participants. [SD=standard deviation; Min-Max=minimum-maximum; VAS=visual analog scale; GP=general practitioner.]
| Low-back pain (LBP) history 3 years prior to inclusion | Intervention group (N=171) | Control group(N=171) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||||
| Mean | SD | N | % | Median | Min-Max | Mean | SD | N | % | Median | Min-Max | |
| Length of history of back pain (year) | 12.8 | 9.5 | 14.5 | 10.8 | ||||||||
| Sick leaves due to LBP episodes | ||||||||||||
| 0 | 82 | 48 | 96 | 56 | ||||||||
| 1 | 48 | 28 | 42 | 24 | ||||||||
| 2–4 | 37 | 22 | 30 | 18 | ||||||||
| ≥5 | 3 | 2 | 3 | 2 | ||||||||
| Duration of sick leave (days) | 15.0 | 34.5 | 16.0 | 33.2 | ||||||||
| Painful days per month | 6.2 | 5.1 | 6.5 | 5.6 | ||||||||
| VAS lumbar pain | 40 | 3–90 | 35 | 0–100 | ||||||||
| VAS radicular pain | 40 | 0–90 | 40 | 4–80 | ||||||||
| Medication use a | 165 | 97 | 166 | 97 | ||||||||
| GP or specialist visits | 157 | 92 | 164 | 96 | ||||||||
| Alternative treatments b | 151 | 88 | 147 | 86 | ||||||||
| Spine surgery | 5 | 3 | 5 | 3 | ||||||||
| Spondylolisthesis or scoliosis | 66 | 39 | 75 | 44 | ||||||||
| Load- or patient-handling training course | 74 | 43 | 72 | 42 | ||||||||
| Healthcare workers’ characteristics | ||||||||||||
| Male | 39 | 23 | 38 | 22 | ||||||||
| Age (year) | 47.1 | 8.5 | 47.3 | 8.5 | ||||||||
| Body mass index (kg/m2) | 24.4 | 3.7 | 24.3 | 4.5 | ||||||||
| Employment status | ||||||||||||
| Administrative | 20 | 12 | 26 | 15 | ||||||||
| Caregivers and medical | 93 | 54 | 93 | 54 | ||||||||
| Technical | 58 | 34 | 52 | 31 | ||||||||
| Years in ongoing employment status | 16.0 | 11 | 18.0 | 12 | ||||||||
| Current smoker | 28 | 16 | 31 | 18 | ||||||||
LBP recurrence outcomes
The recurrence rate of LBP (with or without sick leave) at 2-year follow-up and the rate of chronicization (sick leave due to LBP >3 months) are summarized in table 2. From baseline to 2-year follow-up, 35 workers (24%) in the intervention group and 31 workers (21%) in the control group had ≥1 recurrence of LBP with sick leave. After adjusting for baseline characteristics, no effect was observed between groups (OR 1.22, 95% CI 0.67–2.23, P=0.516). The mean duration of sick leaves due to LBP episodes was comparable between groups [25, standard deviation (SD) 50 days in the control group compared with 32 (SD 65) days in the intervention group, P=0.940]. Additionally, the time from inclusion to the first recurrence of LBP with sick leave was similar between groups [11.8 (SD 7.8) months and 13.4 (SD 8.2) months in the control and intervention group, respectively; P=0.511, log-rank test]. The reduction of recurrence of LBP episode without sick leave in the intervention group (N=106) as compared to the control group (N=123) almost reached statistical significance (P=0.053). Neither the per-protocol nor sensitivity analyses showed significant differences between groups.
Table 2
Recurrence of low-back pain (LBP) at 2-year follow-up. [ORadj=adjusted odds ratio; 95% CI=95% confidence interval.]
| Outcomes | Intervention group (N=147) | Control group (N=151) | |||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| N | % | N | % | ORadj | 95% CI | P-value | |
| Workers with LBP recurrence a | 121/133 | 91 | 129/138 | 93 | 0.68 | 0.27–1.69 b | 0.405 |
| Without sick leave c | 106/124 | 85 | 123/133 | 92 | 0.44 | 0.19–1.03 d | 0.053 |
| With sick leave | 35/147 | 24 | 31/151 | 21 | 1.22 | 0.67–2.22 e | 0.516 |
| LBP recurrence with sick leave | 0.71 | 0.49–1.04 f | 0.079 | ||||
| 0 | 112/147 | 76 | 120/151 | 79 | |||
| 1 | 27/147 | 18 | 13/151 | 9 | |||
| 2 | 3/147 | 2 | 8/151 | 5 | |||
| ≥3 | 5/147 | 3 | 10/151 | 6 | |||
| Workers with chronic evolution g | 6/147 | 4 | 3/147 | 2 | 3.56 | 0.70–18.2 h | 0.127 |
d Logistic model adjusted for HAD-A and work schedule (day/night/night and day) (N=257, 41 missing data).
e Logistic model adjusted for age, number of sick leaves three years prior to inclusion, length of ongoing back pain and fear-avoidance beliefs questionnaire score for occupational activity (FABQ-W) (N=294, 4 missing data).
Psychological outcomes
Participants from the intervention (N=139; 81%) and control (N=141; 82%) groups were assessed at baseline and 18 months for a range of parameters shown in table 3. All of the significant differences that were observed were in favor of the intervention. The intervention group showed a significant improvement for the FABQ-P score with a mean reduction of -3.6 (95% CI -4.8– -2.4) compared to -1.3 (95% CI -2.2– -0.3) in the control group (P<0.05).
Table 3
Evolution of physical and psychosocial variables in the intervention and control groups. [SD=standard deviation; QDSA-S=Saint-Antoine pain questionnaire sensory score; QDSA-A=Saint-Antoine pain questionnaire affective score; VAS=visual analog scale; FABQ-P=fear-avoidance beliefs questionnaire score for physical activity; FABQ-W=fear-avoidance beliefs questionnaire score for occupational activity; HAD-D=hospital anxiety and depression score for depression; HAD-A=hospital anxiety and depression score for anxiety; CSQ= coping strategy questionnaire; SF-12=short form questionnaire; FTF=finger-to-floor.]
| Intervention group (N=139) | Control group (N=141) | P-value a | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||||||
| Baseline | 18-month | Mean difference | 95% CI | Baseline | 18-month | Mean difference | 95% CI | ||||||
|
|
|
|
|
||||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||||||
| Questionnaires (score range from minimum-maximum) | |||||||||||||
| QDSA-S (0-36) | 8.5 | 6.1 | 7.3 | 6.3 | -1.4 | -2.7–-0.2 a | 8.5 | 5.7 | 8.1 | 6.4 | -0.2 | -1.2–0.8 | 0.4674 |
| QDSA-A (0-28) | 7.1 | 7.0 | 5.1 | 6.2 | -1.9 | -3.1–-0.6 b | 6.4 | 6 | 6.1 | 6.5 | -0.4 | -1.6–0.8 | 0.1323 |
| VAS lumbar pain | 41.1 | 22.7 | 36.2 | 21.0 | -8.5 | -16.7– -0.3 | 34.6 | 19.2 | 36.7 | 21 | 5.1 | -2.6–12.7 | 0.1417 |
| VAS radicular pain | 39.8 | 19.6 | 44.2 | 15.8 | -0.8 | -34.9–33.2 | 40.5 | 20.8 | 41.5 | 27 | -4.3 | -42.5–34.0 | 0.7002 |
| FABQ-P (0-24) | 12.1 | 5.7 | 8.5 | 5.8 | -3.6 | -4.8– -2.4 c | 12.8 | 5.6 | 11.7 | 6.1 | -1.3 | -2.2–-0.3 a | 0.0119 a |
| FABQ-W (0-42) | 16.4 | 9.7 | 14.4 | 10.2 | -1.9 | -3.1– -0.7 b | 17 | 9.2 | 15.7 | 9.9 | -1.1 | -2.4–0.3 | 0.7213 |
| Quebec score (0-100) | 24.7 | 14.0 | 19.8 | 15.8 | -5.0 | -7.5– -2.6 c | 26.6 | 15.3 | 24.4 | 16.4 | -2.8 | -5.4–-0.2 a | 0.3075 |
| CSQ-Distraction (5-20) | 11.4 | 3.7 | 12.5 | 3.8 | 1.3 | 0.4–2.1 a | 11.7 | 3.7 | 11.8 | 3.4 | -0.4 | -1.2–0.3 | 0.1410 |
| CSQ-Reinterpreting (4-16) | 6.5 | 2.7 | 7.2 | 3.0 | 0.8 | 0.1–1.4 a | 6.4 | 2.6 | 6.9 | 2.8 | 0.3 | -0.2–0.9 | 0.5850 |
| CSQ-Ignoring (5-20) | 12.1 | 3.6 | 12.1 | 3.3 | -0.3 | -1–0.5 | 11.9 | 3.2 | 11.7 | 3.2 | -0.2 | -0.9–0.6 | 0.8135 |
| CSQ-Catastrophizing (4-16) | 7 | 2.3 | 6.3 | 2.3 | -0.8 | -1.3– -0.3 c | 6.7 | 2.2 | 6.4 | 2 | -0.5 | -0.9–0.0 b | 0.4978 |
| CSQ-Praying (3-12) | 4.5 | 2.1 | 4.3 | 2.1 | -0.3 | -0.6–0.0 a | 4.6 | 2.3 | 4.3 | 2.1 | -0.3 | -0.7–0.1 | 0.7755 |
| SF-12 Physical (0-100) | 44.8 | 7.5 | 47.4 | 7.7 | 2.4 | 0.9–3.8 b | 44.3 | 7.3 | 45.1 | 8.3 | 0.8 | -0.5–2.0 | 0.1647 |
| SF-12 Mental (0-100) | 44.4 | 10.6 | 45.8 | 11.7 | 1.1 | -0.6–2.9 | 44.7 | 9.9 | 44 | 11 | -0.6 | -2.5–1.3 | 0.2595 |
| HAD-A (0-21) | 11.1 | 2.4 | 11.3 | 2.3 | -0.1 | -0.4–0.3 | 11.2 | 2.2 | 11.6 | 2.2 | 0.2 | -0.2–0.5 a | 0.7100 |
| HAD-D (0-21) | 9.1 | 1.7 | 9 | 1.8 | 0.2 | -0.2–0.6 | 8.5 | 5.7 | 8.1 | 6.4 | 0.4 | 0.0–0.7 | 0.3408 |
| Physical parameters | |||||||||||||
| FTF distance (cm) | 8.1 | 11.2 | 6.9 | 10.4 | -1.2 | -2.5–0.1 a | 10.4 | 11.8 | 8.7 | 10.6 | -1.7 | -3.2–-0.2 | 0.8236 |
| Schöber Mac Rae (cm) | 20 | 3 | 19.9 | 3.2 | -0.2 | -0.9–0.5 | 19.7 | 3.6 | 19.6 | 3.8 | -0.1 | -1.0–0.7 | 0.9324 |
| Shirado (s) | 119 | 92 | 127 | 84 | 9.7 | -5.8–25.2 | 117 | 92 | 108 | 82 | -10.2 | -24.6–4.2 | 0.2479 |
| Sorensen (s) | 92 | 53 | 105 | 58 | 13.9 | 3.3–24.5 b | 86 | 53 | 79 | 56 | -8.3 | -17.5–0.9 | 0.0276 a |
a Difference-in-difference (DID) analysis to compare the trend in intervention group from pre-implementation (baseline) and intervention period (18-month) with the trend in control group from pre-implementation (baseline) and intervention period (18-month). DID tests an intervention effect after controlling for temporal trend between periods.
Physical outcomes
For physical parameters, the Sorensen test was significantly improved after the intervention with a mean increase of 13.9 minutes (95% CI 3.3–24.5) in the intervention group versus -8.3 minutes (95% CI -17.5–0.9) in the control group (P<0.05).
Healthcare utilization
Significantly less workers in the intervention group had visited a GP (42% versus 57%, P=0.002) or specialist (18% versus 34%, P=0.011) at least once for their LBP at 2-year follow-up. The intervention group also reported significantly less physiotherapy visits (28% versus 50% with ≥1 visit; P<0.001) and imagery tests (15% versus 26%, P=0.038) for their LBP as compared to the control group. Fewer participants in the intervention group took pain killers (68% versus 77%, P=0.039) but no difference was observed for anti-inflammatory medication.
Process evaluation (attendance, observance, satisfaction)
Attendance indicators showed that 125 subjects (73%) participated in all training sessions in the intervention group, 16 (9%) missed one of the two sessions where absence was tolerated (session 3 or 4), 18 (11%) discontinued the program and 12 (7%) attended none of the sessions. Healthcare workers who discontinued the program attended three sessions on average (minimum–maximum: 1–5). In total, 141 (82%) participants in the intervention group were considered per-protocol. Observance of the home-based exercises was modest and decreased significantly over time as shown in table 4, both in terms of frequency and variety of exercises. The satisfaction survey at six months after the last training session showed that 92% of the workers who attended at ≥1 session were satisfied with the program and 83% were satisfied with its effects on their health status (response rate 81%, 128/159).
Table 4
Exercise training sessions observance rates over time. [SD=standard deviation; Q1-Q3=interquartile range between 1st and 3rd quartiles; Min-Max=minimum-maximum.]
| At 6 months (N=128) | At 12 months (N=123) | At 24 months (N=105) | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||||||||||||||
| Mean | SD | Median | Q1-Q3 | Min-Max | Na | % | Mean | SD | Median | Q1-Q3 | Min-Max | Na | % | Mean | SD | Median | Q1-Q3 | Min-Max | Na | % | |
| Trainings/week | 3 | 2 | 2 | 1–4 | 0–8 | 2 | 2 | 2 | 1–3 | 0–7 | 2 | 2 | 2 | 1–3 | 0–7 | ||||||
| Training duration/week (minutes) | 34 | 25 | 30 | 15–45 | 0–120 | 33 | 34 | 20 | 10–50 | 0–180 | 31 | 30 | 20 | 10–45 | 0–180 | ||||||
| Type of exercise | |||||||||||||||||||||
| Morning warming | 109 | 85 | 89 | 72 | 75 | 71 | |||||||||||||||
| Hamstrings stretching | 88 | 69 | 78 | 63 | 59 | 56 | |||||||||||||||
| Pyramidalis muscle stretching | 77 | 60 | 62 | 50 | 46 | 44 | |||||||||||||||
| Anterior chain stretching | 65 | 51 | 53 | 43 | 43 | 41 | |||||||||||||||
| Relaxing position | 110 | 86 | 83 | 67 | 75 | 71 | |||||||||||||||
The qualitative evaluation of the semi-structured interviews revealed that workplace location and worktime schedule of the training sessions were major facilitators of the participants’ attendance, as well as encouragement from other members in the group (26). The home-based part of the intervention was more problematic as several participants mentioned a lack of sufficient technical autonomy to perform the exercises on their own as well as insufficient social reinforcement to motivate them exercising in the long term. One theory limitation of the program was the overestimation of the observance of home-based exercises. The absence of a component to address biomechanical and/or psychosocial risk factors of LBP in the workplace was also questioned (26).
Discussion
The results of our study could not confirm our initial hypothesis that a brief workplace-based cognitive and exercise intervention, followed by a home-based exercise program, is effective in secondary prevention to reduce LBP recurrence with sick-leave among healthcare workers with a previous history of LBP. Three main lines of arguments may help understand the absence of positive effects for LBP recurrence outcomes.
First, the population included in the study differs from what was expected and presents several characteristics of heterogeneity. The mean number of painful days per month at baseline was surprisingly high in both groups (6.2 and 6.5 in the intervention and control group, respectively). The baseline levels of fear-avoidance beliefs, functional capacity, and pain intensity (table 3) were similar to those observed among subacute or chronic LBP patients in previous French studies (23, 28–32). Thus, the population of our study is likely to be a mix of pain-free workers (as expected) with other workers suffering from “highly recurrent” LBP. Reasons for this unexpected heterogeneity may pertain to the difficult issue of LBP case definition (33), and the pressure on the OP to include workers, maybe to the detriment of the strict application of inclusion/exclusion criteria. As a consequence of this heterogeneity, we may assume that the brief intervention was “too light” to be effective in a population that was more severe than expected. This assumption is corroborated by the poor observance of the home-based exercises, which weakens their potential effects (26), and by the comparison to other programs in secondary prevention of LBP, the duration and intensity of which were higher than in our brief intervention (12).
Second, the absence of a component in the intervention pertaining to workplace physical and psychosocial risk factors of LBP may partly explain its absence of effect on LBP recurrence, despite the advantage of the program being delivered in the workplace and during working hours.
Third, the more important use of healthcare in the control group may have contributed to lower LBP recurrence with sick leave in this group, thus masking the relative effect of the intervention.
Last, the expected number of participants could not be included due to an overestimation of the recurrence rate of LBP episodes with sick leave in the power calculation, resulting in the inability to confirm or reject our hypothesis from a strict statistical point of view.
However, some other positive results of the PRESLO program are worthwhile mentioning. A significant reduction of healthcare utilization was achieved by the intervention (medical and physiotherapist visits, imaging, pain killers), in line with a reduction in physical fear-avoidance beliefs. These results are congruent with a modest but significant gain in physical parameters (Sorensen test). In view of these convergent and positive results, we believe that the PRESLO program can be considered an effective intervention to correct fear-avoidance beliefs of workers with previous history of LBP, improve their muscle endurance, and reduce their healthcare utilization.
Strengths and limitations
The main limitations of our study pertain to the lack of statistical power resulting in an inability to conclude about the main outcome of LBP recurrence with sick-leave, the inclusion of more severe cases than expected, and program theory limitations about the home-based component of the intervention.
The main strengths of our study are its standards of methodological rigor and the adherence to the CONSORT checklist. As such, the positive results of the PRESLO program on secondary outcomes are reliable and likely to have important spin-offs.
Recommendations for future research
Based on our results, we can recommend a careful case definition of workers with previous history of LBP (33) and a better characterization of this subgroup (34) allowing a stepped secondary prevention similar to the primary care stratification developed in LBP (35–37). Another recommendation is to investigate the value of a workplace component to address the physical and psychosocial factors of LBP among workers still at work, as this component has proven its value in other LBP populations (10, 11). Specific attention should be paid to ensure the technical skills of the participants in the realization of their exercises. The logic model of future interventions should be carefully thought ahead (38) with a clear integration of mechanisms to improve participants’ motivation and observance (39–41).
Concluding remarks
It was not possible to assess the effectiveness of a light exercise program, initiated in the workplace and continued at home, in reducing LBP recurrence episodes in the long-term among healthcare workers. However, this program was effective in improving muscle endurance and reducing fear-avoidance beliefs and GP and physiotherapy visits as well as pain medication. Further studies are necessary to better characterize the subgroup of workers with highly recurrent LBP and their needs in order to develop effective interventions to reduce LBP recurrence and related sick-leave.



