Both overweight [body mass index (BMI) ≥25 kg/m2] and obesity (BMI ≥30 kg/m2) (1) are associated with a substantially increased risk of work disability (2–10). In 2016, more than 1.9 billion adults were overweight (1), and having a high BMI is currently ranked second for women and sixth for men in the hierarchy of leading risk factors (11). It has been suggested that high BMI may particularly increase work disability due to musculoskeletal disorders (8, 12, 13), cardiovascular diseases (8, 14) and mental disorders (13, 14), as well as injuries, diseases of the nervous system, and tumors (13).
Weight loss is difficult to achieve and even more difficult to retain over time (15), but increasing the level of physical activity may decrease the risk of future work disability among overweight individuals, irrespective of weight loss (16). To date, little empirical evidence is available to quantify this risk reduction. Increasing the level of physical activity is an integral part of treating obesity and preventing work disability (17), and some studies have suggested that high levels of physical activity may attenuate the health risks related to overweight and obesity (18, 19). In addition, overweight and obese individuals are more likely to become physically inactive than those of normal weight (20, 21), further increasing their risk of work disability. While physical activity has shown to be linked to a reduced risk of sickness absence, particularly due to musculoskeletal disorders (22), the potential contribution of physical inactivity to the overall risk of work disability among overweight people remains unclear.
In this study, we take advantage of recently developed modelling approaches to observational data for analyzing the direct and indirect effects of obesity and physical activity on the risk of work disability (23–25). The first, counterfactual mediation analysis, enables quantifying a realistic scenario regarding the probability of work disability, in which physical activity in overweight individuals is increased to the level observed among normal-weight individuals. The second approach (a pseudo-trial) uses repeat measurements to mimic a trial design, here applied to test the effect of an intervention of increasing physical activity among the inactive overweight individuals. The overall aim of this observational study was to assess the extent to which the risk of work disability among overweight people would be reduced if they adopted a physically more active lifestyle.
Methods
Study populations
Data were derived from two Finnish cohort studies (i): a population-based sample of Finnish working-age adults participating in the Health and Social Support (HeSSup) study (26) and (ii) the employees of ten towns and 21 public hospitals in the Finnish Public Sector (FPS) study (27). Ethical approval for the HeSSup study was obtained from the Turku University Central Hospital Ethics committee, and for the FPS from the Ethics committee of the Hospital District of Helsinki and Uusimaa.
From both cohorts, we included currently employed respondents who were not on long-term sick leave before the start of the follow-up and had responded to two repeated questionnaire surveys at Time 1 (T1) and Time 2 (T2). In the HeSSup study, the survey years were 1998 (T1) and 2003 (T2), and a total of 11 886 participants responded, for whom data on all study variables were available for 11 766. In the FPS, the survey years were 2000–2002 (T1) and 2004 (T2). In total, 27 825 responded, and full data were available for 27 008 participants. The follow-up for work disability (long-term sickness absence and disability pension) in both studies was from T2 until disability or old-age pension, death or end of sickness absence follow-up, whichever came first.
Overweight
BMI at T1 and T2 was calculated from self-reported height and weight. We dichotomized the participants into the overweight or obese (BMI≥25 kg/m2) and normal weight (BMI<25 kg/m2) (28). In sensitivity analyses, we included only the obese (BMI≥30 kg/m2).
Physical inactivity
Physical activity was retrieved from the T1 and T2 surveys using questions on average weekly hours of all kinds of physical activity or exercise during leisure time or commuting within the previous 12 months with varying intensity corresponding to walking, brisk walking, jogging, and running. The response categories were: <30 minutes, 1, 2–3, and >4 hours. Participants were categorized as being physically inactive if they reported physical activity corresponding to <30 minutes per week of brisk walking, jogging, or running; and active if they spent more time in physical activities. Physical activity level corresponding to merely walking (irrespective of the amount) was counted as inactivity (29).
In addition, we measured physical activity with metabolic equivalent task (MET) hours (continuous variable). MET hours were based on the same question regarding weekly physical activity. We used the following scales for calculations: <30 minutes = 15 minutes, 1 hour = 45 minutes, 2–3 hours = 2.5 hours, and >4 hours = 5 hours. The time spent on an activity at each intensity level in hours per week was multiplied by the average energy expenditure of each activity, and expressed in MET, as described earlier (30). Physical activities evaluated to correspond to walking, brisk walking, jogging, and running, were given MET values 3.5, 5, 8, and 11 MET, respectively. The median of MET hours was 4 (range 0–23) for people labelled as physically inactive, and 26–27 (range 4–138) for people labelled as active.
Work disability
We used two indicators to ascertain long-term work disability, ≥90 days sickness absence and disability pension, obtained from the registers of the Social Insurance Institution of Finland and the Finnish Centre for Pensions. The follow-up was from T2 until 31 December 2013 in HeSSup and from T2 until 31 December 2011 in the FPS.
Covariates
Age and sex were obtained from the employers’ registers. Socioeconomic status (SES) was defined using the self-reported vocational education level in HeSSup and the register-based occupational class in the FPS. High SES in HeSSup included those with university, polytechnic, or college-level education, and ‒ in FPS ‒ administrators, managers, experts, specialists, office workers, customer service workers, sales workers, and hospital nurses. Low SES included those with vocational school education, vocational courses, apprenticeship training, or no vocational education (HeSSup), and manual workers such as construction workers, manufacturing, and transportation workers (FPS). Health behaviors, measured at T1, included self-reported current smoking (yes/no) and self-reported average weekly units of alcohol consumption including beer, wine, and spirits/liquors (continuous variable).
Statistical analysis
We examined the baseline characteristic differences between overweight and normal-weight people, and the correlations between variables using X2-tests, t-tests, and hazard ratio (HR) with their 95% confidence intervals (CI), as appropriate for both cohorts separately.
Counterfactual mediation analysis. A prerequisite for mediation analysis is that exposure (overweight) and mediator (physical activity) are correlated, and both are also related to the outcome (work disability). Counterfactual analysis also contains several other assumptions. The assumption of no unmeasured confounding of the exposure–outcome relationship requires that the exposure temporally precedes the outcome. The assumption of no unmeasured confounding of the mediator–outcome relationship requires that the mediator temporally precedes the outcome. The assumption of no unmeasured exposure-mediator confounding requires that the exposure must precede the mediator. And finally, the covariates of mediator–outcome association must be independent from the exposure (31, 32). Thus, we defined exposure at T1, mediator at T2, and the follow-up for the outcome, as beginning after T2.
For counterfactual mediation analysis with survival data, we used the SAS macro presented by Valeri & VanderWeele (31, 32). In both cohorts, we examined the association between overweight and work disability, controlling for age, sex, SES, smoking, and alcohol consumption. We tested the mediator as a dichotomous variable (inactive/not inactive), and as continuous MET hours. The outcome was modelled using the Cox proportional hazard model, the binary mediator was modelled using logistic regression, and the continuous mediator using linear regression. We estimated the causal effects on the HR scale. Mediation was examined by separating these effects into controlled direct effect (CDE), natural direct effect (NDE), natural indirect effect (NIE), and total effect (TE).
The CDE refers to the HR for the association between overweight (exposure A) and work disability, by comparing the normal weight (A = 0) with the overweight (A = 1) when setting physical activity (mediator M) to a fixed level (M = m), ie, the effect of overweight is not mediated through physical activity:
CDE = Hazard(A=1, M=m)/Hazard(A=0, M=m)
The NDE refers to the HR for the association between overweight and work disability in a scenario in which the overweight individuals’ physical activity is at a level similar to that of the normal weight (MA=0):
NDE = Hazard(A=1, MA=0)/Hazard(A=0, MA=0)
The NIE refers to the excess risk of work disability among the overweight that is due to their lower physically activity:
NIE = Hazard(A=1, MA=1)/Hazard(A=1, MA=0)
In TE, both natural direct and indirect effects are taken into account to estimate the association between overweight and work disability:
TE = NDE × NIE
Dissecting the NIE of obesity on work disability risk allowed us to estimate the extent to which the excess risk of work disability among the overweight participants would be reduced if they adopted a lifestyle with physical activity of the same level as that of the normal-weight participants:
1/NIE= Hazard(A=1, MA=0)/Hazard(A=1, MA=1)
Analyzing observational data as a pseudo-trial. To minimize error in analyzing temporal order between overweight and physical activity, we conducted pseudo-trials mimicking non-randomized trials (24, 25). More specifically, we included overweight participants at T1 and T2 who were additionally physically inactive at T1. We compared the relative risk (HR) of work disability after T2 between participants who continued to be inactive at T2 to the risk of those who increased their level of physical activity at T2. When using continuous MET hours as the predictor variable, the cut-point for T1 physical inactivity was set at median value (21 MET hours).
Sensitivity analyses. To keep the study population similar to the general working population, we did not exclude participants with chronic disease at baseline (T1). However, incident disease between T1 and T2 is a major source of bias for analysis of change in BMI as many chronic conditions lead to weight loss and therefore a favorable change in weight may appear as harmful. To minimize this bias, we performed analyses after excluding participants who developed a chronic disease between T1 and T2 (ie, participants who reported a doctor-diagnosed illness in T2 but not in T1, N=3961 participants, 10% of study population). Information on doctor-diagnosed illness were retrieved from survey responses and covered the following illnesses: bronchial asthma, myocardial infarction, angina pectoris, cerebrovascular diseases, arthritis, sciatica, migraine, depression, and diabetes. Chronic disease is an intermediary variable for long-term sickness absence and disability pension, and thus adjustment for chronic conditions would introduce over adjustment bias (33). Moreover, to control for weight change between T1 and T2 among those were overweight in both measurements, we included only participants with ±5% change in BMI between the measurements.
The study-specific results were analyzed using SAS 9.4 (SAS Institute, Cary, NC, USA). We pooled the cohort-specific estimates in fixed effects meta-analysis using Stata 14 software. We examined the heterogeneity of the estimates using the I2 statistic.
Results
HeSSup had 1665 (14%) long-term sickness absence events (mean follow-up = 8.4 years, range 0.01–10.0), and 615 (5%) disability pension events (mean follow-up = 8.9 years, range 0.01–10.0). The FPS had 4328 (16%) long-term sickness absence events (mean follow-up = 6.1 years; range 0.01–7.6), and 1923 (7%) disability pension events (mean follow-up = 6.4 years, range 0.04–7.6).
Smoking was not associated with overweight in HeSSup, whereas smokers were more often overweight in FPS. All other associations were statistically significant (P<0.001) in both cohorts; male sex, older age, lower SES and physical inactivity were correlated with overweight (table 1.)
Table 1
Descriptive statistics of participants in Health and Social Support (HeSSup) and Finnish Public Sector (FPS) studies stratified by overweight at T1. Frequency (percentage), unless otherwise stated. [MET=metabolic equivalent task; SD=standard deviation; IQR=interquartile range].
Supplementary table S1 (www.sjweh.fi/show_abstract.php?abstract_id=3799) shows the associations between overweight at T1 and physical inactivity at T2 as predictors of incident sickness absence and disability pension during the follow-up after T2. In the unadjusted analyses, both overweight and physical inactivity were associated with an increased risk of long-term sickness absence and disability pension. As the hypothesized mediator (physical activity) correlated with both exposure (overweight) and outcome (sickness absence and disability pension), and the exposure also correlated with both outcomes, the prerequisites for mediation were fulfilled. The associations were robust to adjustment for sociodemographic and health behavior factors, except for physical activity and long-term sickness absence in HeSSup, where the association diluted after the adjustments.
Counterfactual mediation analysis
When allowing the exposure (overweight) × mediator (physical inactivity) interaction, the pooled adjusted HR for overweight compared to normal weight was 1.40 (95% CI 1.31–1.50) (ie, the CDE). In a scenario in which physical inactivity among overweight individuals was at the same level as that among normal-weight individuals (the NDE), the HR for overweight was similar: 1.40 (95% CI 1.31–1.48). However, we observed that overweight individuals were less physically active than those of normal weight (prevalence of physical inactivity 26–28/% in the former, and 14–17% in the latter group), and therefore modelled the risk of sickness absence among overweight individuals, which is due to them being less physically active than those of normal weight (ie, the NIE). The risk of long-term absence was 1.03 (95% CI 1.02–1.04) times higher among overweight individuals than among those of normal weight, solely because of the lower physical activity in the first group. Thus, the excess risk of long-term sickness absence would decrease by 3% if overweight individuals increased their physical activity level to that of normal-weight individuals. When both the direct effect of overweight on sickness absence risk and the indirect effect of overweight through lower physical activity were combined, the HR for the association between overweight and incident sickness absence was 1.43 (95% CI 1.35–1.53) (ie, TE). (figure 1, panel A.) The congruent results using continuous MET hours as the mediator are shown in figure 1, panel B.
Figure 1
Counterfactual mediation analysis of the association between overweight and long-term (≥90 days) sickness absence, with (a) binary variable physical inactivity and (b) continuous variable metabolic task hours as a mediator. Study-specific and pooled hazard ratios (HR) are adjusted for sex, age, socioeconomic status, smoking, and alcohol consumption. Controlled direct effect refers to the physical activity-adjusted association between overweight and sickness absence allowing an interaction between overweight and physical activity. Natural direct effect refers to the HR for the association between overweight and sickness absence in a scenario in which physical activity among overweight individuals is at a similar level to that among those of normal weight. Natural indirect effect refers to the excess risk of sickness absence among the overweight individuals that is due to their lower physically activity. In the total effect, both natural direct and indirect effects are considered to estimate the association between overweight and sickness absence. [FPS=Finnish Public Sector study; HeSSup=Health and Social Support study; HR=hazard ratio; 95% CI=95% confidence interval.]
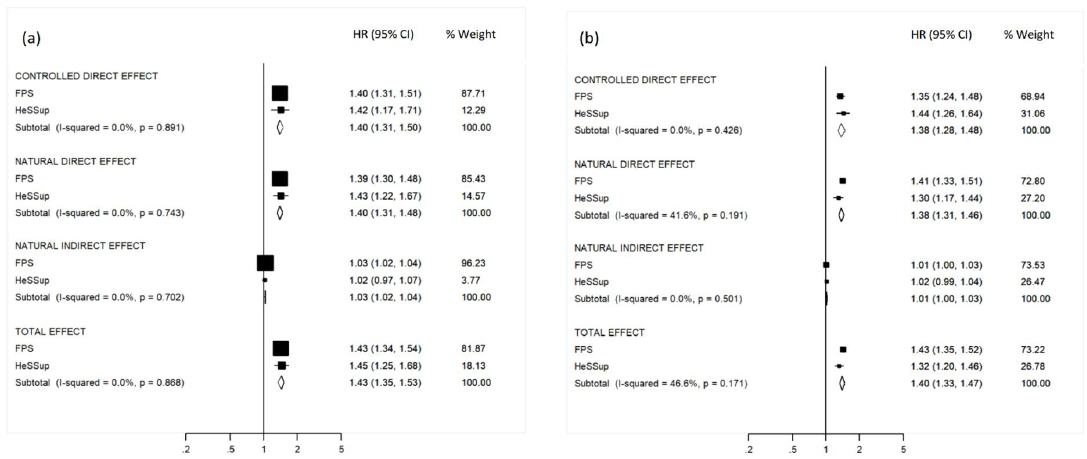
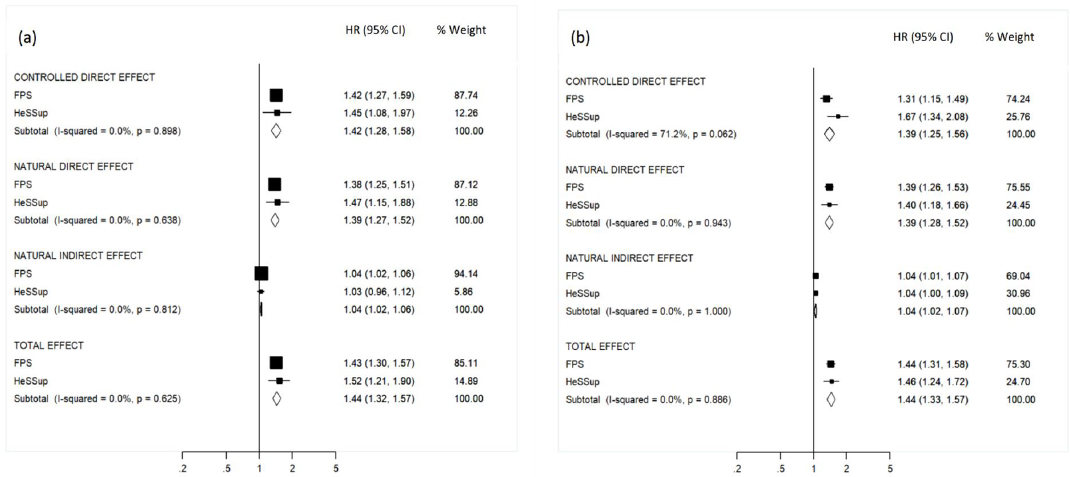
Figure 2 shows the results of the counterfactual modelling of incident disability pension. The pooled adjusted HR for overweight compared to normal weight was 1.42 (95% CI 1.28–1.58) (ie, the CDE). The HR for overweight was slightly lower [1.39 (95% CI 1.27–1.52)] in a scenario in which physical activity among overweight individuals was at the same level as that of individuals of normal weight (ie, the NDE). However, as overweight individuals were less physically active than those of normal weight, the risk of disability pension among overweight individuals due to physical inactivity (ie, the NIE) was 1.04 (95% CI 1.02–1.06) times higher than among those of normal weight, solely because of the lower physical activity in the first group. This means that the risk of disability pension would decrease by 4% if overweight people increased their level of physical activity to that of normal-weight people. Multiplying the direct and indirect effects of overweight led to a HR of 1.44 (95% CI 1.32–1.57) for the association between overweight and incident disability pension (ie, the TE). (figure 2, panel A.) The congruent results using continuous MET hours as the mediator are shown in figure 2, panel B.
Figure 2
Counterfactual mediation analysis on the association between overweight and disability pension, with (a) binary variable physical inactivity and (b) continuous variable metabolic task hours as a mediator. Study-specific and pooled hazard ratios (HR) are adjusted for sex, age, socioeconomic status, smoking, and alcohol consumption. Controlled direct effect refers to the physical activity-adjusted association between overweight and sickness absence allowing an interaction between overweight and physical activity. Natural direct effect refers to the HR for the association between overweight and sickness absence in a scenario in which physical activity among overweight individuals is at a similar level to that among those of normal weight. Natural indirect effect refers to the excess risk of sickness absence among the overweight individuals that is due to their lower physically activity. In the total effect, both natural direct and indirect effects are considered to estimate the association between overweight and sickness absence. [FPS=Finnish Public Sector study; HeSSup=Health and Social Support study; HR=hazard ratio; 95% CI=95% confidence interval].
Supplementary tables S2 and S3 (www.sjweh.fi/show_abstract.php?abstract_id=3799) show the cohort specific results of counterfactual modelling when allowing and not allowing for exposure–mediator interaction, as well as P-values for interaction tests.
Supplementary table S4 (www.sjweh.fi/show_abstract.php?abstract_id=3799) shows the results of counterfactual mediation analysis allowing for exposure × mediator interaction when omitting participants with incident chronic disease between T1 and T2. The results were replicated in this sub-cohort: risk of long-term absence was 1.03 (95% CI 1.00–1.06) times higher among overweight individuals than among those of normal weight due to lower physical activity among the overweight. The corresponding HR for disability pension was 1.04 (95% CI 0.99–1.09).
Analyzing observational data as a pseudo-trial
There were 11 856 overweight participants in T1 (table 1). Of these, 90% were overweight also in T2 (N=10 614). The analysis included overweight and inactive participants at T1, and overweight at T2 (n=3453). We compared the risk of work disability after T2 between participants who continued to be inactive at T2 (N=1592) to the risk of those who increased their level of activity at T2 (N=1861). The pooled risk of both sickness absence (HR 0.82; 95% CI 0.70–0.94) and disability pension (HR=0.71; 95% CI 0.57–0.89) were lower among those who increased their physical activity compared to those who remained inactive. Analyses with MET hours replicated these findings (table 2).
Table 2
Hazard ratio (HR) for work disability among participants who were physically inactive at T1 and overweight at T1 and T2. Physical inactivity is measured as dichotomy and as continuous metabolic equivant task (MET) hours. When using continuous MET hours, cut-point for T1 inactivity was based on median value. [CI=confidence interval].
| N of cases / total N | Pooled HRa | 95% CI | Heterogeneity (I2, P-value) | |
|---|---|---|---|---|
| Long-term sickness absence | ||||
| Physically active at T2 | 702/3453 | 0.82 | 0.70–0.94 | 0%, 0.403 |
| MET hours at T2 per 10-unit increase | 1414/7394 | 0.97 | 0.94–1.01 | 0%, 0.795 |
| Disability pension | ||||
| Physically active at T2 | 331/3453 | 0.71 | 0.57–0.89 | 15%, 0.276 |
| MET hours at T2 per 10-unit increase | 667/7394 | 0.91 | 0.85–0.96 | 0%, 0.333 |
Supplementary table S5 (www.sjweh.fi/show_abstract.php?abstract_id=3799) shows the results of pseudo-trial when omitting participants with incident chronic disease between T1 and T2 (N=3097). The pooled risk of both sickness absence (HR 0.83; 95% CI 0.71–0.97) and disability pension (HR 0.71; 95% CI 0.56–0.90) were lower among those who increased their physical activity compared to those who remained inactive.
Residual confounding remains an issue because weight of the participants can change between the two measurements even when there is no change in weight category. To address this potential source of residual confounding, we repeated analyses including only participants who were overweight both at T1 and T2 and had little (<5%) change in BMI between these time points (N=2071, ie, 60% of the 3453 physically inactive participants who were overweight at T1 and T2). As shown in supplementary table S6 (www.sjweh.fi/show_abstract.php?abstract_id=3799), the results of the pseudo-trial in this population were similar to those for all overweight participants
Finally, we tested whether the results held if we included only consistently obese participants (BMI ≥30). Here the associations diluted, and increased physical activity was not associated with better prognosis of work disability (supplementary table S7, www.sjweh.fi/show_abstract.php?abstract_id=3799).
Discussion
Use of different approaches is important to obtain robust evidence. We used two modelling approaches to estimate the extent to which increasing physical activity would reduce the risk of work disability among overweight people. The counterfactual modelling assumed that it is possible to increase the physical activity level of overweight people to the same level as observed among normal-weight people. We found that overweight individuals were more likely to be physically inactive than individuals of normal weight (prevalence of physical inactivity 26–28% versus 14–17%) and that the relative risk of work disability was 1.38 to 1.40 times higher among overweight individuals when the effects of their lower physical activity were considered. The difference between the physical activity of the two groups accounted for 3 to 4% of the risk of work disability among overweight individuals, suggesting that the relative risk for overweight would be slightly lower if the average physical activity level was increased to that observed among normal-weight individuals. The second approach showed that the benefit would be much greater for those overweight individuals who are physically inactive if they adopted a physically active lifestyle. According to a pseudo-trial analysis, their risk of work disability would reduce by 18–29%. The converging results from two different counterfactual approaches support the robustness of our findings.
On average, individuals of normal weight had 31 weekly MET hours, which corresponds to 6–9 hours of brisk walking per week, including commuting time. As the average level among overweight individuals was 23 MET hours, increasing the level of physical activity among overweight individuals to that of those of normal weight would correspond to an 8 MET-hour increase; 2–3 hours of brisk walking per week. This increase appeared to result in relatively modest reduction in work disability risk. In contrast, for an overweight person who reports being very inactive (median of 4 weekly MET hours), adopting a physically active lifestyle (median of 26–27 MET hours) appeared highly beneficial in terms of disability risk reduction. This reflects the importance of physical activity to retain work ability for overweight people.
Our findings were based on evidence from two independent longitudinal cohort studies with no significant between-study heterogeneity and remained unchanged with two different indices of work disability (long-term sickness absence and disability pension). The findings were not dependent on the scaling of physical activity because the same indirect effect was observed when we used binary operationalization of physical activity (inactive versus not) and continuous MET hour measurement. In addition, we used a pseudo-trial design to strengthen the evidence on causality, and those results corresponded to counterfactual mediation analyses. Low physical activity is related to many chronic diseases, and the lack of increase in physical activity from baseline to follow-up among physically inactive might be due to incident chronic disease. Thus, in sensitivity analyses, we omitted those participants with incident bronchial asthma, myocardial infarction, angina pectoris, cerebrovascular diseases, arthritis, sciatica, migraine, depression, or diabetes between the two measurement points. The results were congruent to main analyses, and thus supporting our conclusions. To control for weight change between T1 and T2 among overweight participants, we included only participants with maximum of 5% change in BMI between measurement points. The results were congruent to the main analyses.
Our results may be of both clinical and practical importance. At the population level, a 3–4% reduction in work disability and subsequent saved work hours is significant. Stable weight loss is difficult to achieve (15), and unhealthy weight cycling is commonly observed (34). It has been estimated that only one in five overweight or obese people intentionally lose >10% of their body weight and maintain this loss for more than one year (35, 36). Physical training, regardless of weight loss, could provide health benefits for overweight people (16) if they were able to maintain their activity level. Lasting weight loss may also be more likely when combined with physical exercise (36). Our results from counterfactual modelling suggest that a small albeit significant reduction in work disability risk would be achieved if overweight people increased their physical activity.
We found a more marked reduction in this risk for a change from physically inactivity to physically active when applying the pseudo-trial approach in a subgroup of participants who were both overweight and inactive. As increase in physical activity may often be accompanied by other favorable lifestyle changes not measured in this study, our results are more likely to be over- rather than underestimates of the true reduction in work disability risk among the physically inactive overweight population. Moreover, it may be unrealistic to assume that obese individuals could be as physically active as normal-weight people due to the pain and other problems resulting from excess weight on joints and bones. Our subgroup analyses of the pseudo-trial supported this view as the estimated impact of the pseudo-trial was greater for overweight than obese people.
One strength of this study was the ascertainment of work disability by two different indicators based on reliable register data with high coverage. We pooled the data from two independent cohort studies, one of which was an employee cohort and the other a general population sample. The fact that the pooled estimates were converging and had no significant heterogeneity increases the strength of the evidence regarding the generalizability of the observed effects.
A major advantage of counterfactual analysis is that it enabled the explicit dissection of the indirect effect of physical activity, providing an estimate of benefit which is more relevant than effect attenuation in terms of policy and practice. Use of pseudo-trial analysis as a complementary approach increased the strengths of our study by including an explicit prospective design to ascertain the correct temporal order in measuring overweight, change in physical activity and risk of work disability.
Some limitations should be considered when interpreting the evidence. Although the measurement of exposure was before the measurement of mediator in our approach, we cannot be certain that the temporal order between the exposure and the mediator was correctly estimated. We were not able to control for all possible confounding factors. For example, we had no relevant data on physical work environment, which may have caused some confounding. However, socioeconomic status taps variation in the physical and psychosocial work environment, and our findings were robust to adjustment for socioeconomic status, suggesting that a major bias is unlikely. Indeed, earlier research has demonstrated that socioeconomic status, age and sex largely account for the effects of the psychosocial work environment on future work disability (37). Furthermore, although both weight gain and physical inactivity have been found to be associated with psychosocial work stressors, these associations are relatively modest (29, 38). The measurements of weight, height and physical activity were based on self-reports and thus open to reporting bias. People tend to underestimate their weight (39), and overestimate their physical activity (40). This could have inflated associations between BMI and physical activity and led either to over- or underestimation of the association between these factors and work disability. Future studies should use more objective measures of weight and physical activity.
In conclusion, we estimated that at the population level, a rather modest increase in physical activity among overweight individuals would have a small beneficial effect on their risk of future work disability. However, for overweight individuals who are physically inactive, adopting a physically active lifestyle was associated with a substantial reduction in work disability risk. These results may be used by occupational health care professionals to advice and motivate their patients to increase their physical activity as a means of treating overweight and preventing work disability.



