Absence from the labor market due to sickness absence and disability pension (DP) is a growing problem in Western countries (1, 2). Sickness absence may have adverse outcomes such as an unfavorable impact on an individual’s career advancement, income, and social interaction (3, 4). Furthermore, sickness absence has been associated with premature mortality (5).
Currently, the two most common reasons for sickness absence are mental and musculoskeletal disorders (6). Mental disorders are also the fastest growing reason for sickness absence in Sweden (7). Further, mental disorders seem to lead to a longer duration of sickness absence compared to other diagnostic groups, and individuals with mental disorders also have the lowest rate of return to work (8). Poor working conditions such as high job demands, low job control, high effort‒reward imbalance, and low social support can lead to mental ill health (9). However, the increase in sickness absence due to mental disorders is not yet fully understood.
Sickness absence is a part of healthcare and treatment and should be an opportunity for healing and rehabilitation before returning to work. However, in more severe cases, prolonged sickness absence or disability pension may be necessary (10, 11). Previous studies have shown some unintended detrimental side-effects of prolonged sickness absence (12), though causality is unclear as this could be due to a complex interplay of disease, treatment and other circumstances surrounding the individual. The nature and severity of the disorder do not seem to be the only driving force behind this transition; other factors are also of importance (13). One study found that among sickness absentees, higher age and longer sick leave spells were risk factors for all-cause DP while having higher education and young children were protective factors (14). Furthermore, in the same paper, investigators reported sickness absence due to mental disorders had a higher risk of all-cause DP compared to sickness absence due to musculoskeletal disorders (14).
Low socioeconomic position is associated with sickness absence and DP (15–17), and occupational class is frequently used as a proxy for socioeconomic position. Occupational class is often categorized as white- or blue-collar workers. In broad terms, the distinction between the two lies in that white-collar workers perform non-manual office work while blue-collar workers perform manual work. Manual workers seem to have a higher risk of DP compared to non-manual workers (18–20), and lower level white-collar workers are more at risk than their higher level counterparts (20). The higher risk of DP within blue-collar workers can be explained by physical working conditions and, to some extent, by lifestyle (21). However, less is known about whether occupational class (ie, blue- or white-collar work) plays a role in the transition from sickness absence to DP, especially long-term sickness-absence (LTSA). Studies of influential factors on the pathway from LTSA to DP are largely lacking. Therefore, we propose to explore occupational class in the present study based on previous knowledge of the association with DP.
Moreover, familial factors (genetic factors and the environment that twins share, primarily in childhood) might also contribute to explaining the risk of moving from LTSA to DP. Familial factors can be examined using a discordant twin-study design. Twin studies take advantage of the natural experiment that there are two types of twins, identical and fraternal, who share different amount of genetics (100% and 50%, respectively). Both types of twins also share environment to the same extent. By using a matched analysis of the discordant twin pairs, where one twin experienced LTSA and the other did not, we can adjust for familial factors. Previous twin studies have shown that both LTSA and DP are moderately influenced by genetic factors (22–25). Although a few studies have shown that the associations between sociodemographic factors, such as occupational class and education, and DP are not influenced by familial factors (19, 20), more studies are needed to confirm these findings, especially while also studying LTSA across occupational classes.
The aim of this study was to investigate the association between LTSA due to mental disorders and musculoskeletal disorders and all-cause DP among blue- and white-collar workers (occupational class). Additional objectives were to examine the influence of familial factors on the association between LTSA and all-cause DP and to study familial influences on the associations across occupational class.
Methods
This is a prospective twin cohort study based on data from the Swedish Twin Project of Disability Pension and Sickness Absence (STODS). Data from two surveys included in STODS were used. Respondents to SALT (Screening across the Lifespan Twin) Study consists of twins born 1925–1958 while respondents to STAGE (Study of Twin Adults: Genes and Environment) consists of twins born 1959–1985. The SALT interview was conducted between January 1998 and March 2003 while the STAGE cohort was invited to answer a web-based questionnaire in 2005, with largely the same questions as in SALT. In total, 64 757 twins answered either the SALT or STAGE surveys conducted by the Swedish Twin Registry (26). All participants in the surveys gave informed consent. The Regional Ethical Review Board in Stockholm, Sweden, approved this study (Dnr: 2007/524-31, Dnr: 2010/1346-32/5, and Dnr: 2014/311-32).
Data were also obtained from several national registers: (i) MiDAS held by the National Social Insurance Agency, contains information on LTSA and DP including ICD-diagnosis, duration, and grade; (ii) LISA held by Statistics Sweden contains information on old age pension, work status, and education; and (iii) Cause of death register held by the National Board of Health and Welfare contains information on the date of death. The data from these registers and surveys were linked using the Swedish 10-digit personal identification number.
We excluded those who at baseline (1 January 2007) were: deceased (cause of death register), missing from the LISA register either in 2005 or 2006, ≥65 years, and on old age pension in either 2005 or 2006 (LISA), on all-cause DP (MiDAS). Those who had no follow-up time due to missing data in LISA in 2007 and 2008 were also excluded (figure 1).
Figure 1
Flow chart of the study population, inclusion and exclusion criteria. LTSA: Long-term sickness absence (>14 days).
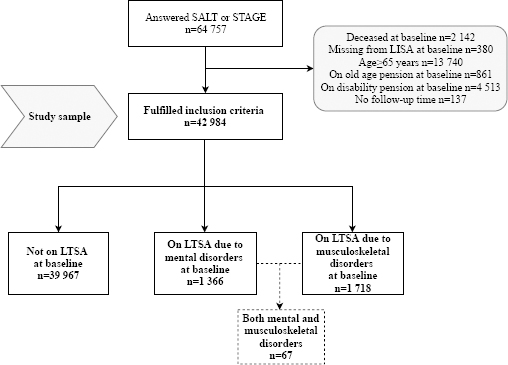
The final sample included a total of 42 984 individuals. Of those, 14 621 were complete twin pairs; 5050 monozygotic (MZ) pairs, 4585 same-sex and 4658 opposite-sex dizygotic (DZ) pairs, and 328 with unknown zygosity. Additionally, data were available for 13 742 twins without co-twins, ie, the twin sibling did not respond to SALT or STAGE, or the twin sibling was excluded based on the above criteria. For details on zygosity determination in the Swedish Twin Registry see Magnusson et al (27). Throughout the rest of the paper, N refers to the total number of individuals, not twin pairs, unless otherwise specified.
The mean age of the participants was 43.8 (standard deviation 12.4) years and roughly half were women (52.8%) (table 1). The sample comprised 53.2% white-and 46.8% blue-collar workers.
Table 1
Characteristics of the sample, stratified by long-term sickness absence (LTSA, >14 days) status at baseline. [SD=standard deviation.]
| Variables | All participants Mean age 43.8 (SD12.4) years | No LTSA a Mean age 43.5 (SD12.5) years | LTSA a Mean age 46.7 (SD11.2) years |
|---|---|---|---|
|
|
|||
| N (%) | N (%) | N (%) | |
| Occupational class | |||
| White-collar | 19 378 (53.2) | 18 185 (54.0) | 1193 (43.6) |
| Blue-collar | 17 061 (46.8) | 15 520 (46.1) | 1541 (56.4) |
| Sex | |||
| Men | 20 290 (47.2) | 19 248 (48.2) | 1042 (34.5) |
| Women | 22 694 (52.8) | 20 719 (51.8) | 1975 (65.5) |
| Zygosity | |||
| Monozygotic | 13 495 (31.4) | 12 556 (31.4) | 939 (31.1) |
| Dizygotic same sex | 13 960 (32.5) | 12 990 (32.5) | 970 (32.2) |
| Dizygotic opposite sex | 14 421 (33.6) | 13 387 (33.5) | 1034 (34.3) |
| Unknown zygosity | 1108 (2.6) | 1034 (2.6) | 74 (2.5) |
| Cohort | |||
| SALT (1925-1958) | 18 800 (43.7) | 17 234 (43.1) | 1566 (51.9) |
| STAGE (1959-1985) | 24 184 (56.3) | 22 733 (56.9) | 1451 (48.1) |
| Education | |||
| Elementary | 5338 (12.4) | 4864 (12.2) | 474 (15.7) |
| Secondary | 20 905 (48.7) | 19 231 (48.1) | 1674 (55.5) |
| Higher education | 16 728 (38.9) | 15 860 (39.7) | 868 (28.8) |
| Employment status | |||
| Not working | 5027 (11.7) | 4797 (12.0) | 230 (7.6) |
| Working | 37 957 (88.3) | 35 170 (88.0) | 2787 (92.4) |
| Urban/rural environment | |||
| Urban | 30 753 (71.6) | 28 691 (71.8) | 2062 (68.4) |
| Semi-urban/rural | 12 231 (28.5) | 11 276 (28.2) | 955 (31.7) |
| Marital status | |||
| Married/Co-habiting | 30 284 (71.5) | 28 109 (71.4) | 2175 (72.9) |
| Single | 12 062 (28.5) | 11 253 (28.6) | 809 (27.1) |
| Children <18 living at home | |||
| No | 27 022 (62.9) | 25 147 (62.9) | 1875 (62.2) |
| Yes | 15 962 (37.1) | 14 820 (37.1) | 1142 (37.9) |
Exposure – sickness absence
All individuals in Sweden >16 years, with an income from work or unemployment benefits, can receive sickness benefits paid by the Social Insurance Agency when disease or injury has caused reduced work capacity for >14 days. Employees receive sick pay from their employers during the first 14 days after a qualifying day without benefits (self-employed usually have more qualifying days). Unemployed individuals have one qualifying day and receive sick pay from the Social Insurance Agency from the second day.
The first LTSA spell (>14 consecutive days between 1 January 2005 to 31 December 2006) either due to mental (ICD-10 codes F00-F99) or musculoskeletal (ICD-10 codes M00-M99) diagnoses, respectively, were used as exposure variables. LTSA was used as both a binary variable (yes/no) and categorized as the duration of LTSA based on net days (calculated by adding up the grade of the LTSA days). Three categories were created: no LTSA, LTSA <6 months, and LTSA ≥6 months.
The majority of LTSA spells were <6 months for both mental (78.5%) and musculoskeletal diagnoses (85.8%).
Outcome – disability pension
A national social security DP scheme covers all citizens in Sweden. To be eligible for disability pension benefits, workers require a medically confirmed disorder or injury that permanently reduces work capacity by ≥25%. The Social Insurance Agency can grant a DP that covers about 65% of lost income based on a thorough assessment of the level of work incapacity.
The participants were followed up for all-cause DP from 1 January 2007 to 31 December 2012. Participants were censored for death, emigration, and old age pension. If a person was missing for two years in the LISA register, emigration date was set at 1 January of the first of those two years. As there was no information on the exact date of old age pension, we chose 1 July of the year as the censoring date. The average follow-up time was 5.4 years.
Occupational class
Occupational class was obtained from the questionnaire data. The answers from an open question (the same question in both SALT and STAGE): “what has been your main occupation for most of your working life?” were coded using the SSYK system (the standard for Swedish occupational classification) (28). SSYK has ten categories which were dichotomized into white- or blue-collar workers following a simplified version of the classification by Thell (29), which is based on what the work entails, education required, and supervision responsibility. The white-collar workers consist of legislators, senior officials, and managers; professionals, technicians and associate professionals; and clerks. The blue-collar workers include service workers and shop sales workers; skilled agricultural and fishery workers; craft and related trades workers; plant and machine operators and assemblers; and elementary occupations. For some individuals in SALT, the SSYK classification was missing. To minimize missing values on this variable, we replaced missing values with the NYK classification code (Nordic Occupational Classification) (28) when available (N=112), however, 15.2% (N=6545) were still missing on this variable.
Other covariates
Marital status was based on the survey question: “What is your current marital status?”. The responses were categorized into married/cohabiting or other (included: divorced, separated, living separately, widow/widower). The cohort effect was binary, ie, belonging to either SALT or STAGE. Sex and date of birth were extracted from the Swedish Twin Registry, the latter of which was used to calculate the age of the participants on 1 January 2007. Information on having children >18 years living at home (yes/no), urban/rural environment (urban or semi-urban/rural), and employment status ie, being currently employed (yes/no), education (elementary, secondary or higher education) were obtained from the LISA register.
Statistical analyses
The association between LTSA and all-cause DP was estimated using Cox proportional hazards regression analyses. The results were presented as hazard ratios (HR) with 95% confidence intervals (CI). The unit of the follow-up time was days. The condition of the proportional hazards assumption was explored via graphs and was met in all the models. We ran two separate analyses: (1) for LTSA due to mental disorders and (ii) for LTSA due to musculoskeletal disorders. The main model was adjusted for sex, age, cohort effect, children <18 years living at home, marital status, urban/rural environment, and employment status. In all models, the standard errors were adjusted for pair identity to take into account the within-pair correlations.
The presence of interaction between occupational class and LTSA was explored using relative excess risk due to interaction (RERI) (30). The RERI is a measure of departure from additivity. It will indicate whether the observed effect of two variables combined is larger (or smaller) than the sum of the individual effects of the two variables, ie, additive interaction. A RERI of 0 suggests no interaction while a RERI >0 suggest a positive additive interaction and RERI<0 suggests a negative additive interaction (30). We calculated the RERI based on the main, fully adjusted model using the Andersson et al method (31). To do this we constructed variables for every combination of occupational class and LTSA possible, with white-collar workers who had not had LTSA >14 days as a reference group.
Familial factors were adjusted for by applying conditional Cox proportional hazards models. The analyses were based on same-sex discordant twin pairs to adjust for familial (genetics and shared family environment) confounding (32). A twin pair was treated as discordant if only one twin of a pair had all-cause DP during follow-up. In discordant twin pair analyses, twins in a pair are optimally matched on genetics (MZ 100% and DZ on average 50%) and shared environmental factors (100%) and for age and sex. If the association found in the age and sex-adjusted analyses of the whole sample disappears or becomes weaker in the analyses of discordant twin pairs, there is a suggestion that familial factors are influencing the association. If a stronger association is observed after controlling for familial factors this would instead suggest a causal link between the exposure and the outcome (32). MZ and DZ twin pairs were pooled for the analyses as there was not enough power to stratify by zygosity. We also did some stratified analyses, ie, investigating the effect of LTSA across occupational class and reported these in the appendix.
Analyses were conducted using Stata IC 12.1 (Stata Corp, College Station, TX, USA), and the significance level was set at α=0.05.
Results
Among the 42 984 participants, there were 989 cases of all-cause DP. As the average follow-up was 5.4 years, the incidence rate (IR) was 423.45 cases per 100 000 person-years. There were 3017 cases of LTSA, of which 1299 and 1651 cases were due to mental disorders and musculoskeletal disorders, respectively. Additionally, 67 individuals had both a mental and musculoskeletal LTSA spell during the inclusion period. As excluding these 67 cases did not lead to important changes in the results, they were included in the analysis of each disorder to preserve statistical power.
The proportion of individuals among white-collar workers granted all-cause DP was 2.0% (379/19 378). The corresponding proportion of blue-collar workers was 3.0% (504/17 061). The relative risk ratio (RR) for white- versus blue-collar (white-collar reference group) was 1.51 (95% CI 1.32–1.72). Looking only at those who were on LTSA due to mental disorders, the proportion of individuals granted all-cause DP was 8.3% (56/672) for white-collar workers and 9.9% (55/556) for blue-collar workers. The RR between white- and blue-collar workers among those on LTSA due to mental disorders was 1.19 (95% CI 0.83–1.70). Finally, when restricting to those who were on LTSA due to musculoskeletal disorders, 10.1% (54/536) of white-collar workers and 12.0% (124/1032) of blue-collar workers were granted all-cause DP, with an RR of 1.19 (95% CI 0.88–1.61).
Sickness absence due to mental disorders
For those on LTSA due to mental disorders, the HR was 4.37 (95% CI 3.61–5.28) in the fully adjusted model compared to those not on LTSA (supplementary table S1, www.sjweh.fi/show_abstract.php?abstract_id=3816). When compared to the reference group of white-collar workers without LTSA, both blue- and white-collar workers with LTSA due to mental disorders had a higher risk of all-cause DP (Table 2).
Table 2
The association between long-term sickness absence (LTSA, >14 days) due to mental disorders at baseline and all-cause disability pension during follow-up, interaction by occupational class (N=42 984). [Blue=blue-collar worker; CI=confidence interval; HR=hazard ratio; IR=incidence rate; ref=reference group; RERI=relative excess risk due to interaction; while=white-collar worker.] Bold=P<0.05.
| LTSA × occupational class × occupation | N | Person years | IR per 100 000 person years | HR (95% CI) a | RERI (95% CI) |
|---|---|---|---|---|---|
| Dichotomized | |||||
| No LTSA | |||||
| White | 18 706 | 99 927 | 323 | Ref | |
| Blue | 16 505 | 88 817 | 506 | 1.50 (1.27–1.77) | |
| LTSA | |||||
| White | 672 | 3488 | 1605 | 4.77 (3.59–6.35) | |
| Blue | 556 | 2897 | 1899 | 5.48 (4.04–7.42) | 0.21 (-1.76–2.17) |
| Duration | |||||
| No LTSA | |||||
| White | 18 706 | 99 927 | 323 | Ref | |
| Blue | 16 505 | 88 817 | 506 | 1.51 (1.28–1.78) | |
| LTSA <6 months | |||||
| White | 526 | 2821 | 815 | 2.44 (1.60–3.72) | |
| Blue | 440 | 2356 | 1273 | 3.73 (2.53–5.49) | 0.80 (-0.89–2.49) |
| LTSA ≥6 months | |||||
| White | 146 | 667 | 4950 | 14.15 (9.90–20.24) | |
| Blue | 116 | 541 | 4623 | 12.91 (8.26–20.20) | -1.73 (-9.14–5.69) |
When LTSA duration was explored (Table 2), there was an increased risk of all-cause DP among blue-collar workers without LTSA (HR 1.51, 95% CI 1.28–1.78), blue-collar workers that had been LTSA for 14 days to 6 months (HR 3.73, 95% CI 2.53–5.49), and blue-collar workers that had been LTSA for ≥6 months (HR 12.91, 95% CI 8.26–20.20) compared to the reference group of white-collar workers without LTSA. Similar patterns were seen for white-collar workers, ie, rising risk with longer LTSA. The RERI for LTSA due to mental disorders and occupational class were all close to 0 or rather low (table 2), which suggests that there was no or negligent interaction between the two variables.
Sickness absence due to musculoskeletal disorders
Those on LTSA due to musculoskeletal disorders had an HR of 5.04 (95% CI 4.28–5.93) for all-cause DP in the fully adjusted model, compared to those who were not on LTSA due to musculoskeletal disorders (supplementary table S2, www.sjweh.fi/show_abstract.php?abstract_id=3816). Compared to being a white-collar worker without LTSA, there was an increased risk of all-cause DP for both blue- and white-collar workers that had been on LTSA (Table 3).
Table 3
The association between long-term sickness absence (LTSA, >14 days) due to musculoskeletal disorders at baseline and all-cause disability pension during follow-up, interaction by occupational class (N=42 984). [Blue=blue-collar worker; CI=confidence interval; HR=hazard ratio; IR=incidence rate; ref=reference group; RERI=relative excess risk due to interaction; while=white-collar worker.] Bold=P<0.05.
| LTSA × occupational class × occupation | N | Person years | IR per 100 000 person years | HR (95% CI) a | RERI (95% CI) |
|---|---|---|---|---|---|
| Dichotomized | |||||
| No LTSA | |||||
| White | 18 842 | 10 0812 | 322 | Ref | |
| Blue | 16 029 | 86 660 | 438 | 1.35 (1.14–1.60) | |
| LTSA | |||||
| White | 536 | 2604 | 2074 | 5.52 (4.11–7.41) | |
| Blue | 1032 | 5054 | 2454 | 6.12 (4.87–7.68) | 0.23 (-1.67–2.13) |
| Duration | |||||
| No LTSA | |||||
| White | 18 842 | 10 0812 | 322 | Ref | |
| Blue | 16 029 | 86 660 | 438 | 1.36 (1.15–1.61) | |
| LTSA <6 months | |||||
| White | 473 | 2385 | 1132 | 3.03 (2.04–4.50) | |
| Blue | 859 | 4371 | 1578 | 4.07 (3.08–5.38) | 0.66 (-0.87–2.19) |
| LTSA ≥6 months | |||||
| White | 63 | 219 | 12 332 | 31.48 (20.43–48.48) | |
| Blue | 173 | 682 | 8060 | 17.69 (13.12–23.85) | -14.23 (-28.22– -0.23) |
Categorizing LTSA due to musculoskeletal disorders according to duration revealed that when compared to white-collar workers without LTSA, both blue- and white-collar workers with LTSA for >14 days to <6 months had similarly increased risk of all-cause DP (white-collar: HR 3.03, 95% CI 2.04–4.510; blue-collar: HR 4.076, 95% CI 3.087–5.386). However, the risk of all-cause DP was much higher for white-collar workers who had been on LTSA for ≥6 months (HR 31.50 95% CI 20.45–48.52) than for blue-collar workers (HR 17.694 95% CI 13.0812–23.7885) where both were compared to white-collar workers not on LTSA. The RERI for LTSA due to musculoskeletal disorders and occupational class were rather low, except for the LTSA of ≥6 months (RERI -14.23). This suggests that that occupational class modifies the relationship between LTSA due to musculoskeletal disorders and disability pension when the duration of LTSA is ≥6 months.
Discordant twin analyses
The results from the discordant twin pair analyses should be compared to that of the age and sex-adjusted results (table 4). An effect of familiar factors is indicated if the associations found in the sex and age-adjusted models differ considerably in the discordant twin models. Our results show that the HR diluted, frequently to statistical non-significance, and are smaller for the association between LTSA due to mental disorders and all-cause DP (table 4) for both white- and blue-collar workers. This suggests that familial factors explain some of the association between LTSA due to mental disorders and all-cause DP. The adjustment for familial factors did not markedly change the results for LTSA due to musculoskeletal disorders and all-cause DP (Table 4). There were 676 twins discordant on all-cause DP, and 4314 were discordant on occupational class.
Table 4
The association between long-term sickness absence (>14 days) due to mental and musculoskeletal disorders at baseline, respectively, and all-cause disability pension during follow-up, interaction by occupational class (N=42 984 for the whole cohort and N=676 for discordant twins (338 twin pairs). [Blue=blue-collar worker; CI=confidence interval; HR=hazard ratio; IR=incidence rate; ref=reference group; RERI=relative excess risk due to interaction; while=white-collar worker.] Bold=P<0.05.
Discussion
In this study, we aimed to investigate if occupational class and familial factors influenced the associations between LTSA due to mental or musculoskeletal disorders and DP. We found that occupational class had an impact on the association between LTSA due to musculoskeletal ‒ but not mental ‒ disorders and all-cause DP. We also found that familial factors explained some of the association between LTSA due to mental disorders and all-cause DP, though the power was somewhat limited.
LTSA due to both mental and musculoskeletal disorders was found to increase the risk for future all-cause DP in both blue- and white-collar workers, which is in line with previous studies (10, 33). Earlier research states that both higher education and income are protective against moving from sickness absence to all-cause DP (14, 34, 35). Although our results are largely in line with this, the risk of all-cause DP was noticeably higher for white-collar workers when the LTSA due to musculoskeletal disorders was ≥6 months than for their blue-collar worker counterparts. The effect modification was considerable, as shown by the high RERI. One explanation for this slight discrepancy may be that income and education are not interchangeable with occupational class (36) since the physical work environment is different between occupational classes. That is, blue-collar workers may need longer sick leave to recover from a musculoskeletal disease or injury than a white-collar worker and, hence, white-collar workers with sick leave >6 months represent the most severe cases.
Working conditions are another possible explanation for why white-collar workers had higher risk estimates for LTSA due to musculoskeletal disorders ≥6 months. Both the physical and psychosocial work environment have been associated with musculoskeletal problems (37, 38), which, in turn, may be of importance for LTSA. There are perhaps more psychosocial risk factors explaining musculoskeletal disorders among white-collar workers. For instance, compared to blue-collar workers, physical risk factors like heavy lifting and awkward work positions are much less prevalent among white-collar workers. This may indicate that it is harder to make successful work adjustments when psychosocial risk factors are involved. Indeed, this may be part of the explanation for the higher within-group risk to receive all-cause DP among white-collars. A health selection might also play a role, ie, that those prone to musculoskeletal disorders choose a less physically demanding career such as office work, while only those with good physical fitness are able to perform the more physically demanding blue-collar work.
The higher risk for all-cause DP among white- compared to blue-collar workers was only observed for those who were on LTSA due to musculoskeletal disorders ≥6 months. Examining LTSA as a binary variable can mask this effect. In clinical terms, shorter sick leave spells would more likely be attributed to workload, stress, flu seasons, etc, while longer spells reflect a more severe underlying condition. Other studies have also demonstrated the importance of looking at different sickness absence durations as predictors for DP (14, 34). Altogether, future studies should include LTSA duration.
Familial factors, ie, genes and early shared environment, influenced the association between LTSA and DP due to mental disorders but did not seem to influence the association between LTSA and DP due to musculoskeletal disorders. This means that genetic and early environmental factors, such as upbringing and family relationships, that contribute to liability for mental disorders may also explain why some transfer from LTSA to DP. Familial factors have been found to influence the liability to both LTSA and DP (24, 25), and a previous study on whether familial factors influence the association between LTSA and DP concluded that familial factors only played a small role in the association (11). However, in that study, all sickness absence diagnoses were pooled together and, thus, might have masked the effects that were observed for LTSA due to mental disorders in the current study. Furthermore, our results are supported by studies that show that mental disorders are heritable (39).
Strength and limitations
The strengths of this study lie in the relatively large sample size and the high quality of the data. The registers cover the whole population, which means we captured all cases of LTSA and DP benefits with no loss to follow-up. Additionally, we differentiated between LTSA diagnoses and quantified the duration of LTSA. Using data from twins enabled us to investigate confounding by familial factors, which can be an important explanatory factor.
The limitations of the study include no data on short-term sickness absence (≤14 days), however, LTSA is probably more important for the risk of transitioning to all-cause DP (14, 34). Another possible design choice would have been to follow the participants not only for disability pension but also for sickness absence as there could be a long interval between the sickness absence spell and disability pension. However, an earlier study with a long follow-up has shown that there is still an effect of sickness absence on disability pension, even after a period of up to 13 years (11). There were some subgroup analyses that were not possible due to low numbers, such as studying more categories of LTSA duration or specific occupational classes. This leads to a rather crude measure of occupation class, which might have masked some associations that a more detailed categorization might have captured. Even though the discordant twin pair analyses may have been low in power, the results give an indication of whether the associations were affected by familial factors. Finally, there was an interval of up to about 7 years between the collection of questionnaire data of the two surveys. We tried to minimize the potential impact of this discrepancy by controlling for cohort effects in the analyses. Importantly, our main variable of interest from the questionnaire (occupational class) asked for the main occupation during most of the respondents’ working life. This variable should, therefore, not have been much affected by the passage of time, especially in the older cohort which answered the questionnaire before the younger cohort.
Concluding remarks
Our results indicate that occupational class plays an important role in the association between LTSA due to musculoskeletal disorders and all-cause DP, with white- and blue-collar workers showing different sick leave patterns leading to all-cause DP. This pattern was not found for LTSA due to mental disorders. We also found that familial factors explained part of the association between LTSA due to mental disorders and DP. Taken together, these results indicate that the pathways from LTSA to all-cause DP are complex and differ depending on the underlying disorder, occupational class, and the importance of familial factors.



