With an increase in life expectancy, the number of people with a chronic disease is growing in many developed countries. In the past years, the World Health Organization (WHO) has published several reports highlighting the high incidence of chronic diseases, such as diabetes, cardiovascular disease, chronic respiratory disease, and cancer. These chronic diseases account for approximately half of the global burden of disease (1, 2), impact individuals in terms of reduced quality of life, and affect employers who have to deal with negative employment outcomes, such as absence from work.
Mental health disorders together with musculoskeletal disorders are the leading causes of sickness absence and work disability in most developed countries (3–6). The high prevalence of chronic diseases implies a public health challenge associated with higher health care costs and decreased workplace productivity (7, 8). Considering the aging population in many western countries, there is a need to prolong active labor force participation. Prevention of chronic diseases and exit from the workforce is therefore essential.
The workplace offers an ideal setting to support the promotion of health of a large proportion of the working population. Offering workplace health interventions is recognized as a feasible and potentially effective strategy for chronic disease prevention and control (1, 2). Workplaces offer the opportunity to promote health on an individual level, eg, by means of behavioral change approaches, but can also target environmental changes to promote health behaviors, such as altering the availability of foods served in the canteen, providing fitness facilities, or nudges to promote taking the stairs for example. Workplace health promotion programs may target the promotion of healthy lifestyle behaviors, as these have been recognized as important modifiable risk factors for several chronic diseases. For example, unhealthy diets, sedentary lifestyles, obesity, and smoking have been identified as important contributing factors for chronic diseases (9, 10).
A systematic review that summarizes the evidence from reviews on the effect of workplace interventions targeting health promotion to improve health outcomes that predict the onset of chronic diseases is currently lacking. In light of the high prevalence of chronic diseases, and the role of the workplace to promote health among workers, a joint action CHRODIS-PLUS work package was initiated to develop a toolkit to support employers in understanding the benefits of health promotion and prevention of chronic diseases to enhance the health and wellbeing of the employees, who are healthy, at risk, or already suffer from a chronic disease. As a first step, this meta-review was performed to systematically summarize the available evidence on the effectiveness of worksite health promotion interventions on physical and mental health outcomes that are related to chronic diseases. For the purpose of this review, the focus was on a selection of chronic diseases, ie, type 2 diabetes mellitus (T2DM), cardiovascular diseases (CVD), and mental health and musculoskeletal disorders, given their high disease burden and lifestyle-relatedness.
Methods
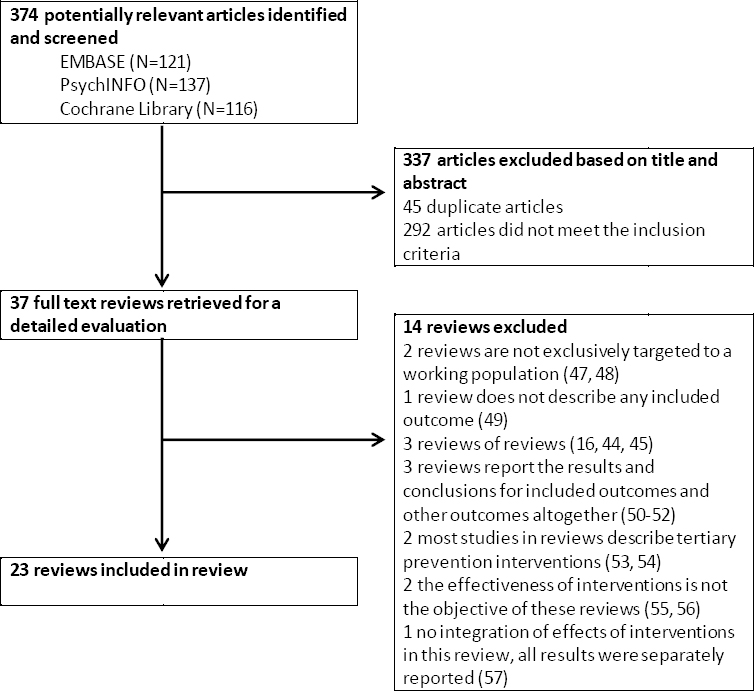
The review was carried out and reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (11).
Literature search
A search for reviews published between January 2009 and February 2018 was performed in electronic databases, ie, www.embase.com (ie, Medline and Embase), PsycINFO, and the Cochrane Library. An experienced librarian assisted in the search strategy and performed the search strategy in the databases. Key terms used in the search strategy referred to the study population or setting, intervention, and outcome under study, and thus included synonyms of terms such as ‘workplace’, ‘worker’, ‘intervention’, ‘health promotion’, ‘lifestyle’, ‘chronic disease’, ‘diabetes’, musculoskeletal disorders’, in combination with ‘review’ or a synonym thereof. An example of the search strategy in www.embase.com is found in Table 1. In addition, the reference lists of the included reviews were checked for additional relevant reviews.
Table 1
Literature search in www.embase.com.
Selection of reviews
Two reviewers independently screened all titles and abstracts retrieved from the search strategy. The records were screened on the inclusion criteria, including the type of design (review), study population (working population), type of intervention (health promotion), and the outcome under study. Reviews were eligible for inclusion if they studied the effectiveness of health promotion interventions targeting a working population. The outcome under review had to be a health outcome that is related to (the prevention of) one of the following chronic diseases: T2DM, CVD, musculoskeletal disorders, or mental health problems. For T2DM and CVD, these included metabolic risk factors, such as elevated blood lipids, cholesterol or systolic blood pressure. For musculoskeletal and mental health disorders, the (self-reported or diagnosed) musculoskeletal or mental health outcomes were included, and could involve a variety of musculoskeletal regions (eg, back, shoulder, knee) and mental health problems (eg, anxiety, depression). Reviews that were primarily focused on treatment of the chronic diseases or work participation with chronic diseases were excluded. The initial screening of the titles and abstracts were discussed between the two reviewers to achieve a list of papers, of which the full-text was retrieved. Then, the two reviewers independently read the full-texts to make the final selection.
Quality appraisal
The methodological quality of the included reviews was evaluated using AMSTAR (A MeaSurement Tool to Assess systematic Reviews) (12, 13). AMSTAR has shown to be a reliable and valid tool for the assessment of the methodological quality of systematic reviews (12) and consists of 11 criteria (13). Table 2 describes all items and the operationalization of the items. For example, two items (#7 and #8) concerned the scientific quality of the included studies, where item 7 was scored positively if a quality assessment tool was used. In case the quality scoring was considered in the analysis, the conclusions of the review, and explicitly stated in formulating recommendations, item 8 was scored positively as well. Each criterion could be scored as yes (1), no (0), or not applicable, yielding a total score between 0‒11. The two reviewers (blinded) independently scored these items for each review included. Afterwards, a meeting took place to discuss and explain their scorings and achieve consensus in case of discrepancies. If consensus could not be reached, a third reviewer was consulted. Based on the scorings, reviews were classified as of high or low quality. If >50% of the criteria was rated positively (score of ≥6 points), the review was considered to be of high quality, otherwise, it was considered to be of low quality (scoring 0‒5 points) (14, 15).
Table 2
Description of the AMSTAR checklist and the operationalization of the items (13).
Data extraction and synthesis of evidence
Two reviewers extracted the data, each doing half of the reviews. A standard format was used to describe the first author, year of publication, type of review, study design of studies included, number of studies included, study population, interventions under study, outcome measures, main results and the authors’ conclusions. Uncertainties were discussed and solved between the two reviewers.
The synthesis of the evidence was based on a best-evidence system used in a previously published systematic review of workplace interventions, consisting of four levels (16): (i) strong evidence (***) in case of >1 high-quality reviews with consistent outcomes; (ii) moderate evidence (**) in case of 1 high-quality and ≥1 low-quality reviews with consistent outcomes; (iii) limited evidence (*) in case of only 1 high-quality or >1 low-quality reviews, all with consistent outcomes; (iv) no evidence in case of only 1 low-quality review, or inconsistent results of the reviews.
Consistency was defined if ≥75% of the reviews showed results in the same direction (14).
Results
Review selection
The literature search identified 374 papers (figure 1). After screening all titles and abstracts, 37 reviews were considered for full-text assessment. Of these, 14 reviews were excluded for various reasons. Consequently, 23 reviews were included in our meta-review.
Quality of the reviews
The two reviewers initially disagreed in 10% of the reviews. As all disagreements were resolved by discussion, a third reviewer was not consulted. Of the 23 reviews, 9 were of high quality (Table 3). Although all reviews reported their funding for the review, they lacked the reporting of source of funding or support for each of the included studies. Thereby, none of the reviews scored positively on the item that involved the conflict of interest. Only 3 reviews met the criterion with respect to the listed in- and excluded studies, and only 4 out of the 23 reviews explicitly stated that they included grey literature.
Table 3
Scores on the AMSTAR checklist for all included reviews.
| A priori design | Duplicate study selection and data extraction | Compre-hensive literature search | Status publication used as inclusion criterion | List of included & excluded studies | Charact-eristics of included studies | Scientific quality assessed & documented | Scientific quality appropriately used in conclusions | Appropriate methods used to combine studies’ findings | Publi-cation bias | Conflicts of interest statement | High a quality | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Anderson et al, 2009 (28) | No | No | Yes | No | Yes | Yes | Yes | No | Yes | No | No | Low |
| Archer et al, 2011 (29) | No | No | Yes | Yes | No | No | Yes | Yes | Yes | No | No | Low |
| Carolan et al, 2017 (17) | Yes | No | Yes | Yes | No | Yes | Yes | No | Yes | Yes | No | High |
| Chu et al, 2014 (17) | No | No | Yes | No | No | Yes | Yes | Yes | No | No | No | Low |
| Conn et al, 2009 (18) | No | No | Yes | Yes | No | No | No | No | Yes | Yes | No | Low |
| Fernandez et al, 2014 (30) | No | No | Yes | No | No | Yes | Yes | Yes | No | No | No | Low |
| Groeneveld et al, 2010 (14) | No | No | Yes | No | No | Yes | Yes | Yes | No | No | No | Low |
| Hafez et al, 2017 (25) | No | Yes | Yes | No | No | Yes | No | N/A | No | No | No | Low |
| Kent Anger et al, 2015 (26) | No | Yes | Yes | No | No | Yes | No | N/A | No | No | No | Low |
| Krungkraipetch et al, 2012 (35) | No | Yes | Yes | No | No | Yes | Yes | Yes | Yes | No | No | High |
| Kwak et al 2014 (27) | No | Yes | Yes | No | No | Yes | Yes | Yes | No | No | No | Low |
| Martin et al 2009 (19) | No | Yes | Yes | No | No | Yes | No | N/A | Yes | Yes | No | Low |
| Mehta et al, 2013 (31) | No | Yes | Yes | Yes | No | Yes | No | N/A | No | No | No | Low |
| Montano et al, 2014 (20) | No | No | Yes | No | No | Yes | Yes | No | Yes | Yes | No | Low |
| Power et al, 2013 (21) | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | No | High |
| Tam et al, 2018 (32) | No | Yes | Yes | No | No | Yes | Yes | Yes | Yes | No | No | High |
| Tan et al, 2014 (22) | No | No | Yes | No | No | Yes | Yes | Yes | Yes | Yes | No | High |
| Tullar et al, 2010 (36) | No | Yes | Yes | No | No | Yes | Yes | Yes | Yes | No | No | High |
| van Eerd et al, 2016 (37) | No | Yes | Yes | No | No | No | No | Yes | Yes | Yes | No | Low |
| van Niekerk et al, 2012 (38) | No | Yes | Yes | No | No | Yes | Yes | Yes | Yes | No | No | High |
| Verbeek et al, 2011 (23) | No | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | No | High |
| Verweij et al, 2011 (24) | No | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | No | High |
| Vuillemin et al, 2011 (33) | No | No | Yes | No | No | Yes | No | Yes | Yes | No | No | Low |
Description of reviews
Most reviews (N=20) were systematic, of which 8 (17–24) performed a meta-analysis. The remaining 3 (25–27) concerned a narrative or scoping review. With respect to the metabolic risk factors for T2DM and CVD, most reviews (14, 18, 20, 21, 24–33) evaluated the effect of workplace health promotion interventions on weight-related outcomes, such as body weight, body mass index (BMI), percentage of body fat, waist circumference. The remaining metabolic risk factors, such as lipid measures, blood glucose, and blood pressure were also studied in 5 reviews (14, 18, 25–27). Defined by depression, anxiety or stress, mental health as outcome was studied in 6 reviews (17–20, 22, 34). Another 6 (20, 23, 35–38) summarized the effect of workplace interventions on the prevention of musculoskeletal disorders.
Effect of interventions on weight-related outcomes
Of the 14 reviews that summarized the effect of workplace health promotion programs on weight-related outcomes, only 3 (21, 24, 32) were of high quality (Table 4). Main outcomes under study included body weight, body mass index (BMI), and body fat percentage. Except for 2 (25, 26), all reviews evaluated studies that targeted the promotion of physical activity and/or healthy diet. These lifestyle behavior interventions however used different strategies, including individually-based approaches and environmental adjustments. A broader approach, such as total worker health interventions in which both health protection and wellness were addressed, was evaluated in 2 reviews (25, 26). All 3 high quality reviews (21, 24, 32) exclusively included randomized controlled trials (RCT) that evaluated the effect of workplace lifestyle interventions targeting diet and/or physical activity. Of these, 2 (21, 24) also performed a meta-analysis of a subsample of their included RCT. Overall, some positive results were found on weight-related outcomes. Verweij et al (24) concluded moderate quality evidence for a favorable effect of workplace physical activity and diet interventions on body weight, BMI, and body fat percentage, but low quality evidence for an effect on body weight of interventions that focused on physical activity only. Furthermore, they recommended the addition of an environmental component to prevent weight gain, which was based on subgroup analyses. Based on the pooled results, Power et al (21) also recommended workplace interventions that targeted both energy balance related behaviors (physical activity and diet) for weight reduction. The third high quality review (32) also concluded some evidence for a positive long-term effect of multicomponent lifestyle interventions targeting obesity and additionally recommended interventions of high intensity or including a motivational component.
The remaining 11 reviews, which were of low quality, overall showed some evidence for beneficial effects on weight-related outcomes although some reported mixed results for different weight-related outcomes. Some reviews recommended specific intervention types to the prevention of weight gain. Archer et al (29), for example, identified six promising practices with sufficient evidence for beneficial effects, including enhanced access to opportunities for physical activity in combination with health education, exercise prescriptions, multicomponent educational practices, weight loss competitions and incentives, and behavioral practices both with and without incentives.
Table 4
Description of the reviews that studied the effect on weight-related outcomes. [RCT=randomized controlled trial; CI=confidence interval; MD= mean different; SMD=standardized mean difference; IQR=interquartile range; CVD=cardiovascular disease.]
| Review | Number and type of studies | Type of intervention | Author’s conclusion |
|---|---|---|---|
| Power et al, 2013 (21) a | N=13 (RCT); N=7 with available data for meta-analysis | Workplace based diet and/or physical activity interventions | 6 interventions reported statistically significant effects on weight related outcomes. Pooling across the 5 studies with follow-up <12 months showed a greater reduction in body weight (-2.03 kg, 95% CI -3.92− -0.15 kg) than controls. No significant difference in body weight change (-2.60, 95% CI -5.37− -0.17 kg) across the 3 studies with ≥12 months follow-up). Workplace interventions targeted both physical activity and diet resulted the largest differences in weight reduction. |
| Tam et al, 2018 (32) a | N=11 (RCT) | Onsite workplace multicomponent lifestyle (exercise and diet) interventions | 5 of the 11 studies reported a statistically significant reduction in BMI lasting 1-2 years; the remaining reported no significant reduction. Some evidence demonstrating long-term effectiveness of multicomponent lifestyle interventions in the workplace targeting obesity. Studies showing significant BMI reductions were of high intensity or included a specific motivational component. |
| Verweij et al, 2011 (24) a | N=43 (RCT); N=22 in meta-analysis | Onsite workplace multicomponent lifestyle (exercise and diet) interventions | Moderate quality of evidence that workplace physical activity and nutrition interventions significantly reduce body weight (MD -1.19kg, 95% CI -1.64− -0.74), BMI (MD: -0.34 kg/m2, 95% CI: -0.46− -0.22) and body fat% (MD -1.12%, 95% CI -1.86− -0.38). Low quality of evidence that interventions targeting physical activity only reduced body weight by MD: -1.08kg, 95% CI -1.79− -0.36). To prevent weight gain, workplace physical activity and nutrition interventions that contain an environmental component are recommended. |
| Anderson et al, 2009 (28) | N=47 (RCT, non-RCT, cohort designs, time series) | Health promotion programs that included strategies involving diet, physical activity, or both. Three types of interventions: (i) informational, (ii) behavioral skills, (iii) policy or environmental. | Only RCT included: SMD weight: -2.8 pounds (95% CI -4.63− -0.96) at 6–12month follow-up (9 RCT); SMD BMI -0.47 (95% CI -1.02− -0.2) at 6–12 months (6 RCT). On basis of all available study designs: Mean change weight: -3.15 pounds (range -14.77− 3.6) at 12 months (12 studies); mean change BMI -0.40 (range -1.57− 0.3) points at 6-9 months (12 studies), -0.02 points (range -0.9− 0.5) at 12 months (12 studies); mean change body fat %: -1.03 (range -2.56− 1.2) at 6-9 months (13 studies). There is evidence of a modest reduction in weight as a result of worksite health promotion programs aimed at improving nutrition, physical activity, or both. |
| Archer et al, 2011 (29) | N=136 (various study designs) | Three strategies: (i) environmental and policy strategies to change the structure of physical and organizational environments to provide healthy food, convenient opportunities for physical activity, and incentives; (ii) informational and educational strategies to change employees’ knowledge and attitudes about the benefits of healthy nutritional habits and opportunities for physical activity; and (iii) behavioral strategies to teach employees skills to successfully adopt and maintain behavioral changes and to create social environments that facilitate and enhance behavioral change. | 6 promising practices identified, with sufficiency of evidence. The following effect sizes (ES) were reported on basis of greatest suitability of study design: Enhanced access to opportunities for physical activity combined with health education (ES -3.24%, IQR -7.24− - 3.09%, 5 studies); Exercise prescriptions alone (ES -2.45%, IQR -3.56− -1.69%, 10 studies); Multicomponent educational practices (ES -2.24, IQR -3.57− -0.99%, 13 studies); Weight loss competitions and incentives (ES -2.66%, IQR -5.34− -1.22%, 6 studies); Behavioral practices with incentives (ES -3.72, IQR -4.69− -1.67%, 8 studies); Behavioral practices without incentives (ES -2.33%, IQR -6.69− -0.55%, 26 studies). |
| Conn et al, 2009 (18) | N=138 (studies with varied designs) | Interventions aimed to improve physical activity | ES: Anthropometric (two-group post-test 0.08 (95% CI 0.02− 0.15); two-group pre-post 0.07 (95% CI 0.03− 0.11); treatment pre-post 0.13 (95% CI 0.10− 0.17) Some interventions improve physical activity in some subjects, which in turn may improve selected health outcomes, but significant heterogeneity requires cautious interpretation of findings. |
| Fernandez et al, 2014 (30) | N=8 (RCT, non-RCT) | Interventions included changes in the food and physical activity environment in the workplace (e.g., cafeteria interventions, establishing walking routes), with or without additional individual-level approaches, with or without changes in policies or programs promoting any aspect of the causal pathways to obesity prevention and control. | 5 studies: body weight and/or fat decrease more in intervention than in control sites, increased more in control than intervention sites, or in intervention sites those measures decreased while in control sites increased. 2 studies: BMI increased more in intervention than in control worksites. 1 study: no quantitative information on the measure of effect. The magnitude of the measure of effect was <1 BMI unit difference in all studies with quantitative reporting. The evidence has low risk of bias since 50% of the studies were deemed to have a low risk of bias. Among the studies evaluated with a low risk of bias, the effect on the measures of body weight or fat was modest and sometimes in the unexpected direction. |
| Groeneveld et al, 2010 (14) | N=31 (RCT); N=20 with body weight/BMI as outcome, N=3 with body fat as outcome | Worksite lifestyle (physical activity and/or healthy diet) or health promotion interventions (such as individual counseling, group education, or self-help) | Strong evidence for a beneficial effect on overall body fat. No evidence for an effect on body weight. |
| Hafez et al, 2017 (25) | N=13 (2 RCT, 1 non-RCT, 1 cluster RCT, 3 single group time series, 2 single group pre-post, 1 multi-group pre-post, 3 cohort studies) | Evidence-based Diabetes Prevention Program (DPP) (N=10) or a non-DPP intervention (N=3) that aimed to prevent type 2 diabetes (T2DM) | DDP: weight loss ranged from 0.4 to 5.1 kg at 3 to 6 months (8 studies) and from 1.43 to 4.9 kg at 7 to 12 months (6 studies). Non-DDP interventions: minimal changes in weight loss at 6 and 12 months (2 studies). Workplace interventions to prevent T2DM are most effective when they utilize the structured, evidence-based DPP curriculum with minimal modifications. |
| Kent Anger et al, 2015 (26) | N=17 (9 RCT, 7 quasi-experimental design, 1 multiple group nonexperimental design) N=5 with weight-related outcome | Total worker health (TWH) interventions: both traditional occupational safety and/or health (OSH, health protection) and wellness and/or well-being should be addressed in the same intervention | Weight significantly changed in ≥3 TWH interventions. Results for weight change were inconsistent in 5 studies. Insufficient evidence to identify best practice interventions. All but one of the 17 TWH intervention programs improved outcomes that are risk factors for injuries and/or chronic diseases and 4 interventions improved ≥10 risk factors. |
| Kwak et al, 2014 (27) | N=10 (RCT) | Interventions implemented by the occupational health services to promote physical activity and/or healthy dietary behavior | Overall study results on the effectiveness of health promotion through the OHS are promising, especially with regard to interventions containing counseling to individuals with one or more CVD risk factors, either as single component or combined with an environmental component. The good-quality studies reported positive intervention effects on biological risk factors for CVD. |
| Mehta et al, 2013 (31) | N=5 (1 RCT, 4 pre-post designs) | Physical activity and healthy eating | Cohen’s d 0.09−0.603. Significant outcomes in all 5 interventions, 3 found significant outcomes in BMI, 3 in weight, 2 in waist circumference, and 1 in waist-to-hip ratio. |
| Montano et al, 2014 (20) | N=12 (RCT) | Cognitive behavioral, ergonomics, health education, health promotion, physical activity, stress management | SMD: BMI: -0.16 (95% CI -0.29− -0.02). Workplace interventions can have small, but positive effects on health outcomes. |
| Vuillemin et al, 2011 (33) | N=33 (RCT, controlled before and after, controlled non-RCT) | Workplace physical activity intervention in Europe aimed at primary prevention; 6 intervention categories: (i) counselling, (ii) exercise training, (iii) active commuting, (iv) walking interventions, (v) stair use, (vi) multicomponent interventions | No or inconclusive evidence for obesity-related outcomes for all physical activity intervention categories. Active commuting and exercise training appear as promising approaches to promote physical activity or fitness in the workplace. The effect of interventions on obesity-related outcomes remains to be further investigated. |
In conclusion, as the three high quality reviews all found consistently favorable effects of lifestyle interventions, there is strong evidence for a positive effect of workplace health promotion targeting physical activity and/or diet on weight-related outcomes.
Effect of interventions on remaining metabolic risk
All 5 reviews reporting on the evidence on metabolic risk factors were rated as of low quality (table 5). A variety of metabolic risk factors were studied, including lipid measures, glucose, and blood pressure. Each of the reviews summarized the evidence on multiple metabolic risk factors. For example, Conn et al (18) studied lipids measures and the risk for diabetes, the latter defined by fasting glucose and insulin levels. Also, Groeneveld et al (14) and Kwak et al (27) used various risk factors as outcome including lipids, blood pressure, and blood glucose. The promotion of healthy lifestyle behaviors (especially physical activity and healthy diet) was the main intervention component in 3 reviews (14, 18, 27). The remaining 2 (25, 26) evaluated more comprehensive approaches.
Table 5
Description of the reviews that studied the effect on remaining metabolic risk outcomes. [CI=confidence interval; CVD=cardiovascular disease.]
| Review | Number and type of studies | Type of intervention | Author’s conclusion |
|---|---|---|---|
| Conn et al, 2009 (18) | N=138 (studies with varied designs) | Interventions aimed to improve physical activity | Effect sizes: Diabetes risk (two-group post-test 0.57 (95% CI 0.06− 1.90); two-group pre-post 0.51 (95% CI 0.27− 0.53); treatment pre-post 0.47 (95% CI 0.38− 0.56). Lipids (two-group post-test 0.13 (95% CI 0.02− 0.24); two-group pre-post 0.17 (95% CI 0.01− 0.33); treatment pre-post 0.12 (95% CI 0.08− 0.17). Some interventions improve physical activity in some subjects, which in turn may improve selected health outcomes, but significant heterogeneity requires cautious interpretation of findings. |
| Groeneveld et al, 2010 (14) | N=31 (RCT); N=18 for blood pressure, N=21 for serum lipids, N=3 for blood glucose | Worksite lifestyle (physical activity and/or healthy diet) or health promotion interventions (such as individual counseling, group education, or self-help) | No evidence for an effect on blood pressure, serum lipid profile, blood glucose, and triglycerides. |
| Hafez et al, 2017 (25) | N=13 (2 RCT, 1 non-RCT, 1 cluster RCT, 3 single group time series, 2 single group pre-post, 1 multi-group pre-post, 3 cohort studies) | Evidence-based Diabetes Prevention Program (DPP) (N=10) or a non-DPP intervention (N=3) that aimed to prevent Type 2 diabetes (T2DM) | DDP: glycemic change: 2 studies showed improvement in HbA1c, 1 study improvement in fasting blood glucose, and 1 showed improvement in fasting blood glucose among women, but worsening among men. Non-DDP interventions: 2 studies found reduction in HbA1c at 12 months, 1 study found worsening fasting blood glucose at 2.5 years. Workplace interventions to prevent T2DM are most effective when they utilize the structured, evidence-based DPP curriculum with minimal modifications. |
| Kent Anger et al, 2015 (26) | N=17 (9 RCT, 7 quasi-experimental design, 1 multiple group nonexperimental design); N=3 with blood pressure as outcome, N=3 with cholesterol as outcome | Total worker health (TWH) interventions: both traditional occupational safety and/or health (OSH, health protection) and wellness and/or well-being (HP) should be addressed in the same intervention | Blood pressure, and cholesterol significantly changed in ≥ 3 TWH interventions. Systolic blood pressure reductions were reported ranging from -6 mm|Hg to -12.79 mm|Hg. Favorable changes in high density lipoprotein cholesterol and total cholesterol were reported based on 3 studies. Insufficient evidence to identify best practice interventions. All but one of the 17 TWH intervention programs improved outcomes that are risk factors for injuries and/or chronic diseases and 4 interventions improved ≥10. |
| Kwak et al, 2014 (27) | N=10 (RCT) | Interventions implemented by the occupational health services to promote physical activity and/or healthy dietary behavior | Overall study results on the effectiveness of health promotion through the OHS are promising, especially with regard to interventions containing counseling to individuals with one or more CVD risk factors, either as single component or combined with an environmental component. The good-quality studies reported positive intervention effects on biological risk factors for CVD. |
The reviews showed mixed findings with respect to the effect on metabolic risk. To illustrate, the systematic review of RCT of Groeneveld et al (14) concluded no evidence for a positive effect of workplace lifestyle interventions on blood pressure, serum lipid profile, blood glucose, and triglycerides, which was mainly due to inconsistencies between the study findings under review. In contrast, Kwak et al (27), who also studied RCT to the effect of interventions to promote healthy lifestyle behaviors, found that high quality studies reported favorable intervention effects on biological risk factors for cardiovascular diseases (CVD). Furthermore, based on the review of studies that evaluated total worker health interventions, Kent Anger et al (26) showed that all but one of the 17 interventions improved outcomes that are risk factors for injuries and/or chronic diseases. Still, they concluded insufficient evidence to identify best practice interventions.
In sum, because of the inconsistent conclusions of the low quality reviews, there is no evidence for a positive effect of health promotion interventions at the workplace on metabolic risk factors (except for weight-related outcomes).
Effect of workplace interventions on mental health
Table 6 describes the studies that examined the effectiveness of workplace interventions on mental health outcomes: 6 reviews (17–20, 22, 34) summarized the evidence with respect to the effectiveness of worksite health promotion interventions on mental health; 2 (17, 22) were of high quality. Mental health was mostly (5 out of 6 reviews) defined by measures including depression and anxiety; 1 review (20) studied the effect of workplace interventions on job stress.
Table 6
Description of the reviews that studied the effect on mental health outcomes. [CI=confidence interval.]
| Review | Number and type of studies | Type of intervention | Author’s conclusion |
|---|---|---|---|
| Carolan et al, 2017 (17) a | N=21 (RCT) | Digital mental health interventions: psychological interventions aimed at increasing psychological well-being (eg, by reducing symptoms of stress or depression) and delivered via the Internet, mobile technology, or a computer program. | Standardized mean difference (SMD) for psychological wellbeing: g=0.37, 95% CI 0.23− 0.50. Digital mental health interventions delivered in the workplace produced a small positive effect on psychological well-being. |
| Tan et al, 2014 (22) a | N=9 (RCT) | Interventions at the workplace aimed at universal prevention of depression. Most interventions used cognitive behavioral therapy (CBT) techniques. | The overall effect (SMD) was 0.16 (95% CI 0.07− 0.24) indicating a small positive effect. A separate analysis of interventions using CBT techniques yielded a significant SMD of 0.12 (95% CI 0.02− 0.22). Good quality evidence that universally delivered workplace mental health interventions can reduce the level of depression symptoms among workers; there is more evidence for the effect of CBT-based interventions than other interventions. |
| Chu et al, 2014 (34) | N=17 (RCT and quasi-experimental studies) | Interventions that involved evaluation of the effectiveness of physical activity interventions (ie, interventions could be supervised or non-supervised physical activity, exercise and yoga programs delivered either at the workplace or home based). | Two RCT of high quality assessed the effects of physical activity on depressive symptoms. One found that participants receiving an exercise training plus behavior modification program significantly reduced depression scores by −26% compared with participants who did not receive the program. The second RCT found an improvement in depression scores among participants who received the exercise training compared with the control group after the 10-week program, but the difference between the two groups was not significant There is moderate evidence for the effectiveness of physical activity interventions to improve depression. |
| Conn et al, 2009 (18) | N=138 (studies with varied designs) | Interventions aimed to improve physical activity. | Effect sizes (ES) : Mood two-group post-test 0.13 (95% CI -0.05− 0.31); two-group pre-post 0.21 (95% CI 0.07− 0.36); treatment pre-post 0.31 (95% CI 0.22− 0.40). Mean ES for mood (0.13) were positive, indicating better outcomes among treatment subjects, but these did not reach significance. |
| Martin et al, 2009 (19) | N=22; N=17 in meta-analysis (RCT, quasi-experimental studies, pre-post without control group) | Psychological interventions (utilized psychoeducation focused on cognitive behavior or training in coping skills within a stress management framework): directly targeting depression and anxiety symptoms, and health promotion interventions: indirectly targeting them via risk factors eg physical activity, poor work environment and cardiovascular disease. | SMD: depression: SMD 0.28, 95% CI 0.12− 0.44; anxiety: SMD 0.29, 95% CI 0.06− 0.51; Composite measures: SMD 0.05, 95% CI -0.03− 0.13. At follow-up 1 months to 3 years after baseline): depression: SMD 0.36, 95% CI 0.14− 0.58; anxiety: SMD 0.36, 95% CI -0.19− 0.90; Composite measures: SMD 0.36, 95% CI 0.07− 0.66. Small, but positive overall effects for symptoms of depression and anxiety but no effects for the composite outcome of the mental health measures. The interventions with a direct focus on mental health had a similar beneficial effect on symptoms as those with an indirect focus on risk factors. |
| Montano et al, 2014 (20) | N=7 (RCT) | Cognitive behavioral, ergonomics, health education, health promotion, physical activity, stress management. | Standardized mean differences (SMD): job stress: -0.37, 95%CI -0.71− -0.04. Workplace interventions can have small, but positive effects on health outcomes |
Consistent results were seen in 2 high quality reviews (17, 22), with both showing a small positive effect on mental health. Based on a meta-analysis of 21 RCT evaluating the effect of digital mental health interventions, Carolan et al (17) found a significant positive effect size for psychological wellbeing, including depression, stress and distress. Psychological interventions delivered through the internet, mobile technology, or computer, were found to be effective on mental health among a diverse worker population. The second high quality review also concluded a small and positive effect of workplace interventions aimed at the prevention of depression with more pronounced effects of interventions that used cognitive behavioral therapy techniques than other interventions (22).
There were 2 (18, 34) low quality reviews that evaluated the effect of workplace physical activity interventions on mental health. Chu et al (34) concluded moderate evidence for the effect of physical activity interventions on depressive symptoms. In addition, Conn et al (18) found positive effect sizes, though not statistically significant, indicating better mental health outcomes for those receiving physical activity interventions. The remaining 2 low quality reviews (19, 20) included a diverse set of interventions including cognitive behavioral, ergonomics, health education, health promotion, physical activity, and stress management. Both reviews reported overall positive, but small effects on depression and anxiety (19) and job stress (20).
In sum, based on the high quality reviews, there is strong evidence that workplace psychological interventions, especially those that use e-health and cognitive behavior techniques yield positive effects.
Effect of interventions on musculoskeletal disorders
The evidence with respect to the effectiveness of worksite health promotion interventions on musculoskeletal disorders was summarized in 6 reviews (20, 23, 35–38), of which 4 were of high quality (23, 35, 36, 38) (table 7). Most reviews used a general musculoskeletal health measure as outcome (eg, musculoskeletal disorders, symptoms, or health), while 2 (23, 37) used a specific musculoskeletal health outcome. Namely, Verbeek et al (23) studied the effect on (incidence, duration, frequency of intensity of) back pain, and Van Eerd et al (37) evaluated the effect of workplace interventions on upper-extremity disorders and symptoms.
Table 7
Description of the reviews that studied the effect on musculoskeletal health outcomes. [OR=odds ratio; RR=risk ratio; CI=confidence interval.]
| Review | Number and type of studies | Type of intervention | Author’s conclusion |
|---|---|---|---|
| Krungkraipetch et al, 2012 (35) a | N=8 (2 RCT, 3 quasi experimental studies, 2 cohort studies, 1 case study with pre-post evaluation) | Interventions targeted biomechanical exposure in the workplace or the organization of work and included health beliefs and attitudes of workers. Three types of interventions: (i) mechanical exposure interventions, (ii) production systems/ organizational culture interventions and (ii) modifier intervention. | Very limited evidence to support the use of three types of interventions, mechanical exposure, production systems/organizational culture and modifier interventions for reducing the incidence, prevalence and intensity of musculoskeletal disorders and to reduce risk factors among informal sector workers. |
| Tullar et al, 2010 (36) a | N=40 (RCT or non-RCT with a control group; N=16 were of medium or high quality and included in best evidence synthesis) | Occupational safety and health interventions in health care settings; primary and secondary prevention interventions conducted at the workplace. Most interventions were multi-component interventions (3 of 16) and exercise interventions (5 of 16) | A moderate level of evidence for a positive effect on improving musculoskeletal health was found for multicomponent patient handling interventions and for exercise programs. |
| Van Niekerk et al, 2012 (38) a | N=5 (3 RCT, 1 pre-post study, 1 single case study) | Chair interventions, chair modifications. Most common feature was an adjustable sea or back height, and the training in the use of the chair i.e. how to adjust appropriately. | A consistent trend that supports the role of a chair intervention to reduce musculoskeletal symptoms among workers who are required to sit for prolonged periods. However, the amount and level of quality of evidence was moderate thus not making strong recommendations. |
| Verbeek et al, 2011 (23) a | N=18 (9 RCT and 9 cohort studies) | Professional education, video, use of back belt, exercise, and occupational training plus lifting aids | Moderate quality evidence from 7 RCT that those who received training reported levels of back pain similar to those with no intervention, with an OR of 1.17 (95% CI 0.68− 2.02) or minor advice (video) with a RR of 0.93 (95% CI 0.69− 1.25). Results of the cohort studies were similar to those of the RCT. |
| Montano et al, 2014 (20) | N=12 (RCT) | Cognitive behavioral, ergonomics, health education, health promotion, physical activity, stress management | Workplace interventions can have small, but positive effects on health outcomes. Standardized mean difference (SMD) for MSD: -0.32, 95% CI -0.51− -0.14. |
| Van Eerd et al, 2016 (37) | N=61 (26 medium or high quality RCT, non-RCT with a control group + 35 from an earlier review) | 30 different workplace interventions for preventing and managing upper MSD | Implementing a workplace based resistance training exercise program, policy or practice can help manage and prevent upper MSD. Strong evidence for 1 intervention category: resistance exercise training; moderate evidence for stretching programs, mouse use feedback and forearm supports. Moderate evidence for no benefit for EMG biofeedback, job stress management training and office workstation adjustment. |
A similar overall conclusion was reached in 3 (35, 36, 38) of the high quality reviews in that they found limited to moderate evidence for a positive effect of the workplace interventions under review. Based on 16 medium or high quality RCT or non-RCT with a control group, Tullar et al (36) concluded moderate evidence for a broad range of occupational safety and health primary and secondary prevention interventions on musculoskeletal symptoms in healthcare workers. Krungkraipetch et al (35) backed this finding, concluding limited evidence to support the use of three types of interventions to reduce musculoskeletal disorders. The interventions in that review were mostly multi-component or exercise interventions. Furthermore, although all five studies included in the review of Van Niekerk et al (38) found a reduction in self-reported musculoskeletal pain in desk workers, the amount and level of quality of evidence was moderate. The fourth high quality review (23) concluded that training proper manual handling techniques or assistive devices are not effective to prevent back pain in those who have manual handling to the extent that it increases their risk for back pain.
The remaining reviews that were considered of low quality (20, 37) had inconsistent results to some extent. While Montano et al (20) showed a positive, but small effect of various workplace interventions on musculoskeletal health, Van Eerd et al (37) found strong evidence for one intervention type on upper-extremity disorders, ie, resistance exercise training. Based on a total of 61 RCT and non-RCT with a control group, Van Eerd et al concluded moderate evidence for stretching programs, mouse use feedback, and forearm supports. In contrast, some other interventions were not supported, with moderate evidence for no benefit of electromyography biofeedback, job stress management training and office workstation adjustments.
To conclude, as 75% of the high quality reviews found some evidence for positive effects, there is strong evidence for the support of workplace interventions to the prevention of musculoskeletal disorders. An exception was the training of proper manual handling techniques or the use of assistive devices, which seemed not effective in the prevention of back pain. Table 8 summarizes the conclusions with respect to the levels of evidence per outcome measure.
Table 8
Levels of evidence for workplace health promotion interventions per outcome.
| Outcome | Low/high quality reviews (N) | Level of evidence meta-review a | Comment |
|---|---|---|---|
| Weight-related | 11/3 | *** | 3 high quality studies concluded positive, though small effects. |
| Metabolic risk | 5/0 | 0 | 0 high quality reviews, inconsistent conclusions of low quality reviews. |
| Mental health | 4/2 | *** | 2 high quality reviews concluded small positive effects for e-health and interventions using CBT techniques. |
| Musculoskeletal health | 2/4 | *** | 3 high quality reviews concluded positive effects of workplace interventions; 1 high quality review concluded no effect of training proper manual handling techniques or assistive devices. |
*** Strong evidence: >1 high-quality reviews with consistent outcomes; **Moderate evidence: 1 high-quality and ≥1 low-quality reviews with consistent outcomes; *Limited evidence: only 1 high-quality, or >1 low-quality reviews, all with consistent outcomes; 0 No evidence: only 1 low-quality review, or inconsistent results of the reviews.
Discussion
This systematic review aimed to summarize the evidence from reviews on the effectiveness of health promotion interventions at the workplace on various physical and mental health outcomes that are related to (the prevention of) chronic diseases, ie, cardiometabolic risk factors as predictors for T2DM and CVD, mental health, and musculoskeletal disorders. We found strong evidence for positive effects of such workplace initiatives on weight-related outcomes, mental health, and musculoskeletal health. The evidence for an effect of workplace interventions on cardiometabolic risk factors, except for weight-related measures, was inconsistent.
The main strengths of this review are the use of meta-review methodology, which enabled coverage of very broad range of health outcomes, the comprehensive search strategy and the quality assessment of each review by two independent researchers. However, the results should be interpreted in the light of some limitations. For study quality, we calculated an overall AMSTAR score and used an arbitrary cut-off (ie, 50%) to distinguish low and high quality reviews. Both approaches are discussed in the literature, since the calculation of an overall quality score assumes that all questions are of equal importance and different cut-offs exist (39, 40). Both other cut-off points to define reviews of high quality as well as a three category approach (with low, moderate, and high quality) have been used to distinguish between reviews of higher or lower quality (39). However, meta-reviews that applied a three category approach often merged findings from moderate and high quality studies in the same category for an evidence synthesis (16). Therefore, and following previously published reviews (14, 15), we decided to use a dichotomy and a cut-off of 50%. If we would have used a higher cut-off point, for example of 75%, as has been done in other reviews [eg, (41)], there would only be one high quality review (21), logically yielding lower evidence conclusions.
As this review found strong evidence for an effect on weight-related outcomes, but not for other cardiometabolic risk factors, it is unknown whether workplace health promotion in the long-term may lead to a reduced incidence of CVD and T2DM. Inconsistencies in the results of multiple reviews hamper decision makers or other stakeholders involved in the prevention of chronic diseases to implement evidence-based interventions (42). This meta-review shows that for weight-related outcomes, mental disorders and musculoskeletal problems consistent positive effects were found of workplace health promotion. Most of the original systematic reviews in this meta-review included a range of very different interventions, which is an important limitation of this review. The studies included not only showed a large heterogeneity in the interventions but also in the outcomes under study. For example, for mental health disorders, the outcomes included depressive symptoms, anxiety, psychological wellbeing, mood, and job stress. The various outcomes may imply different intervention strategies to be effective. This may explain the heterogeneity of the interventions, where those targeting mental health included e-health, cognitive behavioral therapy (CBT) techniques, individual and group-based physical activity interventions, stress management and training in coping skills (17–20, 22, 34). Wherever possible, we indicated the specific interventions for which effectiveness was concluded. For the prevention of mental disorders, these were cognitive behavioral intervention and e-health. Although CBT is particularly applied to patients, these techniques were included in workplace health promotion interventions to target behavioral changes to promote (mental) health (22). CBT intervention has shown to be effective in the prevention and reduction of anxiety problems (25). From this preventive perspective and the focus on behavioral change to promote health, we considered this type of intervention eligible in this review. In general, other reviews on health promotion in the workplace conclude that comprehensive multimodal interventions, including different intervention components, are more effective in the prevention of chronic disease compared to single component interventions (43–45). With respect to a broad implementation of multimodal interventions it is not clear which components in what dose or frequency should be applied and recommendations for employers are therefore not easy to formulate. Another important challenge for employers who intend to prevent chronic diseases is the implementation of health promotion interventions. As a precondition for a successful implementation, it is advised to assess the needs and possibilities at different levels (44, 46). To take a next step and support employers with a practical toolkit for implementing workplace health promotion to prevent overweight, mental and musculoskeletal disorders, more insight in facilitating factors and barriers for the implementation of worksite health promotion interventions is needed.