Carpal tunnel syndrome (CTS) is a common peripheral nerve entrapment disorder (1) and recommended treatment includes carpal tunnel release surgery (CTR) (2, 3). CTR has become a common elective operation, with more than 77 000 CTR procedures expected to be performed annually in the English National Health Service (NHS) alone by 2020 (4). Despite CTR being such a frequently performed procedure, there is currently no evidence-based guidance to inform patients and clinicians about when it is safe to return to work, or other activities, after their surgery. Extended work absence after CTR may have financial consequences for both the worker and employer, whereas returning to work too soon after surgery could be associated with reduced work performance, increased workplace risk due to altered grip and dexterity, or clinical complications.
Whilst there have been previous systematic reviews which included return-to-work (RTW) time after CTR as a measure of the effectiveness of different CTR interventions (5–9), these reviews have not explored the variation caused by occupational factors, such as the type of work, work pattern or whether participants were employed or self-employed. Moreover, RTW may be defined in a number of ways and can include: return to (i) full duties, (ii) amended duties, or (iii) modified working hours. To our knowledge, none of the existing reviews has considered this diversity. We therefore undertook a systematic review of the literature to address the following question: when do patients return to work after CTR, and how do occupational factors influence this timing?
Methods
The review protocol was pre-registered with PROSPERO (registration number: CRD42016034158) (10) and carried out according to the PRISMA guidelines (11).
Selection criteria
Eligible studies were those reporting post-operative RTW time after CTR, using any surgical technique, in a working population. Randomized controlled trials (RCT), cohort studies and case–control studies were eligible for inclusion (table 1).
Table 1
Review eligibility criteria. [CTR=carpal tunnel release.]
Search strategy
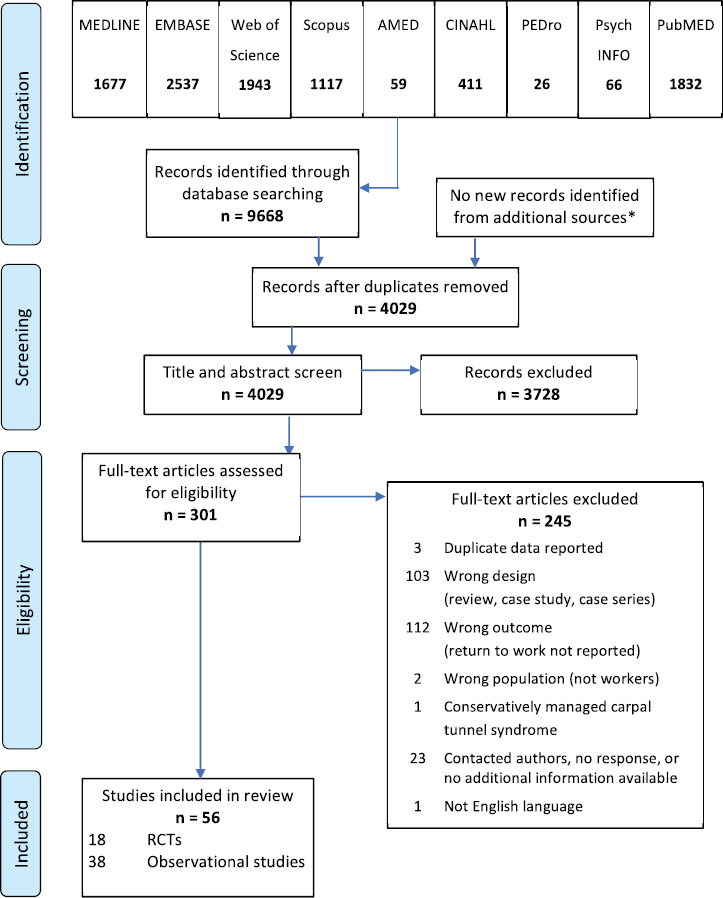
The first author searched 24 electronic sources between February and March 2016. These comprised electronic databases, trials registries, grey literature sources and the electronic records of four relevant journals (figure 1). There were no restrictions for country of origin or date of publication, but due to time and resource limitations, studies were restricted to those available in the English language. The example search strategy for Medline is provided in appendix A (http://www.sjweh.fi/show_abstract.php?abstract_id=3762).
Figure 1
Systematic review flow diagram. Additional sources comprised: (1) trial registries (Cochrane Central Register of Controlled Trials; ClinicalTrials.gov; EU Clinical Trials Register; Alltrials.net; WHO International Clinical Trials Registry; NIHR UK Clinical Trials Gateway); (2) grey literature databases (e-theses Online Service; OpenThesis; ProQuest; OpenGrey; OpenDOAR); and (3) key journals (J Hand Surg - European; J Hand Surg - US; Occup Med; J Occup Rehab).
Eligibility assessment
Two reviewers independently performed title and abstract screening using the Covidence web platform (www.covidence.org). Any disagreements were discussed and taken to an additional independent reviewer if agreement was not reached. All reviewers agreed the final decision. Full text was retrieved for those articles selected from this initial screen and in cases where no abstract had been found. Full text screening was performed according to the review inclusion and exclusion criteria (table 1), following the same process as above.
Data extraction
For the included studies, two reviewers independently performed data extraction using pre-piloted data extraction forms (appendix B, (www.sjweh.fi/show_abstract.php?abstract_id=3762). Data extraction included year of publication, country of research, study population, study design, CTR surgical technique, information about workers’ compensation (or other insurance) status, post-operative management and measurement of RTW time. Where clarification or additional information were required, the first author contacted the relevant author by email.
Methodological assessment
Two reviewers independently assessed study risk of bias using the Cochrane Collaboration’s tool for assessing risk of bias in randomized trials and a modified version of the tool for non-randomized trials (12, 13). The items included in the risk of bias assessment are shown in appendix C (www.sjweh.fi/show_abstract.php?abstract_id=3762). For each item, RCT were rated as low, unclear or high risk of bias and observational studies were rated as low, moderate, serious or critical risk of bias. When there was insufficient information to make a firm judgment about the risk of bias for an individual item, the rating “no information” was used. Summary scores for observational studies were derived from the lowest score (highest risk of bias) for any single item (13). For RCT, the absence of patient blinding was excluded from the summary score because of the difficulties with blinding patients in surgical trials. Studies were rated at low risk of bias if rated low for all remaining domains; high risk of bias if rated high for two additional domains; and unclear for other scoring patterns. Following a pilot, the papers were reviewed independently and any differences in scoring were resolved and agreed by discussion.
Data synthesis
RTW data were reported in two ways: (i) the average time period from CTR to RTW; or (ii) the proportion of individuals who had returned by specified time points. The duration until RTW was reported using a mixture of days, weeks and months. To enable direct comparison within the review, all durations have been reported in days. The basis of the conversion was that one week was equal to 7 days and one month equaled 30 days. In the absence of explicit information, an assumption was made that the reported RTW times included all 7 days of a calendar week, regardless of the participants’ usual working pattern. Heterogeneity in both study methods and populations limited the review to a narrative analysis with summary descriptive statistics. Duration before RTW was summarized using the median and range. For each summary calculation, the number of studies and observations (study arms) that provided these data were documented. Due to inconsistent reporting of the number of workers in the included studies, summary data was not weighted for sample size.
Results
Study characteristics
Results for each stage of the literature search and reasons for exclusion are shown in figure 1. A total of 4029 individual records were identified, of which 56 met the review inclusion criteria; 18 RCT and 38 observational studies. Twenty-four authors were contacted for additional information, with only one providing clarification that enabled the study to be included (14). We found that two papers reported on the same study participants (15, 16), but as different RTW analyses were undertaken, both have been included in this review. Participant numbers and demographics were only counted once for these reports. The included research took place in 16 countries, primarily in North America and Europe, with three studies in Asia and one in Israel. Publication dates ranged from 1992–2016.
Participants
The 56 included studies comprised 14 335 CTR patients (1551 from RCT, 7328 from cohort studies and 5456 from a single case control study). Of these, 7 studies did not report the age of participants (14, 17–22) and 7 did not report the sex (18–21, 23–25). The mean age of CTR participants in the RCT ranged between 44–60 years, compared with 37–66 years in the cohort studies. The male/female ratio of participants was 1:2.4 for RCT and cohort studies and 1:3 for the case–control study. Study characteristics and reported duration until RTW are shown in appendix D (www.sjweh.fi/show_abstract.php?abstract_id=3762).
We found that study inclusion and exclusion criteria varied widely between studies. For example, there were no consistently reported methods of CTS diagnosis. Furthermore, 6 studies included only unilateral CTS (26–31), 7 included only bilateral CTS (32–38); 29 included individuals undergoing either unilateral or bilateral CTR (16, 20–25, 39–60), and 14 did not report whether participants had unilateral or bilateral CTS or CTR (14, 17–19, 48, 61–69).
Duration until RTW was reported by all included studies, however 6 RCT (18, 32, 40, 42, 45, 63) and 7 cohort studies (37, 38, 52, 54–56, 60) did not specify the number of individuals included in their RTW analyses. With the pragmatic assumption that, where unreported, all participants provided RTW data, this yielded a total of 1263 workers from RCT, 7071 from cohort studies and 1529 from 1 case–control study.
Methodological assessment
The risk of bias assessments are summarized in appendix C. Overall, only 4 studies were rated at low risk of bias: 1 RCT (27), 2 cohort studies (48, 69) and 1 case–control study (14). This compared with 27 studies rated at moderate or unclear risk of bias and 25 studies rated at high, serious or critical risk of bias. Common concerns centered on the assessment and reporting of RTW data, issues with the selection of participants for observational studies, and the lack of assessor blinding for RTW data in RCT.
Measurement of return to work timescales
There was no common method of defining or collecting RTW data. Only 36 studies (64%) reported any information on how the period of post-operative work absence was calculated. Of these, three non-hierarchical categories were identified based on the method of RTW data collection: (i) regional/national databases (14, 27, 31); (ii) patient reported questionnaires or telephone interviews (15–17, 22, 25, 29, 37, 40, 42, 48–50, 52, 60, 68); and (iii) medical records. For the latter, RTW information was either recorded during clinical assessment (18, 20, 30, 35, 39, 44, 47, 51, 53, 63, 69) or was extracted retrospectively from the records (24, 38, 54, 56–58, 65).
Return to work timescales
Figure 2 shows the average time to RTW for the included studies. Only 19 studies summarized RTW time as a median. Median RTW time in these studies ranged from 7–60 days with an overall median of 28 days. Mean RTW times were reported in 41 studies, ranging from 4–168 days, with the overall median of 30 days (table 2). Of the 56 included studies, only 8 reported median RTW time and range or interquartile range (14, 27, 32, 35, 42, 46, 48, 55), while 24 studies provided a single point estimate with no measure of the spread of the data. Table 2 summarizes the reported duration to RTW according to different study characteristics: study type, CTR procedure, sample size, RTW data collection method, study location and risk of bias score. Details from the individual studies, including characteristics and reported RTW times are provided in appendix D.
Figure 2
Reported return to work times following carpal tunnel release according to surgical procedure, point estimate (median/mean) and study risk of bias. Symbol size represents the number of study participants per study arm (range 3–1410).
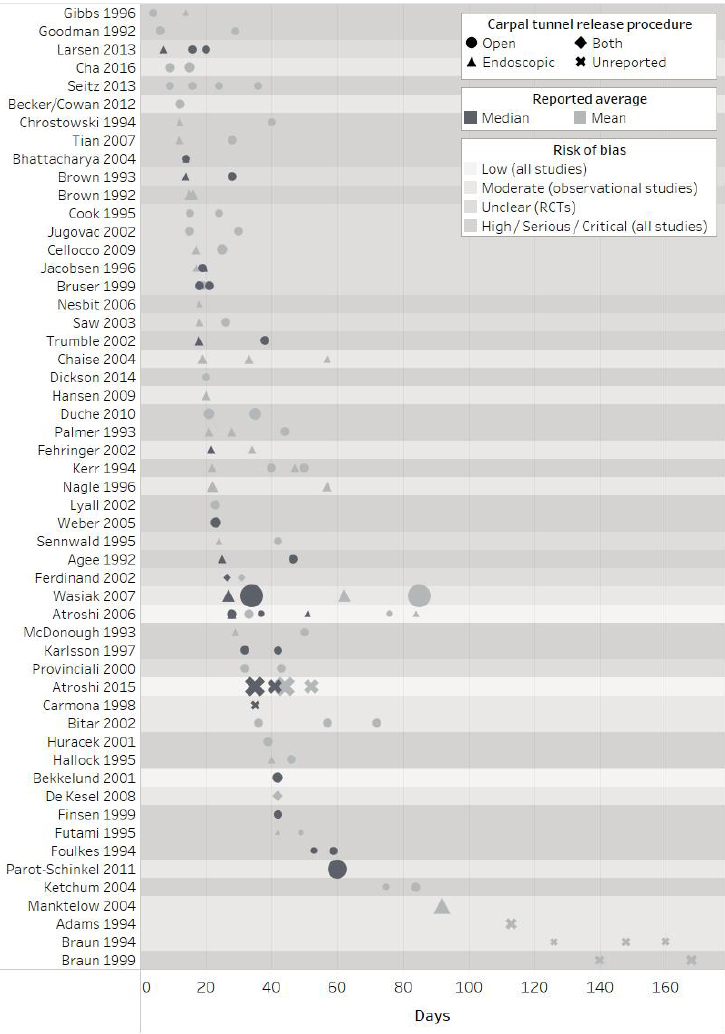
Table 2
Summary of reported return to work times according to methodological characteristics. [CTR=carpal tunnel release
| Subgroup | Studies | Observations a | Return to work time reported as median (days) | Studies | Observations a | Return to work time reported as mean (days) | ||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Median | Range | Median | Range | |||||
| All studies | 19 | 35 | 28 | 7–60 | 41 | 81 | 30 | 4–168 |
| Study | ||||||||
| Randomized controlled trials | 11 | 24 | 26 | 7–59 | 11 | 23 | 25 | 12–84 |
| Observational study | 8 | 11 | 35 | 21.5–60 | 30 | 58 | 36 | 4–168 |
| CTR procedure | ||||||||
| Open CTR | 15 | 21 | 34 | 14–60 | 29 | 44 | 29.5 | 4–85 |
| Endoscopic CTR | 9 | 10 | 18.75 | 7–51 | 21 | 28 | 22 | 12–92 |
| Procedure not reported | 3 | 4 | 35 | 26.5–41 | 6 | 10 | 119.5 | 31–168 |
| Sample size (number of workers) | ||||||||
| <30 | 7 | 14 | 23.25 | 7–59 | 17 | 28 | 29 | 4–126 |
| 30–100 | 9 | 15 | 28 | 14–46.5 | 24 | 40 | 31 | 6–168 |
| >100 | 4 | 6 | 38 | 27–60 | 9 | 13 | 44 | 15–140 |
| Source of return to work data | ||||||||
| Regional or national databases | 3 | 8 | 34.5 | 27–51 | 3 | 8 | 57 | 28–85 |
| Questionnaires or interviews | 4 | 5 | 53 | 35–60 | 9 | 14 | 23 | 4–92 |
| Medical records | 3 | 4 | 22.25 | 14–28 | 15 | 32 | 36 | 6–160 |
| Not reported | 7 | 14 | 23 | 14–46.5 | 14 | 27 | 22 | 6–168 |
| Location | ||||||||
| Scandinavia | 8 | 18 | 30 | 7–51 | 5 | 10 | 34.5 | 17–84 |
| Europe (excluding Scandinavia) | 4 | 6 | 19.5 | 14–60 | 12 | 21 | 26 | 15–57 |
| North America | 8 | 13 | 28 | 13–59 | 22 | 44 | 37 | 4–168 |
| Other | · | · | · | ·· | 3 | 6 | 21.5 | 9–49 |
| Risk of bias | ||||||||
| Low (all studies) | 3 | 7 | 37 | 28–51 | 2 | 6 | 48 | 28–84 |
| Moderate (observational studies) | 4 | 5 | 34 | 13–60 | 12 | 21 | 57 | 9–160 |
| Unclear (randomised controlled trials) | 5 | 10 | 19.25 | 7–28 | 9 | 17 | 24 | 15–43 |
| High/serious/critical (all studies) | 7 | 13 | 38 | 14–59 | 18 | 37 | 29 | 4–168 |
Duration of work absence did not appear to increase or decrease consistently according to the hierarchy of risk of bias categories. Interestingly, the 11 RCT rated at unclear risk of bias generally reported faster RTW times and showed less variability than the studies in other risk of bias categories (table 2). RTW times varied when classified according to the method of data collection; median RTW times obtained from medical records tended to be earlier than those reported in databases or collected by interviews or questionnaires. In contrast, mean RTW times reported by interview/questionnaire were earlier than those recorded by the other methods (table 2). We found no apparent relationship between reported RTW time and year of publication.
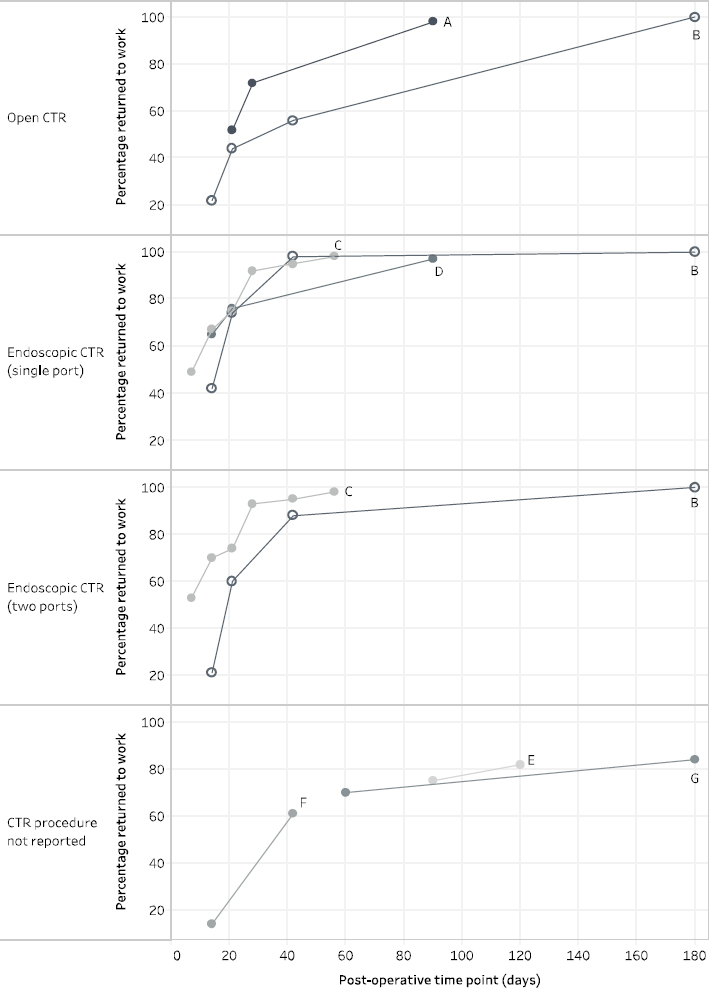
Return to work rates
The percentage of participants who had returned to work by different post-operative time points was reported in 7 cohort studies; however, there was minimal overlap in the timing of data collection for each study (17, 19, 29, 47, 49, 60, 69). The reported time points for at least 50% of study participants to return to work ranged from 7–42 days (figure 3). Only one study recorded 100% RTW and this had occurred by 180 days (6 months) (60).
Occupational information
Table 3 shows the summary RTW times for studies reporting occupational information. Of the 56 studies, 6 reported RTW times for different job types (16, 27, 34, 50, 59, 67), and 4 distinguished between return to modified duties and return to full duties (15, 18, 35, 57). Neither the method of classifying occupation nor the description of what constituted modified or full duties, were consistent across studies. For the purposes of this review, we classified desk-based, sedentary, white-collar or light work as “non-manual”; and light-repetitive, medium, heavy or blue-collar work as “manual”. We also defined a subgroup of “heavy manual” workers which consisted of heavy manual and blue-collar work. Return to light duties, one-handed activity, and light two-handed activity were classified as “modified duties”; return to normal or full duties were classified as “full duties”.
Table 3
Summary return to work (RTW) times according to reported occupational characteristics.
| Subgroup | Studies | Observations a | RTW time reported as median (days) | Studies | Observations a | RTW time reported as mean (days) | ||
|---|---|---|---|---|---|---|---|---|
| Median | Range | Median | Range | |||||
| Work duties | ||||||||
| Modified duties | 1 | 1 | 13 | ·· | 4 | 6 | 20.5 | 12–50 |
| Full duties | 1 | 1 | 63 | ·· | 4 | 5 | 27 | 17–82 |
| Work type | ||||||||
| Non-manual | 1 | 1 | 21 | ·· | 6 | 11 | 21 | 7–49 |
| Manual | 1 | 1 | 36 | ·· | 6 | 14 | 39 | 18–101 |
| Heavy manual | 1 | 1 | 36 | ·· | 3 | 4 | 46.5 | 22–101 |
| Employer | ||||||||
| Employed | · | · | · | ·· | 2 | 3 | 36 | 33–57 |
| Self-employed | · | · | · | ·· | 2 | 2 | 21 | 19–23 |
| Working pattern | ||||||||
| Part-time | · | · | · | ·· | 1 | 2 | 24.5 | 15–34 |
| Full-time | · | · | · | ·· | 1 | 2 | 12 | 10–14 |
| Workers’ compensation status | ||||||||
| Workers’ compensation | 4 | 6 | 56.5 | 27–114 | 16 | 29 | 56 | 23–160 |
| No workers’ compensation | 3 | 5 | 19 | 15–45.5 | 12 | 20 | 18.5 | 3–57 |
| Other health insurance b | 4 | 11 | 35 | 7-51 | 7 | 14 | 35 | 17–84 |
Only Gimeno et al (69) reported return to work rates for different levels of work functioning. They reported that by two months after surgery, 41% of study participants reported working normally, while 28% had work limitations. By six months, this had improved to 58% and 26%, respectively. At both time points, the remainder of participants had yet to return to work. Only one study reported RTW time separately for full- and part-time work (16) and two studies reported RTW times separately for self-employed and employed participants (50, 67).
Participants receiving workers’ compensation took longer to return to work in all studies reporting and comparing insurance types (23, 30, 35, 56, 59, 60, 65, 67). Where other insurance types were stated, such as national insurance schemes or private insurance, mean RTW times tended to be shorter than among those receiving workers’ compensation (67, 56).
Earlier RTW was found in: non-manual workers; those able to return to modified duties; full-time workers; individuals who were self-employed; and those not receiving workers’ compensation.
Return to work advice
Few studies reported that patients received any standardized RTW advice. Four studies recommended returning to work as soon as possible (15, 16, 43, 60); others advised patients to return when able (26, 44) or after suture removal (39). Three studies reported that the surgeon was responsible for suggesting a RTW time (17, 21, 66); one study reported that this was the role of the general practitioner (29); one study reported a combined decision between the surgeon and therapist (57); and two studies reported a combined decision between surgeon and patient (18, 41).
Discussion
This review systematically identified 56 studies reporting RTW timescales following CTR and compared their findings according to different occupational, clinical and study characteristics. Overall, our review points to substantial heterogeneity in the duration of work absence after CTR. Mean RTW times ranged from 4–168 days in 41 studies; median RTW times ranged from 14–60 days in 17 studies. Earlier RTW was reported following endoscopic CTR and in populations without workers’ compensation, findings that are consistent with those of previous systematic reviews (5–9, 70). We also found that return to modified duties occurred sooner than return to full duties and return to non-manual occupations were generally faster than return to manual roles. Where studies categorized the type of work, heavy manual work was associated with the longest period of work absence. This finding is supported by a recent review of the prognostic factors for RTW after CTR, which found that exposure to bending/twisting the hands at work, repetitive activities, heavy lifting and blue-collar work were all associated with delayed RTW (71).
Given that these findings might be expected, it was surprising how few studies adequately reported work-related information, such as occupation, working pattern (full-time or part-time), employment status (employed or self-employed) and availability of paid sick-leave. Only 36 studies gave a definition of RTW or described their method of collecting RTW data. Where this was defined, 50% used the participants’ medical records as their data source. Our observed lack of reporting of work-related information in the included studies may therefore be explained, in part, by an absence of routine collection, or recording, of work-related information in clinical practice.
Two studies reported RTW data for employed and self-employed individuals, and both found that those who were self-employed returned to work sooner than salaried workers (50, 67). A further two studies deliberately excluded self-employed individuals from their RTW analyses (24, 44), the assumption being that the RTW process would be notably different for these individuals. However, a recent systematic review of RTW after hip and knee arthroplasty found no difference in RTW times for employed and self-employed workers, although only 2 of the 19 included studies reported relevant data (72). The role of the type of work contract (permanent, fixed term, zero hours or self-employed) on RTW after elective surgery remains unclear and requires further examination in CTR populations, taking into account issues such as job security and sick-leave entitlement.
We only found one study that specifically compared individuals in full-time work with those working part-time (16). The authors reported shorter periods of post-operative sick-leave among full-time workers, however, it is unclear whether all calendar days, or just those where the participant would usually be working, were included in this estimation.
Interestingly, we found that studies with large sample sizes (>100 workers per study arm) tended to report longer RTW times than medium-sized (30–100 workers) or small studies (<30 workers). One explanation for this finding is the left-censoring of data in at least one of the large studies. Atroshi et al (14) explicitly stated that their RTW data were obtained from a national database that registered work absences >14 days. Therefore, any individuals who returned to work within 14 days of their CTR would be omitted from this study. If every CTR patient had been included, the median time to RTW would be shorter. We could not ascertain whether a similar convention was adopted in the large study by Wasiak & Pransky (31), who also obtained RTW information from regional/national databases. Importantly, when the results were further examined, there was no clear association between RTW times and the method of obtaining RTW data. Moreover, we found no clear relationship between reported RTW times and risk of bias scoring.
Advice provided by healthcare professionals, particularly the surgeon, may be an important determinant of RTW time. Ratzon et al (17) found that surgeon’s advice was a strong predictor of RTW times among their cohort. However, we were unable to explore the role of advice in the current review because so few studies specified what advice had been given and by whom.
The eligibility criteria for our review were deliberately broad to reflect the patients and CTR procedures seen in clinical practice. All studies purported to measure RTW duration after CTR, but key information, such as the definition of RTW, the method of assessment and the number of workers contributing data were frequently unreported. As a result, we provided descriptive summaries of the reported RTW times as the median and range. It is a limitation of the current review that we were unable to pool data for a formal meta-analysis with a sample size weighting.
In order to present the data consistently, all RTW durations were reported in days. In some cases, this involved a conversion from weeks or months to days, which may not truly reflect the timescales collected in the original dataset. It is also possible that some authors calculated RTW duration based on a 5-day working week, although this was not specified.
Time to RTW would not be expected to show a normal distribution because the presence of a few individuals who take much longer to RTW will cause a positive skew to the data. For this reason, summarizing RTW duration as the mean has the potential to inflate the point estimate, as seen in four of the five studies that reported both mean and median (14, 27, 31, 35). At the most extreme, the study by Wasiak & Pransky (31) reported a mean RTW time after open CTR of 85 days as compared with a median of 34 days (31). This bias has obvious implications when interpreting the findings of our review and for patients wishing to know the usual period of time it takes for someone to return to an occupation that is similar to their own. To generate more useful clinical information, future research should report RTW times as the median and range to better enable comparison between studies. Only eight of the studies in our review reported their data in this way and therefore consideration needs to be given to the probable positive skew of the studies which reported only mean RTW time, and the associated consequences of this on the summary data presented in this review.
Despite the weaknesses identified in many of the included studies, our review adds to the existing CTR literature by demonstrating a wide range of RTW times across a large number of international studies using different methodological approaches. Previous reviews have been restricted to either the smaller number of published RCT that were designed to assess the clinical effectiveness of different interventions (5–9); or to studies of prognostic factors for RTW without an assessment of the duration of work absence (71).
Inconsistencies in the definition and measurement of time to RTW in CTR settings have been previously discussed (73). The authors called for standardized assessment of RTW, measured in days, and including information on type of work, insurance status and rehabilitation. The results of the current review show that this information is still not consistently reported and clear standards for the measurement and reporting of work-related outcomes in clinical studies need to be defined. In particular, we would argue for a clear statement of the number of workers in the study sample; provision of summary data on the spread of RTW times, rather than just a point estimate; documentation of the number of workers who had not returned to work by the end of the study period; capturing any subsequent, related periods of sick leave; and making a clear distinction between return to paid work and return to other activities. There is also a need to establish a definition for the assessment of return to modified and full work duties and a standardized categorization of occupational roles. In the current review, only six studies provided information on RTW times for different types of occupation, but the classifications varied so widely that it was only feasible to group into discrete “manual” and “non-manual” categories for purposes of the review summary. As a result, the studies provide only limited information for clinicians to draw upon in advising individual patients of how long it might take to return to specific work roles.
We purposefully included research conducted in any country and acknowledge the potential issues associated with the comparison of findings from different cultural, social, welfare and healthcare backgrounds. In fact, the majority of included studies were conducted in the USA and the results were spread across the range of reported RTW durations, including both the shortest and longest periods of work absence. Scandinavian studies reported longer RTW times than those conducted in other parts of Europe. This finding might also be partly explained by the left-censoring of RTW data captured from national databases, as discussed above. One study included in this review specifically compared RTW times across two different geographical settings. Bitar et al (65) retrospectively assessed post-operative work absence among 81 female workers from USA (34 with workers’ compensation, 47 without) and 42 female workers from Sweden. Both groups from the USA took longer to return to work than the Swedish cohort. The availability of compensation or other paid sick leave is an important determinant of duration to RTW, however the influences of additional cultural and contextual factors on post-operative RTW timescales warrant further exploration.
The key factors underpinning the wide variation in reported RTW times remain unclear, largely due to the heterogeneity of the available studies and incomplete reporting. The findings of our review support the call for greater clarity in the reporting of work-related outcomes in relevant studies. RTW time needs to be measured consistently and include a description of influential factors, such as: type of occupation and employment status, RTW advice and return to modified or full duties. However, despite the limitations of the available studies, our findings suggest that occupational factors play an important role in RTW after CTR. The identified literature suggests longer periods of work absence among those who: were employed (rather than self-employed), worked part-time (rather than full-time), worked in heavy manual occupations, or were required to return to full (rather than amended) duties. Further research is required to determine whether earlier RTW is appropriate for these groups, and if so, to determine the safest recommended timescales.