The individual suffering and economic consequences of long-term sickness absence related to musculoskeletal pain and low-back injuries are a substantial problem in the healthcare sector, both for healthcare employees, workplaces, and society (1–3). The annual prevalence of musculoskeletal disorders (MSD) range from 44–84% across countries and healthcare sectors (4–8). Moreover, a recent review reported an average injury rate of 14% for low-back injuries among healthcare workers at hospitals in the USA (8). The nature of healthcare work tasks is a major reason for the high prevalence of MSD and back injuries. A recent systematic review showed that, among all healthcare tasks, patient transfer is associated with the greatest risk for developing low-back pain (LBP) and injuries among nurses and nursing assistants (9). Shedding light on the mechanisms, biomechanical studies show high loadings on the spine during patient handling, which often exceeds the 3400 N safety limit recommended by the National Institute of Occupational Safety and Health (10–13).
Previous research has suggested different ergonomic approaches to prevent and reduce the occurrence of LBP and injuries among healthcare workers. The majority of preventive strategies have focused on the use of assistive devices (AD), ie, increasing the availability of AD, education, and training in the use of AD. However, according to systematic reviews, these strategies seem to have little impact on LBP and injuries when implemented as a single strategy (14, 15), as these strategies do not seem to improve the use of AD. Thus, increasing availability and training may not necessarily improve the overall use of AD if other barriers remain. Some researchers have therefore suggested that preventive strategies should focus on cultural and behavioral changes at several organizational levels to increase the use of AD during patient handling (16), rather than simply increasing availibility and training.
Participatory ergonomics (PE) offers a promising strategy for reducing work-related risk factors such as LBP and injuries by integrating both behavioral and cultural change through worker involvement (17, 18). Engaging and motivating workers in planning and managing their work tasks has been suggested to be essential for successful workplace interventions, as this ensures a high level of relevance for the worker (17–20). A non-randomized study by Garg & Kapellusch (21) supported this by showing a 60% reduction in patient handling injuries after implementing a PE intervention, which engaged workers to find ergonomic solutions for reducing patient handling injuries. Despite the promising approach, systematic reviews have found only a few medium quality studies (17, 18, ,22), which show PE to have only partial-to-moderate effects on work-related health outcomes. The latter underlines the need for high-quality randomized studies.
Even though most hospitals in the western world have focused on increasing the availability, knowledge, and use of AD, there are still challenges and needs for improvement (23–25). This was also found in a pilot survey conducted for the present study among 300 nurses and nurses’ aides at four hospitals in Denmark, which showed AD for patient handling were only used in one third of relevant situations. The survey revealed that several barriers influenced the use of AD, including availability and sufficient time for using the AD, proper guidelines, training and instruction, concerns about patient safety and integrity, as well as lack of management and collegial support for maintaining motivation for using AD. Similar barriers have also been found in other studies (16, 26–30). As these barriers may vary between hospital departments, using a PE approach that increases ownership and sustainability (22) seems to be a highly relevant strategy, particularly if several barriers can be addressed simultaneously.
The aim of this study was to evaluate a participatory organizational intervention with department-specific solutions for improved use of AD in a cluster randomized controlled trial (RCT). We hypothesized that PE would result in more frequent use of the necessary AD.
Methods
Study design, blinding and randomization
A two-armed parallel-group, single-blind, cluster RCT with allocation concealment was conducted from April 2016 to April 2017. Healthcare workers from five hospitals in Denmark situated in the areas of Zealand (N=4) and Jutland (N=1) participated in the study. Clusters were hospital departments and units seen as separate entities, and cluster randomization was used to avoid contamination between individuals of each group. After the collection of the baseline data, a person blinded to the status of each department performed the randomization by assigning a random number to each department, subsequently sorting the numbers from low to high, and finally assigning every other number (department) to either control or intervention (random numbers table). The same person informed the participants and their department managers by e-mail about their group allocation. The departments were assigned in parallel to either a 12-month participatory intervention group or a control group for a period of 12 months. As part of the preparations for the intervention (phase 2), assessments of barriers and potential solutions were conducted from September 2015 to February 2016 (phase 1). The design and reporting of the study followed the CONSORT statement for cluster RCT (31) and SPIRIT (32, 33) statements. The study protocol has been published elsewhere (34).
Participants
We allocated 27 departments (clusters) with 625 healthcare workers from five community hospitals in Denmark to either a participatory intervention or control group. Baseline characteristics of the 14 departments in the intervention group and the 13 departments in the control group are shown in table 1.
Table 1
Characteristics of study participants in the control and intervention groups. Note: These data differ slightly from the protocol as one of the departments that declined to participate was mistakenly included in the table of participant characteristics. [SD=standard deviation.]
Recruitment and flow of participants
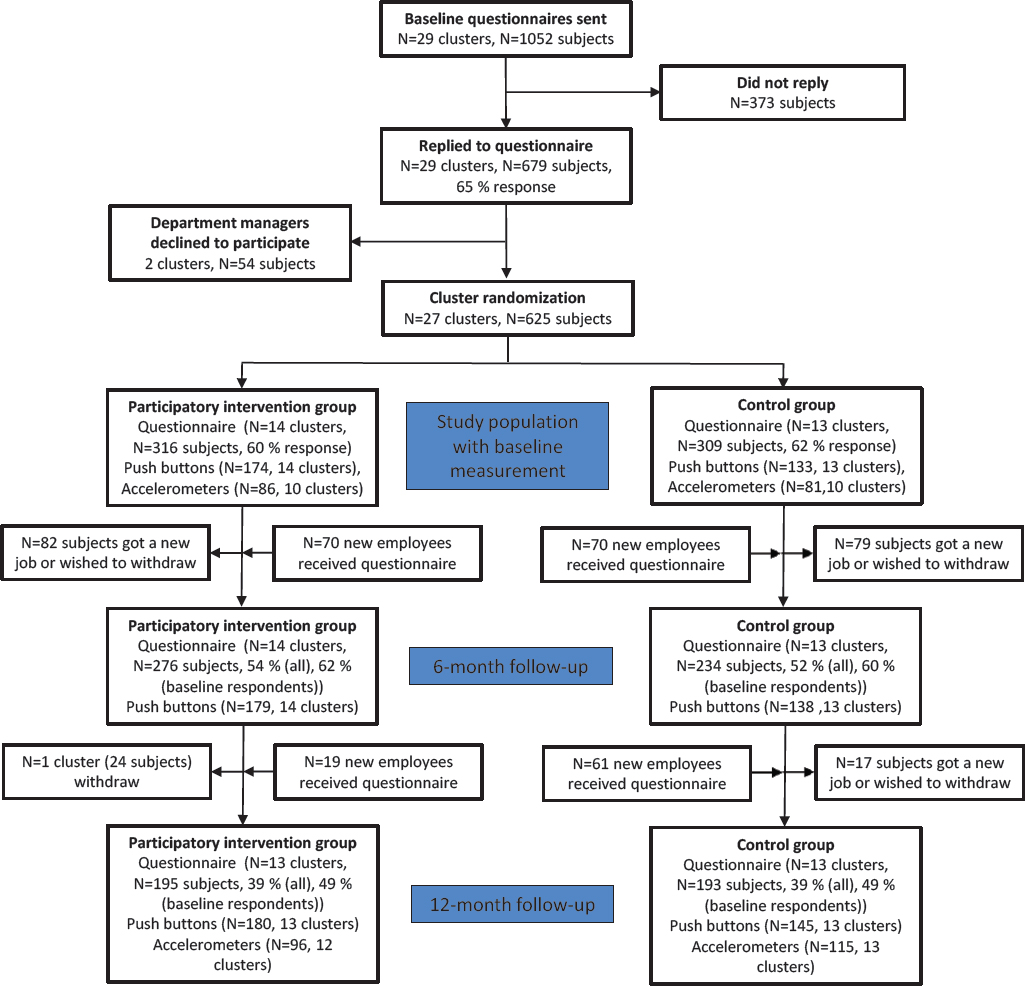
Recruitment of hospital departments started in 2014 and continued throughout 2015 by initially contacting the occupational safety and health (OSH) staff from 11 hospitals, 5 of which were interested in participating. The hospitals’ OSH staff kindly pointed out a total of 35 departments that performed patient transfers daily using AD (inclusion criteria). The final recruitment took place in February 2016 by e-mailing a baseline questionnaire to 1052 healthcare workers (nurses and nursing aids) employed at the 29 departments interested in participating. Prior to randomization, 2 departments withdrew from the study due to limited time resources. Finally, a total of 27 departments with 625 healthcare workers were willing to participate (figure 1).
Phase 1: Assessment of barriers and potential solutions
Prior to randomization, a questionnaire, interviews, observations as well as an analysis of a “best practice” hospital were conducted to collect information about barriers and potential solutions for using AD that could be used for guiding the subsequent participatory intervention. The content of phase 1 has been described in details in the protocol (34). Phase 1 revealed that the most important barriers for using AD were: insufficient time to use AD, outdated AD, misclassification of the patients’ functional capabilities, availability of AD, and lack of space. Having a present and active management that encourages guidance, communication and collaboration in the use of AD and provides sufficient time for patient transfer, as well as ensuring proper space and availability of AD, were suggested as potential solutions for improving the use of AD.
Phase 2: Participatory intervention
The participatory intervention protocol (34) is briefly summarized below. The intervention consisted of two 2-hour workshops. For every workshop at each department, we aimed at recruiting the department manager, 2–5 healthcare workers, who were appointed by their managers, and the hospital’s OSH consultants. Workshop participants were asked to develop and implement an action plan with possible solutions on how to improve the use of AD in their department. To initiate discussions and kick-start the participatory process prior to workshop I, a report summarizing the main results of the department’s baseline questionnaire, as well as results from the general assessment of barriers and solutions, were distributed to the department via e-mail approximately two weeks before the workshop. The general assessment of barriers and potential solutions for the use of AD was conducted before randomization, and consisted of results from the baseline questionnaire, interviews with department leaders and employees in selected departments, and the analysis of experiences of a “best practice hospital” that had been successful with increasing the use of AD [for details see (34)]. Workshop I consisted of two main parts: (i) A brainstorm session based on discussions of the report about the department’s baseline questionnaire results, and the results from the general assessment of barriers and potential solutions for the use of AD. Participants were also asked to identify potential solutions for improving the use of AD in their department. (ii) Development of a simple action plan for the most achievable solution, and subsequently implement it over the course of the following approximately ten weeks prior to workshop II.
Workshop II was conducted approximately 3–4 months after workshop I and consisted of two parts: (i) Discussion of the department’s experiences with implementing the action plan developed in workshop I. (ii) Development of an action plan for implementing up to five solutions that the participants were motivated for and thought would potentially improve the department’s use of AD over the subsequent 6–9 months.
While creating the action plans, the participants were asked to: (i) describe why the solutions were important for their department, (ii) appoint persons responsible for the implementation of the solutions, and (iii) set deadlines for the implementation. Regular checkups of the implementation process were performed using small electronic surveys, e-mail or telephone calls addressed to the department’s workshop participants. After workshop II, no additional counseling on how to succeed in implementing the department’s action plan was provided.
Control group
The control group (N=13 departments) was encouraged to continue with their normal working procedures including living up to standard OSH guidelines during the 12-month study period.
Outcome measures
The outcomes for this study were measured technically using: (i) digital push button counters (primary outcome), and (ii) accelerometers attached to AD (secondary outcome). Other secondary outcomes (see below) were measured using questionnaires.
Primary outcome measure – Use of the necessary AD (Push buttons)
The primary outcome was the technically measured subjective use (at department level) of the necessary AD (ie, sliding sheets, lifts or patient transporters) measured continuously over the entire 1-year intervention period using digital push buttons (Digital Tally Counter, Resultswa, Shenzhen, China). Two digital push button counters were placed next to the doorframe in each patient room. We encouraged the healthcare workers to push either the green or the red button every time they left the room after having performed a patient transfer. The green button (button 1) was labeled: “Press this button if you used the necessary assistive devices for your patient transfer”. The red button (button 2) was labeled: “Press this button if you did not use the necessary assistive devices for your patient transfer”. Accordingly, for each specific patient handling the healthcare workers pressed one of the two push buttons to subjectively rate whether they perceived to have used the “necessary” or proper AD or not for each situation. The primary outcome was measured for each set of counters as the ratio between the number of button 1 counts, and the total number of counts (button 1+2), ie, expressing the percentage of patient transfers where the necessary AD were used. Validation of this method is presented in the supplementary files (www.sjweh.fi/show_abstract.php?abstract_id=3769). Through frequent telephone calls and emails to the department managers and workshop participants as well as through personal contacts, employees were reminded approximately every other month to register their patient transfers using the buttons during the 12-month study period.
The total number of push buttons varied throughout the study due to variations in the number of patient rooms in use at each department (see figure 1).
Secondary outcome – General use of AD (accelerometer-based)
In addition to the measurements by push buttons, the use of AD was also objectively measured using accelerometers (GT3X, Actigraph, FL, USA). The accelerometers were mounted discretely on either patient transporters or lifts (non-disposable AD) to assess the movement of the AD for approximately 1 month at baseline (four weeks before the intervention) and at 12-month follow-up. The term “general use” is an expression for the overall use of non-disposable AD. Because the measurement is solely based on movement of these devices, it provides no information about the right (necessary) use of AD. The accelerometer-based general use of AD was calculated as each department’s average use of AD and normalized to the number of patient transfers performed per day. The number of patient transfers per day was based on the baseline and follow-up questionnaire replies.
The number of departments with non-disposable AD increased from baseline to 12-month follow-up, due to them acquiring new AD (see figure 1). See supplementary files for details on validation and data analysis.
Secondary outcomes – questionnaire based
The remaining secondary outcome measures were assessed by questionnaire.
Pain intensity in the lower-back, neck, and shoulder were rated subjectively using a 0–10 modified visual analogue scale, where 0 indicated “no pain at all” and 10 “worst pain imaginable” (35). The body regions of interest were defined by drawings from a Nordic questionnaire (36).
The occurrence of low-back injuries was obtained by asking the participants:“Have you within the last 12 months injured your back during patient transfers? (Think of situation where the pain appeared suddenly and unexpectedly)” (37).
The participants were also asked about communication and guidance in the use of AD at baseline and at 6- and 12-month follow-up using the following questions and response categories: (i) “Do you discuss the use of assistive devices at your department?” [Discussion of use of AD] answer categories “Yes” or “No”; (ii) “How often have you received guidance in the use of assistive devices during the past year?” [Amount of guidance in use of AD] answer categories: “Never”, “1 time”, “2 times”, “3 times”, “4 times”, “5 times” and “more than 5 times”; (iii) “Do you receive an adequate amount of guidance in using assistive devices for patient transfer?” [Adequate guidance in use of AD] – answer categories: “No, nothing at all”, “Yes, to some extent”, “Yes, very much”; (iv) “Have you experienced a patient transfer situation in the past year, where a colleague made you aware that you should use assistive devices?” [Collegial encouragement to use AD] – answer categories: “Yes” and “No”; (v) “When being handed over a patient from your co-worker: How often are you informed about the assistive devices that are needed for moving the patient?” (think of patients that require AD for being transferred) [Information about use of AD at patient handover] – answer categories: (i) “0 out of 4 patients (ie, almost never)”, (ii) “1 out of 4 patients”, (iii) “2 out of 4 patients”, (iv) “3 out of 4 patients” and (v) “4 out of 4 patients (ie, everyone)”.
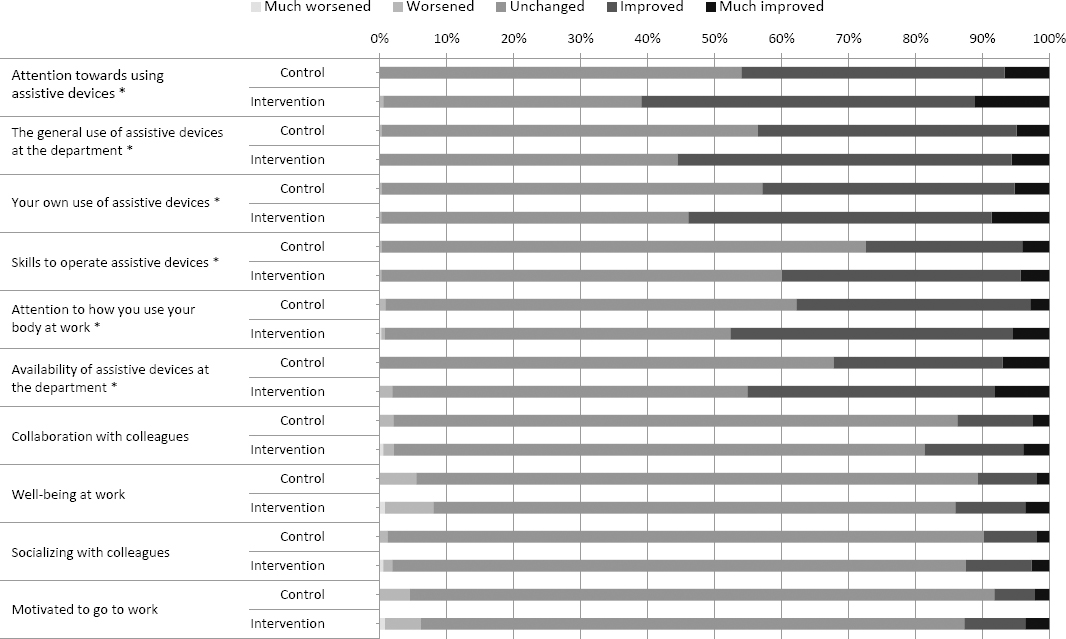
Finally, perceived changes in use of AD and work environment were obtained by asking the following questions at 12-month follow-up: “Which changes have you experienced since the project started in April 2016?: (i) Attention towards using assistive devices, (ii) The general use of assistive devices at the department, (iii) Your own use of assistive devices, (iv) Skills to operate assistive devices, (v) Attention on how you use your body at work, (vi) Collaboration with colleagues, (vii) Availability of assistive devices at the department, (viii) Well-being at work, (ix) Socializing with colleagues, and (x) Motivation to go to work.” The questions were rated on a 5-point scale; 1: “much worse”, 2: “worsened”, 3:”unaltered”, 4: “improved”, 5: “much improved”.
Adverse events
Adverse events (pain and injuries) related to participation in the study were reported in the 6- and 12-month follow-up questionnaire by asking: “Did you experience any side effects (injuries or accidents) as a result of your participation in this project? No or Yes (what type)”.
Sample size
The sample size calculation was based on the primary outcome. A priori power analysis based on previous measurements of the primary outcome revealed that 13 clusters in each group (26 departments in total) were needed for testing the null-hypothesis of equality (α=0.05) with a power of 95%, standard deviation (SD) of 10% and a minimal relevant group-difference in the use of AD of 15%. To the best of our knowledge this is the first time to use push buttons to rate the use of AD. The variation in data was unknown when designing the study. The 15% group-difference was, therefore, based on an estimate.
Statistical analysis
Statistical analyses were performed using the SAS statistical software for Windows (SAS Institute, Cary, NC, USA). Cluster (department) was entered in the model as a random factor. All statistical analyses were performed in accordance with the intention-to-treat principle using a linear mixed model, which accounts for missing values. An α-level of 0.05 was accepted as statistically significant. Outcomes are reported as between-group least mean square differences and 95% confidence intervals (CI) at 6- and 12-month follow-up.
Between-group differences in perceived changes at 12-month follow-up were investigated using a Fisher’s exact test.
Results
Study population, adherence and adverse events
Twenty-six workshops were conducted in total. One department did not participate in any of the two scheduled workshops as it underwent a change in management during the study, resulting in a non-prioritization of the workshops. After approximately six months and the second workshop, one of the departments in the intervention group chose to withdraw from the intervention due to changes in the priority of work environmental challenges. All departments, except one, participated in the two scheduled workshops. Of all participants and among the ones who answered the baseline questionnaire, 39% and 49%, respectively replied to the questionnaire at 12-month follow-up. Only one participant, from the control group, reported increased pain (adverse event) as a result of participating in the project, without specifying what led to the increased pain.
Use of assistive devices during patient transfer
A priori hypothesis testing showed no group×time interaction for the use of necessary AD using push buttons (primary outcome, P=0.631). However, the frequency in the general use of AD measured with accelerometers increased more following the 12-month intervention in the intervention group compared with the control group (secondary outcome, P=0.042) (table 2).
Table 2
Baseline values (least square mean) and between-group (control – intervention) differences at follow up (6 and 12 months) for technical (push buttons and accelerometers) measures of use of assistive devices. [AD=assistive devices; 95% CI=95% confidence interval.]
| Baseline | Between-group differences at follow-up | Gr×Ta | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||||
| Control | Intervention | 6 months | 12 months | ||||||||
|
|
|
|
|
||||||||
| Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | P-value | Mean | 95% CI | P-value | ||
| Use of assistive devices measured with: | |||||||||||
| Push buttons (% of transfers using the appropriate AD) (“necessary use”) | 0.64 | 0.61–0.68 | 0.67 | 0.64–0.70 | -0.23 | -0.70–0.27 | 0.36 | -0.11 | -0.61–0.37 | 0.630 | 0.631 |
| Accelerometers (n patient transfers per day per patient) (“general use”) | 0.26 | 0.05–0.47 | 0.32 | 0.12–0.51 | -0.31 | -0.59– -0.04 | 0.028 | 0.042 | |||
Pain and work-related injuries
Musculoskeletal pain in the lower-back, neck, and shoulder, and occurrence of low-back injuries during patient transfer were unaltered following the participatory intervention (P>0.05, table 3).
Table 3
Baseline values (least square mean) and between-group (control – intervention) differences at follow up (6 and 12 months) for low-back, shoulder and neck pain and occurrences of low-back injuries. [95% CI=95% confidence interval.]
| Baseline | Between-group differences at follow-up | Gr×Ta | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||||
| Control | Intervention | 6 months | 12 months | ||||||||
|
|
|
|
|
||||||||
| Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | P-value | Mean | 95% CI | P-value | ||
| Low-back pain (scale 0–10) | 2.9 | 2.6–3.3 | 2.9 | 2.6–3.3 | -0.1 | -0.7–0.4 | 0.608 | -0.2 | -0.7–0.4 | 0.552 | 0.868 |
| Shoulder pain (scale 0–10) | 2.8 | 2.4–3.1 | 2.7 | 2.3–3.0 | -0.4 | -0.9–0.1 | 0.154 | -0.3 | -0.9–0.2 | 0.244 | 0.205 |
| Neck pain (scale 0–10) | 2.7 | 2.4–3.0 | 2.5 | 2.2–2.8 | -0.4 | -0.9–0.2 | 0.172 | -0.1 | -0.7–0.4 | 0.609 | 0.117 |
| Occurrences of low-back injuries the last year (N) | 1.2 | 1.1–1.2 | 1.2 | 1.2–1.3 | 0.0 | -0.1–0.0 | 0.179 | 0.0 | -0.1–0.0 | 0.399 | 0.903 |
Patient transfer and use of assistive devices (communication, guidance and skills)
A main effect was observed for the number of daily patient transfers (P<0.05, table 4). This effect was mainly driven by a reduction in the control group. The number of self-reliant patients and self-efficacy towards increasing the use of assistive devices did not change during the intervention period. There were group×time interactions and differences at follow-up in favor of the intervention group for discussions of use of AD, adequate guidance and amount of guidance on use of AD, collegial encouragement to use AD, and information about use of AD at patient handover (P<0.05, table 4).
Table 4
Baseline values (least square mean) and between-group (control – intervention) differences at follow up (6 and 12 months) for communication and guidance in the use of assistive devices. [AD=assistive devices; 95% CI=95% confidence interval.]
| Baseline | Between-group differences at follow-up | Gr×Ta | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||||
| Control | Intervention | 6 months | 12 months | ||||||||
|
|
|
|
|
||||||||
| Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | P-value | Mean | 95% CI | P-value | ||
| Number of daily patient transfers (N) | 5.4 | 5.0–5.8 | 4.8 | 4.5–5.2 | 0.5 | -0.1–1.1 | 0.087 | -0.2 | -0.8–0.5 | 0.626 | 0.042 |
| Number of self-reliant patients the past month (N out of 4 patients) | 1.5 | 1.4–1.6 | 1.8 | 1.6–1.9 | -0.3 | -0.5–-0.1 | 0.001 | -0.2 | -0.4–0 | 0.111 | 0.436 |
| Discussion on use of AD (No = 1, Yes = 2) | 1.4 | 1.3–1.4 | 1.4 | 1.4–1.5 | 0.1 | 0.0–0.2 | 0.047 | 0.1 | 0.0–0.1 | 0.192 | 0.002 |
| Adequate guidance in use of AD (Scale 1–3) | 2.1 | 2.0–2.1 | 2.0 | 2.0–2.1 | -0.2 | -0.3– -0.1 | 0.004 | -0.2 | 0.3– -0.1 | 0.003 | 0.001 |
| Amount of guidance in use of AD (Scale 1–7) | 1.6 | 1.4–1.8 | 1.4 | 1.2–1.6 | -0.1 | -0.4–0.1 | 0.332 | -0.2 | -0.5–0.1 | 0.202 | 0.041 |
| Collegial encouragement to use AD (No = 1, Yes = 2) | 1.4 | 1.3–1.4 | 1.5 | 1.4–1.5 | 0.1 | 0.0–0.1 | 0.233 | 0.0 | -0.1–0.1 | 0.935 | 0.018 |
| Information about use of AD at patient handover (N out of 4 patients) | 1.7 | 1.5–1.9 | 1.5 | 1.3–1.7 | -0.2 | -0.4–0.1 | 0.194 | -0.3 | -0.5–0.0 | 0.082 | 0.017 |
| Self-efficacy towards increasing the use of AD (1–3) | 2.4 | 2.2–2.5 | 2.3 | 2.2–2.4 | -0.1 | -0.3–0.1 | 0.395 | 0.1 | -0.2–0.3 | 0.581 | 0.426 |
Perceived changes at follow-up
A greater proportion of the intervention group compared with the control group reported improved perceived changes in: “Attention towards using assistive device”; “The general use of assistive devices in the department”; “Your own use of assistive devices”; “Skills to operate assistive devices”; “Attention on how you use your body at work”; and “Availability of assistive devices in the department” at 12-month follow-up (P<0.05) (figure 2). There were no difference between the groups for: “Collaboration with colleagues”; “Well-being at work”; “Socializing with colleagues”; or “Motivated to go to work” (P>0.05) (figure 2).
Discussion
Contrary to our hypothesis, the main finding of this cluster RCT showed that the frequency of “necessary” AD use was not improved following the PE intervention. However, we found that the intervention improved the general use of AD, measured objectively with accelerometers, and lead to improved communication and guidance in the use of AD. This demonstrates potential benefits for systematic, widespread implementation of this participatory organizational intervention in hospitals in Denmark as a means to promote the general use of AD.
PE programs have in recent years been suggested as an important method for lowering work-related risk factors such as hazardous manual work tasks, and thereby reducing the incidence of MSD (18, 22). Thus, implementing participatory solutions for lowering the risk of LBP and injuries from manual patient transfer (9, 37) through increased general use of AD seems promising. The improvement in the objectively measured general use of AD was supported by perceived improvements in the departments’ overall and workers’ use of AD in the intervention group. Nevertheless, despite the potential reductions in exposure from manual patient transfer, this did not lower the incidence of LBP and low-back injuries. This is somewhat in contrast with previous non-randomized controlled PE interventions conducted among healthcare workers (21, 38). These interventions reduced patient handling injuries using a similar approach by forming PE teams consisting of managers, workers and technical advisors that implemented changes in training and work process with the aim of lowering the risk of injuries (21, 38). Notably, these interventions did not specifically aim at improving the use of AD but rather in reducing work-related risk factors in general. Although low-back injuries have huge individual and socioeconomic consequences, the incidence thereof is somewhat low (<4%) among healthcare workers in Denmark (37).
Insufficient statistical power impairs the chances of identifying significant group×time differences in occurrence of work-related injuries. Burdorf and colleagues (39) have estimated that a sample size of >10 000 healthcare workers (newly hired nurses) is required for demonstrating a statistically significant effect of introducing lifting devices on musculoskeletal injury rates using a randomized controlled design. As it was unrealistic to recruit such a large sample size for this study, we chose to measure the use of AD as an accessible proxy measure for injury prevention. Although we did not find any changes in patient transfer injuries and lower-back, shoulder and neck pain following the intervention, the risk may still be reduced as a result of the improved general use of AD.
Observational and experimental studies have shown that the introduction of additional AD may lead to more frequent use and, in result, reduced injury rates among healthcare workers (40, 41). However, Burdorf et al (39) concluded in a literature review that effective implementation of interventions aiming at increasing the use of assistive devices through, ie, PE, increased guidance and training, are a necessity for effectively reducing LBP and injuries. As a result, this participatory intervention aimed at improving the use of AD through proper implementation of developed solutions that targeted the departments’ specific barriers.
These barriers may have been overcome through improved guidance and communication. In fact, a group×time interaction was observed in favor of the intervention group, in the amount and sufficiency of guidance in the use of AD, the general discussion and collegial encouragement on use of AD in the department and, the level of information about the use of AD at patient handover. Moreover, perceived changes in: attention towards AD, own use of AD, department use of AD, skills to operate AD, attention on how you use your body during patient handling, and availability of AD, were improved in the intervention compared with the control group. Although perceived changes from behavioral interventions should be interpreted with caution, the present subjective measures suggest that improvements in technique and quality of the patient transfer, as well as associated use of AD, may have occurred following the intervention, regardless of how often the AD were used. This is supported by a biomechanical investigation (10) showing that the between-subject variation in low-back compression forces during patient handling, in situations with and without AD, is high, and may not only be related to muscle strength or anatomical differences. This indicates that there seems to be individual differences in patient handling techniques and quality, which may be improved through better communication and guidance in the use of AD.
There may be several explanations for why the necessary (push button-based) use of AD did not change, whereas the general (accelerometer-based) use of AD improved following this 12-month PE intervention. Improving the general use of AD may be the first step in developing high quality patient-transferring skills. Notably, the present participatory intervention focused on improving the general use of AD and not only on the specific use thereof. Although the improved guidance and communication may have increased awareness on the proper use of AD, changing how often healthcare workers use the necessary devices may require more time or workshops than the two 2-hour workshops. In fact, Van Eerd and co-workers (18) stated that the effect of a PE program depends on intervention intensity to provide a sufficient dosage to sustain motivation among participants throughout the study period. Moreover, lack of intervention intensity or delivery of the participatory program due to lack of time, work pressure and management commitment may explain the mixed results shown in participatory studies (42–44). Encouraging the workers to continue working with their barriers and solutions, therefore, seems essential for ensuring sustainability. The majority of solutions developed in the present workshops can be categorized into four groups.
More specific and systematic competence training. Examples of planned activities from departments include: (i) more specific training in the correct use of sliding sheets, (ii) systematic introductory training for new employees in the department, and (iii) better knowledge about moving bariatric patients.
Increasing availability and visibility of existing AD. Examples of planned activities from departments include: (i) purchasing more of the most commonly used AD, (ii) making sure enough sliding sheets are available, (iii) marked “parking areas” for AD not in use, and (iv) setting up inventories of the department’s assistive devices.
Improved knowledge about a patient’s needs for AD: Examples of planned activities from departments include increased documentation of the patient’s capabilities and need for AD in the patient’s online records/journals, on whiteboards above the patient’s bed, or in the nurses office.
Improved teamwork and mutual support in the proper use of AD. Examples of planned activities from departments include (i) always getting a colleague to help move a patient, (ii) reminding each other about good patient transfer techniques, and (iii) involving physical therapists more often.
However, implementing these solutions requires that healthcare workers and, in particular, management need to prioritize time for this. The latter which is easily neglected due to a busy schedule and may, in part, explain the lack of improvements in the necessary use of AD observed in the present study. Therefore, PE interventions by themselves may be too demanding for some workplaces, and rely too much on the department’s own resources to develop and implement improvements. Interventions that focus on a “high-order safe-design approach” (41) (ie, an approach where resources are provided from a higher level than only the immediate department) could be a more effective alternative for such workplaces.
Strength and limitations
Although the push button ratings are technically measured, limitations still exist for using this approach as the rating relies on workers remembering to press the buttons after performing a patient transfer. The use of the push buttons may, however, increase awareness of using AD, which may be regarded as an intervention by itself. Nonetheless, this increase in awareness should be equal in the intervention and control groups. On the other hand, a potential limitation is that increased guidance and communication in the participatory intervention group may have changed the perception of when AD are needed. As studies using self-reported data (21, 29, ,40) may be influenced by recall-bias, an apparent strength of this study was the objective accelerometer-based measurements of use of AD. This may partly explain the differences between the push button- and accelerometer-based use of AD. Nevertheless, the participants reported that they remembered to push the “green” and “red” buttons in approximately 3 out of 4 situations (95% CI 2.7–3.1) (see supplementary files for further details). There were no differences between the intervention or control groups with the green or the red buttons, in how often the participants remembered to push them. Thus, this is unlikely to result in a bias concerning the percentage use of the necessary AD. Another limitation was that the general use of AD was only measured using accelerometers in 25 out of the 27 departments that used lifts and patient transporters. Additionally, due to the relatively low questionnaire response rate, the survey-data should be interpreted with some caution. Finally, the use of a cluster RCT design was a strength, as it protected against contamination between departments allocated to intervention and control.
Concluing remarks
The 12-month participatory ergonomic intervention did not improve the frequency of use of the necessary AD but did lead to increased general use of such devices (measured objectively with accelerometers), as well as improved communication and guidance in the use of AD. These changes may reduce exposure from manual patient transfer and improve the technique and quality of patient handling while using AD, and therefore, potentially lower the risk of LBP and injuries in the long run.
Ethics approval and consent to participate
The Danish National Committee on Biomedical Research Ethics approved this study (the local ethical committee of Frederiksberg and Copenhagen; H-3-2010-062) as part of the research program “Implementation of physical exercise at the workplace (IRMA)”. According to Danish law, neither questionnaire nor register-based studies require approval by ethical and scientific committees or informed consent. Only the participants participating in the workshops were, therefore, asked to give their written informed consent to participate in the study. Nevertheless, all participants receiving the questionnaires were informed about the purpose of the study. The trial “Participatory Organizational Intervention for Improved Use of Assistive Devices for Patient Handling” was registered in ClinicalTrials.gov (NCT02708550) prior to randomization of participants. The National Research Centre for the Working Environment in Denmark has an institutional agreement with the Danish Data Protection Agency about procedures to treat confidential data (journal number 2015-41-4232), eg, by securing data at a protected drive with limited access and making all individual data anonymous.