It has been estimated that in Canada, similar to other industrialized countries, approximately 30% of the workforce is employed in schedules outside of conventional daytime hours (1). Defined as nonstandard shifts, this type of working schedule includes regular evening or overnight shifts and rotations between day and night shifts (2). With the large number of workers employed in nonstandard shifts (1), potential adverse health outcomes related to these schedules have been of increasing concern. These concerns revolve around findings that biological functioning in humans follows a circadian rhythm that promotes activity during daylight hours and recovery when it is dark. Staying awake during normal sleeping hours can lead to circadian desynchronization, changes in normal biological processes, and – over the long term – has been associated with poorer health, including increased risk of chronic disease (3–6). It is believed that work at night also may affect psychosocial and behavioral stressors such as diet and exercise with further deleterious health effects (7). Disruption in duration and quality of sleep attributed to shift work has been associated with increased fatigue and poorer concentration (8, 9). This combination of problems associated with working night-shifts may have a cumulative effect on overall health and job performance (10) which may contribute to an increased risk of work-related injuries (1, 11–14).
Gender differences in work injury risk among shift workers have also been explored. However, there is limited empirical evidence showing an interaction between shift work and gender that definitively points to shift work as more adverse for either women or men. It has been suggested that night shift work for women may result in greater fatigue and reduced work–life balance and may potential lead to a higher risk of work injury (1, 15). For example, a recent study found that trouble sleeping was associated with work injury among women, but not men, who were working nonstandard shifts (6). In many households, women remain the primary family caregivers (16) and spend more time on household duties, such as childcare, than men (17). The added responsibility of work at night may also contribute to job strain, role overload, and role conflict (18) and ultimately may put women at a higher risk for work injuries (19) although it is not clear whether this effect would remain once gender differences in occupation are taken into consideration. Men are more likely to be employed in physically demanding occupations, which increases their chances of being injured at work (20). However, some studies have found that after accounting for occupational physical demands, work during non-regular daytime schedules may be more harmful for women than men in terms of work-related injuries (1, 21).
In understanding the employment trajectories of workers, it is important to recognize that individuals can change their shift type over time. These changes may be voluntary (eg, to take advantage of new job opportunities or for health and lifestyle preferences or concerns) or involuntary (eg, as a result of organization restructuring). However, there is currently little information on whether changes in a worker’s shift type are associated with the risk of work injury over a prolonged period of time. Existing evidence suggests that individuals working regular day shifts have a lesser likelihood than nonstandard shift workers of experiencing work injuries. As such, switching out of nonstandard shifts may provide a “better” working environment in terms of worker safety. The corollary would be that those switching out of day shifts to nonstandard shifts might experience an increased risk of injury as they adjust to being awake and working during normal sleeping hours or deal with variability in work scheduling. In a recent study examining the impact of entering or leaving shift work on sleepiness, results showed that moving from a regular day shift into a nonstandard shift resulted not only in an increased risk of having difficulties with entering recovery sleep but also with increased risk of falling asleep at work (22). For those switching out of nonstandard shifts, the risk of having difficulties entering recovery sleep was significantly reduced. Similar findings were reported among a study of retired shift workers with sleep quality improving after time away from shift work (23).
The purpose of this longitudinal study is to (i) gain a better understanding of the characteristics of workers who change shift types, (ii) characterize the probability of work injury over time, following a change in shift type, (iii) examine if changing shift type is associated with an increased risk of work injury, and (iv) identify whether work injury risks differ between men and women. This expands upon the existing body of studies, which have focused mainly on the risk of work injury associated with specific shift types such as regular nights or rotating schedules (15) or short-term biological responses of greater fatigue and stress during night shifts and recovery days (24–26). We hypothesize that, compared to workers who work regular day shifts only, those who switch from day to nonstandard shifts will have the highest risk work injury. Workers in nonstandard shifts for a prolonged period of time may have acclimatized to their work schedules and thus are expected to have a lower risk of injury than those who have just recently transitioned from regular day shifts. Workers who change from nonstandard to day shifts should benefit from protective effects of day shifts and are expected to have similar injury risks at those working only day shifts. In keeping with emerging findings of gender differences in previous research, we anticipate that women who are transitioning into, or remaining in, nonstandard shifts will have a higher risk of work-related injury than men.
Methods
Data sources and population
This study used data gathered in the Survey of Labor and Income Dynamics (SLID), a household income survey administered by Statistics Canada that collects information regarding an individual’s labor market activity and income over six consecutive years. In each survey group, approximately 17 000 households (34 000 respondents) are interviewed annually in January to report on their labor market participation over the previous 12 months. Approximately 80% of respondents provide permission to gather additional information from their federal income tax forms. The remaining 20% of respondents who decline permission are interviewed for a second time in May to provide additional income information for the previous year (January to December). A stratified, random clustered sampling design provides a representative sample of the non-institutionalized Canadian population. The response rates for the longitudinal panels have decreased with time but still remain high (85% in 1996; 72% in 2010) (27, 28).
Data from three SLID survey groups (1999–2004, 2002–2007, 2005–2010) were used for the study. The study population included all respondents between the ages of 16–69 years who reported working as a paid employee and provided information for all six years of the survey. For respondents who switched shifts more than once during their participation in the SLID, follow-up time was censored to the start of their second shift change. We excluded those with a shift change in their last year of participation in the SLID because injury information post-shift change would not be available in the data.
Outcome and predictor variables
Outcome variable: work-related injuries
Respondents were asked annually whether, over the past 12 months, they received workers’ compensation for an injury sustained at work or were absent from work for a period of ≥1 week that was attributed to a work-related injury or illness. We used the first incidence of workers’ compensation or absence as a surrogate measure for incidence of a work injury resulting in lost work days.
Primary predictor: work schedule
During each survey, respondents in the SLID were asked to select from eight SLID shift-type categories best describing their work schedule in the past 12 months. We collapsed these categories into two shift work types: (i) regular day shifts and (ii) nonstandard shifts. Using definitions from prior studies (1, 2), we defined “nonstandard shift” workers as those who reported working anything other than a “regular daytime schedule”, such as an evening or overnight shift or a rotating day/night shift. A shift change was identified if a respondent reported different shift types in consecutive years during their participation in the SLID.
From this information, four categories were created to describe respondents’ work schedules during the 6-year survey period: (i) regular day shifts only (reference); (ii) switched from regular day shifts to nonstandard shifts; (iii) switched from nonstandard shifts to regular day shifts; and (iv) nonstandard shifts only (ie, never worked a regular day shift during survey participation)
Other independent variables
We formulated two categories of variables (respondent and occupational), which may confound or modify the relationship between shift work and work injury. Respondent characteristics included age, gender, highest education level, and household income. Gender was also treated as an effect modifier to account for hypothesized differences in work and home experiences between men and women. We included province of residence to account for potential regional differences in labor market and worker compensation policies. Occupational characteristics (ie, job permanency, usual weekly hours worked, physical demands, and number of employees in the organization) provided information about working conditions that may be associated with the risk for a work injury. Those new to a work situation, such as those starting a job, who work a greater number of hours, or who work in large organizations have been found in previous research to have increased risks of work injury (29–33).
Limited information is available from the SLID regarding occupational demands. However, we included a measure of occupational physical demands in terms of strength requirements typically used while working. This variable was derived from occupational codes following guidelines defined by Human Resources and Skill Development Canada (34) and has been shown to be strongly correlated with work-related injuries (35, 36). Strength requirements were characterized using four categories: (i) limited – tasks that involve handling loads <5 kg (eg, administrative positions); (ii) light – tasks that involve handling loads of 5–10 kg (eg, shoe repair); (iii) medium – tasks that involve handling loads of 10–20 kg (eg, carpenters); and (iv) heavy – tasks that involve handling loads >20 kg (eg, road construction). Information regarding respondent and occupational characteristics was taken from the first year of survey enrollment for those who worked day or nonstandard shifts only. For those who switched shift types during the study period, this information was obtained from the first survey following the shift change.
Statistical analysis
Each respondent who participated in all six years of the SLID survey was identified. For participants with a shift change, the start of their work-injury follow-up (ie, the period in which we examined presence/absence of work injury) was the year the shift change occurred. For individuals who worked day or nonstandard shifts only during the survey period, the work-injury follow-up period began with the first year of their enrollment into the SLID. End of work-injury follow-up was either at the end of the 6-year survey period, when a work injury occurred, or when a second shift change occurred. The total number of annual paid work hours was summed across years of follow-up for each respondent.
Demographic and occupational characteristics were described for each work schedule group. A test of equality for proportions was conducted to compare our study population with the larger workforce population. Chi-squared tests were used to determine differences in characteristics between shift schedule groups. Incident rates were calculated as the number of incidents over the person-time hours. Incident rate ratios (IRR) were calculated by dividing incident rates for each shift schedule group by rates for daytime only workers. Univariate analyses were completed with Kaplan Meier methods to describe cumulative probability of work injury over time and graphically examine the assumption of proportional hazards. Univariate analyses also showed that work schedule categories violated the assumption of proportional hazards, and therefore this variable was treated as a time-varying variable in our Cox proportional hazard analyses. Log-rank tests determined if differences were significant between groups.
Multivariate analyses were carried out using Cox proportional hazards regression models to assess the risk of work injury over different shift schedules. Adjustments were made for respondent and occupational characteristics, which may confound or modify the risk of work injury. Controlling for year of survey was also included to reflect any policy changes that may have occurred over time and as such, were treated as time-varying covariates. To account for survey non-responses (based on age, gender, geographic region, and income) and the complex sampling design of the SLID, confidence intervals around each estimate were adjusted using a bootstrap technique with 1 000 replicate weights supplied by Statistics Canada (37). Stratified analyses for women and men were completed to examine gender as an effect modifier and to determine risk estimates for each work schedule. Gender differences across independent variables were assessed with a series of interaction terms. Post-hoc pairwise regression comparisons were used to determine significant differences between specific categories of work schedules.
All statistical analyses were completed with Stata version 12 (StataCorp LP, College Station, TX, USA). All P-values <α=0.05 were considered statistically significant. Ethical approval for this study was obtained through the University of Toronto, Health Sciences’ Ethics Committee.
Results
In the three SLID survey panels (1999–2004, 2002–2007, and 2005–2010), there were 94 280 respondents aged 16–69 years. Among them, 70 070 (74%) reported being employed at some point during their participation in the survey. We restricted the population to those who provided responses and were employed in all six years of the survey (N=19 898) and excluded those with a shift change in the last year of survey participation (N=767). Our final population consisted of 19 131 respondents. While this represented only 27% of the population who reported working during some point in their participation in the SLID, both the restricted and full populations were similar in terms of distribution of gender (P=0.33) and income (P=0.41). However, a larger proportion of our final, restricted population were older (P<0.001), had a higher education level (P<0.001), and were employed in stable occupational situations (eg, full time employment, permanent positions, P<0.001 for both) (See appendix).
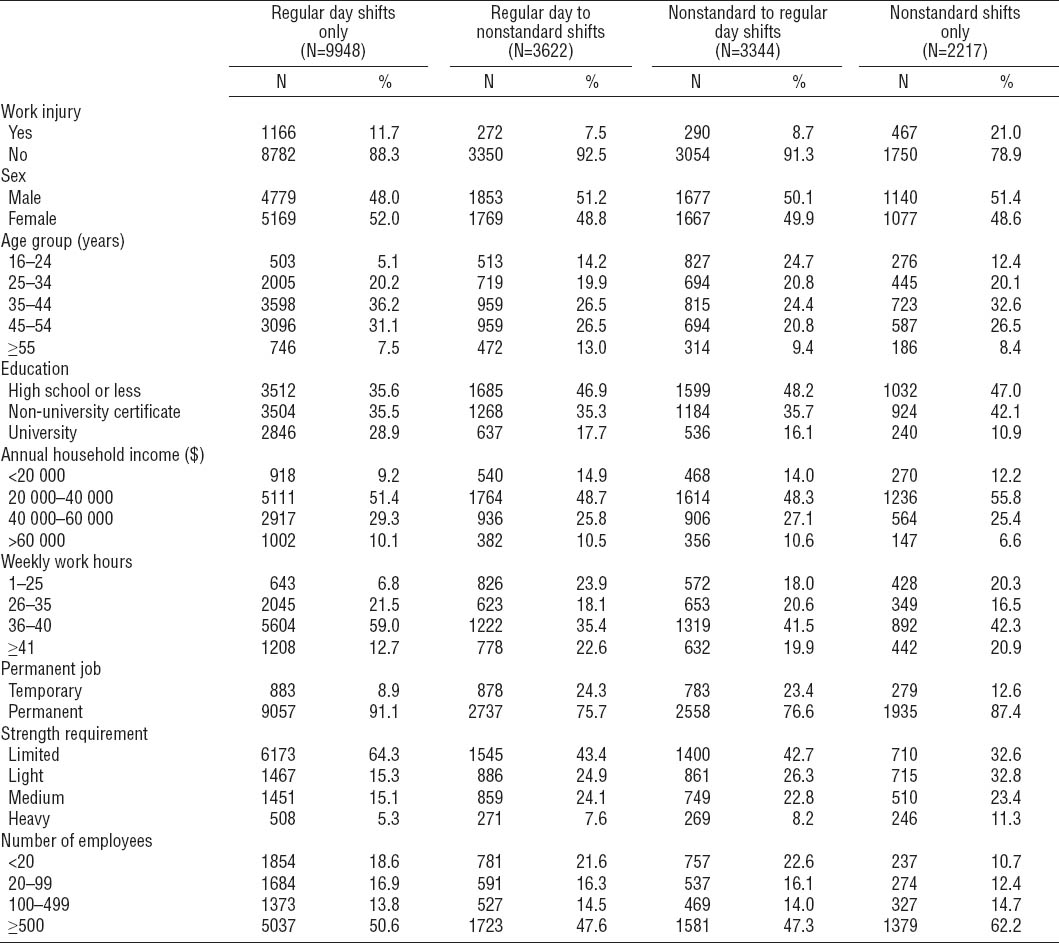
The distribution and characteristics of respondents in each shift schedule group is reported in table 1 (day shifts only 52.0%, day to nonstandard shifts 18.9%, nonstandard to day shifts 17.5%, and nonstandard shifts only 11.5%). Workers who switched from day to nonstandard shifts and from nonstandard to day shifts had more similarities to those who worked nonstandard shifts only than those who worked only regular days (table 1). Specifically, those who worked nonstandard shifts anytime during their participation in the SLID were younger (16–24 years, P<0.001) and had lower educational status (less than or equivalent to high school, P<0.001) than those employed in regular day shifts only. Working conditions were also similar between those who switched shift types and those employed in nonstandard shifts only: a larger proportion worked <25 hours per week (P=0.149) and had jobs requiring medium or heavy strength utilization (P=0.174). Switching between shift types appeared to be related to job permanency, as a larger proportion of respondents were employed in temporary positions compared to those who worked day or night shifts only (P<0.001 for both).
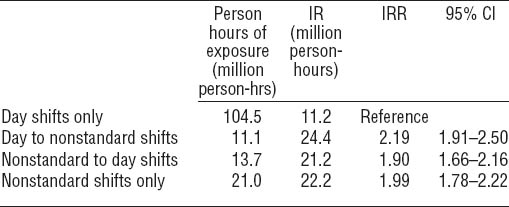
The cumulative injury incidence over the SLID’s 6-year follow-up period was 8.6%, resulting in an annual injury rate of 1.4% (table 1). This corresponds with national estimates of awarded compensation claims from 2010 (38). While regular daytime-only workers worked more hours than other groups and thus had more opportunity for injury incidence (table 2), the incidence rates and IRR among those who switched shifts were approximately double that of daytime-only workers [day to nonstandard: IRR 2.19, 95% confidence interval (95% CI) 1.91–2.50; nonstandard to day: IRR 1.90, 95% CI 1.66– 2.16; nonstandard shifts only: IRR 1.99, 95% CI 1.78–2.22].
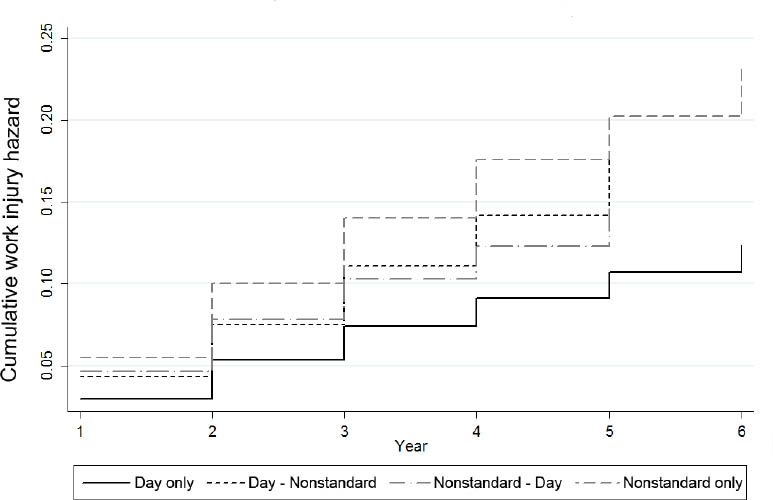
Kaplan Meier analyses revealed that the cumulative probability of injury increased at different rates across categories of work schedules for all workers (figure 1). Results of log-rank tests indicated that probability of injury among those working day shifts only was significantly lower than all other work schedules (P<0.001).
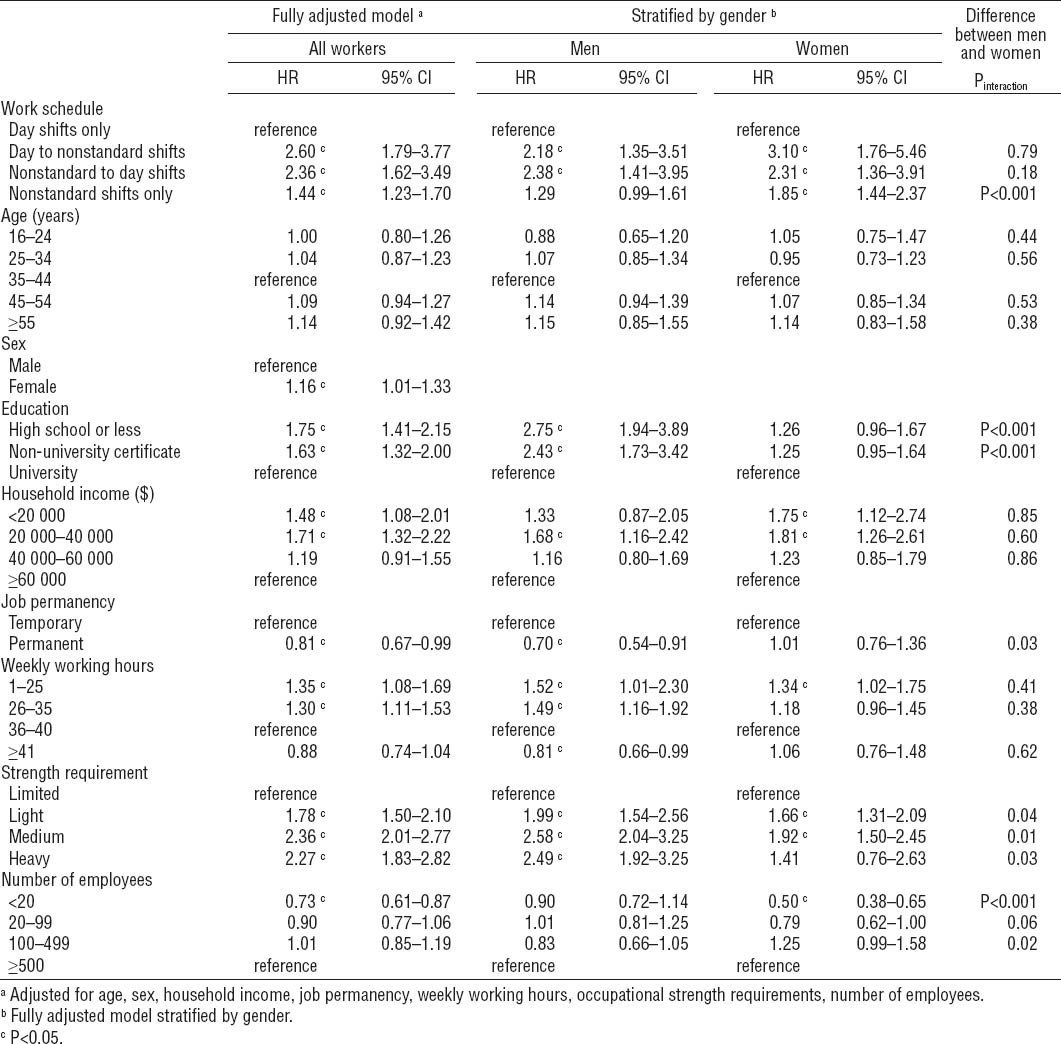
Unadjusted injury hazard ratios (HR) (not shown) resulted in significantly higher risks among all categories of work schedules compared to those who worked day shifts only (day to nonstandard shifts HR 2.47, 95% CI 2.06–2.96; nonstandard to day shifts HR 1.82, 95% CI 1.52–2.17; and nonstandard shifts only HR 1.89, 95% CI 1.64–2.17). In the final model, the risk of injury remained significant after adjustment for respondent and occupational characteristics (table 3). Increased injury risk was observed among those who: switched from day to nonstandard shifts (HR 2.60, 95% CI 1.79–3.77), switched from nonstandard shifts to days (HR 2.36, 95% CI 1.62–3.49), and who remained in nonstandard shifts during the study period (HR 1.44, 95% CI 1.23–1.70). There was no difference in risk between workers who switched shift types (P=0.14), and those who worked nonstandard shifts only (P=0.41). Significantly increased injury risks remained among women and those with less than university-level education, lower incomes, in physically demanding occupations, in non-permanent positions, or working <35 hours per week. We also found that those employed in establishments with <20 employees were less likely to be awarded workers’ compensation or have a work- injury absence for >7 days.
In the gender-stratified analysis (table 3), the only significant difference between men and women were among those working nonstandard shifts only (P<0.001). Within-gender results showed that the risk of work injury was slightly higher for women who switched shifts (days to nonstandard HR 3.10, 95% CI 1.76–5.46; nonstandard to days HR 2.31, 95% CI 1.36–3.91), or worked only nonstandard shifts (HR 1.85, 95% CI 1.44–2.37). Risks were not significantly different between those who switched shift types (P=0.23), but both groups had a significantly higher risk of work injury compared with women working nonstandard shifts only (P<0.001). Among men, the risk of injury remained higher among those who switched shifts (days to nonstandard HR 2.18, 95% CI 1.35–3.51; nonstandard to days HR 2.38, 95% CI 1.41–3.95), with no difference between both these groups (P=0.73). However, the risk among male night-shift-only workers was attenuated and no longer significant (HR 1.29, 95% CI 0.99–1.61).
Discussion
Existing evidence has focused primarily on the risk of work injury or short-term recovery associated with nonstandard shifts. This study fills a gap in our understanding of shift work by examining work injuries among those workers who switch shift schedules. Previous studies have shown that those employed in regular daytime schedules are less likely to be injured on the job, suggesting that regular daytime workers may have a “better” work schedule in terms of prevention of work injuries. As such, we expected that respondents switching from nonstandard to daytime-only shifts would benefit from this “better” schedule with respect to work injuries. However, the results of this study shows that work injury risk associated with changing shift schedules is more complex than previously assumed.
This study extended prior research to examine (i) the probability of sustaining a work-related injury following a change in shift type, (ii) whether work injury risk was associated with changes in shift type, and (iii) whether the pattern of risks were different between women and men. We found that personal and occupational characteristics of those whose shifts changed were often similar to those who worked nonstandard shifts compared to those who worked only regular days. Specifically, workers who changed shifts were generally younger and had lower education and income levels. In prior studies, these same factors have been associated with an increased risk of work injury (39). Moreover, occupational characteristics that were reported among those who changed shift types, namely physically demanding jobs and non-permanent positions also have been identified as factors that are associated with increases in work injury risk (30, 40). Of interest in this research is that even after adjustments for these factors, increased risk of work injury was still present among those who switched shifts. Future studies are needed to replicate these findings and examine other occupational factors (eg, specific job tasks) that may play a role along with changing shift types and the increase of work injury risk. This information could be used to help develop occupational health and safety programs to maintain worker health.
Our results supported the hypothesis that those who switched from regular days to nonstandard shifts would have the highest injury risk. It may be that those new to working nonstandard shifts experience greater fatigue or other difficulties that may increase their risk for work injury. Of concern, however, were findings that those who switched from nonstandard to day shifts had a similar injury risk to those switching in the opposite direction. The explanation for this finding is unclear. Our data did not provide information on the reasons for a change in shift type. It may be that a change in shift was associated with more hazardous work environments, thereby increasing the risk for injury, or poorer health precipitated a shift change and continued to exert a potential impact on increasing the risk of a work injury. Further investigation is needed to understand lifestyle and occupational factors that may have a unique impact on some types of shift changes more than others or that might have similar impacts on a range of work scheduling transitions and the risk of work injury. Finally, those who worked nonstandard shifts only were more likely to be injured at work compared with those who remained in day shifts during the study period. This is similar to findings from previous studies (1, 15). As expected, individuals who worked nonstandard shifts only were less likely to be injured than those who switched shift types. Additional research is needed, but it may be that those who remain in nonstandard shifts for a prolonged period of time are able to adjust to the potentially adverse conditions.
Stratified analyses revealed gender differences for the risk of work injury for respondents who remained in nonstandard shifts, but no differences between men and women who changed shift schedule (in either direction). Results showed that women had a significantly higher injury risk than men when remaining in nonstandard shifts. This finding adds to evidence from previous studies. It may be linked to differences in fatigue or other lifestyle demands (1, 19) or to differences in health and other occupational exposures. Recent studies have shown that women generally report poorer health, restrictions on performing daily activities and more chronic conditions than men (41). Gender differences across some industries, such as healthcare and manufacturing, may also result in different hazard exposures among men and women and influence the risk of work injury. Additional research is needed to pursue whether differences in injury risk are explained by gender, lifestyle factors (eg, care-giving and household responsibilities), the nature of the work experiences of women and men or other variables such as access to compensation for injury. Important to note is that there were no gender differences associated with switching shifts suggesting that the impact of changes in scheduling is equally disruptive and associated with elevated risks of injury for both women and men.
Within-gender analyses revealed that for men, increased injury risk was significant among those who recently switched from days to nonstandard shifts, but not among those who remained in nonstandard shifts. These findings suggest that for men, there may be an initial period of adjustment to working at night that increases their risk for injury, but over time the risks are diminished. For women, those who worked nonstandard shifts only were less likely to report a work injury as women who had recently started nonstandard shifts, but the risk of injury was still almost twice that of women who worked regular day shifts. Both sets of findings speak to the importance of implementing occupational health and safety policies and programs early after changes in shifts. They also point to the potential importance of greater awareness and health and safety action on an ongoing basis. Additional research is needed to examine whether this may be especially true among women.
This study has several limitations that should be addressed in future research. Our secondary analysis of administrative data did not allow us to explore what circumstances may have influenced a respondent to switch shift types. For example, switches to nonstandard shifts may have been voluntary or related to pay incentives, because of organizational changes or health factors. These same factors may have also influenced the risk of subsequent work-related injury. The strict inclusion criteria requiring responses from all six years of participation in the SLID to form the study population may have also influenced findings. A sensitivity analysis with the entire workforce population, regardless of response completeness, was not possible with these data. However, a comparison of demographic characteristics suggests that risks for work injury may have been underestimated given that the characteristics of our study population (ie, higher education and stable occupational situations) may have resulted in less hazardous working conditions than the general working population. Finally, the use of reports of workers’ compensation and work injury absences for >1 week is a more stringent proxy for work injury than most studies and may have excluded many types of acute injuries. By identifying work injuries with these criteria we have highlighted more severe injuries or claims. Some studies have shown that less than half of all workplace injuries are reported (42) and that the nature of the injury is related to absence duration, with acute traumatic injuries resulting in less time away from work than sprain and strain injuries (43). This may mean that our results underestimated the true risk for workplace injuries related to shift work and schedule change.
Despite some limitations, the longitudinal design of the survey allowed us to follow respondents over a 6-year period to examine the subsequent risk of work-related injury among different work schedules. The annual response to the survey also enabled the identification of changes in work schedules using a large representative sample of the Canadian labor force, with information provided from federal income tax forms for 96% of respondents. The findings highlight concerns about the risk of injury, not only among both men and women who switch from day to nonstandard shifts, but also about injury risks remaining elevated particularly among women who work nonstandard shifts for a prolonged period of time. In addition, the benefits of switching from nonstandard to day shifts may not reduce injury risk among men or women. These results have implications for health and safety programs and the need to develop additional strategies to help reduce injury risk among those who change shifts, as well as the need to provide awareness, training, and risk management efforts to reduce injuries on an ongoing basis.