Shift work (especially night work) is associated with more health-related problems, such as ischemic heart disease (1), gastrointestinal disorders (2), and metabolic disorders (3) as compared with day work. Shift work can be defined as fixed evening or fixed night work or variable working hours that include two- or three-shift work with combinations of day, evening, and night work.
Several explanations for the surplus of negative health outcomes among shift workers have been suggested. First, a certain degree of selection of employees with relatively poor lifestyle into shift work appears to take place (4, 5). Second, due to circadian disruption, shift work may lead to behavioral stress reactions (1, 6), such as smoking (4, 7, 8), weight gain (9–11) or physical inactivity (7). Third, shift workers are more exposed to unhealthy work factors, such as low job control, low influence on working hours, and low social support (12–14). In general, shift workers also report lower job demands, although higher cognitive demands and higher emotional demands have also reported (12, 13).
Previously, it has been argued that irregular working hours and shift work may limit the success (15), feasibility and sustainability (16) of workplace health promotion. Therefore, we suggest a fourth pathway from shift work to poor health, as we posit that workplace interventions aimed at improving the employees’ health and health behaviors (ie, workplace health promotion) do not reach shift workers to the same extent as day workers. More specifically, we suggest that both categories of health promotion are not available for shift workers to the same extent as it is for day workers, and that shift workers do not participate in health promotion to the same extent as day workers.
According to the World Health Organization, “Health promotion is the process of enabling people to increase control over, and to improve, their health” (17). Thus, health promotion is a rather broad concept, and, in the present study, we consider both primary prevention (ie, interventions that target risk factors before disease occurs) and secondary prevention (ie, interventions that target early stages of disease) (18, 19). Workplaces have been suggested as suitable arenas for health promotion with the aim of reaching large groups of individuals with similar needs and opportunities to change their health behavior. However, health behaviors may also be affected by circumstances in the working environment, and health promotion is increasingly being suggested to be an integrated part of occupational health activities (15).
Intuitively, if workplace health promotion takes place during day hours, these activities would be less available for shift workers. Furthermore, participation in workplace health promotion is suggested to be enhanced by support from colleagues and managers, and to be decreased by high perceived stress, high demands, and low control at work (20). Participation is also lower among physically inactive employees and employees with poor dietary habits (21). Thus, shift workers have several risk factors for non-participation in health promotion. Therefore, both in terms of availability and participation, there are likely barriers for interventions to reach shift workers. Still, results from previous research are mixed: two studies in the same population found higher participation in health promotion activities among shift workers (22, 23) and two other studies found lower participation among shift workers (24, 25).
Importantly, what may contradict our overall hypothesis of a lower availability of workplace health promotion among shift workers is that the European working hour directive states that night workers must regularly be offered a voluntary health assessment to detect shift-work related health problems at an early stage (26). In Denmark, this health assessment should take place before the employee takes up night work and at least every 3rd year hereafter. The health assessment should, as far as possible, take place during the employees’ usual working hours, and the employer is obliged to cover all expenses and reimburse any loss of income due to participation in the health assessment. The Danish working environment authorities recommend that this individual health assessment consists of general information about night work and potential health consequences. A health professional should provide this information, which should be followed by an individual screening questionnaire or consultation. The aim of this screening is to identify employees that need to be referred to a medical examination in the healthcare system. The results of the health assessment are confidential and must not be passed on to the employer, but still the employee has the right to be transferred to day work as soon as possible if he or she suffers from night work-related health problems (27). Due to this regulation, employees working night shifts might be expected to have a higher availability of and participation in health screenings or similar activities.
With this background, the overall aim of the present study was to investigate the association between shift work and the availability of and participation in workplace health promotion.
First, we studied whether the availability of and participation in workplace health promotion differed between day and shift workers in a representative sample of all employed people in Denmark. Second we studied whether any differences between day and shift workers were due to differences in the occurrence of workplace health promotion across job groups, and therefore we also analyzed a sub-sample consisting only of job groups undertaking shift work.
Shift work was defined as fixed evening work, fixed night work, variable working hours without night work, and variable working hours including night work. Availability of workplace health promotion was divided into activities taking place either during or outside working hours. The analyses of participation in workplace health promotion was restricted to those who were offered health promotion. We adjusted for differences in psychosocial work factors and health behaviors between day and shift workers.
Methods
Study population
We used cross-sectional questionnaire data from the 2010 survey of the Danish Work Environment Cohort Study (DWECS). DWECS consists of a random sample of about 21 000 individuals from the working population in Denmark aged 18–59 years drawn from the Central Population Register of Denmark. A total of 10 605 individuals (53%) participated in the survey.
In our total sample, all the 7555 individuals with non-missing information on working hours and all covariates were included. This sample comprised individuals from 87 job groups (the three biggest groups were office workers, N=452; salespersons, N=327; and school teachers, N=299) and 12 occupational sectors (the three biggest groups were social and health care, N=1587; industry, N=811; teaching and research, N=595).
In our sub-sample, we included job groups with representatives in each of the shift work categories. The study sample for the secondary analyses consisted of 2064 individuals with non-missing information on working hours and all covariates The following 16 job groups fulfilled the inclusion criteria: (i) care work in institutions N=221; 50% shift workers), (ii) family child minder (N=214; 18% shift workers), (iii) nurses (N=213; 51% shift workers), (iv) providers of care and help of elderly in their homes (N=194; 46% shift workers), (v) cleaning assistants (N=173; 22% shift workers), (vi) technicians within non-biological areas (N=162; 10% shift workers), (vii) care work and teaching handicapped people (N=150; 57% shift workers), (viii) self-employed (N=131; 20% shift workers), (ix) warehouse and harbor work (N=115; 27% shift workers), (x) other construction workers (N=99; 10% shift workers), (xi) skilled machine operator (N=97; 10% shift workers), (xii) operation of industry machinery and other unskilled employees (N=91; 31% shift workers), (xiii) manual manufacturing work (N=67; 25% shift workers), (xiv) office assistants and telephone operators (N=66; 26% shift workers), (xv) postmen (N=53; 30% shift workers), and (xvi) paper goods and printing trade-workers (N=18; 39% shift workers).
Availability of and participation in workplace health promotion
The participants were asked about initiatives and activities initiated by their workplace and directed at the individual’s needs and health behavior.
Availability of workplace health promotion during and outside working hours was determined by the question: “During the last year, have you been offered health promotion via your workplace?” The following six types of health promotion were mentioned: smoking cessation, healthy diet initiatives, exercise facilities, weekly exercise classes, contact to health professionals (physiotherapy, psychologist or the like), and health screenings. The response categories were “no”, “yes, during working hours” and “yes, outside working hours”. Participation in workplace health promotion was determined by the question “Have you applied it? (If you did, please mark)”. We included data on all types of health promotion that was available from the questionnaire, first because our a priori assumption was that there would be a general difference between day workers and shift workers with respect to the availability of and participation in workplace health promotion, and second because of the lack of empirical evidence that could guide us in focusing only on a few of them. The availability of and participation in all types of health promotion were analyzed separately.
Shift work
To measure exposure to shift work, we asked: “In your main occupation, which time of the day do you usually work?”. The participants were categorized into “fixed day work”, “fixed evening work (primarily between 15 and 24)”, “fixed night work (primarily between 24 and 05)”, “variable working hours without night work” (ie, day and evening work), and “variable working hours including night work” (ie, combinations of night and day and/or evening work). The distribution of shift work is presented in table 1.
Sociodemographic factors
Information about gender and age was obtained from the Civil Registration System. Information about job group and occupational sector was obtained from Statistics Denmark.
Work factors
The measures of psychosocial work factors were derived from the Copenhagen Psychosocial Questionnaire (28, 29). Influence (1 item) concerned influence over decisions about work. The response options were “always”, “often”, “sometimes”, “seldom”, and “never/hardly ever”. Emotional demands (2 items) concerned having to relate to other people’s problems at work, being brought into emotionally demanding situations, and getting emotionally affected by the work. The response options were “to a very large extent”, “to a large extent”, “somewhat”, “to a small extent”, “to a very small extent”. Quantitative demands (3 items) concerned unevenly distributed work that piles up, whether you do not succeed to complete all your work tasks, and whether it is necessary to work overtime. Pace demands (1 item) concerned whether it is necessary to work very fast. The response options were “always”, “often”, “sometimes”, “seldom”, and “never/hardly ever”. Social support from colleagues (2 items) concerned the opportunity to get help and support from colleagues, and colleagues being willing to listen to problems at work. Social support from leaders (2 items) concerned the opportunity to get help and support from your nearest supervisor, and your nearest supervisor being willing to listen to problems at work. The response options were “always”, “often”, “sometimes”,” seldom”, “never/hardly ever”, and “not relevant”.
For each of the items, a score ranging from 0–100 was calculated according to the guidelines (28, 29). For the statistical analyses, we used the 1-item scale of influence, made a sum score of the three measures of job demands (ie, emotional, quantitative, and pace demands), and made a sum score of the two measures of social support (ie, social support from leaders and colleagues).
Health behavior
Smoking status was categorized into seven categories: 1=non-smokers, 2=ex-smokers, 3=1–5 cigarettes/day, 4=6–10 cigarettes/day, 5=11–15 cigarettes/day, 6=16–20 cigarettes/day, and 7=≥21 cigarettes/day.
Fruit and vegetable intake was measured with the question “How often do you eat fruit, salad/uncooked vegetables, boiled vegetables—except potatoes?” with the six response options 1=≥3 times daily, 2=twice daily, 3=once daily, 4=3–6 times weekly, 5=1–2 times weekly, and 6=more seldom.
Leisure-time physical activity was measured as a combination of intensity and duration by the question “How much time have you spent on each of the following leisure-time activities during the last year (include also commuting to and from work)?” with the following sub-questions: (i) “Walking, biking or other low-intensity exercise, in which you don’t get short of breath or sweat (ie, Sunday walks or low-intensity gardening)?” (ii) “Exercise training, heavy gardening, or higher intensity walking/biking, in which you sweat and get short of breath?” (iii) “Strenuous exercise training or competitive sports?” For each sub-questions the response options were “>4 hours per week”, “2–4 hours per week”, “<2 hours per week” or “do not carry out the activity”. We calculated an index by multiplying intensity (1–3) and duration (0–3), eg, a participant that did low-intensity exercise >4 hours/week and strenuous exercise training <2 hours/week had an exercise score of 1×3+3×1 = 6. The score, thus, increased with increasing intensity and duration of leisure-time physical activity.
Body mass index (BMI) was calculated by dividing weight in kilograms with squared height in meters (both weight and height were self-reported).
Statistical analysis
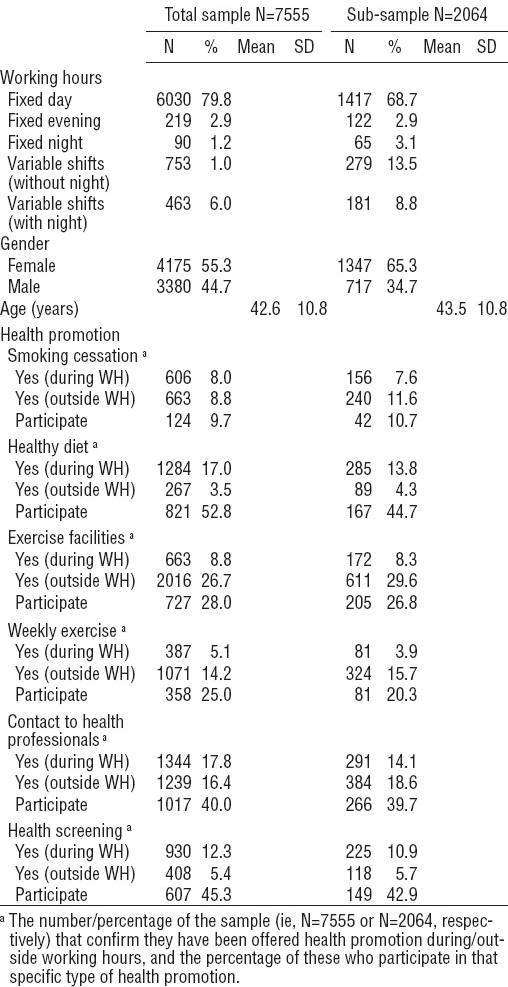
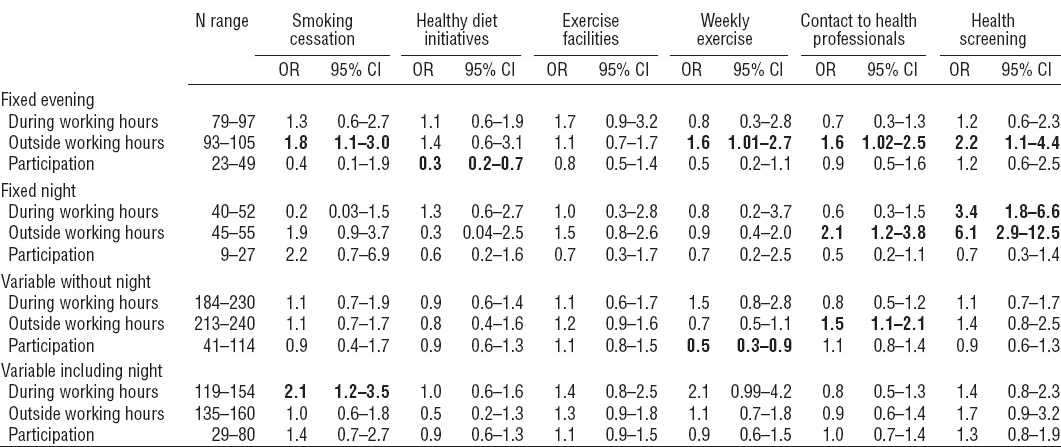
First, we described the study population, ie, the total sample and the sub-sample (table 1). Second, using binary logistic regression, we analyzed the association between shift work and availability of health promotion during and outside working hours in the total sample (table 2) and in the sub-sample (table 3). Third, using binary logistic regression, we analyzed the association between shift work and participation in health promotion among those to whom the specific type of health promotion was available (tables 2 and 3). The associations were adjusted for gender, age, work factors, and health behaviors. Gender was a categorical variable. Age, influence, job demands, social support, smoking, fruit and vegetable intake, leisure-time physical activity, and BMI were analyzed as continuous variables. The results for the total sample are presented in table 2 and the results for the sub-sample are presented in table 3. The effects are estimated as odds ratios (OR) and their 95% confidence intervals (95% CI). We used IBM SPSS Statistics 20 (IBM Corp, Armonk, NY, USA) for all analyses.
Table 2
The table shows the association between shift work and the availability of workplace health promotion during and outside working hours in the total sample consisting of 7555 employed people. The table also shows the association between shift work and participation among those to whom workplace health promotion was available. The reference group is day workers (not shown), and the analyses are adjusted for age, gender, influence, job demands, social support, smoking, fruit and vegetable intake, leisure-time physical activity, and body mass index. Significant estimates are written in bold face. The range of the N for the day workers was 4486–5125 (“During working hours”), 4606–5222 (“Outside working hours”), and 1274–2592 (“Participation”). [OR=odds ratio; 95% CI=95% confidence interval.]
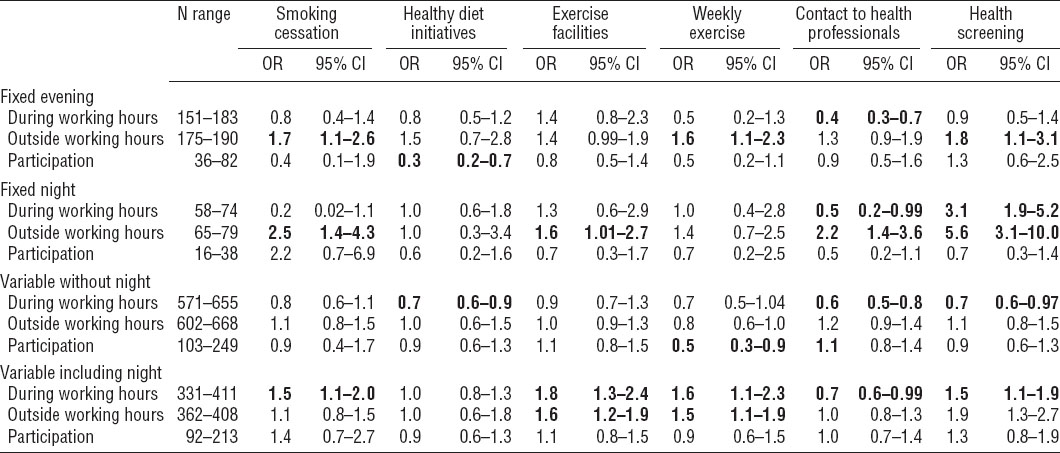
Table 3
The table shows the association between shift work and the availability of workplace health promotion during and outside working hours compared to day workers in the sub-sample consisting of 2064 people employed in job groups undertaking shift work. The table also shows the association between shift work and participation among those to whom workplace health promotion was available. The reference group is day workers (not shown), and the analyses are adjusted for age, gender, influence, job demands, social support, smoking, fruit and vegetable intake, leisure-time physical activity, and body mass index. Significant estimates are written in bold face. The range of the n for the day workers was 974–1156 (“During working hours”), 1053–1180 (“Outside working hours”), and 220–499 (“Participation”). [OR=odds ratio; 95% CI=95% confidence interval.]
Results
In both samples, day workers were the majority (79.8% and 68.7%) (table 1). Females constituted 55.3% of the total sample and 65.3% of the sub-sample, and the mean age was 42.6 years and 43.5 years, respectively.
Availability of and participation in health promotion
Fixed evening work
In the total sample (table 2), we found that among fixed evening workers “contact to health professionals” was less available during working hours. Outside working hours, three types of health promotion, ie, “smoking cessation”, “weekly exercise”, and “health screening”, were more available. Fixed evening workers’ participation in health promotion was not significantly different from day workers’ participation except for a lower participation in “healthy diet initiatives”.
The analyses in the sub-sample (table 3) also pointed to a higher availability of several types of health promotion outside working hours among fixed evening workers. Additionally, in these analyses fixed evening workers and day workers were not statistically significantly different with respect to availability of health promotion during working hours and participation in health promotion.
Fixed night work
In the total sample (table 2), we found that among fixed night workers “contact to health professionals” was less available and “health screening” was more available during working hours. Outside working hours, four types of health promotion, ie, “smoking cessation, “exercise facilities”, “contact to health professionals”, and “health screening”, were more available among fixed night workers as compared with day workers. The participation in health promotion did not differ significantly between fixed night workers and day workers.
The analyses in the sub-sample (table 3) pointed to a higher availability of “health screening” during working hours and a higher availability of “contact to health professionals” and “health screening” outside working hours among fixed night workers. In the sub-sample, fixed night workers did not differ significantly from day workers with respect to participation in health promotion.
Variable shifts without night work
In the total sample (table 2), we found that – among employees working variable shifts without night work – three types of health promotion (ie, “healthy diet initiatives”, “contact to health professionals”, and “health screening”) were less available during working hours compared with day workers. We found no significant differences with respect to availability of health promotion outside working hours. Employees working variable shifts without night work had a lower participation in “weekly exercise” compared with day workers.
The analyses in the sub-sample (table 3) did not support a lower availability of health promotion during working hours among employees working variable shifts without night work. Also in contrast to the analyses in the total sample, we found a higher availability of “contact to health professionals”. We found no statistically significant differences with respect to participation in health promotion.
Variable shifts including night work
Among employees working variable shifts including night work, “contact to health professionals” was less available during working hours, whereas four types of health promotion (ie, “smoking cessation”, “exercise facilities”, “weekly exercise”, and “health screening”) were more available. “Exercise facilities” and “weekly exercise” were also more available outside working hours. The participation in health promotion did not differ between employees working variable shifts including night work and day workers.
The analyses in the sub-sample (table 3) only supported a higher availability of “smoking cessation” during working hours, but did not support the remaining differences between employees working variable shifts including night work and day workers.
Discussion
Main findings
Overall, contrary to our initial hypothesis, the present study could not confirm that shift workers in general report a lower availability of and participation in workplace health promotion.
The three main findings of the present study are that (1) in the general working population, fixed evening workers, fixed night workers, and employees with variable working hours including night work reported a higher availability of workplace health promotion and employees working variable shifts without night work reported a lower availability of health promotion as compared with day workers; (2) in job groups undertaking shift work there are few statistically significant differences between day workers and shift workers, and these few differences appear to favor shift workers, ie, they reported a higher availability of workplace health promotion primarily outside working hours; (3) in general, there was no statistically significant differences between day workers and shift workers with respect to their participation in health promotion once it was available to them.
The essence of the differences obtained from the total sample and the sub-sample is that when studying the general working population shift workers appear to differ from day workers, however, when comparing shift workers and day workers specifically within job groups undertaking shift work, the differences are less pronounced.
Regarding availability of health promotion during and outside working hours, we tentatively suggest that when health promotion is available to shift workers it is primarily outside their working hours. Furthermore, in some instances a higher availability of health promotion outside working hours occurred concurrently with an (insignificantly) lower availability of health promotion during working hours, eg, in the case of “smoking cessation” and “contact to health professionals” among fixed night workers. However, the timing of health promotion and its effect on participation needs further investigation. Also, the apparent differences between different types of shift system with respect to the availability of health promotion indicated in the results of the total sample needs further investigation before any clear inferences can be made.
Comparison with previous findings
We were not able to identify other studies that specifically investigated the association between shift work and the availability of health promotion. However, we suggest that our findings indicate an increased public attention on shift workers’ health and health behaviors. Thus, health promotion may more frequently be targeting job groups undertaking shift work.
Night workers’ legally secured right of regularly offered health assessments (26, 27) may explain our finding that fixed evening and fixed night workers (both samples) and employees working variable shifts including night work (the total sample) were more frequently offered health screening. Nevertheless, it appears that the health screening frequently occurs outside working hours, although the Danish working environment authorities state that the activities included in the night-work induced health assessments should preferably take place during the employee’s usual working hours. Still, financial barriers for participation in health screening as part of the health assessment program should be minimal, as the employer is obliged to cover all expenses and also reimburse loss of income (27).
Importantly, the available data do not enable us to distinguish between health screenings initiated as part of night work-related health assessment, and health screenings initiated for other reasons and with other aims than identifying night work-related health problems. Furthermore, our questionnaire contained no information about the extent to which the employer covered expenses related to the different types of workplace health promotion, and whether participants were offered regular salary during their participation. It is, however, fortunate that health promotion appears to reach shift workers as it may be especially important for this group of employed people. For example, observational studies suggest that the combination of shift work and hazardous health behaviors such as smoking, obesity, and physical inactivity interacted synergistically with regard to their negative effect on cardiac modulation (30), coronary heart disease (31), and daytime sleepiness and insomnia (32). Additionally, changes in dietary habits and physical activity are suggested as means to alleviate the potential disruption of circadian rhythms associated with some shift schedules (3, 33). Four of the six types of health promotion under study addressed “classic” types of health behaviors (smoking, dietary habits, and physical activity) and could be described as primary prevention. Two of the six types of health promotion under study were more likely to address health problems at an early stage (contact to health professional and health screening) and could thus be described as secondary prevention. Therefore, workplaces can play a role both as a health determinant and as a setting for preventive activities (34) not only targeting work-related issues but physical and mental health in a broader sense. However, we do not know to what degree the health promotion activities in the current study were integrated in existing occupational health practices.
Only a few previous studies have investigated differences between day and shift workers with respect to their participation in health promotion. A 2009 review of determinants of participation in workplace health promotion programs (35) reported that out of 23 studies, only one study reported the association between shift work and participation. In that study, swing and graveyard shift workers were less likely to complete the 8-week program including exercise, nutrition, hypertension, and smoking cessation than day workers (36).
The findings from a comprehensive medical program targeting shift workers at a chemical plant were reported. Among other things, the program included medical examinations and health promotion retreats and it was found that, compared with day workers, shift workers participated in more health seminar days (0.68 versus 0.31 days) and more examinations (0.98 versus 0.50 examinations) per work year (22). Using the same study population, it was also reported that 47% of the shift workers and 27% of the day workers attended a 1–3 weeks health seminar program (23). Therefore, when health promotion is directly targeting shift workers, a high degree of participation can be obtained. On the other hand, in a report of the reach of a multi-faceted workplace health promotion and work environment intervention, it was found that shift workers were less inclined to participate in a 30-minutes information meeting about the project. To counteract potential selection of employees into the study, about 40 information meetings were held at different times of the day and written information was provided for employees not present. However, despite these efforts, shift workers were less inclined to give their consent to participate in the study (25).
Nevertheless, contrary to our hypothesis, the present study could not confirm that shift and day workers in general differ regarding their participation in workplace health promotion once it is available to them.
Strengths and limitations
The study population consisted of employed people from various job groups and sectors and this heterogeneity of the study sample can be thought of as both a strength and a limitation. On the one hand, we were able to study the association between shift work and health promotion in the general working population. On the other hand, the heterogeneity increases the risk of bias due to residual and unmeasured confounding. To overcome the shortcomings related to the lack of comparability between shift workers and day workers in the general working population, we also analyzed the association between shift work and health promotion in a sample restricted to job groups that were all undertaking shift work. Hereby, we reduced the degree to which the reference group is “contaminated” by job groups consisting (almost) exclusively of fixed day workers. The inevitable consequence was reduced statistical power, as especially the groups of fixed evening workers (N=122) and fixed night workers (N=65) became even smaller. This explains the wide confidence intervals around the OR and may have resulted in type II errors.
All variables in the present study were measured by self-reports. Therefore, the notion of “health promotion” was open for interpretation, and we were only able to study health promotion of which the employees were aware. Sometimes workplace interventions aimed at affecting behavior is implemented in a form not necessarily considered by the employees as health promotion (for example, changing the offers of the canteens and vending machines, prohibiting smoking at the workplace’s premises, or offering the employees a bike for commuting). In such cases, health promotion may be misclassified, as some employees may report availability of and participation in health promotion and other employees may not. We would suspect such misclassification to increase the risk of type II error, unless the misclassification is differential between day workers and shift workers which increases the risk of type I error. If differential misclassification was the case, employees working variable shift without night work would systematically under-report the availability of and participation in health promotion while employees working variable shifts including night work would systematically over-report the availability of and participation in health promotion in order to spuriously create the associations observed in the present study. However, we have no reason to believe such a difference in misclassification.
Another limitation related to our lack of knowledge about the more specific content of the six types of health promotion. Although workplace health promotion can affect health behaviors to some extent (37–39), we cannot empirically demonstrate that all the health promotion activities reported in the present study would have the same effects. Thus, although we may tentatively suggest that a 50% reduction or a doubling in the OR when comparing shift with day workers constitutes a relevant difference between the groups, we cannot know whether such differences would eventually influence disparities in morbidity between day and shift workers.
Also the exposure (shift work) was self-reported, and to limit the degree of individual interpretation the definition of “evening” and “night” was specified (primarily 15:00–24:00 hours and 24:00–05:00 hours, respectively). Still, we do not know if, for example, knowledge workers with flexible working hours would categorize themselves according to their office hours or according to the degree to which they work from home during the evening and/or night. Similarly, the validity of the remaining variables in the study (eg, psychosocial work factors and health behaviors) may be influenced by individual interpretation, misunderstandings, and recall bias. The direction of these biases is, however, difficult to predict.
Due to the cross-sectional design, we cannot study shift work as a cause of the availability of and participation in health promotion. First, as previously mentioned, the findings in the total sample may be due to confounding by the job groups and sectors which primarily provided participants to the group of day workers (eg, for 23 of the group groups <10% were shift workers). Thus, despite that we adjusted the results for influence, job demands, and social support, we cannot isolate the effect of shift work from the effect of the job and the arena within which the job is performed.
Next, also selection into shift work should be considered as an explanation for differences in the availability of and participation in health promotion. Previous research has shown that some degree of health behavior-related selection into shift work takes place (4, 5). However, we found differences in the availability of health promotion even after adjustment for smoking, dietary habits, leisure-time physical activity, and BMI. Importantly, this may also be considered “over adjustment” as shift work has also been shown to affect health behaviors (4, 7–11) which should then be treated as mediators and, furthermore, health behaviors may obviously be affected by workplace health promotion. Therefore, our results could be considered conservative estimates of the association between shift work and health promotion. With respect to participation, we only observed a few statistically significant differences between day and shift workers. Therefore, the results of our study could not confirm that shift and day workers differ profoundly with regard to their interest in health promotion once it is available to them.
Finally, reverse causality is a potential explanation for observed associations in cross-sectional studies. Still, we consider it unlikely that the outcome (ie, availability/participation) would act as a cause of exposure to shift work.
Concluding remarks
The present study did not confirm our initial hypothesis that workplace health promotion reached shift workers to a lesser extent than day workers. Instead, we found that, in the general working population, individuals working shifts reported a higher availability of workplace health promotion, except for those working variable shifts without night work. In the sample restricted to job groups with representatives in all shift work exposure categories, the differences between day and shift workers were less pronounced, and the few differences pointed to a higher availability of workplace health promotion among shift workers. Overall, day and shift workers did not differ significantly with respect to their participation in workplace health promotion once it was available to them. Thus, the present study shows that – to some extent – workplace health promotion targets the unfortunate health profile of shift workers.