Depressive disorders are characterized by the co-occurrence of specific symptoms, with core symptoms of depressed mood, loss of interest and enjoyment, and feelings of fatigability and diminished energy (1, 2). A depressive episode, also called unipolar or major depressive episode, is typically time limited, however recurrence rates are high (3). Twelve-months prevalence in the general population is estimated to be at about 6–7% (4, 5). Depressive disorders are highly disabling and a leading cause of years of life lost to disability (6).
The etiology of depressive disorders is complex and not well understood, likely involving the interplay of social, psychological and biological factors that act across the life-course (7–9). Whether exposure to adverse working conditions contributes to this complex etiology is controversially debated (10).
The model of effort–reward imbalance at work (ERI) entered the international scientific discussion in the 1990s and is today one of the most widely used theoretical models for conceptualizing the potentially health-hazardous effects of the psychosocial work environment (11, 12). The model posits that a lack of reciprocity between high “costs” (spending high effort at work) and low “benefits” (in terms of monetary gratifications, career opportunities, esteem, respect, and job security) produces emotional distress affecting both mental and physical health. Whereas the main focus of the model is on the work environment, it also includes a personal disposition, called “over-commitment” that is thought to moderate the health effects of ERI (11).
For several reasons, an association of ERI and risk of depressive disorders may be plausible. First, the recurrent experience that effort is not matched by adequate rewards may lead to feelings of humiliation and deteriorating self-esteem, which are considered important psychological processes in the development of depressive disorders (13–16). Second, being forced to remain in a situation of high effort and low reward at work, for example because of lack of alternative choice in the labor market, may evoke recognitions of entrapment and learned helplessness, two psychological phenomena that had been discussed as possible pathways leading to depressive disorders (14, 15, 17). Third, some studies indicated that ERI may lead to dysregulation of the hypothalamic-pituitary-adrenal (HPA) stress axis (18) that is one of several biological pathways considered in the etiology of depressive disorders (19–21).
Although ERI may be a plausible risk factor for onset of depressive disorders, the epidemiological evidence provided in systematic reviews and meta-analyses to date is insufficient for drawing a firm conclusion. The first systematic reviews and meta-analysis on psychosocial working conditions and mental health was published by Stansfeld and Candy in 2006 (22) and reported an association of ERI with risk of “common mental disorders”, an umbrella term including but not limited to depressive disorders. Subsequent reviews in 2008 by Bonde (23) and Netterstrøm et al (24) focused on work environment and depressive disorders but could not identify a sufficient number of studies for ERI. This was echoed in the most recent comprehensive review of psychosocial work environment and depressive disorders published by Theorell et al in 2015 that covered the literature until June 2013 and identified only three articles examining ERI and depressive disorders with a prospective cohort study design of sufficient quality (25).
In August 2016, our research group published a book chapter on ERI and affective disorders (9) that included an electronic literature search in the Pubmed medical study database until July 2nd, 2015. Although we searched for all types of affective disorders (eg, unipolar depression, bipolar disorders, cyclothymia), we only found studies on depressive disorders. The results indicated that ERI was associated with an increased risk of depressive disorders. However, we did not systematically assess the quality of the studies and did not pool the study-specific estimates in a meta-analysis.
Aim of this article
In this article, we present the results of a new literature search (including literature published until 1 October 2016) that is focused on ERI and risk of depressive disorders, extends the literature search by including several electronic databases, assesses the quality of the studies by a standardized quality assessment tool, and presents a meta-analysis of the study-specific estimates together with several sensitivity analyses.
The primary objective of this article is to determine whether employees who are exposed to ERI at work have a higher risk of depressive disorders compared to employees who are not exposed. Only results from prospective cohort studies are included in the review and meta-analysis.
The secondary objective of this article is to explore whether the possible association of ERI and risk of depressive disorders is stronger or weaker in studies (i) of high versus studies of low quality, (ii) using the original ERI questionnaire versus studies using proxy measures, and (iii) ascertaining depressive disorders with self-administered rating scales versus studies ascertaining depressive disorders with other methods.
Methods
Protocol and registration
We conducted this review in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (26). Before the literature review commenced, we registered and published the protocol of the study on the PROSPERO (International prospective register of systematic reviews) website on 14 September 2016 (registration number: CRD42016047581, www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42016047581) (27).
Eligibility criteria
Studies were eligible if they were published in a peer-reviewed scientific journal and fulfilled the following criteria: (i) the design was a prospective cohort study of economically active individuals with ERI as the exposure and depressive disorders as the outcome; (ii) ERI was ascertained at baseline; (iii) depressive disorders were ascertained both at baseline and during follow-up; (iv) the analyses either excluded or adjusted for baseline cases of depressive disorders; (v) the study provided a measure of relative risk [eg, odds ratio (OR), hazard ratio (HR) with 95% confidence intervals (95% CI)] of onset of depressive disorders comparing individuals with high ERI exposure to individuals with low ERI exposure. Studies were also included, if they did not provide a measure of relative risk, but provided information that allowed us to calculate such a measure; and (vi) the study was published in a peer-reviewed scientific journal and in a language that was accessible for us (English, German, Danish, Norwegian, Swedish, French, Spanish).
We excluded studies that had a cross-sectional, case–control, case study or intervention design, did not exclude or adjust for baseline cases and did not analyze onset of depressive disorders but instead examined depressive symptoms as a continuous variable.
Ascertainment of ERI
To be eligible, the study had to provide a quantitative baseline assessment of exposure to ERI, as defined in Siegrist’s ERI model (11, 12). The assessment had to be done with either the original ERI questionnaire or proxy measures that were chosen with the intent to measure ERI. Exposure could be reported as a binary variable (yes/no), a categorical variable (eg, high, medium, low) or a continuous variable (eg, one standard deviation increase on the ERI scale). Studies were excluded, if they (i) did not provide a quantitative assessment of ERI, (ii) assessed aspects of ERI but did not refer to the ERI model, or (iii) assessed effort or reward or both but did not provide a combined measure of ERI.
Ascertainment of depressive disorders
Depressive disorder had to be documented by (i) a psychiatric diagnostic interview, (ii) a diagnosis by a physician, (iii) register data (eg, dispensing of antidepressants, hospital discharge records, administrative data (eg, disability pensioning) with diagnosis of depression); or (iv) a self-administered rating scale that was validated against a clinical measure of depression and that dichotomized respondents into cases versus non-cases.
Search strategy
We searched published studies through a systematic review of the electronic databases PubMed (“All Fields”), PsychInfo (“Any Fields”) and Web of Science Core Collection Database (“Topic”) from inception to 1 October 2016. The search string is listed in e-Appendix 1 (www.sjweh.fi/index.php?page=data-repository). We further scrutinized the reference lists of the eligible articles and of seven previous major reviews (22–25, 28–30) and our own article collections. Finally, we searched the Web of Science citation database for all articles that had cited any of the eligible articles.
Study selection
After exclusion of duplicates, two authors independently screened all titles and abstracts to determine preliminary eligibility. In case of uncertainty, the article in question was retained. Both authors read all preliminarily eligible articles in full to determine final eligibility. Disagreements were resolved through discussion.
If more than one study came from the same study population, we applied a selection that was pre-defined in the study protocol (27). If the studies were virtually redundant, then we selected the study that had the primary aim of analyzing the association of ERI and depressive disorders and excluded the study where this analysis was the secondary aim. If studies used different ERI measures or different depressive disorder measures, we included both studies in the main analysis and examined in additional analyses how the results changed when only one of the studies was included.
Data extraction
From each eligible article, we abstracted the following information: name of first author, publication year, cohort name, study location (country), number of participants, population characteristics (segment of workforce, age, proportion of women), method of ERI and depressive disorder ascertainment, lengths of follow-up, covariates included in the least adjusted model, covariates included in the most adjusted model, number and proportion of cases at follow-up, estimate and 95% CI in the least adjusted model, estimate and 95% CI in the most adjusted model. The first author abstracted the study information and the other two authors checked the information against the original articles. We did not contact the authors of the studies to obtain additional estimates, but exclusively relied on the estimates that were reported in the published articles. In two cases, though, we contacted the authors to obtain descriptive information (number of participants at risk and number of cases) that were missing in the article.
Risk of bias in individual studies
The first and last author independently rated the quality of each included study using the Newcastle-Ottawa scale (31) recommended by the Cochrane Collaboration group for the quality assessment of observational cohort studies (32). The scale assesses quality with regard to the domains “selection”, “comparability” and “outcome”. A detailed description of the scale is provided in e-Appendix 2 (www.sjweh.fi/index.php?page=data-repository). Any differences in the ratings were resolved through discussion.
Statistical procedures in the meta-analysis
To obtain a summary estimate for the association of ERI with risk of depressive disorders, we pooled the log-transformed most-adjusted study-specific estimates and their standard errors in both a fixed-effects and random-effects meta-analysis using the “metan” command (33) in the statistical software package Stata (version SE 14.1, StataCorp, College Station, TX, USA). We further conducted fixed- and random-effects meta-analysis with the least-adjusted study-specific estimates. We used the Mantel-Haenszel method (34) to conduct fixed-effects meta-analysis and the DerSimonian and Laird method (35) to conduct random-effects meta-analysis. As per the study protocol, the interpretation of the results was based on the random-effects meta-analysis of the most-adjusted estimates. The extent of heterogeneity was assessed by calculating the I2, as recommended by Higgins et al (36).
Sensitivity analyses
As pre-defined in the study protocol (27), we calculated additional random-effects meta-analyses for comparing (i) high quality studies with low quality studies, (ii) studies using the original ERI questionnaire with studies using proxy measures, and (iii) studies assessing depressive disorders by self-administered rating scales with studies using other methods.
Results
Study selection
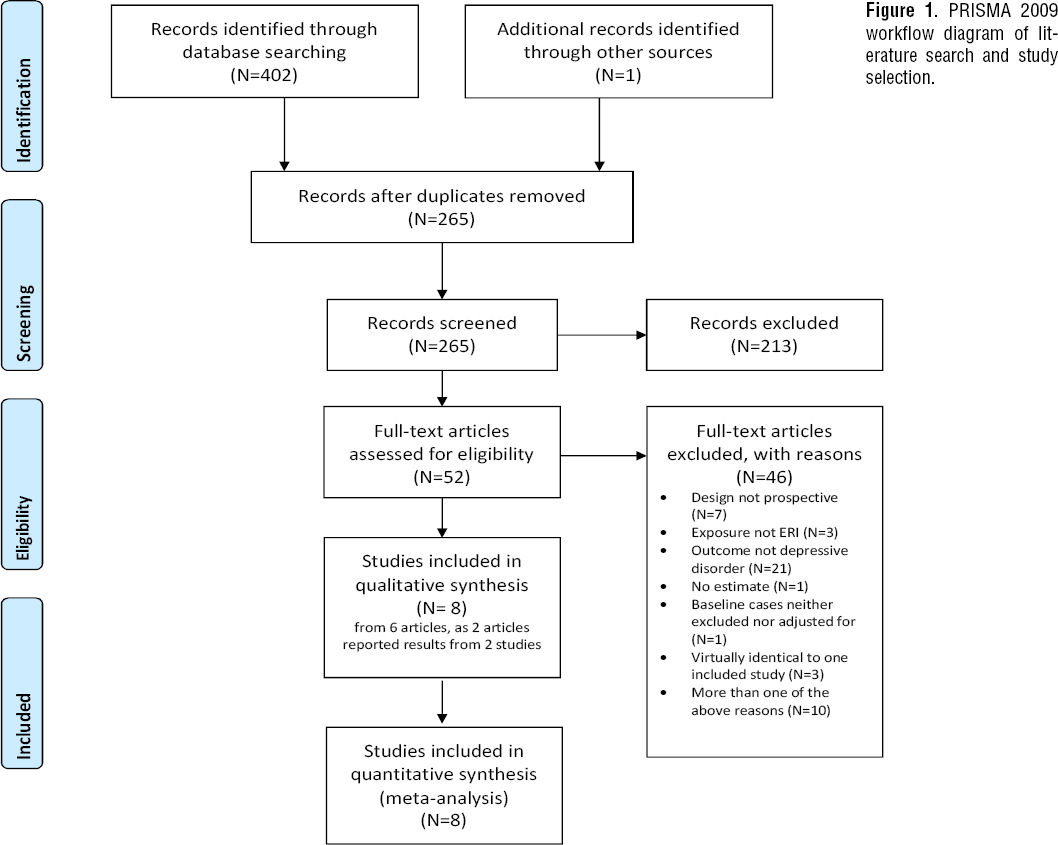
Figure 1 shows the flow diagram of the literature search and the selection of the studies. The electronic searches resulted in 402 articles (108 in Pubmed, 84 in PsychInfo and 210 in Web of Science), which were reduced to 264 after removal of duplicates. The hand search resulted in one additional article. Of those 265 articles, 52 were deemed as preliminary eligible after screening of titles and abstracts. After fulltext reading, eight studies from 6 articles remained eligible (39–44), as the Kivimäki et al (39) and Siegrist et al (42) articles each reported results from two independent studies.
The main reason for excluding studies after fulltext reading was that the study had not examined depressive disorders but either depressive symptoms, measured as a continuous score, or other forms of mental health problems (see figure 1 for details on reasons for exclusion). Four articles presented overlapping analyses from the same research project (42, 45–47). In accordance with the study protocol (27), we retained the one that had the main aim of analyzing the association of ERI with depressive disorders (42) and excluded the others that had the main aim of analyzing effect modification (45, 46) and mediation (47).
On 18 November 2016, we searched the Web of Science core collection citation database and identified 148 articles that had cited ≥1 of the 6 eligible articles. After screening of titles and abstracts, 17 articles were selected for further fulltext reading but none fulfilled the selection criteria.
Study characteristics
Table 1 shows the main characteristics of the eight studies from the six articles included in the review. The studies were published between 2007 and 2016 and were conducted in Finland (N=3), Denmark (N=2), Canada (N=1), USA (N=1) and in a multinational dataset of 12 European countries (N=1). Three studies examined general workforce employees, two studies general workforce employees who were ≥50 years and three studies were restricted to employees from the public sector. Taken together, the eight studies examined 84 963 individuals and identified 2897 (3.4%) cases of new onset of depressive disorders.
Table 1
Study characteristics ordered by online publication date. Characteristics of participant refers to the sample that was used in the analysis with the most-adjusted model when this information was available, otherwise this refers to the basic sample. Number at risk and number of cases at follow-up for #05 and #06 was retrieved by email communication from the authors. [10-Town=10 Town Study; ATC=anatomical therapeutic chemical classification; CES-D short=short version of the Center for Epidemiologic Studies Depression Scale; CIDI=World Health Organization composite international diagnostic interview; DWECS=Danish Work Environment Cohort Study; ELSA=English Longitudinal Study on Ageing; ERI-Q full/short=effort–reward imbalance questionnaire as developed by Siegrist and colleagues (full version/short version); EURO-D=European Depression Scale; FHPS=Finnish Hospital Personnel Study; FPSS=Finnish Public Sector Study; HRS=US Health and Retirement Study; ICD-10=World Health Organization International Statistical Classification of Diseases and Related Health Problems, 10th version; LCWPA=longitudinal cohort from the working population of the province of Alberta; MHI-5=5-item Mental Health Inventory of the Short-Form 36 item (SF-36) Questionnaire; Proxy=proxy measure of ERI with items/scales other than the ones in the ERI-Q (number of items to measure effort and reward); SHARE=Survey of Health, Ageing and Retirement in Europe.]
All studies ascertained ERI by self-report – either using the original ERI questionnaire (N=3) or proxy measures (N=5).
Depressive disorders were ascertained by scoring above a cut-off point on a self-administered rating scale (N=3), self-reported doctor diagnosed depression (N=2), a clinical diagnostic interview (N=1), an ICD-10 diagnostic code attached to a granted disability pensioning (N=1), and registered purchase of antidepressant medication (N=1).
There was some overlap between the included studies. Two studies that were analyzed separately from each other in the article by Kivimäki et al (ID #01 and #02) were collapsed in the study by Juvani et al (ID #07). We retained all three studies, because the two by Kivimäki et al analyzed the association of ERI on the individual-level with risk of doctor-diagnosed depression, whereas the study by Juvani et al analyzed the association of both individual and work-unit level of ERI with risk of disability pensioning. Further, the samples only partially overlapped as Kivimäki et al analyzed samples of 13 825 and 4090 employees respectively, whereas Juvani et al analyzed a much larger sample of 51 874 employees.
The Rugulies et al (ID #04) and Nielsen et al (ID #08) studies both analyzed ERI and depressive disorders in the Danish Working Environment Cohort study. We kept both studies because depressive disorders were assessed by a self-administered rating scale in the Rugulies et al study and by purchase of antidepressant medication in the Nielsen et al study. Further, the two samples only partially overlapped as Rugulies et al and Nielsen et al included 2701 and 4541 participants, respectively.
Risk of bias in individual studies
The quality score for the eight studies is provided in e-table 1 in e-Appendix 3 (www.sjweh.fi/index.php?page=data-repository). There were two studies of high quality, two of moderate quality, and four of low quality. The reason for low quality assessment was in the outcome domain, where all studies deemed as low quality had a combination of self-reported outcome assessment with a loss of follow-up of >20% (or failure to report percentage of loss).
Study-specific estimates on the association of ERI and depressive disorders
Table 2 shows the least- and the most-adjusted study-specific estimates for the association of ERI and depressive disorders in the eight included studies. ERI scores were divided into quartiles in six studies and tertiles in two. OR were estimated in six studies and HR in two.
Table 2
Effort-reward imbalance (ERI) and risk of depressive disorders. Studies #05 and #06 provided estimates after adjustment for cases with depressive disorders at baseline and also estimates after exclusion of cases with depressive disorders at baseline. These estimates were, as expected, highly similar. We selected the estimates after exclusion of cases with depressive disorders at baseline as this was in agreement with the approach used in the other studies. [See table 1 for other abbreviations.]
Seven of the eight studies indicated that ERI predicts depressive disorders, with estimates ranging from 1.49 (95% CI 1.22–1.81, ID #01) to 2.32 (95% CI 1.14–4.73, ID #03) when comparing the groups with the highest exposure to ERI to the reference group in the most-adjusted analyses. One study (ID #08) showed the opposite result, suggesting no association in the least-adjusted model (1.00, 95% CI 0.73–1.37) and a reduced risk, albeit not statistically significant, in the most-adjusted model (0.80, 95% CI 0.57–1.11).
Two studies (ID #01 and #04) reported a dose–response association between increasing ERI and increasing risk of depressive disorders, one study found a dose–response association in the least- but not the most-adjusted model (ID #02), and the remaining five studies did not report dose–response analyses.
One study (ID #07) aggregated the self-reported ERI scores to the work-unit level and reported an association of ERI with risk of depressive disorders in both the individual and the work-unit level analysis. In the following meta-analysis, we used the work-unit-level estimate as this is likely a more conservative estimate than the individual-level estimate, ie, less vulnerable to reporting bias and bias away from the null hypothesis, but more vulnerable to non-differential exposure misclassification.
Pooling estimates in a meta-analysis
Figure 2 shows the forest plots for the eight most-adjusted study-specific estimates comparing risk of depressive disorders among participants with the highest exposure to ERI among participants with the lowest exposure.
Figure 2
Random-effects meta-analysis of the prospective association between effort-reward imbalance and onset of depressive disorders based on the most-adjusted study-specific estimates.
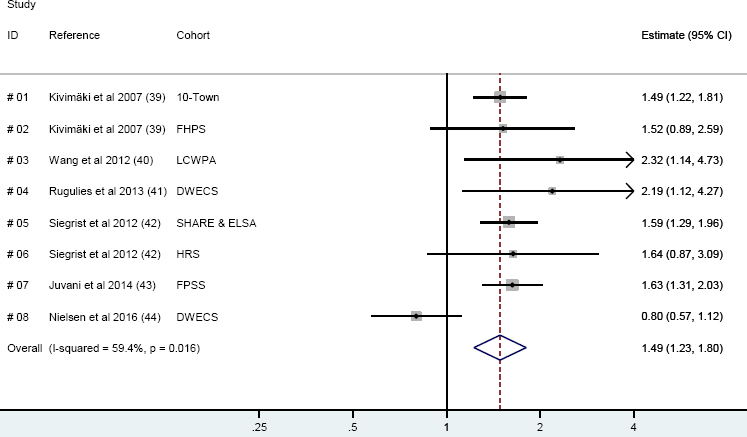
The pooled estimate of all eight studies was 1.49 (95% CI 1.23–1.80, P<0.001) in the random-effects meta-analysis indicating that ERI predicts risk of depressive disorders. Heterogeneity was high with an I2 of 59%. This heterogeneity was exclusively due to one study, which suggested that ERI was associated with a reduced risk of depressive disorders (ID #08). If this study was excluded, I2 was 0% (data not shown).
When we used fixed- rather than random-effects meta-analysis, the pooled estimate was identical to that in the random-effects analysis but with more narrow confidence intervals (1.49, 95% CI 1.34–1.65, P<0.001, data not shown).
Alternative study-specific estimates in the meta-analysis
Replacing the work-unit-level ERI estimate with the individual-level estimate in study ID #07 marginally increased the pooled estimate from 1.49 to 1.53 (95% CI 1.24–1.90) in the random-effects meta-analysis of the most adjusted study-specific estimates (data not shown).
When we used the least- as opposed to the most-adjusted study specific estimates in all studies the pooled estimate was 1.68 (95% CI 1.40–2.01) in the random-effects meta-analysis (e-figure 1 in e-Appendix 4, www.sjweh.fi/index.php?page=data-repository) and 1.63 (95% CI 1.47–1.80) in the fixed-effects meta-analysis (data not shown).
Pre-planned sensitivity analyses
Figure 3 shows the results of the pre-planned sensitivity analyses, where we stratified results by study quality (high and medium quality versus low quality), ascertainment of ERI (ERI-questionnaire versus proxy measures), and ascertainment of depressive disorders (self-administered rating scale versus other methods). The pooled estimates were similar in all analyses: 1.40 versus 1.56 when comparing studies of high/moderate quality to those of low quality, 1.64 versus 1.40 when comparing studies that used the original ERI questionnaire to studies that used proxy measures, and 1.64 versus 1.40 when comparing studies that assessed depression with self-administered rating scales to those using other methods.
Figure 3
Random-effects meta-analysis of the prospective association between effort-reward imbalance and onset of depressive disorders based on the most-adjusted study-specific estimates in relation to A) Study quality, B) Ascertainment of ERI, C) Ascertainment of depressive disorders
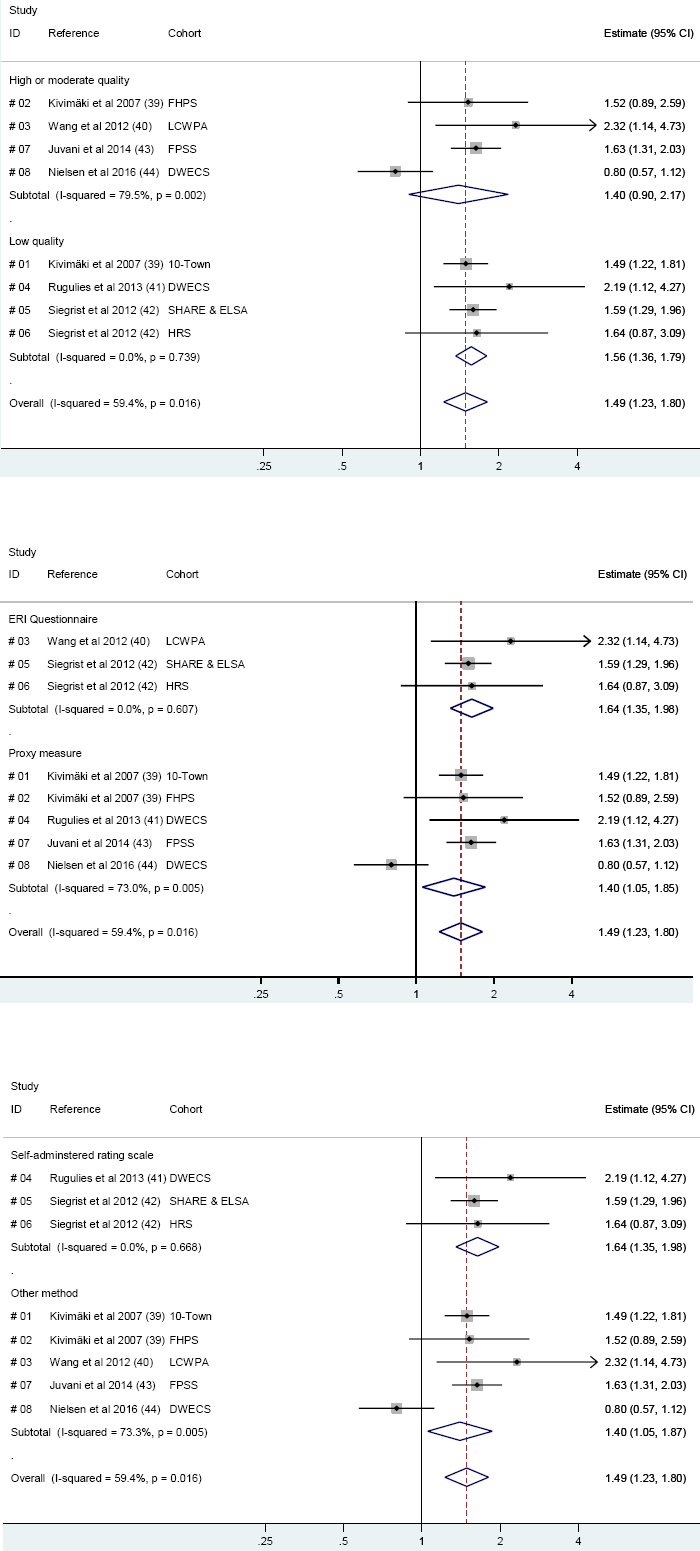
As the subgroups in the sensitivity analyses are rather small (3–5 studies), the impact of each single estimate on the pooled estimate is rather large. It is notable that in each of the three sensitivity analyses, the groups with the lowest pooled estimate are always the groups that included the one study (ID #08) that suggested that ERI was associated with a reduced risk of depressive disorders. We therefore post hoc repeated the three sensitivity analyses after excluding study ID #08 and found that the pooled estimates now were almost identical in all analyses, ranging from 1.56–1.66 (e-figure 2 in e-Appendix 5, www.sjweh.fi/index.php?page=data-repository).
Excluding studies with overlapping samples
When we excluded studies with overlapping samples the pooled estimate changed only marginally. Compared to the estimate of 1.49 when all eight studies were included, the estimates after excluding overlapping studies ranged from 1.45 to 1.59, depending on which study was excluded (e-table 2 in e-Appendix 6, www.sjweh.fi/index.php?page=data-repository).
Risk of bias across studies
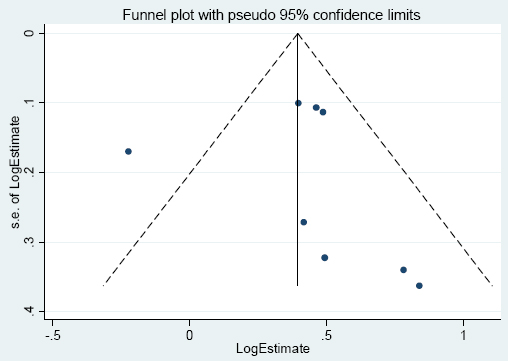
We drew a funnel plot for visual inspection of possible publication bias (figure 4). The funnel plot was skewed to the right, with the two studies with the highest estimates also being the studies with the highest standard error (lower right corner of the plot), which could be an indication of publication bias. Egger’s test did not indicate any publication bias (P=0.79), however, as ≥10 estimates are recommended for this test (37), a meaningful interpretation of this P-value is not possible.
Discussion
Summary of evidence
ERI was associated with a 1.5-fold increased risk of depressive disorders in this systematic review and meta-analysis of eight prospective cohort studies from Europe, Canada, and the US. The estimate remained robust when using alternative study-specific estimates, excluding partly overlapping studies and calculating pre-defined sensitivity analyses.
Seven of the eight studies suggested that ERI predicts risk of depressive disorders, whereas one study, Nielsen et al (44) that used register-data on purchase of antidepressants as the outcome measure, suggested the opposite: that ERI was associated with a reduced risk, albeit not statistically significant. We do not know the reason for this result, but it is conceivable that the divergence relates to the outcome measure. Purchase of antidepressants might not yield results that are comparable to symptoms-based measurements because a substantial proportion of individuals with depression are not treated with antidepressants (4, 48) and antidepressants are also prescribed for other disorders, such as anxiety, sleep disorders, or neuropathic pain (49). Further, purchase of antidepressants requests healthcare utilization, which is determined by a multitude of factors (50) that may cause bias, in particular when studying exposures that are related to socioeconomic position (51). The study by Nielsen et al (44) was from Denmark and two previous studies from this country showed that poor job climate predicted risk of hospitalization for depression (52) but not purchase of antidepressants (53), indicating that antidepressant purchase may be a problematic measure for onset of depression. However, other studies from Denmark reported that psychosocial work environment factors, such as high emotional demands (54), high quantitative demands (55), low workplace social support (55), and high job insecurity (56) predicted purchase of antidepressants, suggesting the usefulness of antidepressant purchase as an indicator for depressive disorders in psychosocial occupational health studies. Based on these conflicting results, we can neither confirm nor reject that the divergent estimate by Nielsen et al (44) was specific to the use of antidepressant purchase as the outcome measure.
Strengths and limitations
The strengths of this systematic review and meta-analysis are the detailed study protocol that was published before the literature search commenced, the comprehensive search strategy, the quality assessment of the individual studies, and the pre-planned sensitivity analyses.
A limitation is that the low number of identified studies did not allow us to statistically assess publication bias. Further, some criteria used in the quality assessment are debatable. Regarding the ascertainment of exposure, the instrument awarded points for either “secure record (eg surgical records)” or “structured interview” but did not allow to award points to the study by Juvani et al (43) that averaged individual responses to the work-unit level to reduce reporting bias. Regarding ascertainment of outcome, the instrument awarded points for either “independent blind assessment” or “record linkage”. Whereas independent blind assessment by a clinical diagnostic interview – used in one of the included studies (40) – is the gold standard for assessing depressive disorders in research (57), the use of record linkage, disability pensioning due to depression, and purchase of antidepressants medication – used in two of the included studies (43, 44) – may be problematic. The award of a disability pensioning due to depression depends not only on the disorder but also on legislations and the possibility of job accommodation. It also typically involves healthcare utilization that is determined not only by the disorder but by numerous other factors (50). Antidepressant purchase also involves healthcare utilization and may be a problematic indicator of depressive disorder as discussed above.
As in all reviews, the validity of our results depends on the quality of the included studies. It is a strength of the included studies that they adjusted for various potential confounders, including other psychosocial workplace factors: job strain in the Wang et al (40) and Juvani et al (43) studies and low organizational justice in the two studies published in the Kivimäki et al article (39). It is a weakness of the included studies that they assessed ERI by self-report. This is a concern because sub-clinical depressive symptoms or low mood at baseline may result into both over-reporting of adversity of working conditions and increased risk of future onset of depressive disorders causing spurious associations between ERI and risk of depressive disorders (10, 23). Two studies tried to address this concern by adjusting for sub-clinical depressive symptoms at baseline (41, 44), whereas one study used work-unit-level averaged ERI scores instead of individual-level ERI scores as the predictor variable (43).
Adjusting for sub-clinical depressive symptoms is not without problems, because it is unclear whether these symptoms are confounders or mediators or both. Baseline sub-clinical depressive symptoms would be confounders, if they caused both over-reporting of ERI at baseline and onset of depressive disorders at follow-up, but they would be mediators if ERI before baseline caused baseline sub-clinical depressive symptoms, which subsequently caused onset of depressive disorders at follow-up. A recent study on job strain and hospital treatment for depressive disorders showed reciprocal associations between job strain and sub-clinical depressive symptoms, suggesting that depressive symptoms are both confounders and mediators for the association of job strain and depressive disorders (58). If this reciprocal association is also true for ERI and sub-clinical depressive symptoms, then the association of ERI and risk of depressive disorders would be underestimated by adjusting and overestimated by not adjusting for sub-clinical depressive symptoms.
All studies assessed ERI only once, at baseline, which is a concern as repeated measures of ERI over a longer time period would have given a more precise assessment. Further, only one study (40) measured depressive disorders with a clinical diagnostic interview and only two studies (43, 44) allowed time-to-event analyses.
The extent to which these limitations have biased results is not known, but it seems plausible that some of these limitations (eg, self-reported assessment of ERI) may have caused an overestimation, whereas others (eg, failure to assess ERI more than once) may have caused an underestimation of the association of ERI and depressive disorders.
Concluding remarks
This review and meta-analysis provides the hitherto strongest evidence that ERI may play a role in the etiology of depressive disorders. In Theorell et al (25) most recent systematic review and meta-analysis based on a literature search until June 2013, only three articles on ERI and depressive disorders were included. Two of these were also included in our review [ie, Kivimäki et al (39), including two studies) and Rugulies et al (41)] whereas we excluded the third article, Godin et al (59), because the ERI measure combined information from both baseline and follow-up, introducing a cross-sectional element in an otherwise prospective study. We included two studies (from one article, 42) that Theorell et al did not include because they were concerned with the quality, a concern we did not share as the studies passed all of our strict inclusion criteria. In addition, we identified one study (40) that may have been overlooked by Theorell et al and two studies (43, 44) that were published after Theorell et al had conducted their literature search. Taken together, our review consisted of 84 963 individuals at risk, more than three times the number of individuals (N=27 136) included in Theorell et al’s analysis.
Although our review showed a statistically significant association of ERI and risk of depressive disorders that was consistent in seven of the eight included prospective studies, there are still several issues future research needs to address. First, more studies on ERI and depressive disorders are needed to allow sensitivity analyses with larger numbers of individual studies than in our review. Second, future studies should in particular aim to address possible reporting bias by either averaging individual-level ERI scores at the work-unit level, as demonstrated by Juvani et al in one of the reviewed articles (43), or by calculating proxy ERI measures based on non-self-reported register data [eg, ratio between number of working hours (effort) and level of salary (reward)]. The development of a job exposure matrix for ERI, ie, calculating job group specific ERI scores for use in epidemiologic analyses, may also be considered, though the feasibility remains to be determined. Whereas job exposure matrices have a long tradition in research on job strain and health eg, (60, 61), this method has, to our knowledge, never been used in research on ERI. Finally, it will be important for future studies to measure ERI repeatedly over a longer time period (ideally, over the whole work-life course) and ascertain depressive disorders more frequently with the gold standard instrument, a clinical diagnostic interview (57).