Stroke is a multi-factorial disease caused by an interplay between genetic and environmental risk factors. Well-documented risk factors include age, hypertension, diabetes, cigarette smoking, physical inactivity, carotid atherosclerosis and atrial fibrillation. During the last few decades, a growing body of evidence suggests that psychosocial factors also contribute. Education and socioeconomic status are consistently reported to be associated with stroke (1), and an association with psychosocial stress has been suggested (2). There is also an accumulating literature suggesting an association between cardiovascular disease and the psychosocial work environment (3–5). The main body of evidence comes from studies on coronary heart disease, while stroke has been less studied.
Among psychosocial work environmental factors, psychosocial stress, including the job–demand–control (JDC) model (6), has received the most attention. This model postulates that high psychological demands in terms of volume and intensity of workload combined with low individual control over pace and content of work tasks result in high strain or stress (job strain). A recent meta-analysis of 14 European cohort studies concluded an increased risk of ischemic stroke for those exposed to job strain (7). There are also recent systematic reviews showing increased risk of stroke in relation to long working hours (8) and shift work (9). Interestingly, in Japan and Taiwan, “karoshi”, ie, sudden death as a consequence of overwork, is predominately attributed to cerebrovascular death and is recognized as a clinical entity qualifying for worker compensation (10). Emotional components of the psychosocial work environment, such as lack of reciprocity between work effort and rewards (11) or workplace conflicts (12–14), have gained increased attention as important stressors. However, investigations of these factors in relation to stroke are scarce.
Here, our aim is to investigate the relation between a first-ever stroke at working age and the psychosocial work environment as assessed by the JCD model, the effort–reward imbalance (ERI) model, and self-reported conflicts at work.
Methods
This study is a multicenter matched case–control study. Cases were recruited at stroke units at four different hospitals in Sweden, geographically located in the very south of Sweden (Malmö, 62 cases), the middle (Göteborg, 64 cases, Linköping, 39 cases) and the north (Umeå, 33 cases). Stroke-free controls were randomly recruited from the population residing in the hospitals’ catchment area using the Swedish population register. The regional ethics board in Linköping, Sweden, approved the study.
Cases
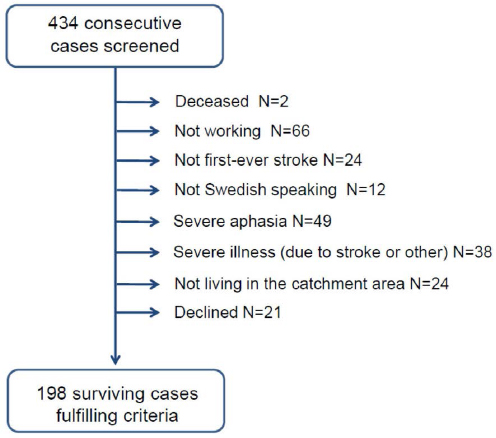
Consecutive cases, aged 30–65 years, presenting with acute stroke at the stroke units from September 2007 to December 2009, were screened by a nurse or an occupational therapist to check for the inclusion and exclusion criteria and to ask for informed consent to participate in a study investigating associations between living conditions and risk of stroke. Inclusion criteria were: diagnosis of first-ever intracerebral hemorrhage (ICD-10: I61) or cerebral infarction (ICD-10:I63). Exclusion criteria were: previous stroke, not working at the time of stroke, unable to answer a questionnaire (in Swedish) in writing or verbally, or severe illness. Screening was performed within four weeks of the acute event. All cases underwent neuroimaging, and for each case, subtype of stroke was recorded as hemorrhagic or ischemic. Ischemic strokes were further classified according to the Trial of Org 10172 in Acute Stroke Treatment (TOAST) criteria (15). Severity of neurological deficits at acute stroke was recorded using the National Institute of Health Stroke Scale (NIHSS). A total of 434 cases were screened, and 21 otherwise eligible patients declined participation. Of these, 12 were males and the mean age was 55.5 years. In all, 198 working cases fulfilled the inclusion criteria and did not meet any exclusion criteria, see figure 1.
Controls
For each case, up to ten controls were randomly drawn from the Swedish population register, six months from admittance of the case. Controls were matched to the cases with regard to age (±1 year), sex and geographical area. Potential controls received a letter with information in which the study was presented as an investigation of associations between living conditions and risk of stroke. The first two respondents who met the inclusion criteria and not the exclusion criteria were used as controls. Exclusion criteria were the same as for cases, and all controls with a self-reported doctors’ diagnosis of stroke (asked for in the questionnaire) were excluded. In all, 2829 questionnaires were sent to potential controls, and the response rate was 49% after one reminder. Respondents and non-respondents did not differ with respect to gender. However, among men the proportion of non-responders was inversely associated to age.
Data collection
All subjects were asked to complete a written questionnaire covering questions about their civil status, education, length of employment, lifestyle habits, anthropometric measures, doctors’ diagnosis of vascular risk factors, family history of stroke, occurrence of sick leave spells, number of sick leave days during the last 12 months, main medical reason for sick leave, and work situation. The time span considered for the exposure measures in the questionnaire was 12 months prior to stroke for the cases. For controls, it was 12 months prior to the time they answered the questionnaire, as exemplified by the question “Have you been involved in any conflicts at your workplace during the last 12 months?”.
Psychosocial work environment
The psychosocial work environment was assessed by means of two psychometric instruments: the Swedish Demand–Control–Support Questionnaire (DCSQ) (16, 17) and ERI (18, 19). The latter model adds the intrinsic (personal coping patterns) work efforts to the extrinsic (work pressure) work efforts and postulates that high effort in combination with low personal reward (financial, status, job security or esteem) is stressful (18, 20, 21). Thus, this model somewhat overlaps the JCD model but differs in that it also incorporates intrinsic aspects such as the negative emotions elicited by the experience of a lack of reciprocity in work effort and gains. Two subscales were derived from the DCSQ: psychological demands (time pressure, and conflicting demands, 5 items), and decision latitude (skill level and decision authority, 6 items). Job strain was calculated as the ratio of the mean of psychological demands in the numerator and the mean of decision latitude in the denominator. Cronbach’s α for psychological demands and decision latitude were 0.74 and 0.68, respectively. Two subscales were derived from the ERI model: effort (time pressure, interruptions, responsibility, working overtime, increasing demands, 5 items), and reward (financial and status-related reward, esteem reward and job security reward, 11 items). The ERI ratio was computed as the ratio of the mean of the effort score in the numerator and the mean of the reward score in the denominator (18). Cronbach’s α for effort and rewards was 0.75 and 0.77, respectively.
Conflict at work
Each subject was asked to report occurrence in the last year of threat, violence, harassment or bullying by supervisors, harassment or bullying by colleagues, involvement in conflicts, or victimization at the workplace as “no, never”, “no, seldom”, “yes, sometimes” and “yes, often”, and of serious conflict in the workplace (life-event coded as “yes”) (total 7 items)(22). Conflict at work was coded as present if one of these questions were answered as yes (“yes, sometimes” or “yes, often”).
Risk factors
Hypertension was defined as responding yes to the question “Have you previously been informed by your physician that you have high blood pressure?” Similar questions were posed for diabetes, high blood lipids, atrial fibrillation, and angina pectoris. Family history of stroke was defined as responding yes to the question “Have either of your parents or your siblings had a stroke?”.
Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. Smoking habits were coded as current smoker versus never or former. Physical activity was assessed by two questions: one on physical activity in everyday life and one on exercise during the last 12 months. These questions were combined, and physical activity was coded as low (none or little everyday activity) versus moderate to high physical activity (almost daily and/or frequent intense physical activity). Civil status was classified as married/cohabiting, single, or other. Education was classified as low (nine-year compulsory school) or high (upper secondary school or university).
Statistical analysis
Descriptive statistics are presented as frequencies or mean values and standard deviations (SD). Differences between groups were examined with the chi-squared test for proportions and with Student’s t test for continuous variables.
The associations between psychosocial work environment (ie, job strain, ERI ratio, conflict at work) and stroke were investigated by conditional logistic regression analyses. In these analyses, each stroke was individually age- and sex-matched with two controls within each center. The psychosocial scales, (ie, ERI and job strain) were standardized before entering the regression analyses; thus the odds ratios (OR) of the psychosocial scales, can be interpreted as the OR when moving one standard deviation on the dimension of the scales. The conditional logistic regression analysis was performed in two steps. In the first step, the OR were adjusted only for the matching factors. In the second step, the OR were additionally adjusted for educational attainment, marital status, smoking, physical activity, high blood pressure, diabetes, high blood lipids, body mass index, and family history of stroke. Two different models were used to explore differences between the job strain and the ERI models. In the first model, job strain and conflicts at work were determinants; in the second model, ERI and conflicts at work were determinants. In a final step, we investigated the combined effect of job strain and ERI in univariate and multivariable regression models. In these models, the psychosocial scales were dichotomized, and those exposed to neither job strain nor ERI was used as the reference category (23).
The proportion of cases or controls with missing values was <10% for all items, except for angina pectoris (17%) and smoking (11%) in cases. Replacement of missing values on measurement scales was performed according to the SF-36 rule(24). Thus, a total score was calculated for a subject if he/she had answered at least half of the questions of the scale, by giving the missing items the average score of the other items in the scale. Cases and controls with missing values for predictor variables were excluded from multivariable analyses. Data were analyzed using the statistical software SAS 9.1 (SAS Institute, Cary, NC, USA). Results were considered statistically significant at P≤0.05 using two-tailed tests.
Results
Among the cases, a total of 20 strokes (10%) were hemorrhagic and 178 (90%) were ischemic. The median NIHSS score was 2 (range 0–22). According to TOAST classification of ischemic stroke, 28 (16%) were due to large artery arteriosclerosis, 19 (11%) to cardiac embolism, and 69 (39%) to small artery occlusion; other causes (mainly dissection of vertebral or carotid arteries) were found in 14 (8%), whereas 48 (27%) were undetermined.
The characteristics of the study subjects are given in table 1. Cases and controls differed significantly with respect to educational level, cohabitation, smoking habits, physical activity, hypertension, BMI, family history of stroke and family history of heart disease. Cases also reported a significantly higher frequency of sick leave spells lasting >14 days, compared with controls. However, there was no difference between the groups regarding medical reasons for previous sick leave. Most common were common mental disorders (79% among cases, 76% among controls) and cardiovascular disorders (17% and 19% respectively).
Table 1
Characteristics of the study subjects. [BMI=body mass index; SD=standard deviation.]
| Cases (N=198) | Controls (N=396) | P-value a | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||||
| N | Mean | SD | N | % | N | Mean | SD | N | % | ||
| Age (years) | 198 | 54.4 | 7.9 | 396 | 54.6 | 7.8 | |||||
| Male gender | 198 | 135 | 68 | 396 | 270 | 68 | |||||
| Low education | 192 | 104 | 54 | 389 | 168 | 43 | 0.01 | ||||
| Length of employment (years) | 174 | 11.7 | 10.3 | 371 | 11.6 | 10.0 | 0.93 | ||||
| Marital status | 193 | 394 | 0.002 | ||||||||
| Married/cohabiting | 132 | 68 | 320 | 81 | |||||||
| Single | 53 | 28 | 64 | 16 | |||||||
| Other | 8 | 4 | 10 | 2 | |||||||
| Smoking | 176 | 50 | 28 | 377 | 53 | 14 | <0.001 | ||||
| Physical activity (moderate or high) | 191 | 54 | 28 | 393 | 155 | 39 | 0.008 | ||||
| Hypertension | 184 | 70 | 38 | 386 | 104 | 27 | 0.007 | ||||
| Diabetes | 192 | 12 | 6 | 393 | 21 | 5 | 0.66 | ||||
| High blood lipids | 192 | 47 | 24 | 394 | 73 | 18 | 0.09 | ||||
| BMI (kg/m2) | 182 | 27.2 | 5.4 | 389 | 25.8 | 3.7 | <0.001 | ||||
| Family history of stroke | 190 | 65 | 34 | 382 | 67 | 18 | <0.001 | ||||
| Atrial fibrillation | 189 | 7 | 4 | 384 | 9 | 2 | 0.37 | ||||
| Angina pectoris | 164 | 10 | 6 | 382 | 12 | 3 | 0.24 | ||||
| ≥1 spell of sick leave b | 183 | 92 | 50 | 393 | 167 | 42 | 0.26 | ||||
| >3 spells of sick leave b | 183 | 18 | 10 | 393 | 26 | 7 | 0.18 | ||||
| ≥1 spell of sick leave >14 days b | 180 | 30 | 17 | 389 | 33 | 8 | 0.004 | ||||
Occupational distribution differed between cases and controls (P=0.003): 38% among cases and 54% among controls had occupations requiring university education or involving management positions; 14% among cases and 9% among controls had occupations requiring no formal education.
The work exposure characteristics of the two groups are shown in table 2. There were significant differences between the groups in their ratings of occurrence of conflict at work, with a higher prevalence among cases, mainly due to higher ratings of involvement in conflicts and serious conflicts at work. Job strain was higher among cases, in particular due to lower decision latitude. The ERI score was higher among cases, mainly due to higher scores for effort compared with the controls.
Table 2
Work exposure characteristics of the study subjects. [SD=standard deviation.]
| Study variables | Cases (N=198) | Controls (N=396) | P-value | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||||
| N | Mean | SD | N | % | N | Mean | SD | N | % | ||
| Conflict at work a | 198 | 71 | 35 | 395 | 91 | 23 | 0.001 | ||||
| Threats b | 187 | 20 | 11 | 388 | 37 | 10 | 0.66 | ||||
| Violence b | 187 | 13 | 7 | 388 | 13 | 3 | 0.05 | ||||
| Bullying by supervisor b | 178 | 10 | 6 | 384 | 13 | 3 | 0.21 | ||||
| Bullying by workmates b | 182 | 10 | 5 | 387 | 12 | 3 | 0.17 | ||||
| Involved in conflicts at the workplace b | 182 | 41 | 23 | 385 | 48 | 12 | 0.002 | ||||
| Victimized at the workplace b | 179 | 14 | 8 | 385 | 16 | 4 | 0.07 | ||||
| Serious conflict at the workplace b | 195 | 39 | 20 | 388 | 40 | 10 | 0.001 | ||||
| Job strain | 191 | 0.90 | 0.29 | 389 | 0.83 | 0.21 | <0.001 | ||||
| Psychological demands | 191 | 13.40 | 2.90 | 390 | 12.96 | 2.63 | 0.07 | ||||
| Decision latitude | 191 | 18.48 | 3.04 | 390 | 19.20 | 2.54 | 0.003 | ||||
| Effort–reward imbalance ratio | 185 | 0.90 | 0.33 | 386 | 0.83 | 0.28 | 0.01 | ||||
| Effort | 192 | 13.05 | 3.45 | 391 | 12.24 | 3.34 | 0.007 | ||||
| Reward | 185 | 33.46 | 5.91 | 386 | 33.57 | 5.43 | 0.82 | ||||
Univariate regression analyses showed that job strain [OR 1.38, 95% confidence interval (95% CI) 1.19–1.59], ERI (OR 1.24, 95% CI 1.06–1.44) and conflict at work (OR 1.87, 95% CI 1.38–2.54) were significant determinants of stroke risk. Gender stratified analysis showed no differences between women (OR 1.46, 95% CI 1.10–1.94, OR 1.17, 95% CI 0.90–1.53, and OR 1.65, 95%CI 1.02–2.66 for job strain, ERI, and conflict at work, respectively) and men(OR 1.33, 95% CI 1.13–1.58, OR 1.29, 95% CI 1.07–1.55, and OR 2.02, 95%CI 1.37–2.99 for job strain, ERI, and conflict at work, respectively).
Results from multivariable regression models are given in table 3. After adjustment for conflicts at work, the OR for job strain and ERI attenuated and only job strain remained significantly associated with stroke risk (OR 1.30, 95% CI 1.12–1.51, and 1.13, 95% CI 0.96–1.33 for job strain and ERI, respectively). Conflict at work remained an independent determinant of stroke after adjustments for job strain (OR 1.64, 95% CI 1.19–2.25) and ERI (OR 1.80, 95% CI 1.30–2.50). Multivariable regression models adjusting for education, marital status, and vascular risk factors showed that job strain, ERI, and conflict at work all remained independent predictors of stroke (Table 3). In a final step, we investigated the combined effect of job strain and ERI (Table 4). In those exposed to both job strain and ERI, the multivariable OR for stroke was 3.01, 95% CI 1.62–5.61. Further adjustment for conflict at work attenuated the association; however, the combined effect, as well as conflict at work, remained significantly associated to increased risk of stroke. There was no significant interaction between job strain and ERI (OR for the interaction term 1.06, 95% CI 0.94–1.19).
Table 3
Multivariate adjusted odds ratios (OR) of stroke and 95% confidence intervals (95% CI) for job strain, effort–reward imbalance (ERI) and conflict at work.
| Variable | Model I (N=580) a | Model Ib (N=455) b | Model II (N=571) c | Model IIb (N=447) d | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||||||
| OR | 95% CI | P-value | OR | 95% CI | P-value | OR | 95% CI | P-value | OR | 95% CI | P-value | |
| Job strain | 1.30 | 1.12–1.51 | <0.001 | 1.30 | 1.05–1.62 | 0.02 | ||||||
| Conflict at work | 1.64 | 1.19–2.25 | 0.003 | 1.75 | 1.07–2.88 | 0.03 | ||||||
| Variable | ||||||||||||
| ERI | 1.13 | 0.96–1.33 | 0.15 | 1.28 | 1.01–1.62 | 0.04 | ||||||
| Conflict at work | 1.80 | 1.30–2.50 | <0.001 | 1.86 | 1.11–3.11 | 0.02 | ||||||
Table 4
Multivariate adjusted odds ratios (OR) of stroke and 95% confidence intervals (95% CI) for combined effect of job strain and effort–reward imbalance (ERI) and conflict at work.
| Model I (N=444) a | Model II (N=444) b | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| OR | 95% CI | P-value | OR | 95% CI | P-value | |
| Neither ERI ratio >1 nor job strain present | 1.00 | 1.00 | ||||
| ERI ratio >1 but job strain absent | 1.53 | 0.79–2.94 | 0.20 | 1.25 | 0.62–2.49 | 0.53 |
| Job strain present but ERI ratio ≤1 | 2.41 | 1.32–4.38 | 0.004 | 2.02 | 1.09–3.72 | 0.03 |
| ERI ratio >1 AND job strain present | 3.01 | 1.62–5.61 | <0.001 | 2.31 | 1.17–4.54 | 0.02 |
| Conflict at work | 1.78 | 1.05–3.02 | 0.03 | |||
Discussion
In this case–control study of first-ever stroke at working age, we observed an association between adverse psychosocial working conditions during the past 12 months and increased risk of stroke. Interestingly, all three measures, job strain, ERI, and conflict at work, were more frequently reported among stroke cases compared with controls. The association between stroke and measures of psychosocial work environment remained after adjustment for education, marital status, and vascular risk factors.
Workplace bullying and harassment is increasingly common and associated with a wide range of negative health effects and emotional reactions (12, 13). Also in our study, conflicts at work were a common exposure, as more than one fifth of the participants in the control group reported occurrence of some kind of conflict at work. Despite this, there are no previous reports about associations to stroke. Thus, our results showing an association between conflict at work and stroke are novel, and add stroke to the list of health problems associated to exposure to workplace conflicts, underscoring the potential detrimental health effects of an adverse emotional psychosocial work environment.
The measures ERI and conflict at work somewhat overlap as they both measure aspects of social interaction at the workplace and the emotional work environment. Interestingly, ERI also showed association to stroke, further indicating an important role for the emotional environment at work. To the best of our knowledge, there are no previous reports on the relation between ERI and stroke. Conflicts at work and job strain showed associations with stroke that were independent of each other, indicating that these measures capture different aspects of the psychosocial work environment that impact the risk of stroke. These results are important, as they indicate that interventions may need to target not only job strain, but also the emotional work environment.
Associations between stroke and job strain or its components have previously been reported from large-scale prospective studies (7, 25–27), while others(28–30) did not find any association between job strain and stroke. There is also conflicting data regarding whether the association between job strain is confined to ischemic stroke or whether it also influences the risk of hemorrhagic stroke(5, 26). In this context, the results from our study are not novel, but lend further support to an association between job strain and an increased risk of stroke at working age. The size of our sample did not allow for separate analysis of different stroke subtypes. However, interestingly, and similar to what has previously been reported in relation to myocardial infarction (23), the combined effect of job strain and ERI was substantial as it was associated with a threefold increase in stroke risk. Moreover, this association remained, however attenuated, after adjustment for conflict at work.
The association between psychosocial work environment and stroke is probably caused by a complex interplay between a numbers of factors. Several different mechanisms have been suggested as possible mediators including activation of the neuroendocrine system, vascular inflammation, oxidative stress, immune dysfunction, development of the metabolic syndrome, hypertension, unhealthy behaviors such as smoking, physical inactivity and poor diet. There is also a complex interplay with education and socioeconomic status(31, 32). As expected, cases reported a higher burden of vascular risk factors compared with controls. Cases also had lower education and were less often in occupations requiring university education or involving management positions. Although we used multivariable regression models to adjust for these factors, residual confounding may remain. However, it should be noted that some of these factors can be considered as mediators for the association.
Cases reported higher frequency of sick leave spells lasting >14 days, compared with controls. Similarly, Medin et al (33) found that stroke cases had accumulated more sick leave during the three years prior to their stroke compared to the general population of the same age. At first glance, this may be perceived as an expected finding based on the higher burden of vascular risk factors. However, the most prevalent reason for sick leave was common mental disorders, and there was no increase in the proportion of sick leave explained by cardiovascular disorders among cases. The explanation for the higher frequency of long-term sick leave prior to stroke is not clear. An adverse psychosocial work environment may contribute not only to cardiovascular disease but also to reduced mental health (34). Conversely, spells of longer sick leave may contribute to an adverse psychosocial work environment, involving worse relations with supervisors and workmates (35), as sick leave may interfere with achievements and social relations at work. Moreover, a recent report indicates a complex interplay between depression, psychological stress, socioeconomic status, and risk of cardiovascular diseases including stroke (36).
Our study is a hospital-based case–control study and potential limitations include those that are inherent to the study design (ie, selection bias and recall bias). According to guidelines in Sweden, all patients with a suspected stroke, including those with milder symptoms, should be admitted to a stroke unit. Controls were randomly recruited from the population residing in the hospitals’ catchment area. However, we were not able to include the most severe cases, ie, fatal cases and those with severe stroke symptoms that interfered with the ability to answer the questionnaire. Moreover, non-Swedish-speaking persons, a group which may have a higher exposure to an adverse psychosocial work environment, were not included. Thus, selection bias of cases in this study may, if anything, have led to an underestimation of the true association. On the other hand, the relatively low response rate among controls is a limitation that potentially may inflate the difference between cases and controls with respect to socioeconomic factors including the psychosocial work environment. However, our findings on education and marital status are comparable with previous studies in the field (1, 26), suggesting that the effects of a possible selection bias of controls were limited.
In order to reduce recall bias, assessments of exposure were made shortly after disease onset, and neither the cases nor the controls were given detailed information about the hypothesis under investigation. When possible, we used validated psychometric instruments (ie, ERI and JDC). Previous studies of coronary disease indicate that these instruments are relatively robust with respect to recall bias. A recent systematic review of high quality studies found similar associations to job strain in case–control and prospective studies (4). Moreover, in a study of myocardial infarction at working age, self-rated and job exposure matrix based assessments of job demands and decision latitude showed similar relations in cases and controls, further supporting a limited influence of recall bias on these measures (37). The classification of vascular risk factors were based on self-reported doctors’ diagnoses and not confirmed in medical journals. Although using the same method in cases and controls, these factors were measured with less precision. Moreover, we did not measure depression and were therefore not able to investigate the contribution of this factor. A particular strength of our study is the relatively large sample of well-characterized cases who had their stroke at working age, with exposure data covering the year immediately preceding the stroke. However, the sample size did not allow for separate analyses of different stroke subtypes.