Low-back pain (LBP) is a substantial health challenge in the general Danish population. In 2013, 47% of workers in Denmark reported pain or discomfort in the back during the preceding 14 days (1). Severe LBP increases the risk for long-term sickness absence and early retirement (2) and has profound consequences for individuals, organizations, and society (3–5).
Biomechanical exposures at work, such as heavy lifting or awkward trunk postures, are believed to be key determinants of LBP (6). However, many traditional work tasks posing heavy physical work demands on the lower back while standing or walking have been replaced by sedentary tasks. Thus, sitting at work has been increasing during the last two decades (7, 8). A Danish study from 2014 (9) showed that 40% of all employees in Denmark were sitting >75% of their working hours. Even in blue-collar occupations, workers now appear to be exposed to considerable sitting during the working day (10–12). This suggests that effects of sitting may also be relevant to address in blue-collar occupations.
In theory, prolonged sitting at work could cause LBP due to limited posture variation (13, 14). This may, hypothetically, decrease flexibility and muscle strength in the lower back (15), which may in turn lead to disc degeneration, rupture, or herniation (16, 17). Yet, evidence supporting these hypothetical mechanisms of mechanical damage to tissues is not convincing. Furthermore, systematic reviews of the available evidence have not been able to verify a consistent association between sitting and LBP (18–20).
The inconsistent results may be due to the different methods used in previous studies to assess sitting, ie, self-reports, observations, or objective measurements, resulting in a dispersion in the extent and quality of information (18, 20). Self-reported sitting is less valid than sitting measured objectively, for instance by accelerometry (21, 22), due to recall bias (23) or differential misclassification (24, 25). Thus, objectively measured sitting is preferable in the context of trustworthiness and also has the advantage of allowing detailed investigations of temporal sitting patterns (10, 12). The development of LBP has even been suggested to be associated with the temporal patterns of sitting (18, 26). A few recent studies have used accelerometer-based sitting data in studies of associations with LBP (11, 27). However, these studies pointed in opposite directions: Gupta and colleagues (11) found that an increased amount of sitting was positively associated with LBP intensity while Lunde and colleagues (27) concluded that sitting was negatively associated with intensity of LBP. Only two studies have addressed associations between LBP and the temporal patterns of sitting, expressed in terms of the occurrence of prolonged uninterrupted periods of sitting (26) or as the frequency of transitions between sitting and other body postures, such as standing (18). Thus, further studies on objectively measured sitting and LBP are justified, focusing on both total amount and temporal patterns of sitting.
Therefore, the objectives of this paper were to (i) investigate the extent to which LBP is associated with the total amount and the temporal patterns of objectively measured sitting, both at work and for whole days, and (ii) investigate whether these associations are influenced by selected moderators.
Our main hypothesis was that more time spent sitting is associated with an increased level of LBP intensity, in particular if sitting occurs for long uninterrupted periods of time.
Methods
Study design and population
This study was based on data from the Danish PHysical ACTivity cohort with Objective measurements (DPhacto). Participants were recruited from 15 companies in the cleaning, transport, and manufacturing occupational sectors between December 2011 and March 2013 in collaboration with a large Danish labor union (21). The study was conducted according to the Helsinki declaration and approved by the Danish Data Protection Agency and local ethics committee (H-2-2012-011). All workers provided their written informed consent prior to participation. Baseline measures included questionnaires, objective measurements of anthropometrics, blood pressure and physical capacity, and objective measurements of physical activity and body postures based on accelerometry. Further details can be found in previous studies based on the DPhacto cohort (28, 29). The present study is a cross sectional analysis of baseline data.
Inclusion criteria for companies were that they allowed measurements to take place during paid working hours. Pregnant workers were excluded from participation in the study. Workers with allergy to bandages or adhesives were excluded from the objective monitor-based measurements (21).
Assessment of exposure
Objective data on sitting were collected using two accelerometers (ActiGraph GT3X+) (30), mounted on the skin at the front of the right thigh (medial between the iliac crest and the upper border of the patella) and at the trunk (at processus spinosus at the level of T1-T2) by adhesives (11, 12, 31). Participants wore the accelerometers for 4–6 days, 24 hours a day. During the measurement days, participants were asked to keep a diary stating: working hours, time off work, time in bed (when they went to bed and got up in the morning), and periods when they did not wear the accelerometers.
Data were sampled by the accelerometers at a frequency of 30 Hz with a dynamic range of ± 6 G and a 12-bit precision. The accelerometers were initialized and data downloaded using the Actilife software version 5.5 (ActiGraph LLC, Pensacola, FL, USA). Accelerometer signals were low-pass filtered at 5 Hz using a fourth-order Butterworth filter and then split up in 2-s windows with 50% overlap. Then, the accelerometer data were analyzed using the customized software Acti4 (31). The Acti4 software determines a variety of body postures and activities and has shown a sensitivity of 99.9% and specificity of 100.0% for sitting in standardized field settings (31). Non-wear periods were identified when one or more of the following criteria applied: (i) the participant registered non-wear in the diary, (ii) the Acti4 detected periods >90 minutes with zero acceleration, or (iii) missing data and/or artefacts were detected by visual inspection.
These analyses only included days where the participant had been working. Measurements during working hours were included if they were ≥4 hours/day (continuous periods) or a duration of ≥75% of average wear time during work across days per participant. Similar inclusion criteria were used for the intervals during time-off work.
Sitting periods were determined using data from the trunk and thigh accelerometers (28) as periods when thigh inclination was >45° and trunk inclination was <45° relative to the recorded vertical reference position (11). Sitting during the whole day was calculated as the accumulated time in sitting while being awake, and expressed in percent of the total duration of the measurement day. For each participant, results were then averaged across days, and this average was used in the statistical models described below. Similarly, sitting during work was calculated for each participant by adding up periods of sitting during working hours for each measurement day, expressing the result as percent of working time that day, and averaging across days.
Temporal patterns of sitting were quantified using exposure variation analysis (EVA) (32). Uninterrupted periods of sitting were identified throughout the entire time line of the processed accelerometer signal. An interruption in sitting was defined to occur when non-sitting occurred for ≥5 consecutive seconds. Sitting periods were then categorized according to duration (10): ie, brief bursts (≤5 minutes), moderate periods (>5–≤20 minutes) and prolonged periods (>20 minutes). For each participant, the mean daily duration (hours/day) spent in each of the EVA categories for both working hours and the whole day was calculated by dividing the total accumulated duration of sitting in the specific category across all measurement days by the number of days. Additionally, the mean time spent in each EVA category was expressed as percent of the daily average of total wear-time, both during working hours and for the whole day.
The distributions of the categorized EVA data were skewed and therefore these variables were square root transformed before proceeding with further analyses. The square root transformation resulted in distributions closer to normal.
Assessment of outcome
Intensity of LBP was determined using the question: “In the last 3 months, state your worst pain in lower back” from the standardized Nordic Questionnaire for the analysis of musculoskeletal symptoms (33), with response options on an 11-point scale from 0 (“no pain”) to 10 (“worst pain imaginable”).
Assessment of potential confounders and moderators
A number of factors have been shown in previous research to be associated both with LBP and the amount of sitting; they were therefore considered as potential confounders: age (34); sex (34); smoking (35, 36); BMI (37, 38); level of occupational lifting (34); occupational sector (39); previously diagnosed with a herniated disc (40); leisure-time physical activity (41, 42); and intensity of physical activity during working hours (43, 44), measured as rate of perceived exertion and aerobic workload in this study.
Since the factors listed above may also act to moderate the association between sitting and LBP, the following factors were entered in the analysis through an interaction term (sitting × factor): age, sex, BMI, occupational sector, level of physical activity during leisure time, and intensity of physical activity during working hours. Factors were centered prior to their inclusion in interaction terms to reduce effects of collinearity between data in interaction and main effects.
Age was based on the date of birth for the participant. Sex was determined from the question: “Are you male or female?”. Smoking was assessed by the question “Do you smoke?” using four response categories, which were merged into a dichotomized variable: yes (“yes, daily”, “yes, sometimes”) or no (“used to smoke”, “I have never smoked”). Objective measurements of body weight (in kg; Tanita BC418) and height (in m; Seca model 123 1721009) were obtained, and used to calculate the BMI (kg/m2). Occupational lifting and carrying was assessed by a single item from the Danish Work Environment Cohort Survey (DWECS): “How much of your working time do you carry or lift?” with a 6-point response scale from 1 (“almost all the time”) to 6 (“never”). Occupational sector was determined by the workplace of the participant and whether the participant stated to be working in administration (white-collar work) or production (blue-collar work). The following occupational sectors were represented: cleaning, manufacturing, transportation and administration (irrespective of occupational sector). A previous diagnosis with a herniated disc was assessed by the question: “Do you have herniated discs?” with the dichotomized response “yes” or “no”. Moderate-to-vigorous leisure-time physical activity was assessed by the Acti4 software, adding up leisure time spent in one of the following activities: running, climbing stairs, and cycling. The accumulated time was expressed as percentage of the total measured leisure time and participants were classified into high or low level physical activity by a median split. Intensity of physical activity during working hours was measured by the rate of perceived exertion, assessed by the question: “How physically demanding do you normally consider your present work?” with a 10-point response scale from 1 (“sedentary, not demanding”) to 10 (“very demanding”); and aerobic workload was assessed in terms of relative heart rate (45), with objectively measured resting heart rate and estimated maximal heart rate (46).
Social support and influence at work were determined by items from the Copenhagen Psychosocial Questionnaire (47). Influence at work was determined by the question: “Do you have a large degree of influence concerning your work?”; “Can you influence the amount of work assigned to you?”. Social support was determined by: “Is there good cooperation between the management and the employees?”; “Is there good cooperation between the colleagues at work?” The response categories were on a 5-point scale, ranging from 1 (“always”) to 5 (“never”). The scale were reversed and recoded to 0–4; answers given for the two items were added up to a 0–8 scale for each dimension as described in the questionnaire manual (available at: www.arbejdsmiljoforskning.dk). Thus, in the analyzed data, higher numbers indicate more influence and better social support.
Statistical analysis
Associations between sitting variables and LBP were determined using linear regression. The different variables of sitting [total sitting, EVA derivatives describing temporal patterns (brief bursts, moderate and prolonged sitting periods)] were analyzed during work and for the whole day in separate regressions. Exposure variables were square root transformed in order to better approach a normal distribution. Intensity of LBP was entered as a continuous variable. The assumption of a linear association between exposure and outcome was justified according to visual inspection of data plots.
Interaction terms between centered variables of exposure and potential moderator factors were included in the regression one by one. If the interaction term showed to influence the association between exposure and outcome significantly (P<0.10), the interaction term was included in the final model, and a complementary stratified analysis was conducted. Those potential moderator factors that did not significantly influence the association between sitting and LBP were instead considered as potential confounders.
Multicollinearity between the potential confounders was assessed by variance inflation; if substantial multicollinearity was present, the potential confounder was not included in the final model. Potential confounders were included in the final model one by one if they significantly (P<0.10) affected the association between exposure and outcome. Three sensitivity analyses were performed based on the final model. In the first, age and sex were added as forced confounders to the final model. In the second, social support and influence at work were added. This second sensitivity analysis could only be performed for cleaning and manufacturing since none of the participants from the transport sector received the questions regarding influence and support at work due to a technical error. In the third sensitivity analysis, the final model was run on a population excluding all participants reporting 0 on the LBP scale, ie, no LBP.
Additionally, analyses both for work and the whole day were conducted in which the EVA derivatives were expressed in percentages of total sitting, as opposed to percentages of the total measurement time, as above. These analyses were performed to determine the extent to which the temporal pattern of sitting was associated with LBP irrespective of total sitting.
Results
Flow of participants
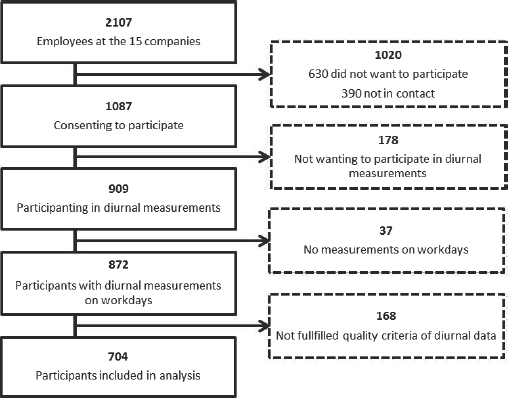
figure 1 shows the flow of the participants from DPhacto included in this study. Of the 909 participants that took part in the diurnal accelerometer measurements of sitting, 704 participants were included in the analysis, based on the quality criteria for accelerometer data described above.
Baseline characteristics of the study population
The DPhacto contains data from three occupational sectors, ie, cleaning, manufacturing, and transport, as well as the administrative staff within these occupational sectors. The study population included 704 of the participants in the DPhacto (figure 1), 312 females and 392 males (table 1), aged 18–68 years. The participants had a mean seniority in their current job of 13.0 [standard deviation (SD) 10.1] years (table 1).
Table 1
Baseline characteristics of the study population (N=704).
The mean intensity of LBP during the last 3 months was 3.4 (SD 3.1) on a 0–10 point scale, where 10 indicated the worst imaginable pain (table 1). More than half of the population (62.8 %) reported a level of LBP <5 within the last 3 months and 30.2% reported to be pain-free. Seventy-three percent of the population stated having <31 days with LBP during the last year and 24.3% stated having no days with LBP during that period.
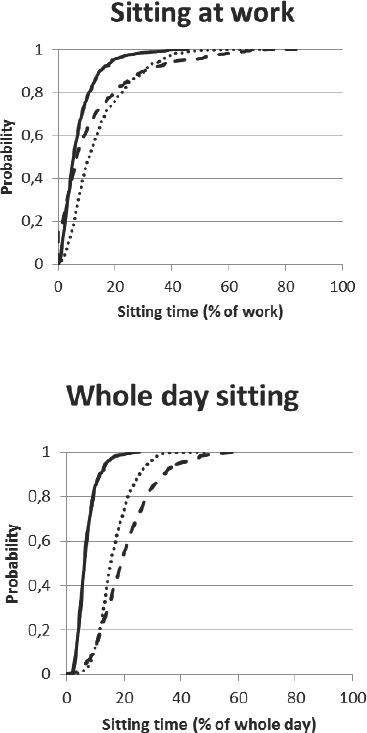
On average, accelerometer data were collected for 2.6 days for each participant (SD 1.0 day), in total comprising 19.9 hours (SD 8.0 hours) of work and 22.9 hours (SD 8.9 hours) of valid recordings off work (table 1). Cumulative distributions of the EVA derivatives describing the temporal pattern of sitting are shown in figure 2.
Figure 2
Cumulative probability distributions of exposure variation analysis (EVA) derivatives in the study population, ie, brief bursts (time in spent sitting <5 minutes), moderate periods (sitting periods of >5-20 minutes) and prolonged periods (sitting for more than >20 minutes) during work and the whole day.
Building of statistical models
Variance inflation estimates did not indicate any critical multicollinearity among the potential confounders.
The models including interaction terms between exposure variables and potential moderators only showed a significant interaction with BMI. Thus, only this interaction was entered in the final model, and other potential moderators were entered as confounder main effect terms. Secondary, a complementary model stratified on high (≥25 kg/m2) and low (<25 kg/m2) BMI was applied.
Of the potential confounders, only diagnosis with a herniated disc and rate of perceived exertion affected the association between exposure and outcome significantly. Thus, the final model included these two confounders only.
Primary analysis of association between sitting and LBP
The results from the crude and final models describing the association between sitting and LBP are shown in table 2. Sitting during work and whole day were not significantly associated with LBP intensity in crude, univariate models, neither for the total sitting nor for the EVA derivatives reflecting the temporal patterns of sitting. However, BMI, as the only moderating factor, appeared to interact significantly with total amount of sitting and sitting in brief bursts and moderate periods both during work and whole day (table 2).
Table 2
Associations between sitting (total time and temporal patterns (EVA derivatives)) during work and for the whole day (waking hours), and the intensity of low back pain (scale 0–10). 701 participants were included in the crude, univariate model (model 1) and 653 in the final model (model 2). [BMI=body mass index; CI=confidence interval.] Significant (P<0.05) associations are marked with bold.
| R2 | B | SE | P-value | 95 % CI | |
|---|---|---|---|---|---|
| Sitting at work Total (% of occupational hours spent sitting) | |||||
| Model 1 a | 0.002 | -0.07 | 0.06 | 0.28 | -0.19–0.06 |
| Model 2 b | 0.04 | 0.04 | 0.07 | 0.60 | -0.10–0.17 |
| Sitting×BMI interaction | -0.002 | 0.001 | 0.03 | -0.005– -0.0002 | |
| Brief bursts (≤ 5minutes) | |||||
| Model 1 a | 0.00 | -0.02 | 0.11 | 0.87 | -0.23–0.19 |
| Model 2 b | 0.04 | -0.01 | 0.11 | 0.91 | -0.23–0.20 |
| Sitting×BMI interaction | -0.007 | 0.003 | 0.03 | -0.01– -0.0006 | |
| Moderate periods (>5–20 minutes) | |||||
| Model 1 a | 0.002 | -0.09 | 0.08 | 0.31 | -0.25–0.08 |
| Model 2 b | 0.04 | 0.01 | 0.09 | 0.92 | -0.17–0.18 |
| Sitting×BMI interaction | -0.005 | 0.002 | 0.02 | -0.009– -0.0007 | |
| Prolonged periods (>20 minutes) | |||||
| Model 1 a | 0.0009 | -0.04 | 0.06 | 0.43 | -0.16–0.07 |
| Model 2 b | 0.04 | 0.05 | 0.06 | 0.41 | -0.07–0.18 |
| Sitting×BMI interaction | -0.0009 | 0.002 | 0.62 | -0.004–0.003 | |
| Whole day sitting | |||||
| Total (percentage of whole day spent sitting) | |||||
| Model 1 a | 0.003 | -0.17 | 0.12 | 0.16 | -0.41–0.07 |
| Model 2 b | 0.04 | 0.01 | 0.13 | 0.92 | -0.24–0.27 |
| Sitting×BMI interaction | -0.004 | 0.002 | 0.04 | -0.008– -0.0003 | |
| Brief bursts (≤5 minutes) | |||||
| Model 1 a | 0.0001 | 0.04 | 0.18 | 0.81 | -0.31–0.40 |
| Model 2 b | 0.03 | 0.08 | 0.18 | 0.68 | -0.28–0.44 |
| Sitting×BMI interaction | -0.01 | 0.01 | 0.03 | -0.03– -0.001 | |
| Moderate periods (>5–20 minutes) | |||||
| Model 1 a | 0.0007 | -0.11 | 0.15 | 0.49 | -0.40–0.19 |
| Model 2 b | 0.04 | 0.02 | 0.16 | 0.90 | -0.29–0.33 |
| Sitting×BMI interaction | -0.01 | 0.004 | 0.01 | -0.02– -0.003 | |
| Prolonged periods (>20 minutes) | |||||
| Model 1 a | 0.003 | -0.15 | 0.10 | 0.15 | -0.35–0.05 |
| Model 2 b | 0.03 | -0.04 | 0.11 | 0.71 | -0.26–0.18 |
| Sitting×BMI interaction | -0.0003 | 0.002 | 0.89 | -0.005–0.004 | |
An alternative model, in which data on temporal patterns of sitting were expressed in percent of the total amount of sitting rather than in percent of the overall measurement time, did not show any significant associations of temporal patterns with LBP intensity, neither for sitting during work nor whole day.
Stratified analyses of association between sitting and LBP
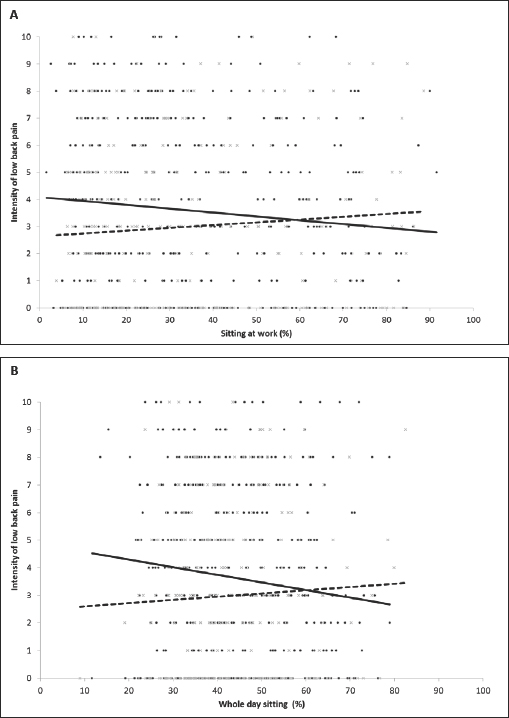
An unadjusted analysis was conducted in sub-populations stratified on BMI (low <25 kg/m2 and high ≥25 kg/m2). These stratified analyses showed that among participants having a low BMI, more sitting (total, brief bursts, and moderate periods) was associated with an increased LBP intensity, both during work and whole day (table 3, figure 3). In contrast, among those having a high BMI, more sitting during work or for the whole day was associated with a decreased LBP intensity. The stratified analysis was additionally adjusted for herniated disc and rate of perceived exertion, just as the final model for the entire population; however, this adjustment didn´t change the estimates numerically or statistically (results not shown).
Table 3
Crude associations between sitting (total amount and temporal patterns (EVA categories)) during work and for the whole day (waking hours), and the intensity of low back pain (scale 0–10), stratified on low (<25 kg/m2, N=238) and high (≥25 kg /m2, N=447) body mass index (BMI). Significant (P<0.05) associations are marked with bold.
Figures 3A and B
Scatter plots and regression lines illustrating the crude association between sitting during work (A) and the whole day (B) expressed in percent and pain intensity and stratified on body mass index (BMI): low <25kg/m2, N=238; high ≥25 kg/m2, N=447. The solid line represents participants in the high BMI category. The dashed line represents the participants in the low BMI category.
Sensitivity analyses
All of the sensitivity analyses – one including age and sex as confounders, one including social support and influence at work as confounders, and one exploring associations only among participants with LBP (N=212) by excluding those reporting to have no LBP – resulted in numerically and statistically similar findings to those reported in table 2 (results not shown).
Discussion
We did not find any significant associations between total sitting and intensity of LBP (table 2), neither during work nor the whole day. Neither did we find associations between temporal patterns of sitting (brief bursts, moderate periods, prolonged periods) and intensity of LBP (table 2). Therefore, we rejected the hypothesis of a positive association between sitting and LBP intensity.
None of the previous studies addressing associations between sitting and LBP (11, 19, 20, 27) considered the possible effect of moderating factors (20). Therefore, we investigated the extent to which the association between sitting and LBP was moderated by factors traditionally classified as confounders (24, 25). Among the investigated potential moderating factors, only BMI significantly interacted with sitting, and was therefore included in the final model. An analysis stratified on high and low BMI indicated that in the low BMI (<25 kg/m2) group LBP intensity increased with an increased amount of sitting, while LBP intensity decreased with an increased amount of sitting in the high BMI (≥25 kg/m2) group (figure 3, table 3); even if none of these associations were very strong. An explanation for the association between increased sitting time and decreased LBP among those with high BMI could be that sitting indirectly protects against alternative non-sitting activities that may cause added strain on the back among those with high BMI. However, high BMI may also reflect high muscle mass rather than obesity, as suggested by Fogelholm (48). If so, the mechanisms behind BMI as a potential modifier are less straight forward and should be further explored in future studies with measurement, eg, muscle mass or muscle strength.
To our knowledge, no previous studies have addressed the temporal pattern of sitting in relation to LBP. Our analyses indicated that EVA derivatives reflecting the temporal sitting pattern (ie, brief bursts, and moderate and prolonged periods) were not associated with LBP intensity. This stands in contrast to studies arguing that breaks from prolonged sitting are beneficial for health outcomes (49–51). However, breaks from sitting may increase the exposure to other risk factors for LBP, such as awkward working postures (6, 52). On the other hand, longer uninterrupted periods of sitting may also increase the risk for LBP due to the constrained body posture. Accordingly, prolonged sitting has been shown to be associated with periods of uninterrupted, low-intensity muscle contractions, which may lead to increased blood pressure and increased systemic levels of pro-inflammatory cytokines (51, 53, 54). The proposed beneficial health effects from breaking up prolonged periods of sitting are consistent with the general notion that sufficient variation in body postures and loads is a necessary prerequisite for good musculoskeletal health (13, 14).
The limited importance of sitting for LBP found in our study suggests that LBP likely depends on what workers do when they do not sit. Thus, future research into associations between sitting and LBP should focus on the whole timeline of physical activities and postures, and examine the effect of combinations of different physical activities, including their temporal pattern. Such studies would be particularly warranted among workers that do not sit for considerable parts of their working hours. Also, emphasis should be given to understanding the extent to which a possible effect of sitting is moderated by what workers do when they do not sit. Additionally, prospective studies of associations between sitting and LBP should be encouraged to gain a better understanding of sitting as a possible predictive risk factor.
Methodological considerations
The present study was based on objective measurements of duration of sitting by use of two tri-axial accelerometers. This allows discrimination of, eg, sitting from lying and standing, and thus minimizes misclassification of exposure. Thus, detailed patterns of sitting (and other activities) can be assessed validly across several days. The relatively large size of the present study population is an additional strength since it allows detection of even small effect sizes with a good statistical power. The study population mainly consisted of blue-collar workers with a reasonably homogenous socioeconomic status, minimizing possible confounding.
However, the study also suffers from some limitations. The cross-sectional design of the study prevents conclusions regarding causal relationships between sitting and intensity of LBP. An additional limitation is the different time windows for assessing exposure and outcome; the exposure was recorded by accelerometers mounted at the health check and measuring during 2–4 working days after that, and the intensity of LBP was measured retrospectively in a questionnaire. However, we assume the recorded exposure to be representative even for a period preceding the measurements, thus these non-synchronous time windows should not present a serious flaw with respect to the investigated associations. Additionally, these results are derived from a population of mainly blue-collar workers and are therefore not valid in other populations, such as mainly white-collar workers. Data were not available from all included participants on self-reported social support and influence at work. Therefore, we could not completely rule out confounding by psychosocial factors. However, we conducted a sensitivity analysis in a sub-sample (N=460) of workers allowing additional adjusting for self-reported level of social support and influence at work. This analysis led to numerical and statistical results similar to the final model on the entire population (table 2), suggesting these results to be robust.
Concluding remarks
The present study found no significant associations between total duration or temporal patterns of sitting and intensity of LBP, neither during work nor for the whole day. Thus, the investigated hypotheses – that an increased amount of sitting will increase the intensity of LBP and the temporal pattern of sitting is important to LBP – were rejected. BMI significantly interacted with sitting and LBP, and a stratified analysis showed weak positive associations among those having a low BMI (<25 kg/m2), and weak negative associations among those with a high BMI (≥25 kg/m2).
Together, these results suggest that sitting may not be independently associated with peak intensity of LBP, which points towards other exposures being more powerful risk factors for LBP or to the association between sitting and LBP intensity being significantly modified by exposures during non-sitting periods of work.