Currently, 322 million people suffer from depression in the world (1) and major depression approximately affects 30.3 million in Europe (2). Depression is the third cause of burden of disease worldwide, and its burden increased by 18% in the 2005–2015 period (3). By 2030, depression will be the leading cause of burden of disease in the world (4).
Although there are effective treatments for depression, they can only reduce the burden of disease by 20–30% (5) due to accessibility problems, errors in diagnosis (6), partial effectiveness of treatments (7) and lack of adherence (8). In developed countries, despite substantial increases in the provision of treatment for depression from 1990–2015, its prevalence has not decreased (9). This is in part due to the so-called preventive gap: the incidence of new cases of depression is very high. Indeed, even in the hypothetical case that all existing cases of depression were treated adequately, new cases could only be avoided through primary prevention.
The effectiveness of psychological and educational interventions in the prevention of depression is small to moderate (10). Educational interventions simply provide information about depression through lectures or fact sheets, while psychological interventions attempt to change the way people think using a variety of strategies (eg, cognitive behavioral or interpersonal therapy). They share a similar working mechanism of action that facilitates changes in attitudes and behaviors so that it makes sense to treat them as similar enough to combine in a meta-analysis. Information and communication technologies (ICT) can be employed for spreading these preventive interventions, as well as their implementation in settings such as school, primary care and the workplace. Currently, there is evidence of the effectiveness of ICT-based depression prevention programs (11) in schools (12) and primary care (13). Nevertheless, there is a lack of evidence regarding their effectiveness in the workplace.
The total cost of work-related depression in the EU27 nearly reaches €620 billion per annum. The major impact mostly affects employers as a result of absenteeism and presenteeism (€270 billion), followed by loss of productivity (€240 billion), the healthcare systems due to treatment costs (€60 billion), and the social welfare system due to disability benefit payments (€40 billion) (14).
In the EU Compass for Action on Mental Health and Well-being, the European Union prioritized seven strategies, two of which consisted of preventing depression and promoting resilience (for 2016) and mental health in the workplace (for 2017) (15). The workplace has been suggested as an appropriate place for the implementation of depression prevention programs for several reasons: (i) Depression affects mostly people of working-age; up to 60% of the world population has some type of employment or work activity, and 60% of our waking life is spent at the workplace (16, 17). (ii) Depression is the leading cause of sick leave and loss of productivity in most developed countries (18). (iii) An adverse work environment is a well-established risk factor for mental disorders in general and for depression in particular (19). (iv) There is growing scientific interest in developing strategies for the prevention of depression in the workplace. This is in part because organizations are increasingly aware they are partly responsible for the health of their employees (20, 21). (v) A systematic review of economic evaluations revealed that prevention interventions or the treatment of mental health problems in the workplace would be cost-effective and a profitable investment (22).
Some systematic reviews and meta-analyses have been conducted to assess the effectiveness of interventions in reducing depressive symptoms in the workplace (23–25). Two of them provided evidence of their effectiveness, but patients with baseline depression were not excluded and the effect of treatment could not be separated from that of prevention. Two other meta-analyses (26, 27) have been recently published on the effect of eHealth and web-based interventions on mental health and stress in the work environment. Although some evidence has been provided of their effectiveness, the effects of prevention could not be distinguished from those of treatment. Therefore, our objective was to evaluate the effectiveness of psychological and educational interventions in preventing depression in the workplace through a systematic review and meta-analysis of RCT.
Methods
This systematic review and meta-analysis was performed in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines (28). The protocol was previously recorded in the international registry of systematic reviews called PROSPERO (International Prospective Register of Systematic Reviews), registration number: CRD42017055728.
Search strategies
We systematically searched six electronic databases, including PubMed, PsycINFO, EMBASE, CENTRAL (Cochrane Central Register of Controlled Trials), CIS-DOC (Occupational Safety and Health Databases) and Open Grey (System for Information on Grey Literature in Europe) from inception to 19 September 2018. No date or language restrictions were imposed. This search strategy was complemented with hand searching of reference lists of reviews on this topic (23–27, 29, 30). In addition, the references of the studies selected were also reviewed. The descriptors used were “depressive disorder”, “prevention”, “workplace”, and “randomized controlled trial”. The search strategy was first tested in PubMed and then adapted to the other electronic databases. More details on search strategies used in this study are shown in supplementary table S1 (www.sjweh.fi/show_abstract.php?abstract_id=3791).
Eligibility criteria
We only selected RCT because this design is the least biased way to evaluate effectiveness (31). Participants were required to have been recruited in the workplace, and the effectiveness of prevention had to be separated from that of treatments. Baseline depression was required to have been discarded through standardized interviews (eg, Composite International Diagnostic Interview), validated self-reports based on standard cutoff points (eg, Beck Depression Inventory) or by a mental health specialist. We selected studies in which the primary or secondary outcome was the incidence of depression or the reduction of depressive symptoms as assessed by standardized structured interviews or validated scales of depressive symptoms. RCT on psychological and educational interventions were included and those on medication or physical interventions (eg, physical exercise) were discarded. The comparators allowed included usual care, non-intervention (the evaluation measurements used were the same as those employed in the intervention group but no specific intervention is performed), waiting list and attention control (active control or placebo).
Selection of studies
Two reviewers independently selected the studies from electronic databases and other sources, and duplicate studies were removed. Titles and abstracts were reviewed to identify studies meeting our inclusion criteria. The studies found to be potentially eligible underwent fulltext reading to determine if all inclusion criteria were met. A third reviewer resolved discrepancies between the reviewers. Based on Cohen’s kappa coefficient (32), the degree of agreement between the initial reviewers was good [Cohen ĸ=0.62, 95% confidence interval (CI) 0.45–0.78] (33).
Data extraction
Two independent reviewers extracted data using a table of evidence based on our protocol and introducing some modifications from real available data. Discrepancies between the reviewers were resolved by consensus. Data extracted from each study included: author(s), year of publication, country, target population, type of prevention, baseline depression as exclusion criteria, sample size (control and intervention), interventions, orientation of interventions, number of sessions, format of interventions, facilitator, outcome, follow-up time and risk of bias score. When required information was not provided in the article, the authors were contacted.
Assessing the risk of bias
The methodological quality of studies was evaluated in accordance with the instrument described in chapter 8 of the Cochrane Collaboration Manual for Systematic Reviews was used (34).This instrument measures the quality of RCT based on six criteria: (i) generation of the sequence, which makes reference to the rule used for allocating interventions to participants based on a random process; (ii) allocation concealment, which refers to the method employed to conceal the allocation sequence to determine whether interventions allocations could have been anticipated before or during enrolment; (iii) blinding of participants and study staff, which refers to the measures used to blind participants and study staff to the intervention each participant received; (iv) blinding of evaluators of outcomes, which refers to the measures taken to blind the evaluators of outcomes to the intervention each participant received; (v) incomplete results data, refers to the methods used to deal with missing data (eg, multiple imputation); and finally, (vi) another source of bias, which refers to the availability of the trial protocol. Items were rated as “high risk of bias”, “unclear risk of bias” and “low risk of bias”. Studies that scored high risk of bias in specific domains (generation of the sequence, allocation concealment or blinding of evaluators of outcomes) were considered to have a high overall risk of bias. Two reviewers independently evaluated quality, and a third reviewer resolved discrepancies. There was an excellent degree of agreement among the reviewers (intraclass correlation coefficient=0.86, 95% CI 0.63–0.95) (35).
Statistical analysis
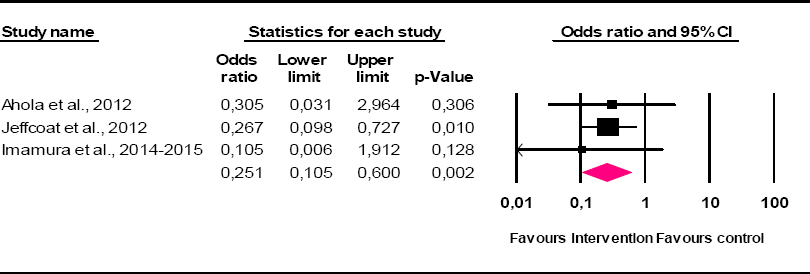
Since the cumulative incidence of depression was reported in all the RCT included in our meta-analysis, odds ratio (OR) could be used to compare results and obtain a global effect size. Fixed- and random-effect models were used to calculate the pooled OR and its CI. According to Brownson et al (36), OR<0.5 and <0.25 should be considered a moderate- and high-effect size, respectively. Pooled OR and OR of each of the studies included in our meta-analysis and their CI were displayed graphically on a forest plot. I2 statistic was estimated to determine if effect sizes were homogeneous across trials. I2 describes the percentage of variability in effect estimates caused by heterogeneity rather than by sampling errors (chance). A rough guide to interpretation would be to assign adjectives of low, moderate, and high to I2 values of 25%, 50%, and 75% (37). The result of the I2 statistic was complemented by Cochrane’s “Q” heterogeneity test. A statistically significant result indicates that effect sizes are heterogeneous and, consequently, the size of the average effect does not represent them well (37). For the introduction and analysis of data, version 2.2.064 of the Comprehensive Meta-Analysis statistical program (Biostat, Englewood, NJ, USA) was used.
The quality of evidence
We followed the Grading of Recommendations Assessment, Development and Evaluation (GRADE) working group methodology (38) for assessing the quality of evidence. We were taken into account the domains of risk of bias, consistency, directness, precision and publication bias.
Results
Searches in electronic databases yielded 2263 potentially eligible articles. After a review of the reference lists of relevant systematic review and meta-analyses, 81 more articles were identified. After duplicates had been removed, the titles and abstracts of 1963 articles were reviewed, of which 1894 were excluded for meeting one or several exclusion criteria. Then, the fulltext of 69 studies was reviewed, of which 66 were excluded for the reasons listed in supplementary table S2 (add URL): 40 because baseline depression was not discarded by standardized diagnostic interviews, validated symptom scales based on a cut-off point or a mental health specialist; 10 because participants were not recruited in the workplace; 6 because their design was other than RCT; 9 because they did not provide outcomes on the incidence of depression or the reduction of depressive symptomatology; and 1 because the comparator group was other than usual care, non-intervention, active control, waiting list or placebo. Only 3 RCT, reported in four publications, met all our inclusion criteria. Figure 1 shows the flowchart (28).
Table 1 shows the characteristics of the included RCT: two (39, 40) were conducted in 2012 and another, reported in two publications (41, 42), was conducted in 2014. An RCT was carried out in Finland (39) with workers from both public and private companies. Another study was performed in the public and private education sector in the United States (40); and another study was undertaken in Japan (41, 42) with workers of the private sector. A total of 1246 participants were evaluated (632 in the intervention group and 614 in the control group). The three RCT evaluated universal prevention programs with non-depressed workers but with any level of risk of depression. As for the instruments used to discard depression at baseline, one RCT (39) used the Beck Depression Inventory (BDI-13 ≤4), another RCT (40) used the Depression Anxiety Stress Scales (DASS-D <10), and the third used the Composite International Diagnostic Interview (41, 42). All preventive interventions were psychological, two with cognitive-behavioral orientation (39, 41, 42) and another was based on acceptance and commitment therapy (40). The number of sessions ranged from 4–6, and only one RCT had a group format (39). The incidence of depression was one of the outcomes assessed in the three RCT, although it was measured by a structured diagnostic interview in only a study (41, 42). Follow-up duration ranged from 2.5–7 months.
Table 1
Characteristics of the randomized controlled trials on the prevention of depression in the workplacethat were included.
Table 2 describes the risk of bias for each of the RCT included in our meta-analysis. The randomization sequence appeared to be appropriately generated in all of the RCT by various forms of computer-based (40), permuted-block randomization (41, 42) and shuffled questionnaires dealt into two piles envelopes (39). Therefore, we assessed this item as at low risk of bias in all included RCT. We rated all the three RCT as being at low risk of allocation concealment bias, as they reported methods which consisted of sealed envelopes (39), random table with password protected and blinded (41, 42) and a computer program (40). The blinding of participants and personnel item was classified as high risk in all of the RCT because the nature of psychological and educational interventions makes them difficult to blind. Blinding of outcome assessment was undertaken in two RCT (40–42) and these studies were therefore judged to be at low risk of bias. The other one was classified as unclear risk of bias due to a lack of sufficient information (39). An intention-to-treat analysis was undertaken in two RCT (40–42) but none of them provided enough information about the imputation of missing data, and thus we judged these two RCT to be at unclear risk of incomplete outcome data. No information about intention-to-treat analysis and management of missing data were found in Ahola et al (39) study, so we judged it to be at high risk of bias. There was unclear risk of selective reporting bias in two RCT because no study protocols were available (39, 40). Only one RCT was assessed as being at low risk as they provided the protocol trial registration (41, 42).
Table 2
Risk of bias of the randomized controlled trials on the prevention of depression in the workplace.
The pooled OR assuming the fixed-effects model was 0.251 (95% CI 0.105–0.600, P=0.002) and heterogeneity was not relevant (I2=0, Q=0.389, d.f.=2, P=0.823). This means that interventions for the prevention of depression in the workplace were effective and the effect size was moderate and statistically significant. When estimates were made by the random-effects model, the result was identical. Figure 2 shows the forest plot.
Quality of the evidence
The initially grading of the quality of the evidence was high since we included only RCT. Once we reduced the rating from high to moderate because the number of RCT included was too small for drawing conclusions about possible publication bias. Imprecision across studies was found (only three trials were included and there were few events) therefore we once again downgraded from moderate to low. Outcome effects were consistent across RCT. Regarding indirectness, it was low since the target population, the interventions and our outcome did not differ from those of primary interest. The risk of bias was not high because none of the studies scored high in any of the domains that we previously considered. In addition, our findings are based on RCT with interventions that have been tested in head-to-head comparisons. In summary, the quality of evidence was low.
Discussion
We carried out a systematic review and meta-analysis of RCT that evaluated the effectiveness of psychological and educational interventions for the prevention of depression in the workplace. The three studies selected were conducted in three different countries and continents and included a total of 1246 workers from the public and private sector. Psychological or educational interventions may prevent depression in the workplace, although the quality of evidence was low.
Strengths
As far as we know, this is the first meta-analysis to evaluate the effectiveness of psychological and educational interventions in the prevention of depression in the workplace. Of the four meta-analyses published so far on interventions in reducing depressive symptoms in the workplace, three obtained a small but statistically significant effect size (23, 25–27) and another did not reveal any effectiveness (24). However, employees with baseline depression were not excluded in any of these four meta-analyses. Therefore, their findings are not applicable to the prevention of depression. In any case, their inferences could be made in relation to the set of depressed and non-depressed employees. In our study, we used a large number of electronic databases that were complementary (biomedical, psychosocial, occupational, grey literature and specific for RCT). Search was complemented with manual search of reference lists of other systematic reviews and meta-analyses and trials. In addition, the search terms used were wide enough for the search to have an adequate sensitivity. Two independent and trained evaluators selected studies, evaluated the risk of bias, and extracted data from trials, which had good reliability indices. Another strength of our study is that only RCT were included in our systematic review, since this design is the least biased way to evaluate effectiveness.
Limitations
The main limitation of our study is that only three RCT met our inclusion criteria. Therefore, we should be cautious when affirming that psychological and educational interventions are effective in the prevention of depression in the workplace. Furthermore, even if representativeness was achieved for a relatively high number of employees (1246 workers) and each of the three trials was carried out on a different continent, the small number of RCT limits the external validity of our study. In any case, when a meta-analysis is approached from the fixed-effects model – as it is our case – it makes sense to estimate a combined effect size from just two RCT (43). It has been suggested that a meta-analysis requires ≥10 studies for conclusive statistical calculations to be performed on the existence of publication bias (44). Therefore, final conclusions cannot be drawn.
Although point estimates of the preventive effects of the RCT included in our study were relevant (all OR were ≤0.30), statistical significance was reached in just one RCT. This is a common problem in approaches to universal prevention (without selecting high-risk participants) (45) and when follow-up is short, as occurred in the three RCT included in our study. This way, at the end of follow-up there were few new cases of depression, which ranged from 0–6 in the intervention groups and from 3–17 in the control groups. Therefore, further RCT on the prevention of depression in the workplace should be performed with samples that have sufficient statistical power and longer follow-up, especially in the context of universal prevention interventions. In fact, no RCT was found with a follow-up of ≥12 months. As a result, we cannot draw conclusions on the long-term effectiveness of preventive interventions. Due to lack of variability, subgroup and sensitivity analyses could not be carried out as proposed in the protocol. Thus, we could not determine – for example – if psychological interventions were more effective than educational ones or if RCT with a higher risk of bias were more effective than those with a lower risk.
The three RCT included in our study evaluated the cumulative incidence of new cases of depression. However, incidence was assessed by a structured standardized interview in just one RCT. The same applies to the exclusion of participants with baseline depression. In principle, standardized and structured interviews have greater validity than symptom scales, when a standardized cut-off is used to establish a diagnosis of depression. With the aim of including only non-depressed participants, in the RCT of Ahola et al (39), we only used the subsample of participants that obtained a score ≤4 on the BDI-13 scale at baseline. This cut-off point has greater sensitivity than the one commonly used in this scale to determine the presence of depression (>9). By using this cut-off point, we minimized false negative diagnoses of depression, thus ensuring that participants did not have depression, although false positives increased and sample size decreased.
Practical implications and research needs
The workplace offers excellent conditions for the implementation of prevention programs for depression to reach a large proportion of the population. If evidence was published that prevention programs of depression in the workplace are effective and cost-effective, decrease sick leaves and increase productivity, many companies would be interested in sharing the costs of these programs. Regarding the economic evaluation, the systematic review that included both non-depressed and depressed patients suggested that prevention interventions or treatment of mental health problems in the workplace could be cost-effective (22) and improve return to work (46). More RCT are needed to evaluate economic and organizational outcomes and assess the physical and mental status of employees.
Larger, long-term RCT with low risk of bias, where baseline depression is discarded and standardized structured interviews are employed to evaluate the occurrence of depression, are needed.