High levels of sitting are associated with negative health outcomes (1, 2). Although workplace interventions can effectively reduce sitting time (3), employers are often concerned with the impact of interventions on productivity, a key metric in the workplace (4). In the most basic terms, productivity is a measure of production quantity and quality from the resources available (5). However, measuring productivity is notoriously difficult, as some of its facets, such as employee interactions, can be difficult to measure (6), while others are more easily quantified. Workplace sitting-reduction interventions could alter various facets of productivity in adverse or beneficial ways, such as increasing distractions (7) or altering blood flow dynamics to the brain with sit-to-stand transitions (8).
In the laboratory, researchers have examined the influence of workplace-sitting-reduction interventions on productivity in a diverse manner, with productivity outcomes ranging from objective performance of work tasks to self-reported overall productivity. Compared to sitting, interventions involving the completion of objective work tasks while standing have shown increased creative problem solving (9) but no significant changes to cognition (10) or computer mouse and keyboard performance (11). Interventions using active workstations have also reported varying impacts on objectively measured work tasks (10, 11). Findings concerning individual components of productivity in a controlled laboratory environment, however, do not necessarily translate to overall productivity in a free-living work environment.
Much of the evidence on potential changes to productivity in free-living workplace interventions has come from questionnaires or focus groups. Qualitative assessments from a treadmill desk intervention reported productivity improvements when measured over a year (12), while interventions with sit-stand workstations have reported no large or significant changes (13–16). Recent reviews concluded that sit-stand workstation interventions have no impact on productivity, but they have highlighted that more research is needed, especially pertaining to free-living interventions of longer durations since greater amounts of time may be needed to see improvements in productivity (17, 18). Additionally, little research exists regarding multi-component intervention strategies which target workplace cultural and individual changes and the extent to which such strategies may differentially impact constructs of productivity (eg, work performance, physical tolerance, psychosocial well-being, social/role functioning, and absenteeism). Brown and colleagues (19) have previously defined and described these five key productivity-related constructs in detail.
As previously reported, the multi-component workplace intervention, Stand Up Victoria, effectively reduced the primary outcome of workplace sitting time (20), improved overall cardiometabolic risk scores (21), but had no significant impact on absenteeism (22). The aim of this study was to examine the initial (3-month) and long-term (12-month) effects of the Stand Up Victoria intervention on the self-reported overall productivity outcomes as well as the individual productivity constructs assessed in the trial. The difference between the short and long-term outcomes, which may diverge due to a positive learning curve effect or conversely a lack of sustainability, was also examined. A secondary, exploratory aim was to examine the association of changes in the composition of workplace sitting, standing, and stepping with changes in overall productivity.
Methods
The Alfred Health Human Ethics Committee (Melbourne, Australia) approved the Stand Up Victoria trial, which was prospectively registered with the Australian New Zealand Clinical Trials register (ACTRN12611000742976). The study was conducted in accordance with the CONSORT guidelines for cluster-randomized trials (www.consort-statement.org). Details have previously been published on the intervention development (23), study protocol (24), the worksite level characteristics (25), the primary activity outcomes (20), including the changes in activity composition (26), the secondary cardiometabolic risk outcomes (21), and the economic impact outcomes (22).
Settings and participants
A single multi-site public service organization was recruited to participate in the study. From this organization, worksites separated by ≥1 km were recruited and randomized to either the intervention or control. Eligibility criteria for participants were: aged 18−65 years, ambulatory, able to speak English, able to stand or sit for ≥10 minutes continuously, and at least 0.6 full-time equivalent work hours with access to a telephone, internet, and desk within the workplace. All participants were informed of the risks involved with the study and each provided written informed consent. Participants and study staff were unblinded to group allocation.
Control – usual practice
Participants in the control group underwent the same assessment protocol as the intervention group. At 3 and 12 months, control participants received written feedback on their activity and biomarker outcomes.
Intervention
Details of the Stand Up Victoria intervention have been described previously (24). Briefly, Stand Up Victoria was a multi-component intervention designed to reduce sitting with an emphasis on reducing prolonged, unbroken sitting bouts lasting ≥30 minutes. Although the goal was to reduce sitting across the entire day, the primary focus was to reduce workplace sitting. The main message of the intervention, “Stand Up, Sit Less, Move More”, targeted the replacement of sitting with either standing or stepping. The intensive phase of the intervention lasted three months and included organizational, environmental, and individual components. The organizational components included consultations where management was informed about the study’s broad aims to gather management support. Following brainstorming sessions to decide on intervention strategies appropriate for the various sites, participants selected site-specific strategies. Additionally, worksite team leaders were recruited to promote the intervention strategies through role modelling and sending emails. The environmental component involved the installation of sit-stand workstations. Lastly, the individual component included one-on-one health coaching which was face-to-face for the initial three days after installing the new workstation and was followed by four telephone calls at 2, 4, 8, and 12 weeks. After three months, the participants retained their sit-stand workstations while the health coaching ceased and the worksites were left to maintain the intervention on their own.
Data collection and measures
Measurements were taken at baseline, 3 months (end of intensive phase), and 12 months via onsite physical and blood-draw assessments, device-based activity monitoring, and a self-administered online questionnaire (LimeService: www.limeservice.com).
Productivity outcomes
Two different productivity questionnaires were used as recommended for studying the relationship between physical activity and work productivity (19): the Health and Work Questionnaire (HWQ) and the Work Limitations Questionnaire (WLQ). The HWQ and WLQ include measurements of 4 out of 5 defined constructs of productivity (work performance, physical tolerance, psychosocial well-being, and social/role functioning). The WLQ also includes measurement of the 5th construct: absenteeism (19). It is acknowledged that both the HWQ and the WLQ overlap in their measurement of constructs and were originally designed to examine the impact of chronic health problems on productivity (19). However, at the time of our study development, we decided to use both measurements as there was limited evidence indicating the ideal productivity questionnaire to use in the context of workplace sedentary behavior interventions, particularly those applying multi-component approaches.
Health and Work Questionnaire (HWQ)
The HWQ is a 30-item questionnaire that asks participants to rate (on a 10-point response scale) their performance over the previous week from multiple perspectives, including their own, and in the eyes of their supervisor and coworkers. These latter items are designed to reduce social desirability bias. HWQ items are grouped and averaged to create a total score and six subscales: productivity, concentration/focus, supervisor relations, non-work satisfaction, work satisfaction, and impatience/irritability (27; details provided in supplementary material www.sjweh.fi/show_abstract.php?abstract_id=3820, table S1). Three items are not included in any subscale and are reported on their own: stress, job control, and ability to finish work on time. Depending on the HWQ outcome measure, higher or lower scores indicate better productivity (see table S1). Strong internal consistency was previously shown in the HWQ total score (α=0.81) and subscales (α=0.72−0.96) (27). There is some validation evidence for the HWQ: its various measures (except non-work satisfaction) have shown significant correlations (ρ≈0.2) with an objective indicator of workplace productivity (27).
Work Limitations Questionnaire (WLQ)
The Work Limitations Questionnaire (WLQ) measures the frequency of difficulty associated with performing work tasks over the previous two weeks using 25 items with a 6-point response scale, including “not applicable” (28). WLQ items are grouped into four subscales: time demands, physical demands, mental/interpersonal demands, and output demands (see table S1), with lower scores indicating better productivity. Each subscale has previously been shown to have strong internal consistency (α=0.90−0.96) (28). A WLQ at-work productivity loss score was also calculated to determine the overall percent productivity lost due to health limitations (29). The weighted productivity loss score has been moderately correlated with objective productivity metrics (r=0.46) (30) and is recommended for studying the relationship between physical activity and work productivity (19). When scoring the WLQ, instructions state to exclude participants who fail to meet the criteria of ≥50% of WLQ subscale items being valid responses rather than missing or “not applicable” (29). However, in view of CONSORT intention-to-treat principles and possible biases, we did not exclude this small number of participants: at most nine individuals for the physical demands subscale and none or one for the remaining subscales.
Workplace sitting, standing, and stepping
A range of activity measures including sitting, standing, stepping and stepping at moderate-vigorous level were collected at baseline and 3 and 12 months via the activPAL3™ (PAL Technologies Limited, Glasgow, UK; minimum version 6.3.0), with a self-completion log used to ensure the measurements excluded time outside the workplace (if appropriate), sleep, and device non-wear. The monitor was secured onto the right thigh with a hypoallergenic patch and participants were asked to wear the monitor continuously (24 hours/day) for 7 days. Full details regarding the methods used including valid day criteria are described previously (20).
Other baseline characteristics
A member of the research team determined body mass index (BMI, kg/m2) which was calculated from average height (measured in duplicate to the nearest 0.1 cm) and weight (measured in the voided and fasted state to the nearest 0.1 kg). Additional data were collected from the self-administered questionnaire. Ratings of fatigue, headaches, digestive complaints, and sleep quality during the previous week were collected (24). The presence/absence of any discomfort in the lower back and lower and upper extremities over the previous seven days were assessed via the Nordic Musculoskeletal Questionnaire (31, 32). Status regarding high cholesterol and diabetes was based on prior diagnosis by a doctor and by fasting levels at baseline, measured as described previously (21). Quality of life was assessed as the physical and mental super domains of the Assessment of Quality of Life tool (AQoL-8D) (33). Workspace satisfaction was assessed using items from a validated questionnaire (34).
Sample size
Sample size details have been described previously (24). The sample size was selected a priori to provide adequate power for the primary activity outcome (workplace sitting time); not the secondary productivity outcomes. In the absence of good data regarding minimal clinically important differences, our minimum difference of interest was set at a “medium” effect size [0.5 standard deviation (SD)].
Statistical analyses
Analyses were performed in Stata Version 15 (StataCorp LLC, College Station, TX, USA) and R version 3.4.2 (R Core Team, Vienna, Austria) with statistical significance set at P<0.05, two-tailed. Interactions are reported at P<0.1. Due to the absence of evidence regarding what might be minimal clinically important differences for the HWQ and WLQ, outcome variables were modelled as a ratio of the baseline standard deviation (outcome / baseline standard deviation), yielding standardized effect sizes that can be considered small (0.2), medium (0.5) or large (0.8) based on the commonly-accepted criteria for doing so. Standardization of scores also facilitated comparisons between results for the various outcomes. Intervention effects and changes within groups were determined using linear mixed models. Models included fixed effects of group (intervention/control), time (3/12 months), the group×time interaction, baseline values of the outcome, potential confounders, random intercepts for workplace (REML estimation), and used an unstructured variance-covariance structure for the repeated measures. From a list of all potential confounders that was first identified a priori, models were adjusted for potential confounders if associated with the outcome at P<0.20 in backwards elimination, along with baseline values of the outcome, age, and gender (see supplementary table S2). Estimates of change within groups, differences between groups (ie, intervention effects), and the comparisons of initial and longer-term effects were obtained from marginal means and pairwise comparisons of marginal means.
Evaluable case analyses were used, with sensitivity to missing data assumptions evaluated. Activity data were included with a 1-valid-day minimum requirement (monitor worn for ≥80% of waking hours and for ≥10 hours when waking hours were inferred from movement). Missing data were imputed by chained equations, with m = 50 imputations. Imputation models included the analytic variables, cluster, and any variables that showed an association with the odds of missing data at P<0.2 (supplementary table S3).
Associations of intervention participants’ changes in the composition of time at the workplace (sitting, standing, and stepping) with their changes in overall productivity were examined using compositional data analysis — a process to outcome evaluation framework that enables valid simultaneous evaluation of all activities at once (35). At baseline and 3 and 12 months, the composition of workplace time (sitting, standing, and stepping) was calculated from the broader composition of time use on those days, including any time not at the workplace, sleep time and non-wear. As in previous papers (26), compositional changes were calculated by Aitchison’s perturbation method (36), transformed via isometric-log ratio transformation, and then tested in relation to outcomes via linear mixed models. Results are presented in terms of marginal means observed with various changes in activity.
Results
As previously reported (20), 278 employees expressed interest in the study, with 231 (5–39 per worksite) eligible and enrolled in either the control (N=95, 7 worksites) or the intervention (N=136, 7 worksites) (supplementary figure S1). Baseline characteristics are provided in table 1. Intracluster correlations (supplementary table S4) showed worksite clustering in productivity measures ranged from inestimably small (<0.001) to 0.100. Relevant data on outcomes and confounders were available from 184–188 participants (80–81%) concerning 3 months and 150–153 participants (65–66%) concerning 12 months. The odds of having missing data were not significantly different between intervention and control groups (P=0.441), but were significantly higher for smokers than non-smokers (P=0.021). There was also a non-significant tendency for participants who had lower- or upper-extremity discomfort and higher baseline workplace sitting time, to be less likely than their respective counterparts to have missing data (supplementary table S3).
Table 1
Baseline characteristics of the Stand Up Victoria participants (N=231, 14 worksites), intervention (N=136, 7 worksites), and control (N=95, 7 worksites) groups. [HWQ=Health and Work Questionnaire; WLQ=Work Limitations Questionnaire; SD=standard deviation; BMI=body mass index.]
| Intervention | Control | All | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Mean (SD) | N (%) | Mean (SD) | N (%) | Mean (SD) | N (%) | |
| Age (years) | 44.6 (9.1) | 136 | 47.0 (9.7) | 95 | 45.6 (9.4) | 231 |
| Female | 89 | (65.4) | 69 | (72.6) | 158 | (68.4) |
| BMI (kg/m2) | 28.61 (6.46) | 136 | 28.61 (5.48) | 95 | 28.61 (6.08) | 231 |
| HWQ a | ||||||
| Total score | 7.0 (1.2) | 131 | 7.3 (1.3) | 89 | 7.1 (1.3) | 220 |
| productivity | 7.2 (1.3) | 132 | 7.3 (1.3) | 89 | 7.2 (1.3) | 221 |
| Concentration/ focus b | 4.3 (2.3) | 131 | 4.0 (2.5) | 89 | 4.2 (2.4) | 220 |
| Supervisor relations | 7.2 (2.1) | 132 | 7.5 (2.1) | 89 | 7.3 (2.1) | 221 |
| Non-work satisfaction | 7.3 (1.7) | 132 | 7.9 (1.9) | 89 | 7.5 (1.8) | 221 |
| Work satisfaction | 6.1 (1.6) | 132 | 6.5 (1.5) | 89 | 6.2 (1.6) | 221 |
| Impatience b | 3.0 (1.7) | 131 | 2.8 (1.7) | 89 | 2.9 (1.7) | 220 |
| Stress item b | 4.9 (2.4) | 132 | 4.7 (2.4) | 89 | 4.8 (2.4) | 221 |
| Job control item | 5.8 (2.5) | 132 | 6.0 (2.2) | 89 | 5.9 (2.4) | 221 |
| Fail to finish Work item b | 2.3 (2.0) | 131 | 2.9 (2.5) | 89 | 2.5 (2.2) | 220 |
| WLQ c | ||||||
| Productivity loss score b | 5.9 (4.0) | 132 | 5.4 (3.9) | 87 | 5.7 (4.0) | 219 |
| Time demands b | 21.1 (20.6) | 132 | 20.8 (19.1) | 88 | 21.0 (20.0) | 220 |
| Physical demands b | 45.2 (38.0) | 132 | 35.2 (36.4) | 89 | 41.2 (37.6) | 221 |
| Mental/ interpersonal demands b | 17.5 (16.3) | 132 | 16.4 (15.4) | 88 | 17.1 (15.9) | 220 |
| Output demands b | 17.5 (19.4) | 132 | 17.1 (20.4) | 89 | 17.3 (19.7) | 221 |
Intervention effects on productivity
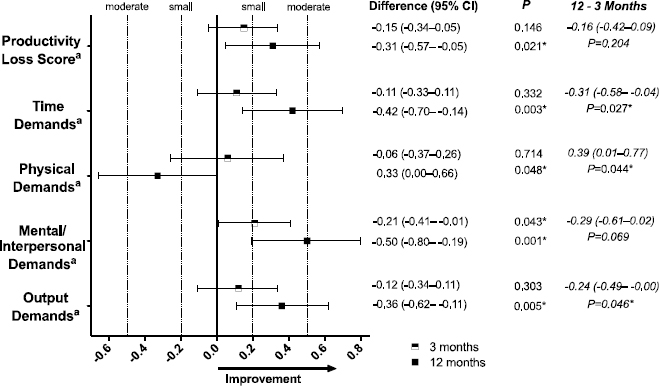
Evaluable case results from confounder-adjusted models are shown in the manuscript. Results in the manuscript are presented as effect sizes. Figure 1 displays intervention effects on HWQ outcomes. At 3 months, there was a non-significant trend towards small improvements in work satisfaction [effect size 0.27, 95% confidence interval (CI) -0.03–0.57, P=0.074] and stress (0.20, 95% CI -0.42–0.03, P= 0.084) while other intervention effects were very small and not statistically significant. At 12 months, there were small non-significant tendencies towards improved non-work satisfaction (0.31, 95% CI -0.00–0.63), stress (-0.26, 95% CI -0.56–0.04) and worsened impatience/irritability (0.28, 95% CI -0.04–0.60) with small or very small non-significant effects on the remaining outcomes. Figure 2 shows the results for the intervention effects on WLQ outcomes at 3 and 12 months. At 3 months, there was a small significant improvement in the mental demands subscale (-0.21, 95% CI -0.41– -0.01) and very small non-significant effects on the remaining outcomes. At 12 months, there was a small significant improvement in productivity loss score (-0.31, 95% CI -0.57– -0.05) and small to moderate significant improvements on every WLQ subscale except for the physical demands subscale, which worsened by a small degree (0.33, 95% CI 0.00–0.66). Results were largely unchanged when using multiple imputation (supplementary figure S2). Unadjusted results are shown in supplementary table S5.
Figure 1
Effect sizes for intervention impacts on the Health and Work Questionnaire (HWQ) at 3 and 12 months and 12–3 months, adjusted for baseline values and confounders. aIndicates a lower value is better (more favorable to productivity) for the difference score. * Signification intervention effect.
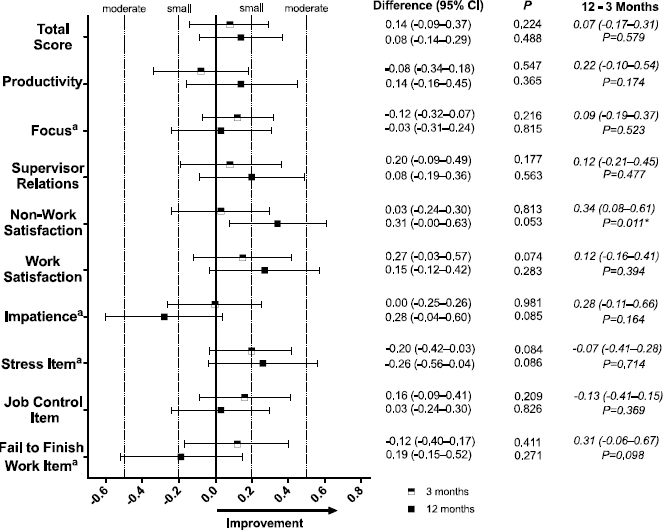
Figure 2
Effect sizes for intervention impacts on the Work Limitations Questionnaire (WLQ) at 3 and 12 months and 12–3 months, adjusted for baseline values and confounders. aIndicates a lower value is better (more favorable to productivity) for the difference score. * Signification intervention effect.
The significant intervention effects sometimes occurred via an improvement in the intervention group, a worsening in the control group, or both (supplementary table S6). Since productivity subscales were not designed with responsiveness to a sitting intervention in mind, some further descriptive information regarding the mean intervention group changes (net of control) in the individual items of the HWQ and WLQ (supplementary figures S3 and figure S4, respectively) is provided. More items tended towards improvement than worsening; however, the degree of change was not uniform, often even for items within the same subscale (except for the WLQ physical demands items and for the almost uniform lack of change in WLQ items at 3 months).
Comparison of longer-term and initial effects
Significant differences between intervention effects at 12 versus 3 months were seen in all of the WLQ outcomes except for the mental-interpersonal demands subscale (figure 2), for which there was a borderline difference (P=0.069) and for HWQ’s non-work satisfaction subscale only (0.34, 95% CI 0.08–0.61; P=0.011) but not the other HWQ outcomes (figure 1). The direction of these results consistently indicated at 12 relative to 3 months there was a stronger extent of improvement (or worsening in terms of the physical demands subscale).
Activity composition and changes in productivity
No significant associations were seen between changes in intervention recipients’ workplace activity and their changes in overall productivity as indicated by the HWQ total score and the WLQ productivity loss score (table 2). The effect sizes were consistently small or very small, and the direction of associations mostly indicated a slight tendency towards improvement when replacing sitting with standing and a slight tendency towards worsening when replacing sitting with stepping.
Table 2
Marginal mean changes in Health and Work Questionnaire (HWQ) total score and Work Limitations Questionnaire (WLQ) productivity loss score, predicted at specific changes in the composition of workplace time (sitting, standing, stepping)a [CI=confidence interval.]
| 3 months | 12 months | |||
|---|---|---|---|---|
|
|
|
|||
| HWQ Mean (95% CI) | WLQ b Mean (95% CI) | HWQ Mean (95% CI) | WLQ b Mean (95% CI) | |
| No change from baseline in mean sitting, standing, and stepping | 0.02 (-0.39–0.43) | -0.25 (-0.60–0.11) | -0.03 (-0.42–0.37) | -0.19 (-0.45–0.08) |
| Mean sitting -1h/8h at work, replaced with 100% standing | 0.13 (-0.14–0.38 +0.11 vs no change | -0.31 (-0.54– -0.08 -0.06 vs no change | 0.13 (-0.21–0.45 +0.16 vs no change | -0.27 (-0.46– -0.08) -0.08 vs no change |
| Mean sitting -1h/8h at work, replaced with 100% stepping | -0.11 (-0.98–0.77) -0.13 vs no change | -0.01 (-0.76–0.75) 0.24 vs no change | -0.19 (-1.05–0.66) -0.16 vs no change | -0.20 (-0.95–0.55) -0.01 vs no change |
| Omnibus test b | F[2]=0.308, P=0.546 c | F[2]=0.53, P=0.591 c | F[2]=1.71, P=0.188 c | F[2]=1.05, P=0.336 c |
Discussion
We have previously shown the Stand Up Victoria intervention resulted in significant reductions in workplace sitting time primarily by increasing standing (20). The present study examined the impact of the intervention on secondary outcomes pertaining to productivity, as captured by effect sizes for the HWQ and the WLQ. In general, we saw that the intervention initially (ie, at 3 months) had very limited impact on productivity; however, by 12 months, a larger and more diverse array of significant intervention effects were observed, nearly all of which were improvements. We further found 12-month effects were sometimes significantly enhanced relative to the 3-month effects. One adverse effect was seen: a small significant worsening in the WLQ physical demands subscale. While there was clear evidence the Stand Up Victoria intervention improved some facets of productivity in the longer-term, the manner in which it did so is unclear. There was no large or significant association between the extent of workplace activity changes that intervention participants made and their productivity gains. Possibly other elements of the participatory multi-component intervention were important in enhancing productivity.
Our significant improvements in productivity at 12 months broadly resembled improvements seen following a 12-month treadmill desk intervention (12) but somewhat diverged from some of the other free-living workplace sitting-reduction interventions, of which many studies have reported null findings (7, 13–16, 37–39). Since we saw differing results for productivity as measured by the HWQ and WLQ in our study, and differing results across productivity subscales, it is likely the mixed results in the literature and differences relative to our study may partly owe to differences in measurement tools and/or a non-uniform response across various facets of productivity. Studies have assessed productivity via different questionnaires (13, 16, 39), focus groups (14, 15), and objective productivity components (eg, words typed) (37, 38). Possible reasons for the tendency to see better effects with the WLQ is that it may have better validity relative to objective measures (27, 30) and better capacity to assess social aspects of productivity (19). The short (<12 month) timeframes of many studies, as noted in some reviews (17) may also have led to the tendency towards null results in the literature.
The adverse effect observed on the WLQ physical demands subscale warrants consideration. This subscale focuses on the extent that physical or emotional problems limit performance of work-related tasks such as walking, repeating motions, and using hand-held tools (including using a keyboard). The increase in standing associated with the intervention is a plausible explanation for the increase in the physical demands subscale measured at 12 months (32) although the physical demands subscale was not altered at 3 months when standing amounts were the greatest (20) and some studies report reduced musculoskeletal pain with sit-stand desks (7, 14). Instead, the finding may reflect adverse experiences we reported in our qualitative (40) and primary (20) evaluation, some of which were specific to the model of workstation used in Stand Up Victoria. Participants sometimes reported the platform of the workstations reduced their ability to use a computer mouse and perform other work tasks such as writing, while sometimes mentioning pain in the upper body or the lower limbs as a reason for discontinuing use of the workstation (20).
Mental health in the workplace is of increasing concern to employers in part because it can influence productivity (41). Traditional recommendations for improving mental health suggest performing moderate--to-vigorous-intensity physical activity (42) however, activity at such an intensity can be difficult to perform within the workplace. Evidence from a laboratory trial suggests breaking up sitting with standing reduces stress as indicated by lower cortisol levels (43), while participants in free-living interventions have also reported reduced stress symptoms (13). We observed small but significant benefits as represented by improvements in the mental/interpersonal demands subscale, and a small non-significant tendency towards improved experience of stress (as measured by a single item). The benefits to the mental/interpersonal demands subscale are consistent with focus group and interview findings of increased communication and improved team dynamics within the intervention group (40) and indicate the need for future research exploring the impact of workplace interventions on mental health.
Intervention recipients’ changes in workplace activity did not show any large or statistically significant associations with productivity changes. However, while the participants were clustered within geographically separate workplace environments, the study was conducted within a single government organization and productivity improvements were not observed within the control group (supplementary table S6). Thus, while not definitive, and subject to limitations such as measurement error, our findings suggest that productivity improvements were likely to have been due to some aspect of the intervention. The intervention involved elements including staff workshops, communication with supervisors, and individual coaching sessions. These elements were designed to be as participative as possible to encourage participants’ feelings of ownership of the program, and to include overt displays of organizational support for the program (23, 24). Many previous studies lacking these interactive sessions failed to observe changes to productivity (13–15, 37, 38), possibly highlighting the importance of this participatory approach for improving productivity. Furthermore, participants in the intervention were provided with a sit-stand workstation (and “satisfaction with the physical environment” was one of the highest-ranking individual-item improvements). These aspects of the intervention which sought to create a cultural and workplace-wide change may have been relevant for improving measures of productivity by improving employee workplace satisfaction and motivation but may also involve a learning curve similar to that observed with a treadmill desk intervention (12). At 3 months, intervention effects on productivity tended to be small and non-significant, but were significantly enhanced at 12 months. Although speculative, our findings suggest at least 3 months of the intervention may have been required to change behavior and/or the way participants’ work was done (ie, ≥3 months of learning, changing, adapting), and that in between 3 and 12 months those behaviors and changes were consolidated, became embedded and occurred consistently, thus resulting in significant productivity benefits by 12 months. Future research is needed to both replicate this finding and specifically investigate the mechanisms of change.
Our use of a cluster-RCT design to assess both short and longer-term impacts of a variety of facets of productivity in a behaviorally successful sitting-reduction intervention conducted in a free-living work environment was a key strength of the study. A further strength was the evaluation of the possible direct role of activity changes, using ActivPAL activity monitors which accurately measure sitting and standing amounts (the activities targeted by the intervention). There were limitations. Productivity was self-reported and determined from questionnaires that were designed to examine the impact of worker health on productivity rather than the impact of workplace interventions on productivity. The use of questionnaires rather than direct measures of productivity limits the ability to interpret the observed small-to-moderate improvements in productivity. Some aspects of the questionnaires (eg, ability to lift and carry objects) may have limited relevance to these desk-based workers’ job roles. The study was not powered a priori on the productivity outcomes, and appeared to have had limited power with respect to some 12-month outcomes. For the null results at 3 months, CI indicated only small or very small effects were likely, whereas greater effects were plausible for some of the 12-month effects and the 12 versus 3-month comparisons. The lack of power may have limited the detection of meaningful differences in these non-significant effects, especially in measures derived from the HWQ. Participants were also recruited from a single government organization; workers in other occupations may respond in a different manner.
In conclusion, in addition to reducing workplace sitting (20) and improving employee health in terms of selected biomarkers indicative of cardiometabolic risk (21), the Stand Up Victoria multicomponent workplace intervention also improved productivity. Improvements were small to moderate and mostly seen at 12 months, but seen overall and across multiple (but not all) facets of productivity. Additionally, changes in productivity were not related to changes in activity, suggesting other aspects of the intervention may have been relevant to improved productivity. Taken as a whole, our findings provide additional support for the feasibility and benefits of workplace interventions to reduce sitting and suggest the importance of including measures of productivity when evaluating the effectiveness of future interventions.
Conflict of interest statement
Stand up Victoria was funded by a National Health and Medical Research Council (NHMRC) of Australia project grant (#1002706), project funding from the Victorian Health Promotion Foundation’s Creating Healthy Workplaces program and, by the Victorian Government’s Operational Infrastructure Support Program. James Peterman was supported by an Australian Government Endeavour Fellowship. Genevieve Healy was supported by a NHMRC Career Development Fellowship (#1086029). Elisabeth Winkler was supported by a NHMRC Centre for Research Excellence Grant on Sitting Time and Chronic Disease Prevention – Measurement, Mechanisms and Interventions (#1057608), on which GNH, EGE, NO, and DWD are chief investigators. Marj Moodie was supported by a NHMRC Centre for Research Excellence in Obesity Policy and Food Systems (#1041020). Elizabeth Eakin was supported by a NHMRC Senior Research Fellowship (#511001). Neville Owen was supported by a Centre of Research Excellence (#1057608) and a Senior Principal Research Fellowship (#1118225) from the National Health and Medical Research Council of Australia, and by the Victorian Government’s Operational Infrastructure Support Program. David Dunstan was supported by an NHMRC Senior Research Fellowship (#1078360) and the Victorian Government’s Operational Infrastructure Support Program. Anthony LaMontagne was supported by Centre grant funding from the Victorian Health Promotion Foundation (#15732).
The authors acknowledge and thank all the participants of the Stand Up Victoria study, as well as other staff involved at the Australian Government’s Department of Human Services, particularly Tony Vane and Megan Evans. We wish to thank Parneet Sethi for her assistance with data processing, Dr Takemi Sugiyama for his contribution to questionnaire development, and the following project field staff: Glen Wiesner, Mary Sandilands, Kirsten Marks, Lisa Willenberg, Cameron Johnson, Bethany Howard, Stephanie Fletcher and Michael Wheeler. We also wish to acknowledge the assistance of the Department of Human Services liaison officers Sevasti Athiniotis and Valerie McRorie. The views expressed in this paper are those of the authors and not necessarily anyone in this acknowledgement list.
The study funders had no role in study design; collection, analysis, and interpretation of data; writing the report; or the decision to submit the report for publication. Trial registration: ACTRN1211000742976



