Most people will spend up to one-third of their adult life at work, thus workplace health promotion interventions are considered to have great potential for improving health. For instance, occupational organizational changes have been initiated to help increase smoking cessation, reduce alcohol consumption and introduce healthier diets (1). The increasing proportion of people working in sedentary jobs is a contributing factor to the cumulated insufficient physical activity in the general population during the past decades (2–4) and insufficient physical activity is now globally one of the main causes of increased mortality and reduced ability (5). Occupational sedentary behavior is suspected to be associated with health risks (6) and many workplaces have focus on counteracting sedentary behavior through workplace exercise interventions.
Mental health
Mental health problems among workers is another major challenge and impacts workers themselves, employers, and society through reduced work ability, increased sick leave, and higher risk of disability retirement (7, 8). Work-related stressors are listed as the main cause of stress in 70% of workers with self-reported stress in the Danish workforce (9) and, despite political and occupational interventions to reduce work-related stressors, statistics show that the problem is still increasing (9).
Workplace exercise interventions
The positive effects on health of regular exercise are well known, such as reducing the risk for obesity, cardiovascular diseases, diabetes, osteoporosis and some types of cancer (2, 10, 11). Regular exercise is also known to help prevent depression (12), reduce self-reported emotional stress (13–15), and improve quality of life and self-rated health (3, 10, 16).
Recently there has been an increasing number of studies examining the effects of workplace exercise interventions, showing that regular workplace exercise can reduce musculoskeletal complaints (17, 18), improve fitness, and reduce the risks of cardiovascular disease (19, 20). Effects on other parameters, such as mental health, quality of life, and the psychosocial work environment have also been suggested. For example, in their 2014 systematic review, Chu et al (21) evaluated the effects of work or home based exercise intervention on workers’ mental health. The evaluated outcomes included depressive, anxiety, and stress symptoms, where 2 out of 3 studies showed significant effect on depressive symptoms, 2 of 7 showed evidence of reducing anxiety symptoms, and 7 of 13 showed possible improvement of stress relieve. In a meta-analysis from 2009 (19), Conn et al evaluated the effects of workplace exercise interventions on different health parameters and found a positive association on quality of life and mood measurements, though not reaching statistical significance. More recently, Danish studies have indicated that work place exercise might influence workplace parameters such as work ability (22, 23) and sickness absence (22) as well as the psychosocial work environment, eg, social capital (24, 25). Other studies have shown uncertain effects of workplace exercise interventions (19, 26).
Thus, there might be a positive effect of workplace exercise intervention on both mental health as well as the psychosocial work environment.
Psychosocial work environment
Psychosocial work environment is a known predictor for common mental health problems (27), but a possible link between workplace exercise and how this impact the psychosocial work environment is not clear. Based on studies showing positive effects of workplace exercise on physical capacity, reduction of pain and employee wellbeing, one might hypothesize that this could lead to effects on factors impacting the psychosocial work environment. Furthermore, integration of exercise interventions will inevitably change the context and framework of a workday (eg, meeting colleagues and leaders in a different setting, changes in the distribution and organizing of employees’ work assignments and break schedules, changes in work-life-balance (as exercise during work hours may influence leisure time activities, etc.) which also might influence parameters of the psychosocial work environment.
One of the models to operationalize the psychosocial work environment is Karasek’s job-strain model (28), which points to the essential relationship between job demands and decision latitude. According to the job-strain model, the amount of work demands together with the amount of work control arbitrate the amount of psychological strain. The model was later expanded to include occupational social support (29), also known as the iso-strain model, as social support affects how demands and control at work are perceived. The authors of the present review acknowledge the definition of psychosocial work environment based on the iso-strain model. However, when measured as an outcome in research, the difference between psychosocial work environment and mental health parameters are not always clearly separated. Often, the fields seem to interconnect in the measurement tools used. For instance, measurement outcomes could be social capital, (including cooperation, trust, vitality), quality of life, job strain (including psychological demands, work load, levels of influence, effort‒reward balance), perceived job stress, vitality, fatigue, general wellbeing, burnout, as well as specific depression and anxiety scores.
As the two fields not always are clearly separated, we found it relevant to clarify a possible correlation between workplace exercise interventions to both mental health and psychosocial work environment.
We are not aware of any published reported or ongoing studies evaluating effects of workplace exercise on psychosocial work environment as well as mental health.
Objectives
The aim of this study was to evaluate peer-reviewed randomized controlled trials investigating the effects of workplace exercise on psychosocial working environment and mental health among employees. The study follows the PRISMA (Preferred Reporting Items for Systematic Review and Meta-Analysis) statement guideline for systematic reviews (30).
Methods
Eligiblity criteria
Study design, setting and language. The following inclusion criteria were used for this systematic review: (i) Peer-reviewed publication (in press or accepted for publication) reported in English; (ii) Study method consisting of a randomized controlled trial; (iii) Exercise intervention for employees occurring at the workplace or during working hours; (iv) Intervention conducted minimum on a weekly basis; (v) Outcome including ‘mental health’ and/or ‘psychosocial environment’.
As there are a great variety of different tools used to measure mental health and the psychosocial work environment ‒ and as many of the measured outcomes seem to overlap ‒ we found it necessary to use these broad outcome definitions. To ensure relevance of the studies included, each study’s outcomes were therefore specifically addressed, sorted, and organized after best relevance, based on the studies own categorization.
In our protocol, we initially chose an inclusion criterion of a minimum of 12 weeks intervention duration as we expected a great amount of studies eligible for review inclusion. After performing the initial study searches however, we chose to remove this criterion. We realized that, overall, there were not many studies meeting all inclusion criteria, meaning we could potentially miss relevant studies for our purpose.
Studies measuring workability, absenteeism, and sick leave without other psychosocial or mental health outcomes were not included. In order to assess current workplace and labor market conditions, we included original, peer-reviewed published articles in English from 1 January 1998 to 15 August 2018.
Information sources
The following electronic databases were searched for eligible published studies: Medline, Cochrane database, PsycINFO and Web of Science. The search ended on 15 August 2018. No new studies were included after this date.
Search strategy
The search terms included words related to the eligible criteria of setting, intervention, and outcome. Separate search strings were formed for each of the databases, taking into account their different frameworks (Table 1). The complete search strategy for all databases is available in the supplementary material (www.sjweh.fi/show_abstract.php?abstract_id=3832).
Table 1
Cochrane database. Results: N=204
Study selection
Selection process, and data management. Two researchers independently screened the papers identified in the listed databases on title and abstract level for possible eligible studies meeting inclusion criteria. Systematic reviews in the research field were also screened for eligible studies. The software program Endnote was used for sorting and duplicate removal. Eligible full-text articles were then read and evaluated for possible inclusion. Two researchers independently extracted data and assessed risk of bias. Any disagreements in the selection and extraction process was discussed between the two researchers until consensus was reached. When necessary a third researcher offered assistance in the evaluation process.
Data extraction
The following data were extracted from the studies: Country where the study was conducted, year of publication, population (type of workplace or job task, recruitment process, number of participants, inclusion health status), description of the intervention (type of training, duration, group- or individual-based), information of statistical comparison analyses, outcomes measured (including type and validation of surveys used for measurement), information on follow up measurements.
Risk of bias in individual studies
The Cochrane tool for assessing risk of bias from the Cochrane Handbook for Systematic Reviews of Interventions (31) was used to assess potential biases in the included studies. This assessment of bias includes potential biases of selection, performance, detection, attrition, reporting, and other sources from seven risks of bias domains (random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, as well as other potential threats to validity).
Quality assessment
Quality was evaluated using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach (32), which grades studies as followed: very low, low, moderate, high. The quality assessment was based on the findings in data extraction, and follows the domains of quality evaluation in the GRADE approach: risk of bias, inconsistency, indirectness and imprecision (figure 1).
Results
Study selection
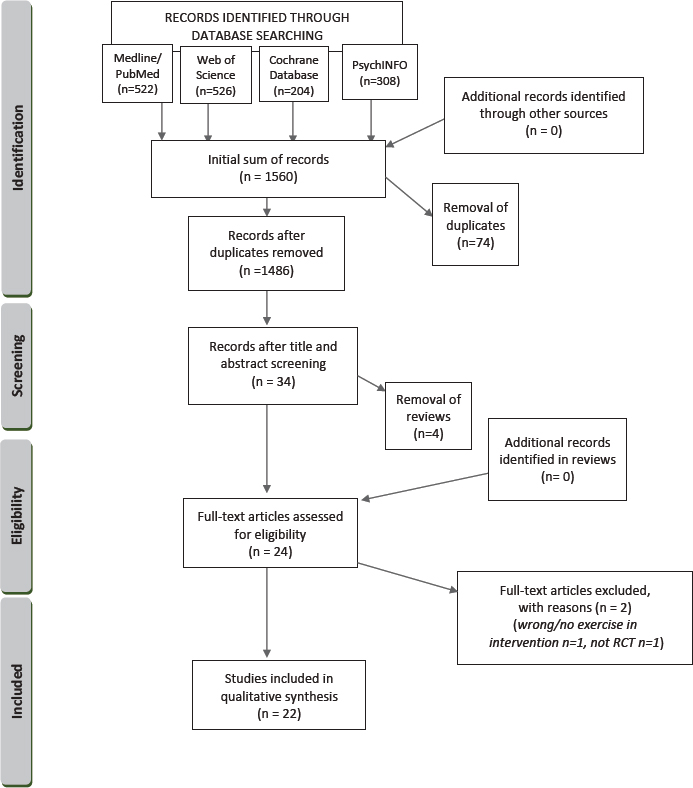
A total of 1560 records were identified by searching the databases PubMed, Web of Science, PsycINFO and the Cochrane database. After duplicate removal (N=74), review removal (N=4), and title abstract screening, 24 studies were evaluated for eligibility by full-text reading. The four reviews were screened for possible included eligible records, but no additional studies meeting the inclusion criteria of this review were identified. Two studies did not meet the inclusion criteria (one was not a randomized controlled trial and the other did not offer exercise as part of its intervention) and were excluded, leaving a final inclusion of 22 studies.
Study characteristics
The characteristics of the studies included are presented in Table 2. Most studies (N=17) (24, 25, 33–47) were conducted in Europe, the rest in North America (48, 49), Japan (50, 51), and Australia (52). The workplace settings varied from employees working in office/having administrative tasks (N=10) (34, 35, 37, 38, 41, 43, 47–49, 52), to health personnel in hospitals/nursing homes (N=5) (25, 33, 44, 46, 50), to laboratory technicians (N=2) (39, 42), to other manual job settings or workplaces with a mix of work tasks (N=5) (24, 36, 40, 45, 51). Sample size ranged from 24–860 participants, with a total of 4010 participants throughout the studies. The majority of studies (N=12) (25, 33, 34, 36, 38, 40, 42, 43, 46, 50–52) were based on healthy workers, three studies (24, 39, 48) examined workers with musculoskeletal problems, three studies (41, 45, 49) looked at sedentary/physical inactive workers, two studies (35, 47) included workers with light mental health complaints, one study (37) looked at workers with both mental and/or musculoskeletal complaints, and another (44) examined high aged workers. The exercise interventions consisted of a wide range of different exercises offered from 6–86 weeks (21 months), with most studies offering an intervention period ranging from 8–12 weeks (24, 25, 33–37, 39, 47, 48, 50–52) N=13. Interventions could be subdivided into cardio/aerobics (N=3) (35, 36, 46), strength/resistance (N=6) (24, 25, 33, 40, 42, 43), yoga (N=4) (37, 38, 48, 52), walks (N=2) (34, 45), web-based (N=1) (41) and mixed (N=6) (39, 44, 47, 49–51), though with wide individual differences between studies. Group training was most common with thirteen studies (24, 25, 33, 35-38, 40, 46, 48, 50–52) offering this, individual training occurred in two studies (41, 47), and a mix in seven (34, 39, 42–45, 49). Many studies were designed with an active reference group, offering an alternative exercise (24, 25, 33, 34, 36, 43, 49).
Only four studies (35, 38, 45, 47) had psychosocial outcomes as their primary outcomes. In ten (24, 25, 33, 34, 39, 41, 42, 46, 50, 52), it appeared as secondary outcome whereas it was one equal outcome among others in eight studies (36, 37, 40, 43, 44, 48, 49, 51). The same trial was used in two studies (25, 33) (intervention and study population) to conduct two different analyses with different outcome measures. Thirteen studies (34–39, 41, 43–45, 47, 49, 50) focused on mental health outcomes, while two (33, 42) focused on psychosocial environment, and seven (24, 25, 40, 46, 48, 51, 52) examined effects on both. All psychosocial outcomes were measured through self-reported questionnaires. Some questionnaires were recurring in the studies, the Copenhagen Psychosocial Questionnaire COPSOQ was seen in two (25, 42), the survey SF-36 was used in five, with focus on quality of life in three studies (40, 46, 52) and mental health in the two latter. Other measures reported revealed a great variety in types of questionnaires used in the different studies. Some mentioned questionnaires were: the Maslach Burnout Inventory–General Survey for burn out; 4DSQ for psychological complaints; the Demand/Control Model and the Job Affect Scale (JAS) for psychological demands; Profile of Mood States Bipolar (POMS-Bi); Inventory of Positive Psychological Attitudes (IPPA); PHQ-9; Center for Epidemiologic Studies Depression Scale (CES-D); Beck Depression Inventory-Second Edition (BDI-II) 9 for depressive symptoms; SF-8 for mental health; State-Trait Anxiety Inventory (STAI) for anxiety; Perceived Stress Survey (PSS) and Cohen’s perceived stress questionnaire for stress symptoms; PANAS-X and Warwick-Edinburgh Mental Well-Being Scale for mental/ psychological well-being; the Arthritis Self efficacy scale (ASES) for self-efficacy; the Work Extrinsic and Intrinsic Motivation Scale for work motivation; the Copenhagen Psychosocial Questionnaire (COPSOC) for psychosocial work environment; and the General Nordic Questionnaire for Psychological and Social Factors at Work for social capital.
Table 2
Summary of findings. [C=control; I=intervention; N/A=not available; NW=nature walk; UW=urban walk.]
Furthermore, many measurements were based on self-reported 5-point Likert scales rating of perceived subejctive symptoms as well as psychosocial work environment, developed for the studies.
All studies performed between group statistical analysis and included sufficient description of which methods were used in the study. Most studies measured outcomes two times: at baseline and at the end of the intervention period, a single study [Thøgersen et al (45)] measured continuously through mobile phones twice a week during the intervention period.
Quality assessment including risk of bias
The quality assessment of the included studies is presented in table 3. Risk of bias assessment was performed using the Cochrane Risk of Bias tool (31) and based on the evaluation the studies were graded into four categories: very high risk, high risk, moderate risk, low risk. Other parameters used to evaluate the quality of the studies were based on the GRADE approach (32) and included (i) description of statistics used for comparison, (ii) representative value of the included population, (iii) sample size, (iv) accessibility and transferability of the exercise intervention, (v) outcome comparison, (vi) outcome measurement validity, and transferability and (vii) presence of and duration of follow up
Table 3
Quality assessment. [C=control without intervention; C+I=control with other intervention.]
| Study | Risk of bias (4=very high 3=high 2=moderate 1=low) | Statistics a | Representative | Number of participants | Intervention | Comparison | Outcome | Extended follow-up >1 month | Quality of Evidence | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||||
| Population | Exclusion consequence b | Realistic | Easy integration | Common measure | Validated question-naire | |||||||
| Eriksen et al, 2002 | 2 | + | Healthy | Yes | >100 | Yes | Yes | C and C+I | Yes | Yes | Yes | Moderate |
| Van rhenen et al, 2005 | 4 | + | Specific | Yes | >100 | Yes | Yes | C | Yes | Yes | Yes | Very low |
| Sjögren et al, 2006 | 2 | + | Healthy | No | >100 | Yes | Yes | C | Yes | Yes | Yes | Moderate |
| Tveito et al, 2009 | 3 | + | Healthy | No | 31‒100 | Yes | Yes | C | Yes | Yes | Yes | Low |
| De zeeuw et al, 2010 | 2 | + | Specific | Yes | 31‒100 | Yes | Yes | C | Yes | Yes | No | Moderate |
| Hartfiel et al, 2011 | 3 | + | Healthy | Yes | <30 | Yes | Yes | C | Yes | Yes | No | Low |
| Hartfiel et al, 2012 | 3 | + | Specific | Yes | 31‒100 | Yes | Yes | C | Yes | Yes | No | Low |
| Mesquita et al, 2012 | 4 | + | Healthy | Yes | >100 | Yes | Yes | C c | Yes | Yes | No | Very low |
| Strijk et al, 2012 | 2 | + | Specific | No | >100 | No | No | C | Yes | Yes | No | Moderate |
| Cheema et al, 2013 | 2 | + | Healthy | Unclear | 31‒100 | Yes | Yes | C | Yes | Yes | No | Moderate |
| Roessler et al, 2013 | 2 | + | Healthy | No | >100 | Yes | Yes | C | Yes | Yes | No | Moderate |
| Brown et al, 2014 | 3 | + | Healthy | Yes | >100 | Yes | Yes | C d | Yes | Yes | No | Low |
| Andersen et al, 2015 | 2 | + | Healthy | Yes | >100 | Yes | Yes | C+I | No | Yes | No | Moderate |
| Jay et al, 2015 | 2 | + | Specific | Yes | >100 | Yes | Yes | C | Yes | Yes | No | Moderate |
| Thøgersen et al, 2015 | 4 | + | Specific | Yes | 31‒100 | Yes | Yes | C | No | No (mobile) | No | Low |
| Taylor et al, 2016 | 3 | + | Specific | No | >100 | Yes | Yes | C | Yes | Yes | No | Low |
| Andersen et al, 2017 | 2 | + | Specific | Yes | 31‒100 | Yes | Yes | C+I | Yes | Yes | No | Moderate |
| Chopp-hurley et al, 2017 | 3 | + | Specific | Unclear | <30 | Yes | Yes | C+I | No | Yes | No | Low |
| Jakobsen et al, 2017 | 2 | + | Healthy | Yes | 31‒100 | Yes | Yes | C+I | No | Yes | No | Moderate |
| Matsugaki et al, 2017 | 3 | + | Healthy | Unclear | <30 | Yes | Yes | C+I | Yes | Yes | No | Low |
| Michishita et al, 2017 | 3 | + | Healthy | Yes | 31‒100 | Yes | Yes | C | Yes | Yes | No | Low |
| Puig-ribera et al, 2017 | 2 | + | Specific | Yes | >100 | Yes | Yes | C | Yes | Yes | Yes | Moderate |
Risk of bias. No studies were graded as having low risk of bias, eleven (24, 25, 33, 35, 36, 39, 41–44, 52) met the criteria for having moderate risk, eight (34, 37, 38, 46, 48–51) were graded to have high risk, and three (40, 45, 47) were found to have a very high risk of bias. Blinding was declared not possible or not commented on in most studies, with the exception of two [Jay et al (39) and Puig-Ribera et al (41)] who reported to be single-blinded. All reported outcomes relevant for this review were collected with self-reported questionnaires and thus not blinded. There were great differences in drop-out ranges. Ten of the studies (24, 25, 33, 35, 36, 39, 42–44, 52) reported that intention-to-treat analyses were performed, leaving the remainder (N=12) (34, 37, 38, 40, 41, 45–51) with high risks of attrition biases.
-
(i) Statistics. A sufficient description of a relevant performed statistical analysis for comparison was delivered in all studies, with a large variety of methods observed.
-
(ii) Population. Generally, the participants represented highly selective groups of workers, as many studies investigated workers with specific issues (eg, neck and shoulder pain), and/or because participants were recruited through self-responsive invites where responsive rate was low, and/or many participants were excluded from the study due to health-related issues or other reasons.
-
(iii) Sample size. Ten of the studies (25, 33, 36, 39–42, 44, 47, 49) had a participant population >100, eight studies had 31–100 participants (24, 34, 37, 38, 43, 45, 46, 51), whereas three studies (35, 48, 50) were performed with very small sample sizes N<30.
-
(iv) Intervention design. Most studies presented exercise interventions that, from the descriptions in the study designs appearedeasy to implement and access at the work places
-
(v) Comparison. When presenting results, all studies included between-groups analyses, within-group analyses or subgroup analyses performed in many studies were not included in this review.
-
(vi) Measurement. Most measurement surveys were well-known validated questionnaires, however, studies also introduced uncommon and non-validated surveys. Use of single questions from domains was also seen in some studies.
-
(vii) Extended follow-up. Only four studies (36, 41, 43, 47) conducted extended follow-up measurements (ie, analyses a time period after intervention ended) with one year follow up being the longest duration of follow up.
The quality of evidence assessment revealed that twelve studies met the criteria for moderate quality, eight were rated with low quality and two very low quality of evidence. No studies met the criteria for high quality of evidence. Overall, positive effects on mental health and psychosocial work environment were typically found in only a single or a few parameters in the surveys used, the effects reported were found in different psychosocial parameters in the different studies, the reported effect sizes were found to be small. Six studies, Tveito et al (46), Hartfiel et al (38), Hartfiel et al 2012(37), Brown et al (34), Thøgersen et al (45), Chopp-Hurley et al (48), and Jakobsen et al (25), reported a beneficial effect on mental health after intervention. Brown et al (34) reported that the positive effect found probably was not valid due to low adherence. Two studies by Andersen et al (24, 33) reported positive effects on the psychosocial work environment “social capital” (33) and “social climate” and “vitality” (24), respectively. Two studies, Mesquita et al (40) and Michishita et al (51), reported positive effects on both mental health and psychosocial environmental outcomes on a variety of different parameters. However, these two studies were graded with “very low” and “low” quality of evidence, which should be taken into account when evaluating effects. A total number of eleven studies [Eriksen et al (36), Van Rhenen et al (47), Sjögren et al (43), De Zeeuw et al (35), Strijk et al (44), Cheema et al (52), Roessler et al (42), Jay et al (39), Taylor et al (49), Matsugaki et al (50) and Puig-Ribera et al (41)] reported no effects at all on psychosocial outcomes.
Discussion
Summary of evidence
The results of this review revealed that workplace exercise generally have limited positive effects on the psychosocial work environment and employers’ mental health. The majority of the included studies reported no or limited effects on a single or few parameters measured. None of the studies reported a negative effect on the psychosocial work environment. Thus, it is possible that exercise interventions may have effects on psychosocial parameters, both in mental health and psychosocial environment outcomes, however these effects seem to be small and dependent on the setting. The wide range of effects on different parameters probably reflects the great variety of design and methods of the studies.
Strengths and limitations
Value of results. To the best of our knowledge, this is the first study to review workplace exercise interventions and its effects on the psychosocial work environment as well as on mental health. By including a broad range of psychosocial outcomes, we are able to report a comprehensive evaluation of an emerging field of attention: workplace interventions to improve employers’ health. Thus, the results of this review might influence attitudes and actions for improving the work environment and potentially affect the overall working population. Workplaces today offer a great variety of types and integration of workplace intervention programs to improve health. Given the amount of time the working population spend at the worksite, workplace intervention programs are seen as possible efficient ways to enhance employees’ health (17). The results of this review indicate, however, that the effects of these programs on psychosocial parameters is limited. Nevertheless, workplace interventions are today acknowledged and encouraged by both governments and health organizations as a part of a general occupational health promotion (53–55), and workplace wellness, including fitness or other types of exercise at work, are commonly offered by employers (17, 56, 57).
Naturally, developing and implementing convenient programs and settings for exercise enhancement have concurrently been in focus, which was reflected in the studies of this review as most of the intervention designs chosen appeared to be easy to integrate and would transfer to other settings.
Strengths
This review included searches in many different academic databases, hereby reducing the risk of missing relevant studies for inclusion. We did not include grey literature or unpublished materials as we judged the academic literature to be the best source to answer our research question. It is possible that we have not included all trials in the area, but we do not think this influenced our conclusion. By following the PRISMA guidelines for systematic reviews, we ensured a systematic research process, which included a parallel independent screening, data extraction, and risk of bias assessment by two researchers, a method that reduces errors in the evaluation across studies.
Limitations
Still, the results of this review must be interpreted with caution and in accordance with its limitations. Of the 22 included studies, none were graded as having high quality evidence. A main reason for this is the weight of selection, performance, and detection bias (blinding) applied in the quality assessment method (Cochrane and GRADE). Blinding of participants in behavioral interventions is not possible, as participants are aware of what they are doing. Furthermore, psychosocial outcomes are difficult to measure without self-reported questionnaires. Still, we chose to evaluate studies with these risk of bias assessment tools as blinding increases credibility and validity of study results, and using the original, non-modified tool for risk of bias ensured transparency in our methods.
The inclusion of study results from the two studies graded as very low (40, 47) did not change the overall findings in this review.
Due to the great variety of study designs (population, types and duration of exercise interventions, tools used for self-reported measures of psychosocial outcomes), it is difficult to perform a synthesis across studies, which affects the possibility of drawing overall conclusions. The study populations were typically highly selected groups of participants, which lowers the external validity of the outcomes. Finally, we do not know if a longer period of intervention would have changed outcomes for some of the trials, but there was no consensus in positive results in the eight studies offering the intervention for >12 weeks.
Perspectives
Based on connections between physical and mental health, and mental health and the psychosocial work environment, we hypothesized that there might be positive effects of workplace exercise on psychosocial parameters. This was not supported in the results of this review. However, our findings can also illustrate the complexity in evaluating the wide range of workplace health promotion interventions offered, as physical and mental health at work might, as mentioned, be interconnected, and context-dependent local culture might affect outcome together with the different variables as type of workplace, population, setting, intervention, motives for implementation etc. Overall, the large heterogeneity of the studies strongly implies the need for more corresponding intervention designs and use of measurement tools in the future to enable better comparison.
Better methods for studying workplace interventions are desirable, but difficult as blinding is not possible. Some of the studies included in this review provided an option to blinding by offering two different interventions, where the participants are likely to believe that both may have benefits. This was done in the studies by Eriksen et al (36), Brown et al (34), Andersen et al (24, 33), Taylor et al (49), and Jakobsen et al (25), where there were active comparison groups. Examples of such were comparison of exercise at home versus work (25, 33), instructor- versus computer-based exercise (49), instructor-based exercise versus ergonomic instructions at work (24), and comparison of different types of exercises between intervention groups (34, 36). This procedure is likely to minimize the effects of placebo on the outcomes, as all groups receive an intervention that possibly may be beneficial. Another method used for implementation and evaluation of interventions which cannot be blinded is stepped wedged design (58). Here, cluster randomizing of teams or workplaces as a whole together with gradual offering of interventions to the included clusters enables comparison with the participants as their own controls. Thøgersen et al (45)conducts a small-scale similar method by using delayed start of intervention for their reference group.
Concluding remarks
Workplace exercise seem to have limited effects on mental health and the psychosocial work environment. The great variety across populations, types of interventions, and outcome measures in the included trials in this review hampers possibilities to draw conclusions across studies. Evaluating effects of behavioral workplace interventions is challenging due to difficulties with blinding and independent outcome measure. Alternative designs should be prioritized in the future.