Recent surveys have concluded that heavy occupational lifting is described as a risk for low-back pain (1), however heavy lifting also affects the cardiovascular system through acute increases in blood pressure (BP) (2). Some workers perform occupational lifting for several hours per day, many days per week, and therefore may be at risk for developing hypertension due to the frequency and duration of acutely increased BP (3). Thus heavy occupational lifting may act as an occupational risk factor for hypertension (4, 5). The prevalence of hypertension varies across occupational groups, supporting the impact by the working environment (6). Hypertension is a major preventable cardiovascular risk factor (7–9) and is estimated to cause 14% of all annual deaths globally (10). However, only few studies (4, 5, 11) have investigated the relation between heavy occupational lifting and hypertension, showing conflicting results. Thus, investigating these associations could reveal a potential for prevention of hypertension, especially among the 22% of the Danish workforce and 32% of European workers estimated to be exposed to heavy occupational lifting on a regular basis (12) (6th survey in Eurofound).
This study’s objective was to explore associations between heavy occupational lifting and hypertension in the Copenhagen City Heart Study, with the hypothesis that heavy occupational lifting is associated with a higher prevalence of hypertension and an increased incidence of new-onset hypertension in normotensives.
Methods
A detailed protocol for this study has been reported elsewhere (13). Briefly, randomly selected Copenhagen citizens, aged ≥20 years, were examined in the Copenhagen City Heart Study, containing person-based information on health as well as a large variety of biological, environmental and lifestyle-related factors (14). Data from the third (1991–94, response rate 61.2%), fourth (2001–03, response rate 49.5%) and fifth (2011–15, response rate 46.6%) examination were included in this study. Thus, the cross-sectional analysis had a possibility of three observations per participant, and the prospective analysis had possibility of two observations per participant.
Inclusion criteria
All participants with data on BP, level of occupational physical activity (OPA) (including heavy lifting) and use of anti-hypertensives were included in the cross-sectional analysis.
All normotensive participants with data on level of OPA at the third and/or fourth examination (n) and data on BP and use of anti-hypertensives in examination (n and n+1) were included in the prospective analysis.
Assessment of heavy lifting
Self-reported level of OPA was obtained by use of the same question in all three examinations: “Please describe your level of occupational physical activity within the past year” with the following response categories:” (i) predominantly sedentary; (ii) sitting or standing, some walking; (iii) walking, some handling of material; (iv) heavy manual work”. If answering iii or iv, an additional question regarding heavy occupational lifting was applied: “Do you lift heavy burdens?” with the response categories: yes or no. In the analysis, the participants were classified as exposed to heavy occupational lifting by answering “yes” to the question concerning heavy burdens, and those participants answering i, ii and iii or iv in combination with not lifting heavy burdens were set as the reference group.
No information was collected in between examinations. In the prospective analysis, the stability of exposure was accounted for by cross-tabulating the self-reported exposure at examination three by exposure at examination four, and also the self-reported exposure at examination four by exposure at examination five. An evaluation of the agreement (Cohen’s kappa) between exposures to heavy occupational lifting across the examinations showed fair agreement (13), and thus the baseline exposure were regarded as valid and used throughout.
Definition of hypertension
Hypertension, the primary outcome measure, was defined as reported use of anti-hypertensives or a measured systolic blood pressure (SBP) ≥140 mmHg or diastolic blood pressure (DBP) ≥90 mmHg (15) in the cross-sectional analysis. In the prospective analysis, hypertension was defined as the shift from from no use of anti-hypertensives in examination (n) to use of anti-hypertensives in examination (n+1) or an above median delta value of SBP [SBP in examination (n+1) – SBP in examination (n)]. Additionally, pulse pressure (PP) (PP = SBP – DBP), mean arterial pressure (MAP) (MAP = (2×DBP + SBP)/3)) and mid BP (½ SBP + ½ DBP) were investigated as secondary outcomes.
BP was measured according to the WHO guidelines recommended by Rose & Blackburn (16). Using a London School of Hygiene sphygmomanometer (17), BP was measured one time on the non-dominant arm after 5-minute sitting rest. The fall of the mercury column was set to 2 mm/s. The specially trained technicians were instructed in the same way, and all conditions during the measurements were identical at all examinations.
Assessment of covariates
A number of factors have previously been shown to be associated both with exposure to OPA, such as occupational lifting, and BP. Thus, the following factors were included as covariates: sex (male/female) (18); age (<40, 40–49, 50–59, 60–69, 70–79, >80 years) (19); body mass index (BMI) (<18.5, 18.5–24.9, 25.0–29.9, ≥30 kg/m2) (20) calculated from measured body height and weight; smoking (non-smoking; currently smoking) (21); length of education (no formal education; low educated up to 3 years; vocationally educated 1–3 years; higher educated; academically educated) (22); and, for the prospective analysis only, additional adjustment for vital exhaustion, split in four categories defined elsewhere (0, 1–4, 5–9, 10–17) (23); self-rated cardiorespiratory fitness (lower, similar, higher cardiorespiratory fitness compared to peers of same sex and age) (24); SBP at baseline (80–89, 90–99, 100–109, 110–119, 120–129, 130–139, ≥140 mmHg) (25), and DBP at baseline (40–49, 50–59, 60–69, 70–79, 80–89, ≥90 mmHg).
Statistical analyses
The primary null-hypothesis for the cross-sectional analysis was that heavy occupational lifting is not associated to hypertension, defined as using anti-hypertensives or having a measured SBP ≥140 mmHg or DBP ≥90 mmHg. In the prospective analysis, the primary null-hypothesis was that heavy occupational lifting at baseline does not increase the incidence of new-onset hypertension in normotensives.
The overall significance level was set at 0.05. However, Bonferroni corrections were applied meaning that the two primary hypotheses were tested at a significance level of 0.025 (13). The exploratory secondary analyses were not tested for statistical significance but reported by 95% confidence interval (CI).
Primary analyses
In the cross-sectional and prospective analyses, as a function of heavy occupational lifting, the odds of being hypertensive and becoming a SBP case, respectively, were estimated using logistic regression in a generalized estimating equation (GEE) model, with no exposure to heavy occupational lifting as reference. Observations from the same person were treated as repeated measurements. A first order autoregressive correlation structure was assumed. The cross-sectional analysis was controlled for sex, age, BMI, smoking and education. In addition, the prospective analysis was controlled for self-rated cardiorespiratory fitness, vital exhaustion, and BP at baseline.
Secondary analyses
Linear regressions. The associations between heavy occupational lifting and SBP, DBP, PP and MAP (mmHg) were investigated, first cross-sectionally and then prospectively (change in mmHg from examination n to examination n + 1), by use of linear regression models. These linear regressions were applied to both the entire included population as well as a population excluding those participants who reported to use anti-hypertensives.
Sensitivity to choice of comparison group. To investigate how sensitive the adjusted primary analyses were to the choice of comparison group, we performed an additional linear regression with SBP as outcome only. Here the comparison group was split into three different subgroups according to the self-reported categories of OPA, thus an exposure variable with four instead of two categories was created.
Sensitivity to the definition of hypertension. Due to the variety in cut-points for defining hypertension [SBP ≥160 mmHg or DBP ≥100 mmHg (14); SBP ≥180 mmHg or DBP ≥110 mmHg (15, 26) or SBP ≥130 mmHg or DBP ≥80 mmHg (25)], we investigated whether the OR for hypertension as a function of heavy occupational lifting was sensitive to the cut-point for defining hypertension. Thus, two additional cross-sectional logistic regression analyses were conducted using alternative cut-points: SBP ≥160 mmHg or DBP ≥100 mmHg and SBP ≥130 mmHg or DBP ≥80 mmHg.
Stratification by age. Due to the lack of occupational exposures as a result of old age pension (65 years) and/or early retirement (60 years) at the follow-up examination, analysis similar to the primary analysis stratified by age at baseline (≥ versus <50 years) were performed.
Results
From examination three, 5106 observations were excluded: 2717 from examination four and 1689 from examination five. Hence, 7052 and 4014 participants were included in the cross-sectional and prospective analyses, respectively (figure 1 and table 1).
Figure 1
Flow of the observations and participants in the third, fourth and fifth examination of the Copenhagen City Heart Study.
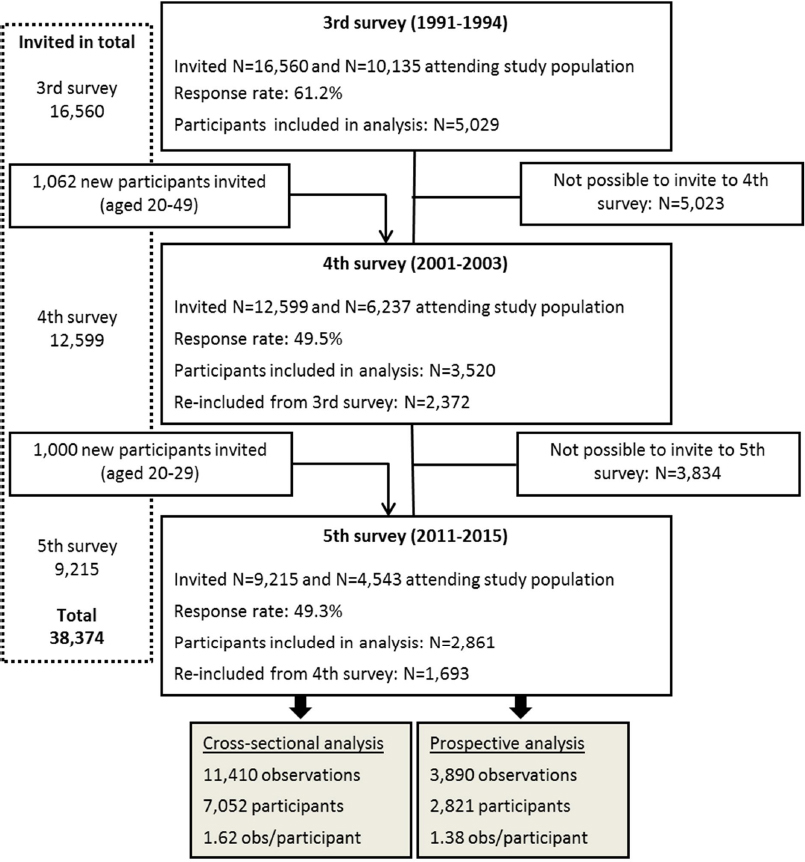
Table 1
Baseline characteristics of the included participants for the cross-sectional analysis; 11 410 observations on 7052 participants, and for the prospective analysis; 3890 observations on 2821 participants. [MVPA=moderate-to-vigorous physical activity; SD=standard deviation.]
Primary analysis
The crude primary cross-sectional analysis showed that those performing heavy occupational lifting had a 12% higher prevalence for hypertension than the non-exposed. However, when adjusting for relevant confounders, heavy occupational lifting did not affect the prevalence of hypertension (table 2). The prospective models did not show significantly increased risks for becoming a SBP or DBP case when exposed to heavy occupational lifting (table 2).
Table 2
Crude and adjusted odd ratios (OR) of prevalence of being hypertensive (in the cross-sectional model) and for becoming a systolic blood pressure (BP) case (in the prospective model) by self-rated exposure to heavy occupational lifting. No exposure to heavy occupational lifting was reference. All models include a repeated statement. [CI=confidence interval.]
| Heavy occupational lifting | Crude model | Adjusted model | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| N | OR | 95% CI | P-value | N | OR | 95% CI | P-value | |
| Cross-sectional hypertensive a | 11 410 | 1.12 | 1.01–1.24 | 0.04 | 11 039 | 1.06 | 0.94–1.20 | 0.34 |
| Prospective systolic case b | 3890 | 1.11 | 0.95–1.30 | 0.19 | 3668 | 1.10 | 0.92–1.31 | 0.29 |
| Prospective diastolic case b | 3890 | 1.11 | 0.95–1.31 | 0.18 | 3668 | 1.06 | 0.88–1.27 | 0.54 |
Secondary analyses
Linear regressions. Secondary analyses were performed by linear regressions to investigate the differences in SBP, DBP, PP, and MAP between participants exposed, or not, to heavy occupational lifting (13). The linear regressions relating heavy occupational lifting to BP showed no significant associations with any of the BP outcomes either in the cross-sectional or in the prospective analyses (supplementary material, www.sjweh.fi/show_abstract.php?abstract_id=3850, table S1). The linear regressions relating heavy occupational lifting to BP, stratified on use of anti-hypertensives, showed that, among participants not using anti-hypertensives, no significant associations between heavy occupational lifting and any of the BP outcomes neither cross-sectionally nor prospectively were seen (table 3). Also among users of anti-hypertensives no significant associations were seen cross-sectionally (table 3). However, positive associations between heavy occupational lifting and SBP and MAP were seen prospectively among users of anti-hypertensives (table 3).
Table 3
Adjusted associations between self-reported heavy occupational lifting and systolic blood pressure (BP) (mmHg), diastolic BP (mmHg), pulse pressure (mmHg) and mean arterial pressure (mmHg), stratified on use of anti-hypertensive. Occupational physical activity groups are clustered by answering “yes” or “no” to exposure to heavy occupational lifting; “yes” are in the heavy lifting category and “no” are divided in the other categories set by their self-reported level of occupational physical activity where the categories of walking, some handling of material AND heavy manual work, but no heavy lifting are collapsed. [CI=confidence interval.]
| Heavy occupational lifting | Cross-sectionala | Prospectiveb | ||
|---|---|---|---|---|
|
|
|
|||
| β (mmHg) | 95% CI | β (mmHg) | 95% CI | |
| NOT using anti-hypertensives | 9945 observations 6574 participants | 3589 observations 2752 participants | ||
| Systolic BP | 0.45 | -0.45–1.35 | -0.08 | -1.29–1.14 |
| Diastolic BP | 0.34 | -0.25–0.94 | -0.02 | -0.84–0.81 |
| Pulse pressure | 0.12 | -0.59–0.83 | 0.01 | -1.04–1.07 |
| Mean arterial pressure | 0.36 | -0.26–0.99 | -0.03 | -0.87–0.80 |
| USING anti-hypertensives | 1096 observations 967 participants | 84 observations 79 participants | ||
| Systolic BP | -1.98 | -5.22–1.26 | 15.91 | 5.30–26.52 |
| Diastolic BP | -0.38 | -2.43–1.67 | 4.02 | -2.21–10.27 |
| Pulse pressure | -1.59 | -4.44–1.27 | 7.87 | -0.06–15.80 |
| Mean arterial pressure | -0.94 | -3.05–1.18 | 7.46 | 0.67–14.24 |
Sensitivity to choice of comparison group
By stratifying the participants by their self-reported level of OPA the sensitivity to choice of comparison group of the secondary linear regression was tested. However, this analysis did not show any significant associations neither in the cross-sectional nor the prospective analysis (supplementary file, table S2).
Sensitivity to definition of hypertension
The sensitivity analyses applying cut-points for the definition of hypertension being higher (SBP ≥160 mmHg or DBP ≥100 mmHg) and lower (SBP ≥130 mmHg or DBP ≥80 mmHg) than the cut-point used in the primary analysis (SBP ≥140 mmHg or DBP ≥90 mmHg), showed that the OR for being hypertensive as a function of heavy occupational lifting was sensitive to the cut-points for definition of hypertension. By application of the higher cut-points, no relation between risk for hypertension and heavy occupational lifting was seen (OR 0.96, 95% CI 0.82–1.11), whereas the lower cut-points showed a tendency towards an increased OR for being hypertensive when exposed to heavy occupational lifting (OR 1.13, 95% CI 0.99–1.28).
Age stratified analysis
The cross-sectional and prospective analyses among both participants <50 and ≥50 years old showed that heavy occupational lifting did not affect the odds for being hypertensive or becoming a SBP or DBP case (table 4). However, a tendency of an increased risk for becoming a DBP case was seen among participants ≥50 years old.
Table 4
Adjusted odd ratios (OR) for being hypertensive, in the cross-sectional model, and for becoming a systolic blood pressure (BP) case, in the prospective model, stratified on age at baseline (≥ versus <50 years). No exposure to heavy occupational lifting was reference. All models include a repeated statement. [CI=confidence interval.]
| Heavy occupational lifting | Age ≥50 years | Age <50 years | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| N | OR | 95% CI | P-value | N | OR | 95% CI | P-value | |
| Cross-sectional hypertensive a | 5670 | 1.06 | 0.90–1.24 | 0.50 | 5371 | 1.09 | 0.90–1.32 | 0.36 |
| Prospective systolic case b | 1435 | 1.22 | 0.90–1.66 | 0.20 | 2233 | 1.03 | 0.83–1.30 | 0.77 |
| Prospective diastolic case b | 1435 | 1.30 | 0.97–1.73 | 0.08 | 2233 | 0.94 | 0.74–1.19 | 0.59 |
Discussion
This study aimed to investigate cross-sectional and prospective relations between heavy occupational lifting and hypertension. Neither the cross-sectional nor the prospective analysis could reject the primary null-hypothesis of no effect of heavy occupational lifting on the prevalence nor incidence of hypertension since non-significant increases in the prevalence and incidence of hypertension by 6% and 10%, were seen (table 2). The secondary analyses showed large rises in BP (ΔSBP 16 mmHg, 95% CI 5–27 mmHg, and ΔMAP 7 mmHg, 95% CI 1–14 mmHg, table 3) among participants using anti-hypertensives when exposed to heavy occupational lifting. Another sensitivity analysis indicated that participants aged ≥50 years were at 30% increased risk (OR 1.30, 95% CI 0.97–1.73) for becoming a DBP case when exposed to heavy occupational lifting. Further investigations of these associations are therefore warranted for prevention of hypertension, particularly across older workers and workers using anti-hypertensives.
These indications of increases in BP can be explained by the acutely increasing effect on BP from lifting, due to the acute increases in total peripheral resistance from the occlusion of vessels by the static muscle activity (2, 28). However, longitudinal studies show that leisure time resistance training lowers BP (29, 30), which may be explained by the physiologic adaptations in the cardiorespiratory system, taking place during restitution, leading to beneficial effects as increased cardiorespiratory fitness (28). Yet, the lack of these beneficial effects from OPA could be explained by the insufficient recovery due to the high frequency (5 days a week) and long duration (7–9 hours per day) (31, 32). Across some occupations, heavy occupational lifting is a part of OPA, and could therefore prospectively raise BP due to the high frequency and duration of lifting combined with an insufficient recovery (3). However, studies investigating the relation between heavy occupational lifting and BP are few and conflicting (4, 5, 33).
One major challenge in this research field is the healthy worker selection, described as workers migrating away from occupations with high OPA into more sedentary occupations (34). This selection could be based on symptoms of deteriorated health, eg, angina pectoris. Hypertension could be seen as non-symptomatic, however high SBP are thought to impact risk for angina (35). Future analysis should therefore investigate relations between heavy occupational lifting and risk factors for cardiovascular disease (CVD) by use of non-symptomatic outcomes or precursors of hypertension to bypass the healthy worker selection.
The secondary analyses revealed two sub-groups: users of anti-hypertensives and participants aged ≥50 years as being particularly vulnerable for exposure to heavy occupational lifting.
The prospective linear associations relating heavy occupational lifting to BP, stratified on use of anti-hypertensives, showed large rises in BP (ΔSBP 16 mmHg, 95% CI 5–27 mmHg, and ΔMAP 7 mmHg, 95% CI 1–14 mmHg, table 3) among users of these medications. Additionally, the 95% CI for the prospective linear relations between heavy occupational lifting and ΔDBP and ΔPP likewise indicated clinically relevant hazardous increases (25). These increases in BP may be explained by these participants being more susceptible to having a low compliance in the arteries due to decreased elasticity caused by the endothelia damage from the increased level of mean arterial pressure (36) initially causing the use of anti-hypertensives. Low arterial compliance decreases the ability of the arteries to dilate sufficiently when the blood are being pumped from the heart, this combined with occlusion of the vessels during static activities, such as lifting, will lead to major increases of the BP (28).
The estimated OR from the analysis stratified by age (</≥50 years) showed tendencies of stronger associations between heavy lifting and hypertension among participants aged ≥50 years (OR of becoming a SBP case of 1.22 and a DBP case of 1.30) compared to among participants aged <50 years (1.03 and 0.94) (table 4). This can be explained by the age and health-dependent decreases in aerobic capacity, leading to increased cardiorespiratory load from performing heavy occupational lifting (37). Also, the age-dependent loss of compliance in the arteries contributes to increases in BP due to the increased total peripheral resistance (28, 38).
The literature proposes differences in cut-points for being classified as hypertensive (15, 26, 27), and therefore two additional cut-points of hypertension [SBP ≥160 mmHg or DBP ≥100 mmHg (15, 26) and SBP ≥130 mmHg or DBP ≥80 mmHg (27)] were applied to the cross-sectional analyses. These sensitivity analyses showed that the OR for being hypertensive as a function of heavy occupational lifting seemed to be sensitive to the choice of cut-point; the cut-point of SBP ≥130 mmHg or DBP ≥80 mmHg yielded an OR of 1.13, whereas the cut-point of SBP ≥160 mmHg or DBP ≥100 mmHg yielded an OR of 0.96, and the cut-point of SBP ≥140 mmHg or DBP ≥90 mmHg yielded an OR of 1.06.
Taken together, this paper contributes to the knowledge of risk for hypertension from heavy occupational lifting and sheds light on the need for specific attention among those performing heavy occupational lifting while using anti-hypertensives (25). These results could therefore feed into prevention initiatives of hypertension specifically targeted workers exposed to heavy occupational lifting.
Methodological challenges
These analyses should be interpreted in light of the present limitations: the self-reported exposure to heavy occupational lifting and level of cardiorespiratory fitness might be affected by recall bias (39, 40); self-reported data are only collected from participants at the examinations, which could add a selection bias to the collected data. To collect exposures of heavy lifting independently of participation, future studies could consider receiving the exposure data from job exposure matrices, additionally could the recall bias be bypassed by use of technical measures of exposure to heavy occupational lifting. The collection of BP only in consultation during rest gives a lower prognostic value than obtained by monitoring of 24 hours BP or BP during sleep (41, 42); and the lowered odds for having prolonged working hours when exposed to heavy occupational lifting (33), which was not possible to adjust for in the present analysis due to the lacking information of amount of weekly working hours. Future studies investigating these relations could consider collecting the exposure information by use of a job exposure matrix or technical measures, not holding the limitations of being self-reported.
However, the analysis also holds some strengths; the follow-up time of 8–10 years and the determination of hypertension based both on use of prescription medicine and the resting BP in mmHg, limiting the risk of classifying participant as false negative. Also the randomly selected study population is a strength as well as the inclusion criteria of no use of anti-hypertensives, as these medications potentially may conceal, reverse or otherwise distort effects of heavy occupational lifting on BP. In line with this, participants diagnosed with hypertension at baseline were excluded from the prospective analysis because they were likely to receive anti-hypertensive medication in the in the time period between examinations. On the other hand, exclusion of those participants being diagnosed as hypertensive and/or using anti-hypertensives decreases variability of the analyzed population towards a more healthy population and thereby lacks the potential of investigating the effects of heavy occupational lifting among a population proposedly at higher risk for cardiovascular endpoints (31).
Implications of the results
Heavy lifting acutely increases BP (2). Approximately 22% of Danish workers and 32% of European workers are regularly exposed to heavy occupational lifting (12) (6th survey in Eurofound), and due to the frequency and duration of the occupational lifting, it is likely that increases in BP and hypertension will occur (3). Hypertension is a major risk factor for CVD and mortality (7, 8, 10). In spite of this, the Danish Working Environment Authority guideline for occupational lifting from 2005 (arbejdstilsynet.dk/da/regler/at-vejledninger/l/d-3-1-loft-traek-og-skub) only concerns risk factors for musculoskeletal disorders. Therefore we conducted this study to feed into the discussion on cardiovascular risk factors from heavy occupational lifting. This study finds that the prevalence and incidence of hypertension, to some extent, may increase by exposure to heavy occupational lifting. Although these OR are uncertain, the indications of rises in risk for hypertension up to 10% might still be of preventive importance for the general working population.
Secondly, the results showed that workers using anti-hypertensives would be expected to experience rises in SBP – from exposure to heavy occupational lifting – by 16 mmHg, which indicates a major increase in CVD risk (7, 9, 25). Also older workers (aged ≥50 years old at baseline) seemed to be more vulnerable to developing hypertension from exposure to heavy occupational lifting than younger workers (aged <50 years old at baseline). Hence, exposure to heavy occupational lifting could impact the workability as well as employability among workers aged ≥50 years old or those who use anti-hypertensives due to the fact that high SBP are thought to impact risk for angina (35), and thereby migration from occupations exposed to heavy occupational lifting to occupations with more light physical activity levels. Thus, it could be considered that tailoring the exposure to heavy occupational lifting to the age and general health of the worker would impact risk for hypertension and work sustainability beneficially.
These results suggest that the risk for hypertension might be lowered by reducing the exposure to heavy occupational lifting, especially among workers using anti-hypertensives and aged ≥50 years. These results are drawn among participants who showed up at examinations in a randomly selected adult Danish population and since the work environmental laws and regulations of occupational lifting are the same in the entire nation, we believe that the result of the study to some extent may be generalized to the entire Danish workforce. Yet, these conclusions are solely based on those who participated in examinations and, thus, a future investigation of this association might benefit from a study design not dependent on participation, such as a job exposure matrix. Nonetheless, knowledge is still needed to verify these findings and also to investigate the effect of accumulation of exposure from heavy occupational lifting on hypertension. Future studies investigating these relations could consider collecting the exposure information by use of job exposure matrices or technical measures, without the limitations of being self-reported.
Concluding remarks
No associations between heavy occupational lifting and prevalence and incidence of hypertension were seen among the general population. The secondary analyses showed positive associations between heavy occupational lifting and risk of hypertension among two vulnerable sub-groups, ie, (i) users of anti-hypertensives, and (ii) workers aged ≥50 years. Yet, these conclusions should be interpreted with the methodological limitations of this study in mind, and therefore further research is needed to confirm these associations.



