Psychosocial work stressors represent the objective characteristics of the work environment, including design, organization and context of work, which may elicit stress response in workers and cause physiological or psychological harm (1). Exposure to psychosocial work stressors have been associated with coronary heart disease (CHD), diabetes, clinical depression, as well as a range of other physical and mental health outcomes (2–18). Work stressors have also been associated with poor organizational outcomes, including sickness absence and presenteeism (19–21).
Research into the effect of psychosocial work stressors on mortality is sparse and has produced inconsistent results. Most studies thus far have examined components of the Karasek’s job-demand-control model, which is composed of the psychosocial factors job demands which refer to the pace and intensity of work, and job control comprising decision authority and skill discretion (22, 23). The model posits that job strain which results from the combined effects of low job control and high job demands may cause stress-related ill-health (23). The model was further extended to include an additional component representing social support in the workplace (24). Work stressors conceptualized and measured according to the job-demand-control-support model has been found to increase the risk of mortality in some studies (25–31), but not in others (32–43).
The concept of work stressors was broadened beyond proximal job task characteristics to include organizational factors in the effort-reward imbalance (ERI) model which recognizes both the effort and the reward structure of work (44). The model is based upon the premise that work-related benefits depend upon a reciprocal relationship between efforts and rewards at work and that lack of reciprocity due to an imbalance between high effort and low rewards is stressful to workers and may result in adverse health outcomes (44). Cohort studies examining the effect of high ERI on mortality have had mixed findings (28, 34, 39). A further work stressor model, the organizational justice model, which measures employees’ degree of perceived fairness of treatment in the workplace proposes that increased perceived unfairness may lead to increased stress responses, resulting in physiological and behavioral reactions adversely impacting on workers’ health and well-being (45, 46). The effect of increased perceived unfairness on mortality is not clear (47, 48). More recently, broader constructs of work stressors encompassing labor market arrangements including long working hours, shift work and job insecurity have been examined as risk factors for mortality with mixed results (11, 26, 36, 49–55).
Given these mixed findings and the fact that there have been no previous reviews of evidence about psychosocial work stressors and mortality, a comprehensive systematic review and meta analyses is needed to clarify the relationship. The objective of this study was to evaluate the evidence for the association between (i) psychosocial work stressors and all-cause mortality and (ii) psychosocial work stressors and mortality due to CHD. We included CHD mortality as a secondary outcome because the association with job stressors is biologically plausible, and it is one of the most frequently studied mortality outcomes (56).
Methods
A comprehensive systematic review of the available literature until the end of 2017 for studies providing information on the risk of mortality in relation to psychosocial work stressors was conducted as per the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines (57). A search strategy was formulated to identify studies systematically that answer the research question “What is the effect of psychosocial work stressors on mortality?”. The question was specified by defining the “PICOS’ modules as follows: Population (P) = workers; Intervention or exposure (I) = exposed to the psychosocial work stressors: low job control, high job demands, high job strain, low support at work, job insecurity, organization injustice, ERI, long working hours, shift work; Outcome (O) = total mortality, mortality due to cardiovascular heart disease; and Study type (S) = longitudinal studies.
Search strategy
A search of seven electronic databases covering a range of disciplines − including Medline, PubMed, EMBASE, Web of Science (medical science database), Scopus (social science database), PsycINFO (psychology database), and Global Health (public health database) − for eligible literature published from their respective commencement date to present was undertaken. A three-tier search strategy was used to identify eligible studies (see table 1 and supplementary material www.sjweh.fi/show_abstract.php?abstract_id=3854, table S1). The first and the second stages were combined with an “or” operator and matched with the third using the “and” operator. No restrictions were placed on the date, status, or language of publications. A secondary search included examination of the reference list of all studies identified for potential inclusion in the systematic review. The first author conducted the initial data searches and, together with the last author, independently screened all potentially relevant titles and abstracts to retrieve relevant articles to minimize the possibility of selective selection.
Table 1
Search terminology and strategy for systematic review.
Eligibility criteria
Original articles that had the key search terms in the title or abstract and mortality as an outcome variable were considered for inclusion in the systematic review. We excluded reviews, letters, editorials, case reports, book chapters, studies with no English translation, and conference abstracts. Studies investigating physical exposure to work-related factors including physical, chemical, ergonomic, and biological factors were excluded as the focus of the review is exposure to psychosocial work stressors in association with mortality. Studies examining deaths from karoshi, the Japenese term for death by overwork, were excluded from the review as karoshi conflates the exposure and outcome making it difficult to assign a common cause of death. Prospective population-level studies (cohort studies) and case control studies that contained quantitative estimates and 95% confidence intervals (CI) of the relative risk, rate ratio (RR), odds ratio (OR, or hazard ratio (HR) for mortality associated with psychosocial work stressors were included in the systematic review.
Studies were screened for eligibility using a two-stage process. Titles and abstracts of studies with the key search terms in the title or abstract, retrieved using the search strategy, were screened independently by the two review authors to identify studies that potentially met the inclusion criteria. Following review of the full text, studies that met the eligibility criteria were retained and any disagreements were resolved by consensus or through discussion with an independent researcher.
Data extraction
Methodological details and data including study description, author, cohort, year, country, population (sample size, gender, age), exposure assessment and exposure level, description of mortality (method of assessment and incidence), study design, duration of follow-up, number of events, confounders adjusted for in the analyses, effect size for mortality, and CI were extracted from each included study.
Quality assessment
The quality of studies was assessed by the same two independent researchers using the Scottish Intercollegiate Guidelines Network (SIGN) methodological checklist for cohort and case-control studies version 3 (58) (supplementart table S2). Studies with little or no risk of bias were rated as high quality. Studies that mostly agreed with the guidelines but containing some flaws with an associated risk of bias were rated as acceptable. Studies that did not agree with the criteria or contained significant flaws with respect to study design were rated as low quality. Disagreements over quality assessment were resolved by discussion, with involvement of a third independent researcher where necessary.
Data analysis
There was limited scope for quantitative synthesis because of the heterogeneity in exposures measured across a small number of studies. But where possible, we conducted quantitative analyses of studies with sufficiently similar exposures, outcomes and study populations. For multiple studies reporting on the same study data, only the most recent study with longer follow up period was included in the quantitative analysis. Multiple studies with the same author/s were included in the meta-analysis insofar as the study sample, exposures, or outcomes differed. Studies were included if age-adjusted effect estimates were available, otherwise we excluded studies with unadjusted crude measurements because age is such a strong predictor of mortality. OR, RR, and HR were combined to estimate pooled effect sizes (59).
We conducted inverse variance random-effects meta-analyses to assess the association between each psychosocial work stressor and the primary outcome: all-cause mortality; and the secondary outcome: deaths due to CHD, in minimally- and multivariable-adjusted analyses. Our analyses were restricted to combining estimates when more than two studies were available for pooling. For studies reporting multiple levels of an exposure (eg, job strain quartiles), the referent group was only included once in the meta-analyses. Hence highest job demands level was compared to lowest job demands level, job strain was compared to no job strain, and lowest job control level was compared to highest job control level. For studies reporting multiple categories of shift work (eg, evening shift work, night shift work, rotating shift work), the category with the highest frequency was compared to the referent category, no shift work.
In addition to the pooled effect size for individual psychosocial work stressors, we undertook separate subgroup random-effects meta-analyses for studies where effect estimates were stratified by gender. The I2 statistic was used to measure the heterogeneity between studies. Funnel plots were used to assess the precision of estimates and publication bias (60) and a modified Egger’s test was performed to test for small study effects by regressing effect estimates on their standard errors weighted by the reciprocal of the variance of intervention effect estimates (61).
Two sensitivity analyses were conducted. The first sensitivity analysis tested differences between studies without low quality assessment compared with the inclusion of all studies irrespective of quality assessment. The second sensitivity analysis tested differences between studies that assessed relatively healthy study samples (participants with pre-existing diseases and/or cancer other than melanoma were excluded from the study analysis or the study controlled for health status) compared with studies that did not exclude participants due to ill health from their analysis or control for health status.
All analyses were conducted using Stata 14.2 (Stata Corp, College Station, TX).
Results
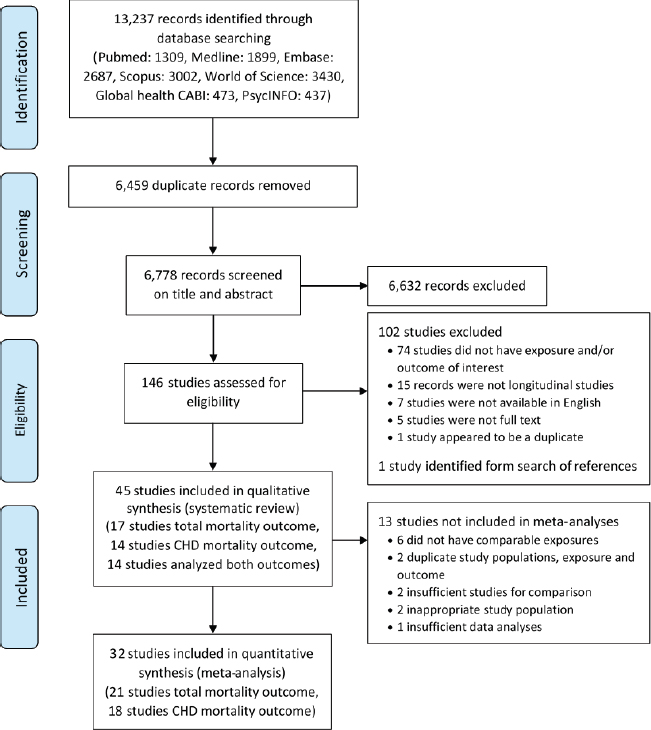
A total of 13 237 studies were initially identified (figure 1). After removing duplicates, 6778 records were screened by the title and abstract and 146 were further screened by full text for eligibility assessment and the reference lists were examined. 102 studies were excluded (supplementary table S3) resulting in 45 eligible studies for inclusion in the systematic review (11, 25–43, 47, 49–55, 62–78). Too few studies examined the risk of mortality and low social support at work, high ERI, or long working hours hence 32 studies were included in the quantitative analyses for low job control, high job demands, high job strain, shift work or job insecurity and mortality (11, 25–42, 50–54, 65, 66, 71–74, 76, 77).
Quality assessment
Twenty-seven studies were assessed to be of acceptable quality and eighteen studies were assessed as low quality (supplementary table S4). No study was judged to be of high quality.
Characteristics and results of reviewed studies
Twenty-seven studies were from Finland, Sweden and Denmark (11, 25, 28–30, 35, 37–39, 42, 43, 47, 50, 51, 53, 63, 64, 67–74, 76, 78). A further nine studies came from the USA (26, 27, 31, 32, 36, 41, 62, 65, 75), two studies from UK (54, 66) and Japan (40, 77), and one study each in Poland (34), Israel (33), France (49), Ireland (55), and Russia (52). The earliest study was published in 1981 (30) and the most recent published in 2017 (62, 74). The 45 articles included in the review used data from thirty-seven different studies. Four studies used data from the Valmet study (28, 39, 43, 47); and the Nurses’ Health Study (41, 75), Copenhagen Male Study (69, 70), Stockholm Heart Epidemiology Program (67, 68), Statistics Finland Quality of Work Life Surveys (50, 51), and UK industrial cohort (54, 66) data were used in two studies each (supplementary table S5).
The effect of psychosocial work stressors on mortality was based on males in thirteen studies (11, 25, 30, 42, 54, 64–66, 69, 70, 73, 76, 77), and females in five studies (27, 36, 41, 74, 75). Twenty-six studies examined psychosocial work stressors and mortality in all persons (26, 28, 29, 31–35, 37–40, 43, 47, 49–51, 53, 55, 62, 63, 67, 68, 71, 72, 78). Components of the main job-strain model used to measure work stress (22–24), including job demands, job control, job strain, support at work and/or iso-strain and the risk of mortality were investigated in twenty-seven studies (25–43, 49, 51, 62, 64, 65, 67, 71, 72). Eleven studies examined shift work and mortality (11, 50, 53, 54, 63, 66, 73–77), six studies looked at job insecurity and mortality (26, 36, 51, 52, 68, 78), three studies explored ERI and mortality (28, 34, 39), two studies included working hours and mortality (55, 69), one study inspected organizational justice and mortality (47), and another psychological pressure and mortality (70). Most studies used self-reported exposure measures, however five studies used a psychosocial job exposure matrix to assign job demands and job control values for each occupation (26, 27, 29, 42, 65), one study used both self-reported and occupation-based measures of work-related stress (38), four studies assessed shift work exposure from company records (54, 66, 73, 76), and one study used company records to assess employment status (78).
Median follow up in these studies ranged from 4–30 years. The outcome, all-cause mortality, was identified independently of the exposure from official national or regional death registers in almost all studies. One study did not report on outcome ascertainment (32), and three others relied on outcome status information provided from relatives and friends (26, 52, 62). Deaths due to CHD were ascertained from International Classifications of Diseases codes assigned for cardiovascular disease, ischemic heart disease, myocardial infarction and/or strokes on death certificates. Seventeen studies reported on specific working populations (industrial workers (28, 39, 43, 47, 54, 65, 66, 71, 73, 76), health professionals (36, 41, 74, 75), municipal and/or hospital employees (35, 72, 78)), two studies used non-fatal acute myocardial infarction cases (67, 68), and one study examined graduates from Wisconsin high schools in 1957 (62). The other twenty-five studies used a random working population sample drawn from the general population.
Various effect sizes were reported across studies. Thirty studies used HR (27, 28, 31, 33–39, 43, 47, 49–53, 55, 63, 67–75, 77, 78), nine studies used RR (11, 25, 29, 32, 40–42, 64, 65), four studies used OR (30, 54, 62, 66), and one study used standardized relative rates (76). The referent group for components of the job-strain model, job demands, job control and job strain differed across studies due to variation in exposure measurements and classifications between studies. Some studies reported results as continuous measures (31–33, 43, 62, 65) and various categorical measures were derived across studies. Different referent groups were used among studies with shift work exposure (supplementary table S6).
Quantitative analysis
Individual meta-analysis results for each of the five exposures, and risk of all-cause mortality and risk of CHD mortality are shown in supplementary figures S1–S17, and pooled results are depicted in figures 2–5. Pooled results for psychosocial work stressors and mortality in minimally adjusted analysis showed that employees in low control jobs had a significantly higher mortality risk than those in high control jobs (all-cause mortality: HR 1.21, 95% CI 1.07–1.37, k=3; CHD mortality: HR 1.50, 95% CI 1.42–1.58, k=5). The increased risk for low job control and mortality persisted in multivariable-adjusted analysis (all-cause mortality: HR 1.05, 95% CI 1.01–1.10, k=10; CHD mortality: HR 1.23, 95% CI 1.17–1.30, k=6), although risk estimates were attenuated.
Figure 2
Summary of pooled effect estimates for psychosocial work stressors and all-cause mortality minimally adjusted analysis.
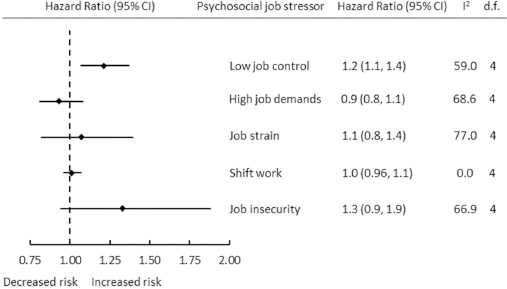
Figure 3
Summary of pooled effect estimates for psychosocial work stressors and CHD mortality minimally adjusted analysis.
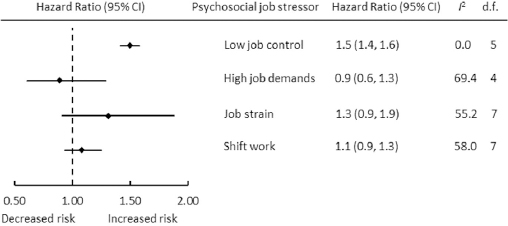
Figure 4
Summary of pooled effect estimates for psychosocial work stressors and all-cause mortality multivariable-adjusted analysis.
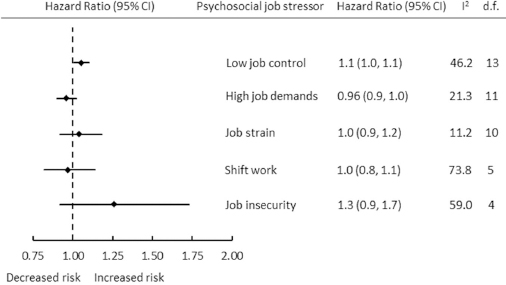
Figure 5
Summary of pooled effect estimates for psychosocial work stressors and CHD mortality multivariable-adjusted analysis.
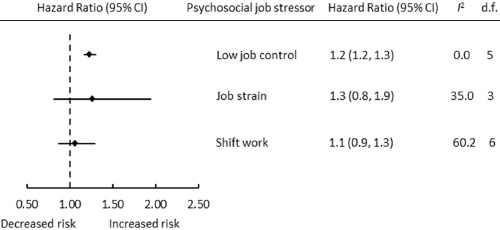
Pooled results for high job demands, job strain, and shift work were not associated with risk of all-cause mortality (HR 0.93, 95% CI 0.81–1.08, k=3; HR 1.07, 95% CI 0.82–1.39, k=3; and HR 1.01, 95% CI 0.96–1.07, k=5 respectively) or CHD mortality (HR 0.89, 95% CI 0.61–1.29, k=4; HR 1.31, 95% CI 0.91–1.88, k=7; and HR 1.08, 95% CI 0.94–1.25, k=7 respectively) in minimally adjusted analysis.
The pooled result for high job demands was not found to be associated with all-cause mortality in multivariable-adjusted analysis (HR 0.96, 95% CI 0.90–1.02, k=8) and differed little from pooled results for job demands and mortality in minimally adjusted analysis. Pooled results for job strain and risk of all-cause mortality (HR 1.04, 95% CI 0.92–1.18, k=7) and risk of CHD mortality (HR 1.26, 95% CI 0.82–1.94, k=4) included the null. An effect of shift work on all-cause mortality (HR 0.97, 95% CI 0.82–1.14, k=5) and CHD mortality (HR 1.06, 95% CI 0.87–1.29, k=6) was not observed, though the risk estimates were in opposite directions. Results for high job demands and CHD mortality were not able to be pooled due to insufficient number of studies available for analysis.
The pooled results for job insecurity and all-cause mortality were inconclusive (minimally adjusted analysis HR 1.33, 95% CI 0.94–1.88, k=3 and multivariable-adjusted analysis HR 1.26, 95% CI 0.92–1.73, k=3). Pooled estimates for job insecurity and CHD mortality were not able to be calculated due to insufficient number of individual studies.
Some heterogeneity was observed in studies pooled for examination of low job control and all-cause mortality (I2=59.0%, P=0.045), high job demands and mortality (all-cause mortality I2=68.6%, P=0.013; CHD mortality I2=69.4%, P=0.011), job strain and mortality (all-cause mortality I2=77.0%, p=0.002; CHD mortality I2=55.2%, P=0.029), shift work and CHD mortality (I2=58.0%, P=0.020), and job insecurity and all-cause mortality (I2=66.9%, P=0.017) in minimally adjusted analysis. Heterogeneity was also seen in studies pooled for analysis of shift work and mortality (all-cause mortality I2=73.8%, P=0.002; CHD mortality I2=60.2%, P=0.020), low job control and all-cause mortality (I2=46.2%, P=0.030), and job insecurity and all-cause mortality (I2=59.0%, P=0.045) in multivariable-adjusted analysis.
No heterogeneity was observed in studies pooled for analysis of low job control and CHD mortality (I2=0.0%, P=0.543) or shift work and all-cause mortality (I2=0.0%, P=0.707) in minimally adjusted analyses, or in studies pooled for analysis of low job control and mortality (CHD mortality I2=0.0%, P=0.983), high job demands and all-cause mortality (I2=21.3%, P=0.234), or job strain and mortality (all-cause mortality I2=11.2%, P=0.337; CHD mortality I2=35.0%, P=0.202) in multivariable-adjusted analysis.
Investigation of funnel plots (supplementary figures S18–S21) suggested some degree of asymmetry. Almost all studies had small standard errors and risk estimates ranging from under one to approximately two. The few studies with larger risk estimates approximating four had larger standard errors estimates possibly due to small study effects or methodological limitations. Due to the small number of studies included in the meta-analyses, it is difficult to reliably assess publication bias solely based on the funnel plots (79), hence formal testing for asymmetry was performed using Egger’s test (61). Formal statistical testing did not detect strong evidence of small study effects and risk of publication bias in the studies included in quantitative analyses, however there was some suggestion of small study effects for job insecurity and mortality (minimally adjusted analysis P=0.09 and multivariable-adjusted analysis P=0.08).
Sensitivity analyses excluding studies with low quality assessment resulted in attenuated pooled estimates and wider confidence intervals, probably due to validity issues with low quality studies. However, the association between exposure to low job control and mortality remained the same (minimally adjusted analysis: all-cause mortality HR 1.16, 95% CI 1.06–1.26, k=2; CHD mortality HR 1.36, 95% CI 1.19–1.56, k=4 and multivariable-adjusted analysis: all-cause mortality HR 1.03, 95% CI 1.00–1.06, k=5; and CHD mortality HR 1.19, 95% CI 1.01–1.40, k=4). As to be expected there was almost perfect overlap between studies with low quality assessment and studies that did not exclude or adjust for unhealthy participants at baseline, hence results of the sensitivity analyses examining differences between studies that assessed relatively healthy participants and studies that did not exclude unhealthy participants or control for health status were very similar to the aforementioned results.
Discussion
Main findings
This systematic review and meta-analysis examined the association between mortality and psychosocial work stressor exposures. Our findings show that workers with low job control have a 21% increased risk of all-cause mortality, and 50% increased risk of CHD mortality, compared with workers with high job control. Even after adjustment for relevant confounders in the multivariable-adjusted analysis, the increased risk of low job control and CHD mortality persisted as did the risk of all-cause mortality remain elevated, albeit attenuated, for workers with low job control. Excluding studies with low quality assessment attenuated the risk estimates but the association between low job control and mortality persisted. Low job control increased the risk of all-cause mortality by 3% and the risk of CHD mortality by 19% in the multivariable-adjusted analyses. A decreased risk of mortality for workers with exposure to high job demands was persistent across all subgroup analyses but was not statistically significant. Similarly, an elevated, but not significant, risk of mortality was observed for job strain and job insecurity. There did not appear to be any evidence supporting an association between exposure to shift work, and CHD mortality or all-cause mortality.
Comparison with other studies
This is the first review to synthesize systematically and quantitatively the respective epidemiological evidence for psychosocial work stressor exposures and CHD mortality or all-cause mortality. The observed association between low job control and increased all-cause mortality, in addition to CHD mortality, in minimally adjusted and multivariable-adjusted analyses strengthens the argument that job control is predictive of mortality. Many individual studies observe an elevated risk of mortality and low job control, but the association was not supported following adjustments for relevant covariates (28, 32, 35, 42, 65, 71, 72). However, these studies were generally small and underpowered to detect associations between mortality and job control, with most reporting less than several hundred deaths (28, 32, 42, 65, 71, 72), thus combining studies in a meta-analysis greatly increased the power to detect an association. A few studies detected decreased or no risk of mortality and low job control (31, 33, 38, 40). Variations in the underlying methodological design across studies, including differences in the measurement of the exposure and referent group, and assessment of potential confounders, may have contributed to inconsistent results.
Results for high job demands and mortality are consistent with results of individual studies. Most studies observed a reduced but non-significant risk of mortality and high job demands (26, 27, 33, 40, 51, 65), in contrast to Karasek (30) who found that high job demands increased the risk of CHD mortality. Self-reported assessments of job demands may not be a homogeneous measure across different occupations as job demands are experienced and interpreted differently across various occupational groups. There is a such a diversity of demands that responses might represent a range of job demands, such as psychological, physical, emotional, social, or organizational. It may also be that perceptions of job demands have changed over time. This along with inconsistent harmonization of scales across studies may explain the inconsistency in the literature.
Analyses of job strain and mortality were suggestive of a relationship between job strain and CHD mortality, but results were not conclusive. There is growing evidence that job strain and increased risk of mortality may be more pertinent in workers with existing cardiometabolic disease than for healthy workers. A study of patients with CHD based on three small prospective studies (67, 80, 81) reported a 60% increased risk of recurrent CHD events associated with job strain (82), and a more recent multicohort study examining work stress and mortality in workers with and without cardiometabolic disease reported a 70% increased risk of mortality in men with prevalent cardiometabolic disease (83). Analyses of job strain and CHD mortality were for healthy participants in all individual studies included in this review.
Results of the effects of shift work are consistent with the limited epidemiologic evidence that is available (12). Studies investigating shift work exposure can be prone to healthy shift work hire worker and healthy shift worker survivor selection bias due to unhealthy workers being less likely to take up shift work and healthier workers being more likely to remain in shift work employment compared to less healthy workers. This may explain the variation in mortality rates across studies. The evidence for job insecurity and mortality was inconclusive due to the small number of published studies available for inclusion in this review.
Biological plausibility
The observed associations are biologically plausible. Changes in brain stress-responsive neurocircuitry stimulate peripheral physiological responses in the sympathetic autonomic nervous system and hypothalamus–pituitary–adrenal (HPA) through the release and control of adrenaline and stress hormone cortisol throughout the body, and increase inflammatory protein levels despite the absence of pathogens (56). To cope with stress, the body’s systems adjust psychological and physiological processes, resulting in chronic over-activity or under-activity of allostatic systems, fixing new baselines levels for psychological and physiological performances, causing deterioration of body systems from repeated and unresolved stressors (84). The cardiovascular system is particularly affected by stress. Combined effects of dysfunction of both the autonomic nervous system and HPA-axis responses over time can result in increases in platelet activation, blood fibrinogen levels and blood pressure levels, accelerating the atherosclerotic process and increasing the likelihood of fatal and non-fatal cardiovascular or cerebrovascular events (56, 84).
Strengths and limitations of the study
The review has several strengths, including thorough systematic review conducted according to PRISMA guidelines (57) of 45 studies and the inclusion of 32 studies from Europe, United States, Israel, and Japan, most of which were assessed as acceptable quality. Sensitivity analyses attenuated results, but still excluded the null, with estimates remaining consistent even when omitting studies with low quality assessment or studies that did not exclude or adjust for unhealthy participants at baseline. Assessment of study quality was conducted using a rigorously validated scoring tool recognized as a useful assessment tool for assessing quality and susceptibility to bias in observational studies (58, 85).
There was some heterogeneity in pooled study results, ranging from 0–77% across the analyses, likely due to the variation in composition and classification of psychosocial work stressor exposures and referent groups between studies, and variation in composition of study sample (eg, general working population, specific industries, gender-specific), as well as due to variations in study period and geography. Furthermore, participants with previous history of CHD and/or cancer were excluded in some studies but not by others.
There is a concern about insufficient variance for psychosocial work stressor exposures when using generic work strain instruments in single occupation studies that may have biased our results towards the null. These generic measures although well-validated may not have measured psychosocial work stressors pertinent to some occupations, eg, healthcare workers’ exposure to violence. It should be also mentioned that the design of the review precluded assessment of the relation between single stressful occupations and mortality.
Nearly all studies measured exposure to psychosocial work stressors along with occupational, behavioral and/or biological risk factors at baseline and estimated their association with mortality during lengthy follow-up periods. Studies with single assessment of job characteristics and long follow-up periods without repeated assessment of exposure status over time measuring cumulative exposure, may bias results to null due to assessment of exposure to work stressors temporally distant from the outcome (86). Measurements of psychosocial work stressor exposures were self-reported in most individual studies and may have been subjected to reporting bias, however external measurements of work stress, like organizational downsizing, have been found to be associated with an increased risk of cardiovascular mortality (87). A few of the studies included in the review used occupation-based measures of psychosocial work stressors based on a job exposure matrix and may be susceptible to nondifferential exposure misclassification bias, biasing toward the null. In particular, job demands, a subjective measurement, may not be suitable for use in an exposure imputation system designed to measure environmental differences (30, 42, 65).
The individual studies had some degree of potential selection bias, including selective attrition due to cessation of employment as a result of job stressor exposure during the follow up period, and survivor bias (healthy worker effect) due to healthier participants being more willing to participate in health surveys, and less likely to be in low status jobs with high stress, that may have attenuated results. Of concern in shift work studies, the composition of the reference category may have influenced mortality risk estimates as healthier workers are more likely to take up shift work than less healthy workers and remain in shift work employment compared to those who develop debilitating conditions and depart shift work or retire from work altogether.
The lack of high-quality studies for inclusion in the meta-analyses is a limitation that may have potentially biased the results of our study towards the null. However, our analyses represent a summary of the existing knowledge. The fact that no high-quality study has been conducted is significant. More recent epidemiological methods including marginal structural methods and causal mediation analysis should be considered in future studies examining mortality outcomes in longitudinal studies with long periods of follow-up. It must be noted that this review’s narrow focus on psychosocial work stressors conceptualized from well-studied and validated work stress models is a limitation. Other conceptualizations of psychosocial work stressors for example burnout due to chronic exhaustion in combination with a negative attitude and diminished efficacy at work as a result of imbalance between job demands and resources (88, 89), and cognitive ergonomics such as the mental burden of specific tasks (90) and extra burdens created by time pressure and barriers hindering performance (91), were not included in this review. However, research into these work stressors and mortality is limited and their broad psychosocial framework may not be consistent with assumptions of homogeneity and variability between studies required for meta-analyses (92).
The outcomes, all-cause mortality and mortality due to CHD, were ascertained through record linkage and ICD codes for most studies included in the review following the assessment of exposure to psychosocial work stressors. Potential reverse causation due to confounding was considered by study authors, and controlled for in the analysis, or at the design stage of the study by the exclusion of participants at baseline based on health status. Despite the evidence for psychosocial work stressors and mental health disorders (10), suicide-related mortality was not included as a third outcome in this study, as several of the authors involved in this review had previously undertaken a comprehensive systematic review and meta-analysis of psychosocial job stressors and suicidality (93). The association between psychosocial work stressors and mortality may have been modified by gender, but we were unable to assess this effect moderation due to an insufficient number of studies presenting gender-stratified results. Nonetheless, we did provide pooled results by gender in supplementary figures S1–S17.
Concluding remarks
In conclusion, the results of the systematic review and meta-analyses suggest that workers with low job control are at increased risk of all-cause and CHD mortality compared to workers with high job control. Given the observed association between low job control and mortality along with the inconclusive findings for the other work stressors, further research is recommended to examine mechanisms underlying the observed effect between low job control and mortality and to elucidate the relationship between psychosocial work stressors and mortality. The strongest effect observed was that of deaths due to CHD and low job control, even after controlling for relevant confounders and the exclusion of low-quality studies. If the observed association is causal, then policy and practice interventions to improve job control could contribute to reductions in all-cause and CHD mortality.