Multimorbidity, the co-occurrence of ≥2 diseases, is highly prevalent among older adults (1). Multimorbidity is associated with high mortality, reduced functional status, and increased use of healthcare services (1). Due to the ageing population, increased survival rates, and the high prevalence of lifestyle-related risk factors (such as tobacco use, obesity and physical inactivity), multimorbidity rates are projected to increase in the coming years (1). Estimates of the prevalence of multimorbidity vary widely, depending on the types of diseases included, definition of multimorbidity, and population.
Most research on multimorbidity has been conducted on middle-aged and older adults in general population and primary care settings (2). In contrast, the multimorbidity of younger adults does not appear to have been a focus of research. However, younger adults, especially young working adults, are an important group from an economic perspective. With an aging population the dependency ratio increases, meaning that there are increasingly less workers for every non-worker in the general population. This is placing a greater burden on younger workers, in terms of both work participation and work productivity (3–5). Furthermore, early work behaviors can influence work behavior at an older age (6) and thus the impact of lost work productivity (ie, absenteeism and presenteeism) of young adults is likely to accumulate over time.
The extent of work productivity loss specifically in young workers is not well understood. Several health conditions – such as arthritis and other musculoskeletal disorders (7, 8), asthma (7), depression (7), chronic obstructive pulmonary disease (7), and multimorbidity (9) – are known to negatively impact work productivity. Previous studies have found that among young adults, spinal pain (6) and mental ill-health (10) negatively impact work productivity. However, the evidence regarding the influence of health conditions on the productivity of young working adults is limited (1, 11). Also, whilst evidence from older workers suggests clear sex and occupational group differences in both multimorbidity (12–14) and work productivity (15–17), sex and occupational class differences in multimorbidity and associated work productivity in young workers are not well evidenced. To our knowledge, there has not been an examination of overall multimorbidity and its relation with work productivity among young workers, nor have analyses stratified or adjusted by sex and occupational group been reported.
More information regarding the impact of multimorbidity on work productivity could lead to an improved understanding of the burden of multimorbidity among young workers and inform interventions targeted at young workers. Therefore, the aim of this study was to (i) determine the occurrence of both multimorbidity and work productivity loss among young adults with paid work and (ii) analyze the association of multimorbidity with work productivity.
Methods
Study design and participants
We conducted a longitudinal study utilizing data from the Raine Study (rainestudy.org.au). The Raine Study is an ongoing cohort established between 1989 and 1991 comprising women who attended antenatal clinics in Perth, Western Australia. From the 2900 women who enrolled in the study, 2868 offspring were included in the cohort (18). Our study was based on the children who participated in the Raine Study follow-up when they were 22 years of age, also known as Gen2-22. The results of our study were reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement guidelines (equator-network.org/reporting-guidelines/strobe). Ethics approval was obtained from the University of Western Australia, Princess Margaret Hospital and Curtin University human research ethics committees (HR84/2005, HR67/2013; RA/4/1/5202; RA/4/1/2646). The study was conducted in accordance with the Declaration of Helsinki. Informed consent was obtained from the participants.
Data collection
At the Gen2-22 follow-up, participants attended a clinic for a range of physical assessments and completed a broad ranging questionnaire, which included assessment of their medical history (19). Subsequently, quarterly questionnaires about work productivity were asked via text message and electronically distributed questionnaires over the following 12 months.
Health conditions and multimorbidity
Self-reported health conditions were assessed from three different parts of the questionnaire. First, participants were asked about the occurrence of any of the following 26 health professional diagnosed medical conditions or health problems relating to: acne; anxiety; arthritis or joints; asthma; attention; behavior; bladder control; chronic respiration or breathing (other than asthma); coordination; coeliac disease; depression; diabetes; eating disorder/weight; hay fever or some other allergy; hearing impairment or deafness; heart conditions; hemochromatosis (iron overload disease); intellectual disability; learning; menstruation; migraine or severe headache; sleep disturbance; speech and or language; thyroid gland; vision; and other medical conditions. Participants could answer “no”, “yes, in the past”, “yes, now”, or “yes, now and in the past”. If a participant chose one of the latter two options, the health condition was considered present. As cancer is usually listed in multi-morbidity studies, we examined all conditions reported by participants under other conditions and collated cancer reports as a separate condition.
Participants were asked separately if they had any food allergies (yes/no), restless legs (considered present with a positive answer on: “a strong urge to move the legs when sitting or lying down, accompanying dysesthesia, a relief by movement and a worsening of symptoms during the evening/night and had symptoms at least 5 times per month”) (19), sleep apnea (high risk of sleep apnea based on the Berlin questionnaire) (20), insomnia, and excessive sleepiness (moderate or severe sleepiness based on Epworth Sleepiness questionnaire) (21).
Additionally, several questions about musculoskeletal pain were included. Participants were asked whether their low back or neck/shoulders had been painful at any time in the last month (yes/no), and whether their low back or neck/shoulder pain ever lasted for >3 months continuously or on and off (yes/no). Chronic neck/shoulder pain and chronic back pain were operationalized as having the condition in the last month and it being chronic (continuously or on and off). Furthermore, participants were asked if they currently experienced any body pain in their right arm, left arm, right leg, left leg, upper back or somewhere else. Current other pain was operationalized as experiencing pain in any of these sites. Finally, the presence of obesity (body mass index ≥30kg/m2) was estimated from measuring body weight and height during physical assessments in a clinic.
In total, data on the presence of 36 health conditions were available. While there are no gold standard lists of conditions or groups of conditions, the conditions and groups used in the current study are similar to those commonly used in recent research on multimorbidity (22) and align to the International Classification of Diseases on condition categories of “diseases of the immune system”; “diseases of the musculoskeletal system or connective tissue”; “sleep-wake disorders”; “mental, behavioral or neurodevelopmental disorders”; “endocrine, nutritional or metabolic diseases”; “diseases of the circulatory system”; “diseases of the digestive system”; and “neoplasms”. Conditions from the ICD-11 categories “diseases of the visual system” and “diseases of the ear or mastoid process” were combined into a category based on sensory conditions. Disease counting is the most frequently used method to characterize multimorbidity, due to its ease of use. However, the longer the list of conditions, the greater the chance that participants have ≥2 conditions. Therefore, we also grouped all health conditions in the following ten categories: (i) allergies and respiratory, (ii) cancer, (iii) cardiovascular, (iv) gastrointestinal, (v) metabolic and endocrine, (vi) musculoskeletal, (vii) neurological, (viii) sensory, (ix) sleep, and (x) other medical conditions (see supplementary material, file 1 www.sjweh.fi/show_abstract.php?abstract_id=3858, for an overview of all conditions and condition categories). Multimorbidity was defined in the current paper as having ≥2 of these 10 condition categories.
Work productivity
The Health and Work Performance Questionnaire (HPQ) was used to measure total absenteeism, sickness absenteeism, and total presenteeism (22, 23). Participants were asked how many days they missed from work in general (total absenteeism), and due to health-related reasons (sickness absenteeism). No specific instructions were given to participants about reporting on pregnancy, so participants could have interpreted questions to include pregnancy-related leave as “health-related” or not. Presenteeism was estimated by asking participants to rate their overall job performance on the days worked in the past four weeks on a 0–10 scale (with 10 indicating no presenteeism). Validation studies show HPQ self-reports of absenteeism have good concordance with payroll records and that HPQ self-reports of presenteeism correlate well with work audits and ratings from peers and supervisors across a broad range of industries and occupations (24).
Additional variables
Sex of the participants was available from birth data. From the Gen2-22 follow-up, employment status (ie, being employed; yes/no), occupation (eg, manager, laborer – see table 1 for a full list of occupational groups), working hours per week, and after-tax weekly income were provided.
Table 1
Descriptives of work productivity, condition categories, multimorbidity and occupation. [IQR=interquartile range; SD=standard deviation.]
| Females (N=320) | Males (N=284) | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Mean (SD) | Median (IQR) | % | Mean (SD) | Median (IQR) | % | |
| Work productivitya | ||||||
| Total absenteeism (hours/year)b | 63.6 (108.1) | 24.0 (91.2) | 65.8 (145.6) | 0.0 (72.0) | ||
| Total sickness absenteeism (hours/year)c | 41.0 (74.5) | 12.38 (54.8) | 40.6 (112.0) | 0.0 (45.0) | ||
| Total presenteeism (hours/year)d | 111.2 (161.4) | 49.2 (173.7) | 90.6 (179.5) | 0.0 (115.2) | ||
| Total productivity loss (hours/year)e | 178.4 (246.7) | 82.8 (267.3) | 160.6 (300.4) | 0.0 (221.9) | ||
| Condition categories | ||||||
| Allergies and respiratory conditions | 35.9 | 28.5 | ||||
| Cancer | 0 | 0.4 | ||||
| Cardiovascular conditions | 1.3 | 0.7 | ||||
| Gastrointestinal conditions | 0.9 | 0 | ||||
| Mental and neurological conditions | 20.1 | 15.1 | ||||
| Metabolic and endocrine conditions | 19.1 | 12.0 | ||||
| Musculoskeletal conditions | 39.5 | 21.8 | ||||
| Other medical conditions | 40.9 | 18.0 | ||||
| Sensory conditions | 34.3 | 23.2 | ||||
| Sleep conditions | 28.4 | 22.9 | ||||
| Multimorbidity (number of condition categories) | ||||||
| 0 | 13.4 | 26.8 | ||||
| 1 | 23.1 | 31.7 | ||||
| 2 | 25.3 | 21.5 | ||||
| 3 | 20.9 | 14.4 | ||||
| 4 | 7.5 | 3.9 | ||||
| 5 | 5.9 | 1.4 | ||||
| 6 | 2.8 | 0.4 | ||||
| 7 | 0.9 | 0.0 | ||||
| Occupation | ||||||
| Managers | 3.5 | 3.9 | ||||
| Professionals | 17.0 | 12.3 | ||||
| Technicians and trades workers | 6.3 | 24.3 | ||||
| Community and personal service workers | 21.1 | 14.4 | ||||
| Clerical and administrative workers | 24.8 | 9.5 | ||||
| Sales workers | 20.8 | 15.1 | ||||
| Machinery operators and drivers | 0.9 | 5.2 | ||||
| Laborers | 5.7 | 15.1 | ||||
Data analysis
Total and sickness absenteeism (expressed in lost hours/in the last four weeks) was estimated from the four quarterly absenteeism measurements. To determine presenteeism, we first divided the self-reported hours worked over the past seven days by the number of days at work during those seven days to calculate the average hours per day that the participants were at work. Then, we took 10 minus the HPQ productivity rating, converted it to a percentage, and multiplied by the average hours per day that participants were at work to determine hours lost over the last four weeks. Quarterly time points of both absenteeism and presenteeism over the last four weeks were averaged for participants who presented data of ≥3 of the 4 quarterly work presenteeism assessments. An estimate per year was then calculated by multiplying average hours lost over the last four weeks by 12. The resulting annual estimates for absenteeism and presenteeism were based on 48 working weeks/year to account for the Australian standard of four weeks/year of annual leave.
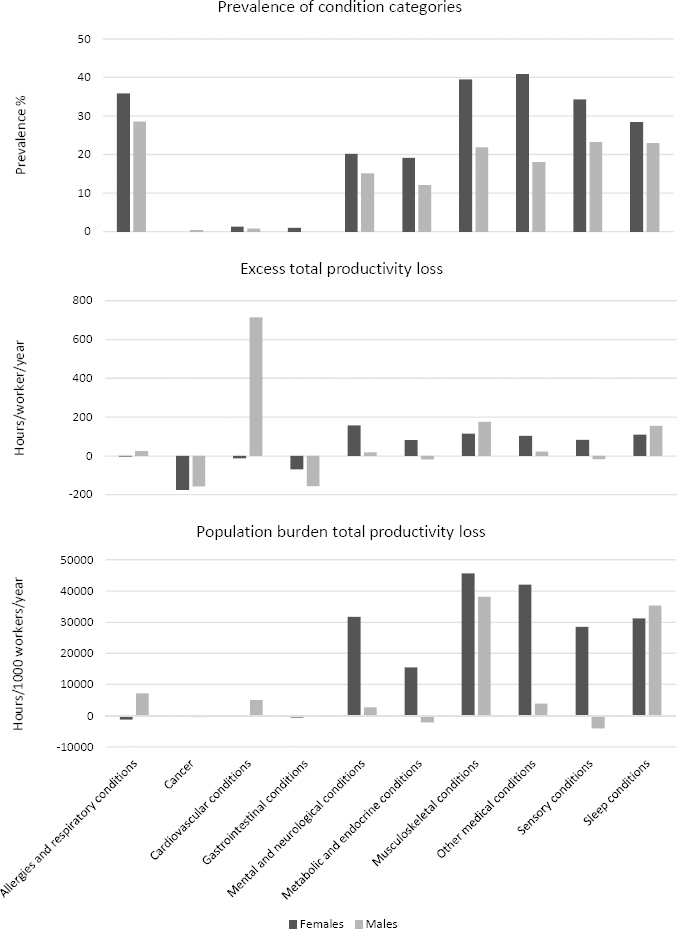
Descriptive statistics were used to present the prevalence of young workers (stratified by sex) reporting each condition category. To describe the contribution of having a specific condition category on an individual’s work productivity, the “excess” total productivity loss was calculated as the difference in total absenteeism and presenteeism hours/worker/year between individuals that were categorized in a certain condition category and those that were not. This excess thus represents the extra absenteeism/presenteeism that participants with ≥1 condition from a particular condition category have, as compared to those who do not have conditions from this category (but who may or may not have conditions from other categories). To describe the population burden associated with a specific condition category, the excess productivity loss was multiplied by the prevalence of each condition category (expressed as a percentage) to determine the population burden of total productivity loss, expressed in hours/1000 workers/year.
Regression analyses were conducted to assess the association of multimorbidity and work productivity during early adulthood. Due to the count nature of the work productivity measures and the potential for high prevalence of no productivity loss, we used zero-inflated negative binominal (ZINB) regression (25, 26), as has been used previously for work productivity loss data (27). This method allows for modelling of participants with a high propensity to have zero hours of productivity loss (the zero-inflated part of the model) and participants with substantial probability of at least one hour of productivity loss (the count part of the model).
The count of condition categories was treated as a continuous independent variable. Sensitivity analyses were conducted using a categorical variable based on the number of condition categories (0, 1, 2, 3, 4 or ≥5) and using the number of conditions, which led to similar results (data not reported). Total absenteeism, rather than sickness absenteeism, was used as the dependent variable because workers might not be able to well discriminate health-related from non-health-related absenteeism and some workers use absenteeism other than sickness absenteeism to manage health issues (24). Incidence rate ratios (IRR) with 95% confidence intervals (CI) were estimated from crude models, stratified by sex, and models in which we also adjusted for occupation. P<0.05 was considered statistically significant and all statistical procedures were performed using Stata version 13 (StataCorp, College Station, TX, USA). In the zero-inflated part, only variables that contributed to the model in a statistically significant manner (with P<0.05) and the constant term were maintained. The likelihood-ratio test of alpha was used to establish the added value of the ZINB models above zero-inflated Poisson (ZIP) modelling, which would be the case if the 95% CI of the alpha term does not overlap 0. Also, models were checked for any undue influence of outliers.
Results
Sample
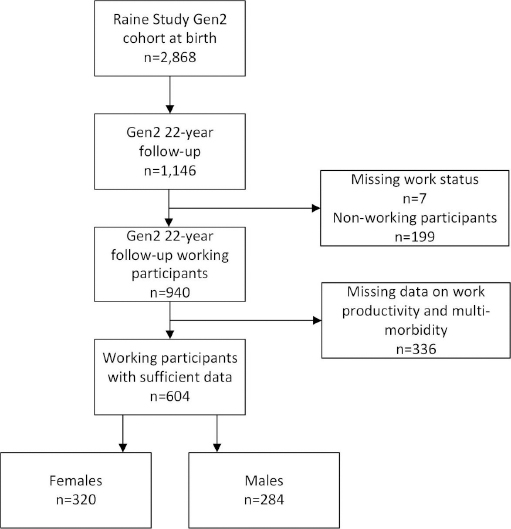
Of the 1146 participants in the Raine Study Gen2-22 follow-up, 940 were employed and 604 provided sufficient data on their work productivity (figure 1). Characteristics of these 604 participants, consisting of 320 females and 284 males, are provided in table 1.
Work productivity
On average, participants reported 64.7 [standard deviation (SD)127.0] absenteeism hours/worker/year, of which 40.8 (SD 93.9) were sickness absenteeism hours. Furthermore, participants reported on average 101.6 (SD 170.3) presenteeism hours/worker/year. Total productivity loss (absenteeism and presenteeism) was 170.1 (SD 273.0) hours/worker/year. Males reported slightly more absenteeism hours/worker/year compared to females [65.8 (SD 145.6) versus 63.6 (SD 108.1)], whereas females reported more presenteeism hours/worker/year compared to males [111.2 (SD 161.4) versus 90.6 (SD 90.6)].
Health conditions, categories and multimorbidity
The prevalence of condition categories for the total sample, and stratified by sex, is presented in table 1. The most common condition categories were allergies and respiratory (32.5%), musculoskeletal (31.2%), other medical (30.1%), sensory (29.1%), and sleep (25.8%) conditions. In the supplementary file 1, the prevalence of individual conditions is described. We observed substantial differences in condition categories and individual conditions between females and males (figure 2). For females, the condition categories with the highest prevalence were other medical (40.9%), musculoskeletal (39.5%), allergies and respiratory (35.9%), sensory (34.3%), and sleep (28.4%) conditions. For males, the condition categories with the highest prevalence were allergies and respiratory (28.5%), sensory (23.2%), sleep (22.9%), and musculoskeletal (21.8%) conditions. The prevalence of multimorbidity (ie, having diseases from ≥2 disease categories) was 53.1% for the total population, 63.5% for females and 41.5% for males (table 1 and supplementary file 2).
Health conditions and productivity loss
In figure 2 and supplementary file 3, the prevalence, excess total productivity loss, and population burden of total productivity loss are shown. While the conditions with the highest prevalence were allergies and respiratory, musculoskeletal, other medical, sensory, and sleep conditions, the disorders with the highest excess in total productivity loss were cardiovascular (232.9 hours/year), musculoskeletal (137.1 hours/year), sleep (130.0 hours/year), mental and neurological (88.1 hours/year), and other medical (74.9 hours/year) conditions.
The population burden of total productivity loss, based on the product of both excess productivity loss and the prevalence of the condition category, was highest for musculoskeletal (42 444 hours/1000 workers/year), sleep (33 581 hours/1000 workers/year), other medical (22 519 hours/1000 workers/year), and mental and neurological (15 650 hours/1000 workers/year) conditions.
For several condition categories, a higher population burden of total productivity loss was found for females compared to males, such as other medical (41 963 versus 3834 hours/1000 workers/year), mental and neurological (31 645 versus 2578 hours/1000 workers/year), sensory (28 494 versus -4148 hours/1000 workers/year), and metabolic and endocrine (15 495 versus 5028 hours/1000 workers/year) conditions (figure 2 and supplementary file 3).
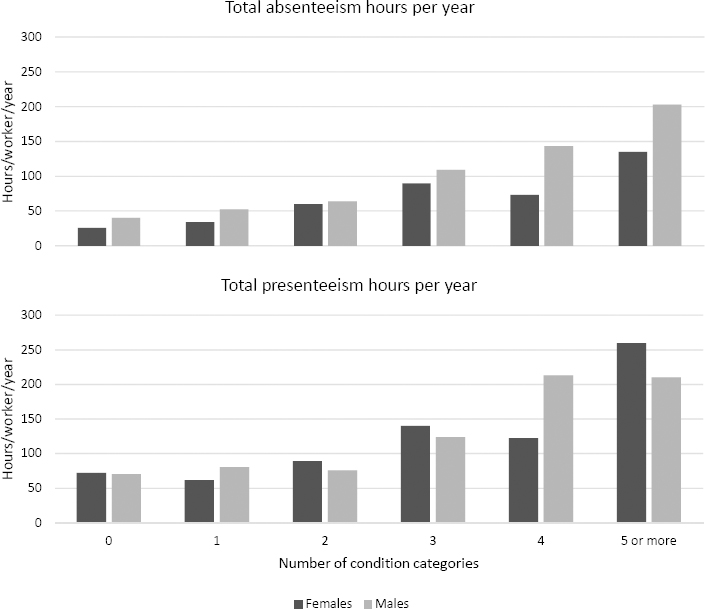
Association between multimorbidity and productivity loss
Figure 3 shows a gradual increase in total absenteeism and total presenteeism as the number of condition categories increased. In table 2, the association between condition categories and work productivity loss from the ZINB models are shown, stratified by sex. Model characteristics are provided in supplementary file 4. Females reported statistically significant higher total absenteeism as the number of condition categories increased (IRR 1.13, 95% CI 1.04–1.24), meaning a 13% increase in days of total absenteeism with each increase of one condition category. Similar results were found for sickness absenteeism (IRR 1.10, 95% CI 1.02–1.19) and total presenteeism (IRR 1.14, 95% CI 1.05–1.22). Adjusting for occupation, results were similar (IRR 1.13, 95% CI 1.04–1.23; 1.09, 95% CI 1.01–1.18; 1.12, 95% CI 1.04–1.20, respectively). Males also reported statistically significant higher total absenteeism as the number of condition categories increased (IRR 1.20, 95% CI 1.05–1.36), meaning a 20% increase in days of total absenteeism with each increase of one condition category. Comparable results were found for sickness absenteeism (IRR 1.15, 95% CI 1.01–1.32) and total presenteeism (IRR 1.13, 95% CI 1.01–1.26), and after adjustment for occupation (IRR 1.18, 95% CI 1.04–1.35; IRR 1.15, 95% CI 1.01–1.32; and 1.16 95% CI 1.04–1.30, respectively).
Table 2
Associations between the count of condition categories (continuous variable) and work productivity loss. [SD=standard deviation; IRR=incidence rate ratio; CI=confidence interval.]
Discussion
We aimed to (i) determine the extent of both multimorbidity and work productivity loss among young adults and (ii) analyze the association of multimorbidity with work productivity among young adults. Our findings indicate that multiple health conditions are already prevalent among working young adults (53.1%). While more than half of the population experienced multimorbidity, prevalence of multimorbidity was substantially higher among females compared to males. We found significant associations between the number of health condition categories and work productivity loss in both males and females. Of these categories, the highest population burden of productivity loss was found for musculoskeletal, sleep, other medical, and mental and neurological conditions.
Interpretation of results
A systematic review on the prevalence of multimorbidity found general population estimates ranging from almost non-existent up to almost 100% (2). These large differences were noted to be influenced by worker’s age and variations in methods, for example the number of reported conditions, and whether data were self-reported, retrieved from databases, or collected during a medical examination (2), which is a limitation for comparison of studies. Our study found higher rates than the only prior study reported on multimorbidity in the general population around 22 years of age, which reported a rate close to zero (28). However that study only asked about seven conditions (arthritis or rheumatism, cancer, diabetes, hypertension, cardiovascular diseases, chronic obstructive pulmonary diseases, and mental disorders), meaning the chance of having ≥2 from this more limited list was less. Although a review by Fortin et al (2) reported multimorbidity rates were low among workers in their 20s and increased substantially from 55–70 years of age, these models were based on few data from early adulthood. The rate found in our study was higher but is consistent with a high prevalence in young adulthood of several conditions such as for spinal pain (29), depression (17), and sleep problems (30).
Furthermore, we found that the condition categories with the highest prevalence – such as allergies and respiratory conditions – or those with the highest impact on individual productivity loss, such as cardiovascular problems, were not necessarily conditions with the highest population burden of work productivity loss. Musculoskeletal, sleep, other medical, and mental and neurological conditions had the greatest societal burden because of their relatively high prevalence and their high impact on work productivity loss. These major burden categories differ from those found in older workers (31) and the general population (32). Therefore, particular attention should be paid to conditions within these categories in young adults.
The clear pattern we identified, indicating greater work productivity loss with a greater number of condition categories, is consistent with other studies of middle-aged and older workers (9, 31, 33, 34), suggesting that the impact of multimorbidity on work productivity needs to be a matter for priority consideration of young and not just older workers. This could be done through interventions, such as those making adjustments to the workplace or job content and those targeted at the individual worker improving the worker’s capacity and work ability and/or reducing the (mental or physical) workload. Such interventions have previously been targeted at older workers (35, 36) and need to be reconsidered to also target younger workers.
The relatively steady pattern for increasing work productivity loss with a greater number of conditions, as shown in figure 3, suggests a partially additive, rather than multiplicative effect. For example, the productivity loss associated with having conditions in four categories was double that associated with two categories. The synergistic effects of various combinations of conditions are likely to vary from amplifying the effect of individual conditions to ameliorating the effect. For example, having a mental health condition may increase the productivity loss associated with having a musculoskeletal condition, whereas having a cardiovascular condition in addition to a musculoskeletal condition may result in no additional productivity loss. Analysis of these synergistic effects is worth further exploration to understand particularly detrimental combinations of conditions.
Similar to other literature, we found a higher multimorbidity rate for females compared to males (12, 13). Several of the included conditions were more common in females compared to males, especially those from musculoskeletal (37), sensory, and the other medical conditions categories. Within the other medical conditions category, differences are especially large for migraine or severe headache (13), acne, other medical conditions, and menstrual problems. Menstrual disorders can have a serious impact on work productivity (38–40) but are frequently overlooked in research. However, even though sex differences in multimorbidity were large, this did not alter the strong association of multimorbidity with work productivity loss. Since occupation is associated with both sex and work productivity loss, we adjusted for occupation, but did not find any substantial difference compared to the unadjusted results.
Strengths and limitations
The strengths of the current study include the broad, general working population of young adults, use of a best practice repeated measure of work productivity loss and analyses allowing for non-normal distributions of work productivity loss, sex differences, and occupation influence.
The study limitations include the use of a single cohort from a single geographic region with mainly Caucasian participants and some attrition (18). It has been reported before that while there was some greater attrition of socially disadvantaged participants, there was no apparent resulting selection bias (41). Further, a study on spinal pain and sickness absenteeism within the Raine Study found limited differences between those with full data at the Gen2-22 follow-up and those without (6). To investigate whether attrition influenced the current study sample, we conducted a non-response analysis (supplementary file 5). Whilst the pattern of morbidity was very similar between those included in the analysis and those not included, there were some differences. Amongst females, we found that prevalence of musculoskeletal conditions was higher in the study sample compared to the non-responders (39.5% versus 32.4%). We found that the prevalence of very high multimorbidity (≥4 categories) was lower in the study sample compared to the non-responders (17.1% versus 21.1%) as was the prevalence of zero conditions (13.4% versus 17.1%). Amongst males, we found that prevalence of other medical and mental and neurological conditions was lower in the study sample compared to the non-responders (18.0% versus 24.5% and 15.1% versus 22.2%). Furthermore, the prevalence of very high multimorbidity was lower in the study sample compared to the non-responders (5.7% versus 9.8%). These findings indicate that we may have underestimated the prevalence of multimorbidity and thereby its impact on productivity loss.
Even though data on the presence of 36 conditions were available, 17.4% of females and 9.9% of males reported having a condition different to the current list of 36 conditions. Whilst a best practice measure of multimorbidity was used, this high prevalence of other medical conditions, especially among females, indicates that our list was not exhaustive and that the prevalence of some condition categories might have been higher if we had been able to correctly classify these conditions.
Concluding remarks
In conclusion, the current study found that multimorbidity is already highly prevalent among young working adults and is strongly related to work productivity loss. Since multimorbidity rates are projected to increase in the upcoming years, and the increasing dependency ratio is placing a greater burden on young workers, tackling health-related work productivity loss is important for young workers, their employers, and society at large. These findings emphasize the importance of early prevention and management targeted at minimizing the impact of disorders among young workers through strategies such as reducing multimorbidity, increasing employees’ ability to cope with their conditions, and improving the accessibility of workplaces for employees with health conditions. These strategies need to be already implemented at the start of young workers’ careers.