Low-back pain (LBP) is a considerable health problem with negative impact on long-term sickness absence and early retirement (1), influencing both individuals, workplaces and society (2–4). A survey from 2014 among Danish workers showed that 47% reported pain or discomfort in the back during the past 14 days (5). Hence, knowledge regarding risk factors linked to occurrence, aggravation or reduction of LBP is needed to specify and optimize prevention.
Sitting at work has been suggested to be a risk factor for LBP (6, 7). The reason for this may be that prolonged sitting could relate to LBP by uninterrupted, low-intensity muscle contractions, which may increase systemic levels of pro-inflammatory cytokines (8–10), as well as the loss of muscle strength due to inactivity (11). However, previous reviews, mainly using self-reported duration of sitting, have not established significant associations between duration of sitting and LBP (12–14). However, duration of sitting measured mainly by self-reports, like questionnaires, has been shown to be both biased and imprecise when compared to objective measurements (15–17). Studies using objective measures of the total and temporal patterns of sitting durations in relation to time course of LBP also show mixed findings (17–19). These results could be explained by the cross-sectional nature of the studies (17, 19) or the few measurements of pain over time (18). Also, the association between sitting and LBP has been investigated among different occupational groups with a variety of occupational tasks during sitting, which might affect the relation to LBP differently. Recently, a cross-sectional study showed that the association between duration of sitting and intensity of LBP was moderated by body mass index (BMI) (19). Furthermore, age (20), sex (20), smoking (21, 22), level of occupational lifting (20), occupational sector (23), a diagnosis with a herniated disc (24), level of leisure-time physical activity (25, 26), intensity of physical activity and rating of perceived exertion (RPE) during working hours (27–29), previous episodes of LBP (30), and influence and social support at work (31, 32) have also shown associations with duration of sitting and/or intensity of LBP.
Therefore, the primary objective of this paper was to investigate the association between total and temporal patterns of objectively measured sitting duration at work and individual time course of LBP across one year. The secondary aim was to investigate whether these associations were modified by individual or work-related factors.
Methods
Study design
In brief, this prospective study is based on the Danish PHysical ACTivity cohort with Objective measurements (DPHACTO), enrolling participants from 15 companies in the cleaning, transport and manufacturing sectors between December 2011 and March 2013 (33). The data collection was conducted according to the Helsinki Declaration and approved by the Danish Data Protection Agency and local ethics committee (H-2-2012-011). All workers provided their written informed consent prior to participation.
Baseline measures included web-based questionnaires, objective measurements of anthropometrics and accelerometry. Moreover, workers were asked to state their intensity of LBP every fourth week from baseline to one-year follow-up via text messages, thus a total of 14 text messages were sent (34).
Criteria for inclusion and exclusion
Fever on the day of testing and/or pregnancy excluded workers from participating in the study, and workers with allergy to bandages or adhesives were excluded from the accelerometer measurements (33). Workers were included in the analysis if they answered ≥1 of the 14 sent text messages and had valid accelerometers based measurements for ≥1 working period (valid work period: duration ≥4 hours/day or ≥75% of average wear time during work).
Assessment of exposure
Objective measurements of duration of sitting were collected using two accelerometers (ActiGraphs GT3X+, ActiGraph LLC, Pensacola, FL, USA, actigraphcorp.com), directly mounted on the skin at the front of the right thigh (at the right thigh medial between the iliac crest and the upper border of the patella) and at the back at T1-T2 level by adhesives (17, 35, 36). If the data from the accelerometer mounted at the back did not fulfill the quality criterion, data from the hip accelerometer were used (below the upper point of the iliac crest at the right side). Sitting duration was continuously measured during 4–6 days, 24 hours a day. During these days, the participants were asked to complete a diary stating: working hours, time in bed (when they went to bed and got up in the morning), periods without wearing the monitors, and specific time of reference measurements (upright stance for 15 seconds each day). The reference measurement was used to find the transformations of coordinates between the orientation of the thigh and the axis of the accelerometer (17).
Acceleration data were sampled at a frequency of 30 Hz with a dynamic range of ± 6G and a 12-bit precision. The accelerometers were initialized and data was downloaded using the Actilife software (version 5.5). Accelerometer signals were low-pass filtered at 5 Hz using a fourth-order Butterworth filter and then split up in 2-second windows with 50% overlap, and then analyzed in the customized software called Acti4 (36). Non-wear periods were classified based on the following criteria: (i) the participant registered non-wear in the diary, (ii) the Acti4 detected periods >90 minutes with zero acceleration, and (iii) missing data and/or artefacts were visually detected.
Sitting posture was derived from the accelerometer at the trunk and thigh (37) and classified by a thigh inclination >45° combined with a trunk inclination <45° relative to the recorded reference position (17). The Acti4 software has shown a sensitivity of 99.9% and specificity of 100.0% for determining sitting in standardized field settings, and 98.2% and 93.3% during free living (36).
For this analysis, the duration of sitting at work was computed as total duration, as well as the temporal patterns. Total duration per day was calculated by dividing the total accumulated duration of valid periods of sitting at work across the measured workdays by the number of workdays. The temporal patterns of sitting were quantified by the exposure variation analysis (EVA) (38). For each measurement day, the time-line from the processed accelerometer signal was divided into uninterrupted sitting periods during work. Non-sitting periods were detected as interruptions from sitting for ≥5 seconds. The different EVA categories of sitting were selected from previous studies (35, 39), “brief bursts” (BB) (sitting periods ≤5 minutes), “moderate periods” (MP) (sitting periods of >5–20 minutes), and “prolonged periods” (PP) (sitting periods >20 minutes). The mean duration (hours/day) for each participant spent in each of the EVA categories was calculated by dividing the total accumulated duration of valid periods of sitting during work across all measured workdays by the number of workdays.
Assessment of outcome
During one year, the participants were asked to rate their intensity of LBP by answering text messages every fourth week, collected using SMS track (sms-track.com), resulting in a total of 14 text messages sent (34). The text messages asked “On a scale of 0–10, grade the worst pain you have experienced in your lower back within the past month?” (0=no pain, 10=worst possible pain)”. Previously, the numeric rating scale has been evaluated as valid and reliable for assessment of pain (40). The time scale for the repeated measures of LBP was defined by the time since baseline.
Data collection of potential confounders and moderators
Objective measurements of body weight (Tanita BC418) and height (Seca model 123 1721009) were performed. BMI (kg/m2) was calculated from the objectively measured body weight (kg) and height (m). Age was based on the date of birth for the participant. Sex was determined from the question: “Are you male or female?”. Smoking was assessed by the question “Do you smoke?” using four response categories, which was merged into a dichotomized variable: yes (“yes daily”, “yes sometimes”) and no (“used to smoke”, “I have never smoked”). Time course of LBP was determined by the question: “In the last 3 months, state your worst pain in: lower back?” with an 11-point response scale from 0 (“no pain”) to 10 (“worst pain imaginable”) (41). Use of pain medication was determined by the question:” In the last three months, how many days have you been taking analgesics because of pain in muscles and joints?” using seven response categories, which were merged into a dichotomized variable: 0–14 days (“0 days”, “1–2 days”, “3–7 days”, “8–14 days”) and ≥ 15 days (“15–30 days”, “31–60 days”, “61–90 days”). A diagnosis with herniated disc was assessed by the question: “Do you have herniated discs?” with the dichotomized response “yes” or “no”. Seniority in the current job (years) was assessed using the question: “For how long have you had the kind of occupation that you have now?”. Four items from the Copenhagen Psychosocial Questionnaire (42) assessed influence at work (decision authority) and social support by the questions: “Do you have a large degree of influence concerning your work?”; “Can you influence the amount of work assigned to you?”; “Is there good cooperation between the management and the employees?”; “Is there good cooperation between the colleagues at work?”. The 5-point response scale ranged from 1 (“always”) to 5 (“never”). For the analysis, the scale was recoded to 0–100%, whereby a higher score indicate a higher social support and more influence. For each of the two items, the mean was calculated. Due to a technical error in the data collection neither of the participants from the transportation sector was asked these questions regarding social support and influence at work. Occupational lifting and carrying were assessed by a single item from the Danish Work Environment Cohort Survey (DWECS): “How much of your working time do you carry or lift?” with a 6-point response scale from 1 (“never”) to 6 (“almost all the time”) (43), these six response categories were dichotomized into carrying or lifting ≥50% of the working time or carrying or lifting <50% of the working time. Occupational group was determined by the workplace of the participant and whether the participant stated to be working in the administration (white-collar work) or in the production (blue-collar work), thereby representing four groups: cleaning, manufacturing, transportation and administration. Moderate-to-vigorous physical activity (MVPA) at leisure was assessed by accelerometer measurements, adding up leisure time spent in: running, walking in stairs, and cycling (44). The MVPA duration was normalized to the total measured leisure time. RPE was determined by the question: “How physically demanding do you normally consider your present work?” with a 10-scaled response category (1–10), where 10 was the most demanding. The following variables were tested as moderators: age, sex, BMI, occupational group, MVPA and RPE.
Statistical analysis
All statistical analyses were performed in the SAS version 9.4 (SAS Institute, Cary, NC, USA). The association between objectively measured sitting time (% of working time, continuous variable) and time course of LBP (self-reported intensity on a 0–10 scale across one year) was analyzed in a linear mixed-model for repeated measurements, using an autoregressive covariance structure (AR1) to adapt for the weakening of correlations due to the increased time span. Participants having missing values of intensity of LBP were not excluded from analysis. In the mixed-model analysis, the random factors were participant and intercept, and the fixed factors were the different variables of sitting and time (14 time points across one year), their interaction, denoting an association between sitting and time course of LBP, as well as the confounders. The different variables of sitting (total sitting and brief bursts, moderate and prolonged sitting periods) were analyzed as the independent factor in separate models. The intensity of LBP and time were entered as continuous variables.
All interaction terms between sitting and the potential moderating factors (sitting × moderating factor) were included in a model to investigate whether the relation between sitting and LBP was moderated due to these factors. If the interaction was statistically significant (P<0.10), the interaction term was included in the final model and a complementary stratified analysis was conducted. If the potential moderating factor was not significantly moderating the association, they were considered potential confounders. The potential confounders were tested for critical multicollinearity by the variance inflation estimate; if multicollinearity was present (variance inflation factor > 5), the potential confounder was not included in the adjusted model. Potential confounders were included in the adjusted model by significant (P<0.10) effect on the association between exposure and outcome. By default, the level of LBP the last three months from baseline and sitting during leisure time was included in the adjusted model.
Sensitivity analyses were performed to examine the robustness of the findings. One sensitivity analysis excluded those participants who stated to be free of LBP throughout all of the text measurements (answering 0 at all times). In separate sensitivity analyses, the final model was additionally adjusted for (i) influence and social support at work; (ii) use of pain medication; and (iii) self-reported changes in level of occupational physical activity across the year where the text messages were sent.
Results
Flow of participants
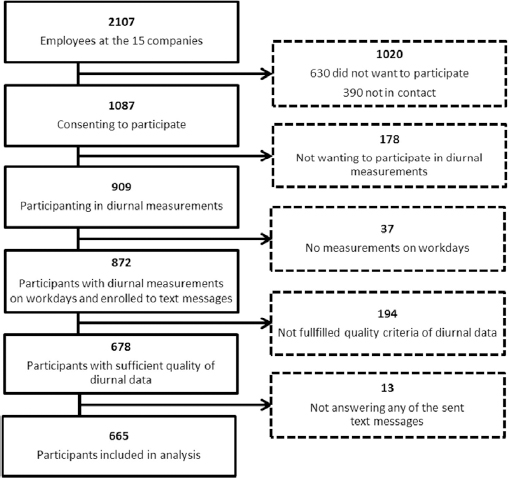
figure 1 shows the flow of participants from the DPhacto included in this study. Of the 2107 employees at the enrolled companies, 665 participants were included in the analysis.
Baseline characteristics of the study population
The baseline characteristics of the study population are shown in table 1. Among the 665 participants constituting the population included in the analysis, 439 (65%) answered all 14 text messages and 576 (85%) answered 12 of the 14 sent text messages.
Table 1
Baseline characteristics of the study population. [SD=standard deviation; LBP=low-back pain]
| Analyzed population (N=665) | ||||
|---|---|---|---|---|
|
|
||||
| Mean | SD | N | % | |
| Age (years) | 45.0 | 10.0 | ||
| Sex (females) | 294 | 44.2 | ||
| Sector | ||||
| Cleaning | 119 | 17.9 | ||
| Manufacturing | 448 | 67.4 | ||
| Transport | 56 | 8.4 | ||
| Administration | 42 | 6.3 | ||
| Body mass index (kg/m2) | 27.4 | 4.9 | ||
| Current smoker | 192 | 28.9 | ||
| Moderate-to-vigorous physical activity during leisure (minutes) | 2.4 | 3.6 | ||
| Daily use of pain medication ≥15 days in last 3 months | 74 | 11.2 | ||
| Seniority in current occupation (years) | 13.2 | 10.1 | ||
| Rating of perceived exertion (scale 1–10)a | 5.1 | 2.2 | ||
| Influence at work (scale 0–100%) | 63.6 | 25.9 | ||
| Social support at work (scale 0–100%) | 78.9 | 16.1 | ||
| Lifting and carrying at work (scale 1–6)b | 3.6 | 1.4 | ||
| Lifting and carrying at work ≥50% work time | 273 | 41.3 | ||
| LBP - duration and intensity | ||||
| Average LBP in text messages through 52 weeks (scale 0–10) | 2.3 | 2.1 | ||
| Peak LBP intensity past 3 months at baseline (scale 0–10) | 3.4 | 3.1 | ||
| LBP intensity, at baseline <5 | 415 | 62.4 | ||
| LBP intensity, at baseline ≥5 | 247 | 37.3 | ||
| Days with LBP in past 12 months >30 days | 176 | 26.5 | ||
| Technical objective measures of sitting time | ||||
| Total measured working hours | 20.0 | 8.0 | ||
| Average working hours per day | 7.7 | 1.6 | ||
| Occupational sitting (% work time) | 33.6 | 22.8 | ||
| Occupational sitting in brief bursts (% work time) | 3.4 | 4.0 | ||
| Occupational sitting in moderate periods (% work time) | 6.3 | 6.1 | ||
| Occupational sitting in prolonged periods (% work time) | 5.6 | 9.1 | ||
Construction of statistical model
Due to the non-normal distribution of the exposure variables, a square root transformation was applied to make them fit a normal distribution. No critical multicollinearity was indicated by the multicollinearity diagnostics applied to all of the potential confounder variables, thus all of the variables were kept in the analysis.
Of the potential modifiers, time was the only variable significantly interacting with sitting on LBP across one year, in the model also adjusted for confounding factors. However, RPE (P=0.01) and age (P=0.05) were also considered as moderators due to their significant interaction with sitting duration during work in an unadjusted model. Therefore, analysis stratified on median age and RPE were applied.
The potential confounders kept in the model were diagnosis with herniated disc, peak intensity of LBP during the past three months collected at baseline, occupational lifting and sitting during leisure time.
Primary analysis of association between sitting and LBP
Table 2 shows the results from the crude and adjusted models for sitting at work (in total duration and in the temporal variables) both of which showed, significant negative associations with the time course of LBP. Back transformation, by taking the square root of the beta, shows that these negative associations corresponds to decreases in the one year time course of LBP of approximately -0.05 points, on a 0–10 scale of LBP (corresponding change in pain in adjusted model are total time: -0.03; BB: -0.06; MP: -0.06; and PP: -0.06). Thus, for every 1% (corresponding to approximately five minutes) increase of sitting at work, a decrease in one year time course of -0.05 points in LBP will be expected. These results indicate that an increase in duration of sitting, independent of bout duration, would decrease the time course of LBP.
Table 2
Associations for square root transformed total and temporal patterns (exposure variation analysis derivatives) of sitting during work with the time course of low-back pain (scale of 0–10 scale). Duration of sitting is reported as 10% increments of sitting time. Estimates denote the interaction sitting × time.
| B | SE | P-value | 95% CI | |
|---|---|---|---|---|
| Total sitting (% working time) | ||||
| Model 1a | -0.050 | 0.007 | <0.001 | -0.065– -0.037 |
| Model 2b | -0.050 | 0.007 | <0.001 | -0.065– -0.040 |
| Brief bursts (% working time in bouts of ≤5 minutes) | ||||
| Model 1 | -0.124 | 0.017 | <0.001 | -0.158– -0.090 |
| Model 2 | -0.118 | 0.017 | <0.001 | -0.152– -0.084 |
| Moderate periods (% working time in bouts of >5−20 minutes) | ||||
| Model 1 | -0.121 | 0.017 | <0.001 | -0.155– -0.088 |
| Model 2 | -0.117 | 0.017 | <0.001 | -0.151– -0.084 |
| Prolonged periods (% working time in bouts of >20 minutes) | ||||
| Model 1 | -0.123 | 0.018 | <0.001 | -0.158– -0.088 |
| Model 2 | -0.123 | 0.018 | <0.001 | -0.158– -0.088 |
Stratified analyses of association between duration of sitting and time course of LBP
Adjusted analyses similar to model 2 were conducted in sub-populations stratified on age (median split of ≥/< 46 years) and RPE (median split of ≥/<6 on scale from 0–10). All of the analysis in the sub-populations of age and RPE showed results numerically and statistically similar to the results reported in table 2 on the non-stratified population (results not shown).
Sensitivity analysis
The sensitivity analysis excluding participants without any LBP throughout the study (ie, reporting 0 in pain intensity during all 14 time points, N=47), showed estimates numerically and statistically similar to model 2 on the whole population (results not shown).
The sensitivity analysis additionally adjusted for influence and social support at work showed estimates numerically and statistically similar to model 2 (results not shown).
The sensitivity analysis excluding participants answering to use pain medication >15 days across the previous three months (N=74, 11%), showed estimates numerically and statistically similar to model 2 on the whole population (results not shown).
Additionally, the analyses of associations between sitting and time course of LBP were conducted on sitting during all waking hours (leisure and work summed); the analyses showed results numerically and statistically similar to those reported in table 2 (results not shown).
Discussion
The primary analysis showed a statistically significant interaction between sitting and time, which indicates that time significantly moderated the association between sitting and one year time course of LBP. That is, higher durations of sitting at work, both in total duration and temporal patterns, were associated with a favorable time course of LBP intensity across one year. This finding suggests that more sitting at work is a beneficial factor for LBP, which is in contrast to what a number of previous studies have suggested (8–11). However, one recent study by Lunde and colleagues (18) also found sitting at work to lower LBP prospectively. Such beneficial effect of sitting may reflect that workers are not exposed to other harmful work tasks for LBP occurring during non-sitting, and that time spent sitting may be used to recover from hazardous work tasks. For example, in this population of primarily blue-collar workers, time not spent sitting is likely allocated to other occupational activities, eg, lifting and carrying tasks, known to increase the risk for LBP (45–47).
Moreover, of the potential modifiers, only time showed to significantly interact with sitting in the adjusted model. Also age and RPE significantly interacted with sitting in the crude model, but the analysis stratified on age and RPE did not show results different from the primary analysis, indicating that age and level of RPE do not moderate the relation between sitting and time course of LBP. Although the cross sectional analysis showed a moderating effect from BMI (19) this prospective analysis did not.
Previously, a cross-sectional study in the same dataset found similar findings of the association of temporal pattern of sitting and LBP (19). Considering the results of both the cross-sectional analyses and the current prospective analyses, it seems like sitting, per se, does not impose a risk for LBP among this population of workers from primarily blue-collar sectors. These findings, of associations between sitting and LBP, is in line with some of the previous literature, using both self-reported and objective methods for retrieving information on duration of sitting (12–14, 18). In contrast, some cross-sectional studies, using both objective and subjective methods for retrieving information on duration of sitting have reported significant positive associations between sitting and LBP (17, 48, 49). Hence, the lack of consistency in associations between studies does not seem to be explained by the method for retrieving information on duration of sitting, and neither by low frequency or few measures of pain. Instead, the inconsistent findings on associations between sitting and LBP can be due to the great variety of study populations, eg, including a higher proportion of white- or blue-collar workers.
Methodological considerations
This study used two tri-axial accelerometers to objectively measure duration of sitting. The accelerometer data were analyzed in the Acti4 software which discriminates sitting from lying and standing and thereby minimizes the misclassification of exposure. Additionally the large size of the homogenous study population of workers is a strength due to the possibility of detection of small effect sizes with sufficient statistical power. Additionally, the sensitivity analysis showed results similar to the results in table 2, indicating robust results.
However, some limitations are also present; the homogenous study population of blue- and white-collar workers from blue-collar sectors may limit the generalizability of the results to other populations of mainly white-collar workers. For example, exposure to other non-sitting occupational factors being risk factors for LBP is more likely among blue- than white-collar workers. Also, the rather few white-collar workers in DPhacto limit the possibilities of comparison between white- and blue-collar occupational groups. Not all participants answered the question regarding social support and influence at work due to a technical error; therefore we are unable to completely rule out confounding by these factors. Hence, a sensitivity analysis in the sub-sample of participants answering these questions (N=464) was conducted with additional adjustment for social support and influence at work. This sensitivity analysis indicated our results to be robust because it showed numerical and statistical results similar to the final model in table 2 on the entire population. Another limitation is the large amount of workers with pain during baseline. Thus, it was not possible to estimate risks among initially pain-free workers. Furthermore, this study showed small associations between sitting at work and time course of LBP, implicating that future studies should take the entire exposure from body postures and physical activities into account, like in a compositional data analysis (50).
Concluding remarks
Both total and temporal patterns of sitting at work were significantly associated with a favorable time course of LBP across one year. None of the investigated moderators significantly interacted with sitting, except time. The associations indicate that sitting may be a beneficial factor for LBP by protecting from aggravation of LBP among populations of mainly blue-collar workers. However, this finding needs to be confirmed in other occupational groups.