Sickness absence among pregnant women is frequent (1–5). A number of studies indicate that the amount of sickness absence in pregnancy has increased over the past decades, yet without clear medical explanations (5–8). Factors such as course of pregnancy (9), occupational exposures (10), levels of social benefits (8, 11), and attitudes towards sickness absence, experiences and worries (2) have been associated with levels of sickness absence. However, a number of other factors could potentially also influence sickness absence levels.
The combination of work outside the home, domestic duties, and natural physical fatigue increases the total strain among pregnant women, and this may particularly affect sickness absence among multiparous women (9, 12). Body mass index (BMI) could be hypothesized as a risk factor for sickness absence in pregnancy, as BMI is positively associated with pregnancy-related pelvic pain (13), and high BMI has been suggested to reduce the capability to perform manual work during pregnancy (14). BMI among European women has increased in the past decades, which also affects an increasing number of pregnant women (15).
The number of assisted reproductive therapy (ART) treatments has increased steadily during the past 15 years, and today 8% of childbirths arise from ART (16). ART is often linked to prolonged waiting time to pregnancy (TTP), and women who become pregnant after ART experience more pregnancy-focused anxiety compared to women conceiving spontaneously (17, 18). We hypothesize that this could lower thresholds for sickness notification among ART-pregnant women and women with prolonged TTP.
Physical exertion at work and risk of adverse pregnancy outcome has been investigated in numerous studies with conflicting results (19–24). In consequence, precautionary principles are followed, and pregnant women are advised to reduce occupational exposures like heavy lifting as well as prolonged walking and standing, especially late in pregnancy (22, 25, 26). On the other hand, pregnant women are not discouraged from leisure time physical activity – hereafter referred to as physical exercise – and the Danish Health and Medicines Authority currently recommends physical exercise at a moderate intensity level for a minimum of 30 minutes per day for women with uncomplicated pregnancies (25).
On the basis of limited knowledge about how these factors are associated with sickness absence, we aimed to investigate associations between parity, pre-pregnancy BMI, ART, TTP and engagement in physical exercise and the risk of sickness absence in pregnancy from 10–29 completed pregnancy weeks.
Methods
Study population
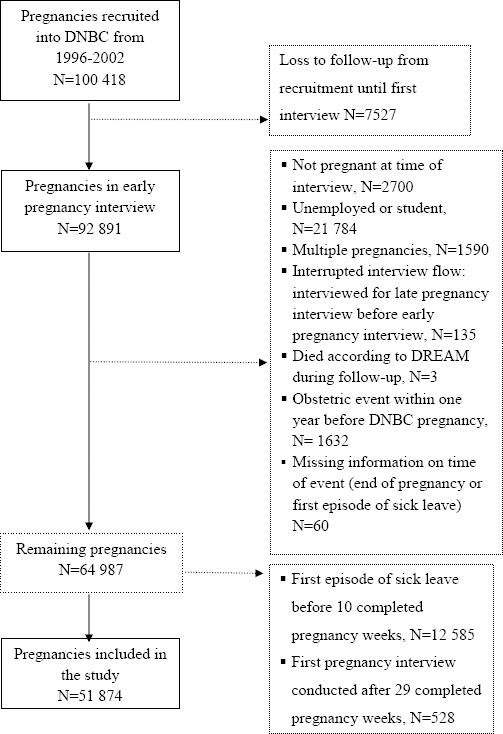
We used data from the Danish National Birth Cohort (DNBC), a population-based pregnancy cohort, including 100 418 pregnancies enrolled between 1996–2002. Women were invited to participate at the first antenatal visit with their general practitioner. Inclusion criteria were: (i) Danish residency, (ii) an intention to complete pregnancy, and (iii) sufficient fluency in Danish to participate in four telephone-based interviews. The basic data collection in DNBC included four computer-assisted telephone-based interviews, three blood samples, and a food frequency questionnaire. Two interviews were conducted during pregnancy (around pregnancy week 17 and 30) and two postpartum (6 and 18 months). The cohort is described in detail elsewhere (27). In this study, we included pregnancies where information was collected in the first pregnancy interview (N=92 891). For definition of the studied pregnancies, see (figure 1). The final number of pregnancies studied was 51 874 among 49 708 women, as some women contributed with more than one pregnancy. The Scientific Ethical Committee approved the cohort, and the Danish Data Protection Agency and the DNBC Steering Committee approved storage, handling, and linkage of data for the current study (approval number 2012-41-0086 and 2012-06).
Predictors
All independent variables came from the first pregnancy interview (in completed pregnancy weeks: 18 (mean); 17 (median); 25th percentile: 14, and 75th percentile: 20). The following questions and corresponding answer categories all available at www.dnbc.dk were used (translated from Danish). Parity [yes/no (reference)]: “Have you given birth before?” BMI: “What was your weight before the pregnancy?” and “How tall are you?” BMI was calculated as weight (kg)/[height (m)]2 and grouped according to WHO classification: underweight (<18.5 kg/m2), normal weight (18.5–<25 kg/m2 [reference)], overweight (25–<30kg/m2) and obese (≥30 kg/m2) (28). TTP: “For how long time did you try to get pregnant before you succeeded?” (Did not try to get pregnant, got pregnant immediately (reference), 1–2 months, 3–5 months, 6–12 months, for more than 12 months). TTP for women reporting not trying to get pregnant were coded as missing. ART [yes/no (reference)]: “Did you get any infertility treatment prior to this pregnancy?” Engagement in physical exercise (yes/no): “Do you get any kind of exercise during pregnancy?” If yes, “What kind of exercise?”, “How many times a week do you exercise?” and “How many minutes at a time do you exercise?” Minutes of weekly physical exercise were calculated and categorized in five groups: 0, 1–30 (reference), 31–60, 61–120, and >120 minutes. All independent variables that were answered “do not know” or “do not want to answer” were coded as missing.
Sickness absence
We used the Danish Register for Evaluation of Marginalisation (DREAM) to measure sickness absence (29). DREAM contains weekly information on more than 100 types of public benefit payments, varying from state educational funds to retirement pension. Each type of benefit is characterized by a unique code, sickness benefits are coded according to the type of employment preceding sick leave. In Denmark, sickness during pregnancy is classified as sickness absence or pregnancy-related sickness absence, the latter due to either abnormal course of pregnancy or due to conditions in the work environment potentially harmful in pregnancy. At the time of data collection, reimbursement of sickness absence benefit, a prerequisite for DREAM registration, was conditional on a minimum of two weeks of consecutive sickness absence paid by the employer. Thus, sick leave <15 consecutive days was not registered in DREAM. As for pregnancy-related sickness absence, employers received reimbursement from the first days of sickness absence. Finally, a weekly registration in DREAM requires merely one day of sickness benefit payment during the week in question.
For each completed pregnancy week from 10–29, we estimated sickness absence for gainfully employed women, using the following DREAM codes: 774 (sickness absence from flexi-jobs – jobs for people with reduced ability to work because of chronic illness), 881 (maternity leave and pregnancy-related sickness absence), 890, 892, 893, 894, 895, 896, 897, 898, and 899 (all sickness absence codes for either ordinary employment, various job training programs, apprenticeships or part-time sick leave) (29).
Time of first episode of sickness absence from 10 to 29 completed pregnancy weeks was the primary outcome in this study.
Potential confounders
We adjusted for the following a priori selected potential confounders based on the literature: age, daily smoking, weekly intake of alcoholic drinks, physical and psychological demanding work environment, socioeconomic status, weeks of sickness absence two years prior to the DNBC pregnancy, and chronic diseases. Parity analyses were furthermore adjusted for family structure. The variable age was the women’s age at the time of first pregnancy interview. Mean of self-reported alcohol intake (drinks/week) and daily tobacco smoking (yes/no) were generated from questions in the first pregnancy interview. Physical and psychological job demands (often, from time to time, seldom) were generated based on first pregnancy interview data. Socioeconomic status in five categories (unemployed, unskilled workers, skilled workers, lower grade professionals, higher grade professionals) was based on educational level and the Danish version of International Standard Classification of Occupations (DISCO-88). If educational level or DISCO-88 codes were missing for the pregnant women, information for the spouse or cohabiting partner was used. The women provided this information at the first pregnancy interview. Sickness absence prior to the DNBC pregnancy was assessed using DREAM data. We included information 104 weeks back in time from the onset of the DNBC pregnancy and counted the number of weeks each woman received sickness benefit payment (excluding pregnancy benefits). Sickness absence prior to the DNBC pregnancy was categorized in five groups (≥26, 9–25, 5–8, 1–4, and 0 weeks). The variable “chronic diseases” (yes/no) was generated from information on self-reported diseases and included cardiovascular, metabolic, musculoskeletal, epilepsy, and psychiatric disorders as well as other diseases classified as severe. Finally, a variable family structure was created, which included information on civil status and having children in the household.
Statistical analysis
Data were analyzed by multivariate Cox regression models using pregnancy week as the underlying time variable. The calculation of pregnancy week was based on self-reported due date from the first pregnancy interview and the date was based on last menstrual period. If these data were missing, data from the late pregnancy interview were used.
Time at risk started at first pregnancy interview, and ended at first episode of sickness absence, pregnancy termination (abortion, preterm delivery or still birth), or end of the study period at 29 completed pregnancy weeks, whichever came first. Pregnancies of women with sickness absence at the time of first pregnancy interview or prior to the first interview were excluded from the analyses.
Risk estimates are presented as crude and adjusted hazard ratios (HR) for the whole study period and for four pre-defined completed pregnancy week periods; (week 10–14, 15–19, 20–24, and 25–29). Time at risk in each of the four pregnancy week period started at the beginning of the time intervals and ended at first episode of sickness absence, pregnancy termination (abortion, preterm delivery, or still birth), or end of the time period, whichever came first. No pregnancies were included in the pregnancy week period analyses before time of first pregnancy interview. Women on sick leave were excluded from the analyses in the following pregnancy week periods. Trend test estimates for dose–response relations represent the following unit changes: BMI (one-unit change in BMI), TTP (one-unit change in TTP category), and physical exercise (one-unit change in exercise category). We calculated time-varying coefficients for all the predictors to estimate time-dependent effects of the predictors with time since 10 completed pregnancy weeks. Trend tests were calculated for the time-varying coefficients, and represent trends on weekly HR from 10–29 completed pregnancy weeks for the predictors. Finally, we conducted three sub-analyses in which we (i) excluded ART pregnancies to take the close relation between ART and TTP into account, (ii) further adjusted for selected pregnancy-related disorders (vaginal bleeding, painful Braxton hick’s contractions, risk of giving preterm birth, nausea and vomiting during pregnancy), and (iii) restricted the analysis to the first DNBC participation for women participating more than once in DNBC in order to estimate possible clustering of events. Pregnancy-related disorders were included, because they are risk factors for sickness absence. Data on the pregnancy-related disorders were obtained from the second pregnancy interview at (mean) 32.2 completed pregnancy weeks.
Data were analyzed using STATA, version 13.0 (STATA Corp LP, College Station, Texas, USA).
Results
In 12 585 pregnancies (19.5%), the first episode of sickness absence occurred before the first pregnancy interview. Cumulative incidence proportion of sickness absence was 36.0% from onset of pregnancy until 29 completed pregnancy weeks and 20.6% from first interview until 29 completed weeks. Table 1 gives a description of sickness absence prevalence for each pregnancy week from 10–29 completed pregnancy weeks. In the study period, the prevalence of sickness absence increased from 2% to 17%.
Table 1
Prevalence of sickness absence according to pregnancy week from 10–29 completed pregnancy weeks (N=51 874).
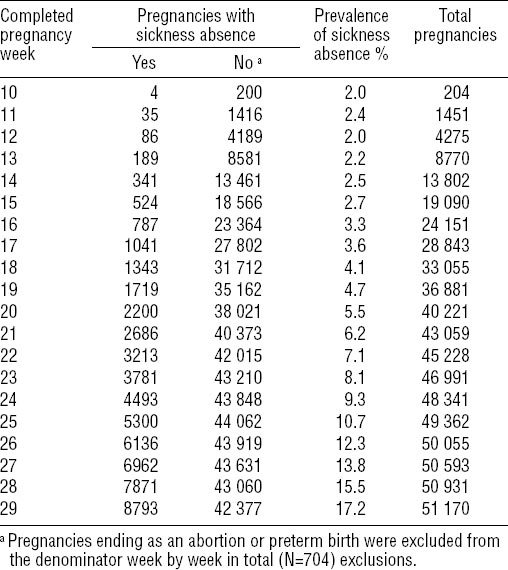
Table 2 provides a description of the pregnancies according to the first episode of sickness absence between 10–29 completed pregnancy weeks or no sickness absence. There were small and probably not clinical important differences in mean age and mean pregnancy week at first interview between pregnancies in women with and without sickness absence. Pregnancies with sickness absence were more frequent among women who were smokers and alcohol abstainers compared to pregnancies in women without sickness absence. Larger proportions of pregnancies resulted in sickness absence among women, who suffered from chronic diseases, and who reported physically and psychologically demanding working conditions. Sickness absent women were more often skilled and unskilled workers and sickness absent the two years prior to study entry and had more often children in the household compared to non-sickness absent women.
Table 2
Characteristics of the pregnancies (N=51 874) according to first episode of sickness absence from 10–29 completed pregnancy weeks. [SD=standard deviation]
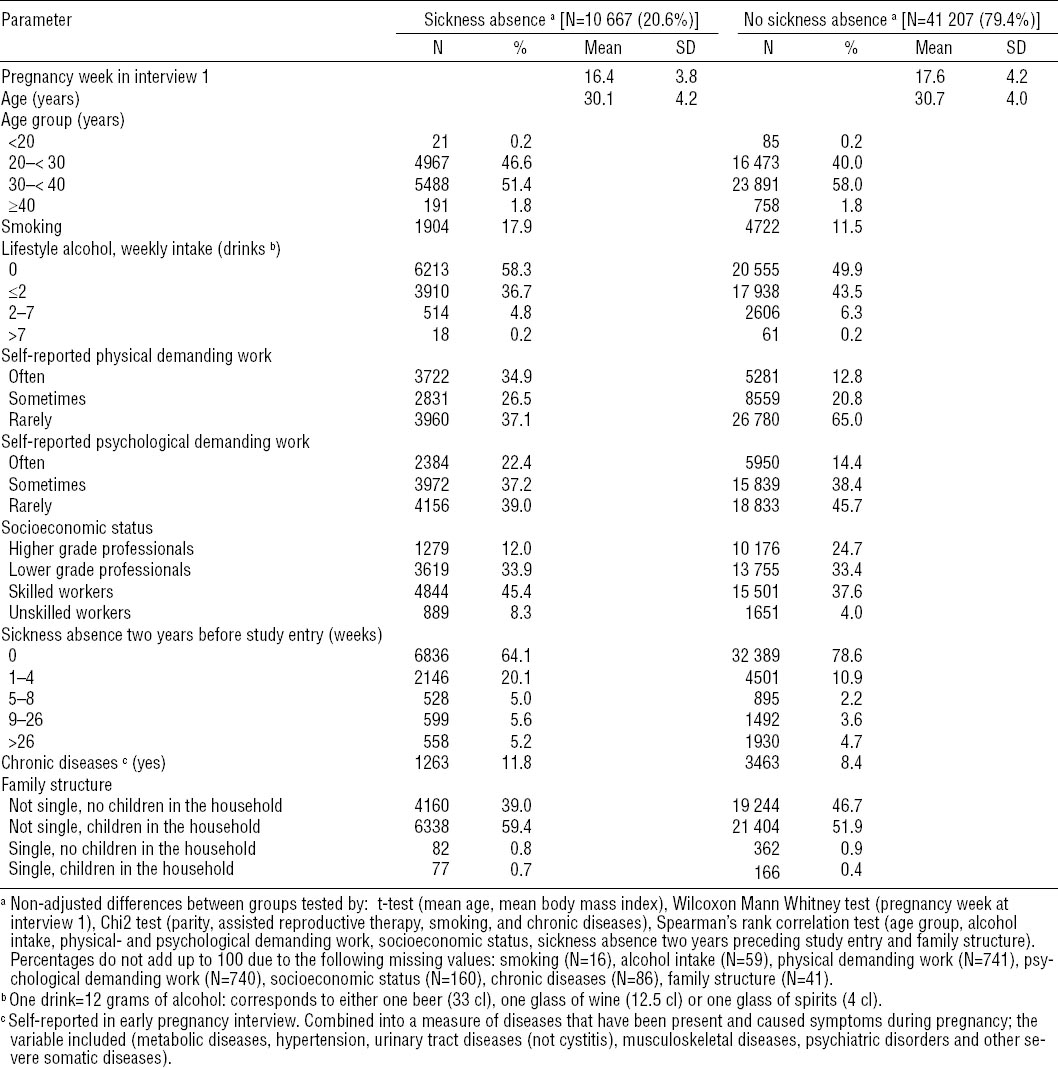
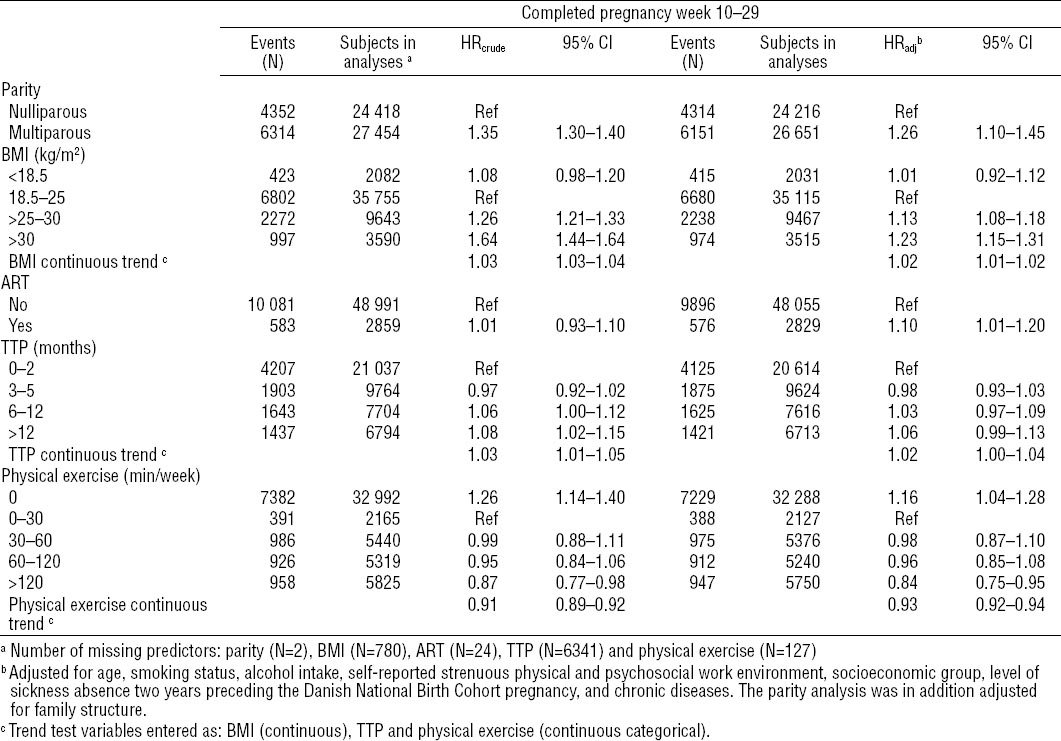
Table 3 shows crude and adjusted HR with 95% confidence intervals (95% CI) for first episode of sickness absence from 10–29 completed pregnancy weeks. In the adjusted analyses, multiparity, overweight, obesity, ART, and no engagement in physical exercise were associated with higher HR of sickness absence compared to the reference groups. HR increased in a dose-dependent way with increasing BMI and TTP in crude as well as adjusted analyses. Engagement in physical exercise of >120 minutes per week was associated with lower risk of sickness absence compared with the reference group, and physical exercise was associated with lower risk of sickness absence in a dose-dependent way.
Table 3
Crude (HRcrude) and adjusted (HRadj) hazard ratios of first episode of sickness absence from 10–29 completed pregnancy weeks according to predictors N=51 874. [95% CI=95% confidence interval; BMI=body mass index; ART=assisted reproductive therapy; TTP=time to pregnancy.]
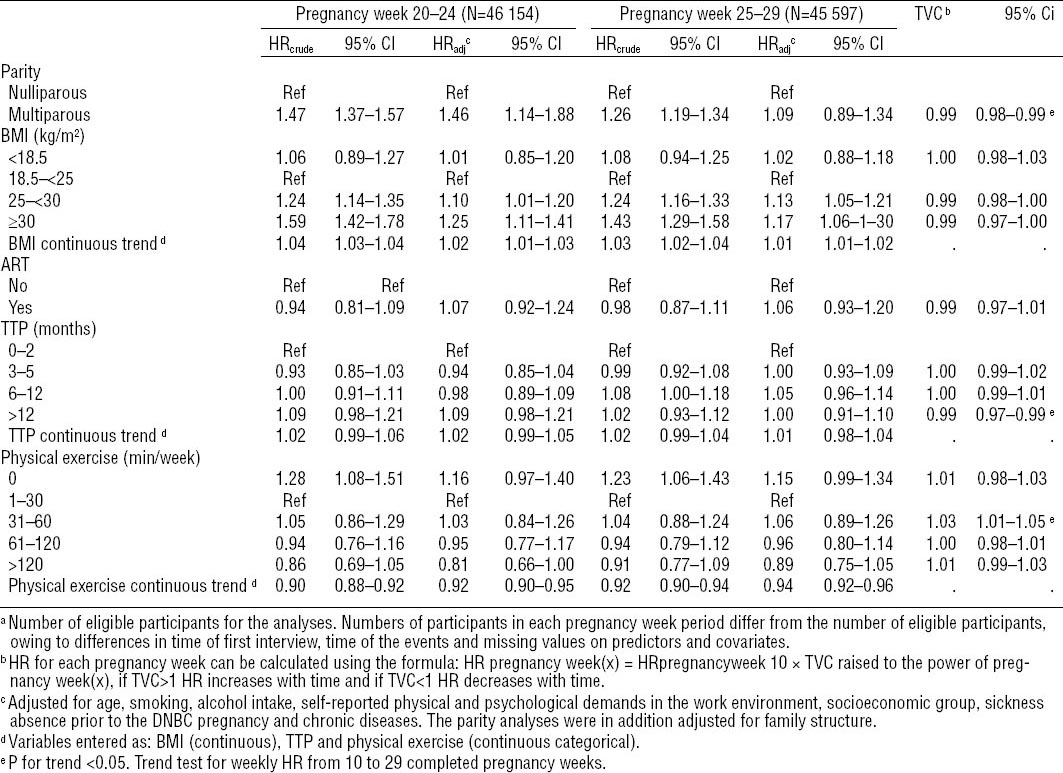
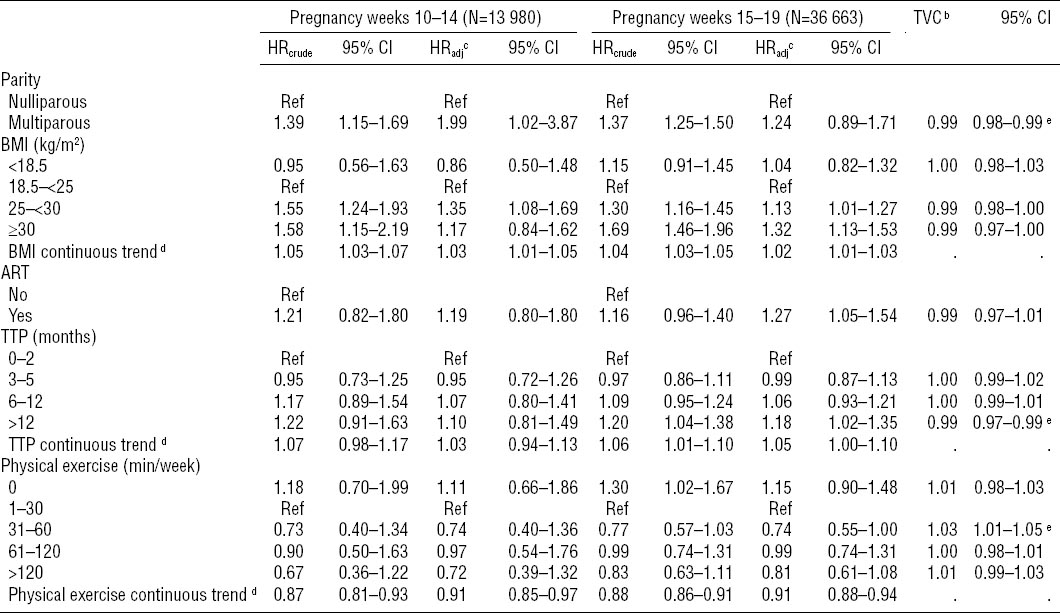
The study period was split into four time periods to evaluate time-dependent effects of the predictors measured by time-varying coefficients (table 4). We found increased HR for sickness absence during all four time periods for multiparity, overweight, obesity and ART. HR for TTP of 6–12 months and TTP>12 months were in most intervals increased compared to the reference groups. The effects of multiparity and TTP >12 months were time dependent, as HR decreased with number of completed pregnancy weeks in a statistically significant way. Time dependent effects indicated increasing hazards of sickness absence with time at levels of physical exercise between 31–60 minutes per week. There was no substantial difference in HR according to time period for BMI, ART, and remaining TTP and physical exercise intervals.
Table 4a
Crude (HRcrude) and adjusted (HRadj) hazard ratios of first episode of sickness absence from 10 until 29 completed pregnancy weeks according to predictors in four pregnancy week period intervals. Follow-up started at time of first pregnancy interview, pregnancies of sickness absent women at that time of or before time of follow-up started were excluded from the analyses N=51874 a [95% CI=95% confidence interval; BMI=body mass index; ART=assisted reproductive therapy; TTP=time to pregnancy; TVC=time varying coefficient.]
To address the possible close relation between ART and TTP, we made a sub-analysis in which pregnancies resulting from ART (N=2859) were excluded (supplementary table A, www.sjweh.fi/data_repository.php). Overall, the results were in the same direction as in the main analyses. We did not adjust for pregnancy-related disorders in the main analyses, as we did not have such information by the time-of-first-pregnancy interview. In a sub-analysis, we used data from the late pregnancy interview to adjust for self-reported pregnancy complications. However, these adjustments did not change the results appreciably (supplementary table B, www.sjweh.fi/data_repository.php). The sub-analysis for possible clustering of events did not change the results either (data not shown).
Discussion
We found multiparity, overweight, obesity, ART and TTP >12 months to be associated with a higher risk of sickness absence. Physical exercise was associated with a lower risk.
In Scandinavian studies, the reported cumulative incidence of sickness absence during pregnancy varies from 29% to 72% (9, 10, 30–32). These variations can largely be explained by differences in definitions of sickness absence. We found a cumulative incidence proportion of 36.0% from onset of pregnancy until 29 completed pregnancy weeks and of 20.6% from 10–29 completed weeks. These results are in accordance with results from the Norwegian Mother and Child Cohort Study that is similar to DNBC in structure, where the authors reported 36.2% of the participants having >14 days of sickness absence by pregnancy week 28 (32). Absence risk between pregnancy week 17–30 in the Norwegian Mother and Child Cohort Study was associated with young age (55%), low education (45%), high parity (40%), multiple pregnancies (87%), and smoking (35%) (32). Risk associated with parity ranged from 26% (nulliparous) to 40% (para ≥4). Although we classified multiparity differently from the Norwegian Mother and Child Cohort Study, our results are in accordance with the Norwegian results. Other studies have also investigated associations between parity and sickness absence with conflicting results (3, 31, 33). A Danish study found no significant association between multiparity and sick leave among hospital employees [odds ratio (OR) 1.3, 95% CI 0.9–1.9] (3), whereas two Norwegian studies found significant associations between multiparity and measures of sick leave in pregnancy (OR 1.40; 1.55) (31, 33). A Swedish study investigated sex differences in sickness absence patterns in relation to parental status and found a relation between having custody of children and sickness absence among women (34). These results suggest that women in general might be more sensitive to imbalances between work and personal life compared with men, and this could at least partially explain the observed association between parity and sick leave in pregnancy.
To our knowledge, only one previous study has examined the associations between obesity and sickness absence and social benefit payments among pregnant working women (14). In Sweden, there are two types of benefits additional to sick leave, parental benefit, and pregnancy benefit. Parental benefit ensures women the right to take time off after delivery, yet up to 60 days of the parental benefit can be used before delivery. These days will subsequently be subtracted from the after-delivery parental benefit period. Pregnancy benefit can be granted to women having demanding and monotonous jobs from between 60 to 10 days before delivery and granting is not based on the women’s actual health. In the Swedish study, authors found that obese women made more use of both parental benefits and pregnancy benefits compared to normal weight women, suggesting that there may be a possible incompatibility between pregnancy, obesity, and engagement in employment (14). Surprisingly, the authors did not find obesity to be predictive of increased number of sick leave days (14). Sickness absence without relation to pregnancy has been found to be associated with obesity in several studies (35–37). Associations are first of all believed to originate from obesity-related co-morbidities, possible susceptibility to non-chronic health problems, longer recovery time or even discrimination, but obesity could also reduce the ability to meet physical work load requirements in some jobs (36). We do not know whether the association we found between BMI and sickness absence was due to obesity, per se, or a combination of obesity and pregnancy.
Only one study previously investigated associations between ART and sick leave during pregnancy (33); the authors found an association between ART and sick leave in all three trimesters (OR 1.77; 95% CI 1.27-2.46), which is in agreement with our results. However, the authors included multiple pregnancies and did not adjust for co-morbidities and measures of work load in their study, which makes both interpretation and comparison with our results difficult. The findings, though, are not surprising, as we expect ART-pregnant women to be more anxious about the course of pregnancy and more alert and worried about natural pregnancy-related discomfort compared to women conceiving naturally. We found no studies in our literature search investigating associations between sickness absence and TTP.
Several studies using prospectively collected data have found that physical exercise is associated with reduced sickness absence (38–40). A Norwegian study found an association between no weekly exercise and increased odds for sick leave in pregnancy (OR 1.79; 95% CI 1.69–2.31) (33). Our results corroborate these findings. However, pregnant women who exercise may be of better health than non-exercising pregnant women, and, thus, our results could overestimate the presumed beneficial effect of exercise. Furthermore, if some of the pregnant women stopped exercising due to pregnancy disorders associated with future sickness absence, we might overestimate the beneficial effect of exercise due to reverse causation.
Strengths of our study include the large sample size and the ability to adjust for a wide range of prospectively collected potential confounders. The overall participation rate in DNBC was approximately 31% and varied according to education, occupation, income, and civil status (41). Non-participation in DNBC was either caused by the general practitioners (approximately 50% participated) or the women themselves (approximately 60% participated). This selection, partially associated with socioeconomic factors, could cause confounding. However, we believe that the adjustment for socioeconomic status in the statistical analyses minimizes important confounding due to this selection. Even so, the selection into DNBC can affect the external validity of our study, and our results may not apply to other populations of pregnant women.
Information on predictors and covariates was based on self-reports and could be subject to misclassification. Yet, if present, misclassification is not believed to be related to sickness absence, and our results would therefore most likely be biased towards the null. The outcome of interest (ie, sickness absence) was based on register information from DREAM. This register has recently been validated in a study comparing employer registration of sickness absence with DREAM registration (42). Sensitivity and specificity were very high for ordinary sickness absence but very low for pregnancy-related sickness absence (42). We believe this could be due to exclusion of pregnancy-related sickness absence or maternity leave (DREAM code “881”) from the analyses. A validation of DREAM data in relation to sickness absence in pregnancy is thus still required. We have included women, who refrain from working due to exposures in their work environment. These women are not specifically identifiable in DREAM because they have no specific DREAM code. However, we do not believe misclassification of their outcome is concurrently associated with the predictors. The misclassification may therefore most probably lead to bias towards the null.
We adjusted for a number of possible confounders, yet residual confounding and confounding by variables not included in the models cannot be ruled out. Adjustment for pregnancy-related disorders diagnosed by the women’s general practitioner or obstetrician would have been relevant, but unfortunately we did not have these data.
In summary, we found higher risk of sickness absence in pregnancy with multiparity, overweight, obesity, ART, and prolonged TTP, and lower risk with leisure-time physical exercise. Only few studies have investigated these associations, and our results should be confirmed in other studies of pregnant women.