Construction painters are occupationally exposed to a multitude of chemical substances in paint such as binders, solvents, pigments, extenders, and additives. Dust and volatiles are inhaled and chemicals with small molecular weight are absorbed by the skin (1). In 1989, the International Agency for Research on Cancer (IARC) classified the occupational exposure of construction painters as a group 1 carcinogen (2). This classification was reinstigated in 2010 and 2012 (3, 4), although the assumed causal workplace exposures have not been identified. The classification as a group 1 carcinogen raises concerns that occupational exposures of pregnant construction painters also constitute a risk factor for unborn children. If the carcinogens are targeting parental germ cells in the pre-conception period, they might induce DNA damage that could affect the conceptus (5). Furthermore, carcinogenic effects may influence embryonic or fetal development. Impaired development may result in fetal death, malformations, restricted growth, or functional disruptions (6). Moreover, several components of paints and lacquers are classified as reproductive toxicants without a concomittant classification as carcinogen (3, 7).
In Denmark, the prevalence of live-born children diagnosed with malformations within the first year of life was reported to be 4.2% in 1994 and 5.0% in 2005 (8). Whether the slight increase in prevalence in fact reflects an actual higher incidence is unknown, but it is plausibly driven by better examination and diagnostics. In Denmark, the paint industry employs a large number of women, constituting 50% of those who are enrolled in vocational paint training (9). Physicians recommend pregnant women to change to alternative work tasks or to go on paid sick leave if there is any suspicion of harmful exposures in the working environment. However, these precautions might not be sufficient to protect the unborn child. The vulnerable period for induction of structural anomalies is from the third to the eighth gestation week (10). During this time, the pregnancy is often unconfirmed and the woman might not have informed her employer. On the basis of the large number of women involved in construction painting, the insufficient protection of the unborn child in the vulnerable period, and IARC’s classification of paint exposures as carcinogenic, it is relevant to study pregnancy outcomes of maternal painters. Studies that provide information about potential reproductive risks for construction painters can be used to improve the working environment through counselling of pregnant construction painters and the paint industry as a whole.
A Danish cohort study from 2012 on 19 935 pregnant women found an increased risk of congenital anomalies of the renal system among children of mothers who were exposed to paint fumes in their residence in the first trimester (11). The pregnant women did not necessarily do the painting. It must be assumed that construction painters have higher exposure than domestically exposed women because of their repeated exposure during paint application and removal.
The aim of this nationwide register study was to investigate whether there is an association between maternal or paternal employment as a construction painter and the risk of congenital malformations among live-born children.
Methods
Data sources
We obtained data on births, parental employment status, and hospital diagnoses of congenital malformations from the Danish Civil Registration System, (12) the Fertility Database, (13) the Employment Classification Module from Statistics Denmark, and the Danish National Patient Register (14). All inhabitants in Denmark are given a unique 10-digit identification number assigned from the Danish Civil Registration System, which we used to link parents to their children in the Fertility Database. The Employment Classification Module from Statistics Denmark annually collects information on employment status for every tax-paying Danish citizen from the age of 15. It provides an occupational and industrial classification code for the main source of income every year. The occupations are coded according to the occupational position group (NYSTGR) in 1980–1990; the Danish Version of the International Standard Classification of Occupations of 1988 (DISCO-88) in 1991–2009; and the International Standard Classification of Occupations of 2008 (DISCO-08) from 2010. The industries are coded according to the Danish Industrial Classification (DB), which is the Danish version of EU’s nomenclature (NACE). The codes have changed over time: DB77 was applied in 1980–1992; DB93 in 1993–2002; DB03 in 2003–2007; and DB07 from 2008. The Danish National Patient Register (also known as the National Discharge Register) provides data from all inpatient hospital admissions from 1977 and outpatient contacts from 1994 and has been validated for registration of congenital abnormalities (15, 16). Diagnoses of malformations are registered according to the International Classification of Diseases 8th Revision (ICD-8) in 1977–1993 and the 10th Revision (ICD-10) from 1994 until today.
Cohort
The cohort includes all singleton live births in Denmark in the period 1 January 1980 to 31 December 2010. Children who emigrated before the age of one were excluded, but children who died within the first year of life are included in the cohort. Only children of women with an active employment status in the year of pregnancy were included in the main cohort. Active employment status was defined as an occupational and an industrial classification code registered for the year of interest. Unemployed, students, retired, and persons with an unknown occupational status were not included. We applied the employment status from the previous year for births between January and June. For births between July and December, we applied the employment status from the birth year.
For sub-analyses concerning the paternal exposure, a cohort consisting of children with occupationally active fathers in the year of pregnancy of his spouse was constructed.
Exposure
The fetuses were considered to be exposed when both the occupational and industrial codes for construction painting were present for their mother, ie, a code starting with 1293, 4593, 4693, or 4695 in NYSTGR; 1223, 1313, 7141, or 9313 in DISCO-88; 1323, 71311, or 9313 in DISCO-08, and at the same time 50150 in DB77; 454410 in DB93 and DB03; or 433410 in DB07 (table A, www.sjweh.fi/data_repository.php). The exposed group included children of self-employed, skilled, and unskilled construction painters working with painting in the construction industry. We did not include children of industrial spray painters and artists working with paints. Unexposed children had a mother working in any other occupation.
Outcome
The outcome was congenital malformations diagnosed by hospital physicians after birth. We excluded diagnoses coded as referral diagnoses as these are provisional diagnoses. The hospital admission date was applied as the date of diagnosis. The outcome “any malformation” was a diagnosis coded with Q00.0-Q89.9 in ICD-10 or equivalent in ICD-8 and included all malformations except chromosomal aberrations. Organ-specific outcomes were malformations ordered by organ system according to ICD-10’s classification (table B, www.sjweh.fi/data_repository.php). We only included results for those organ-specific groups for which an odds ratio (OR) of 2 could be detected with 80% power (5% α-level) calculated by the POWER procedure in the statistical software package SAS version 9.3 (IBM, Armonk NY, USA). The included groups were circulatory, genital, musculoskeletal, and other malformations. We added renal malformations as an increased risk has been reported for women exposed to paint fumes in their home (11). A child with malformations in more than one organ-group was included in each analysis of the relevant organ-groups. The European Surveillance of Congenital Anomalies (EUROCAT) recommends exclusion of all minor anomalies, described as malformations with lesser medical, functional, or cosmetic consequences (17). From an occupational health perspective, it is unreasonable to neglect even small anomalies if these are possible effects of occupational exposures. In concordance with Hjortebjerg et al (11), we did, however, exclude diagnoses that are unlikely to be caused by teratogenic agents and transient conditions that disappear shortly after birth. The exclusions were: pyloric stenosis (Q40.0 in ICD-10 and 75.019 in ICD-8), plagiocephaly (Q67.3 in ICD-10), torticollis (Q68.0 in ICD-10 and 75.681 in ICD-8), and macrocephaly (Q75.3 in ICD-10), which occur during or after birth; short tongue tie (Q38.1 in ICD-10) and hypoplasia of umbilical artery (Q27.0 in ICD-10 and 74.759 in ICD-8), which are not defined as congenital anomalies; and hiatus hernia (Q40.1 in ICD-10), tracheomalacia (C32.0 in ICD-10), and laryngomalacia (Q31.4 and DQ31.5 in ICD-10), which are transient conditions that disappear shortly after birth.
Data analysis
The main analysis focused on maternal exposure at the time of pregnancy and congenital malformations diagnosed within the first year of life. Prevalence OR with 95% confidence intervals (95% CI) were estimated using multiple logistic regression analysis to compare the prevalence of malformations overall and in organ-specific groups in children of construction painters with children of women in other occupations. We performed crude analyses and analyses adjusted for a priori defined potential confounders. These were birth decades (1980–1989, 1990–1999, and 2000–2010), maternal age (difference between birth year of the mother and her child: <25, 25–29, 30–34, and ≥35 years) and geographical region (the counties of Copenhagen, Frederiksborg, Roskilde, Western Zealand, Storstrøm, Bornholm, Funen, Southern Jutland, Ribe, Vejle, Ringkøbing, Aarhus, Viborg, Northern Jutland, and the combined municipalities of Copenhagen and Frederiksberg). The missing values for covariates were included in the analyses as separate categories.
Supplementary analyses
Additional analyses were made to test the robustness of the main findings and compare the effect of paternal exposure. We made sensitivity analyses with restriction to severe malformations (table C, www.sjweh.fi/data_repository.php) according to Irgens et al’s classification (18), to children of maternal painters with a minimum of two years of pre-pregnancy exposure and firstborn children. Moreover, we used maternal healthcare assistants and kitchen workers as two specific reference groups (table A, www.sjweh.fi/data_repository.php). Furthermore, we made an analysis with diagnoses registered up to the age of ten in the subcohort of children born 1980–2001. Within this cohort, the risk of cryptorchidism (75.21 in ICD-8 and Q53 in ICD-10) among boys was investigated, as this condition generally requires a longer follow-up. We made analyses stratified by maternal age, birth year, and sex of the child. Lastly, we made overall and organ-specific analyses concerning paternal exposure as a construction painter. These analyses were additionally adjusted for paternal age (<25, 25–29, 30–34, and ≥35 years). All analyses were performed in SAS statistical software version 9.3.
Results
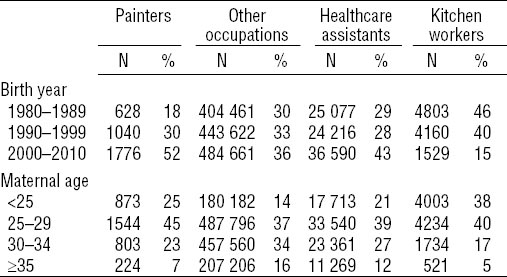
From a total of 1 930 397 potentially eligible children, 13 128 emigrated before the age of one and 64 346 were not singleton births. Of the remaining 1 852 923 children, 1 336 188 (72%) were born to 807 568 occupationally active women and were thus included in the maternal study cohort. Of these, 3444 were born to 2434 female construction painters. Within the first year of life, the time to diagnosis of malformations in our study was distributed with a median of 0 days among children of both female construction painters and other occupationally active women with an interquartile range of 0–32 days and 0–56 days in the exposure group and the reference group, respectively. The paternal cohort included 1 522 040 children with 870 925 occupationally active fathers, where 5945 male construction painters had 9003 children. The distribution of the children in the maternal and paternal cohort according to birth year and parental age is shown in Table 1 and supplementary table D (www.sjweh.fi/data_repository.php), respectively. Children of maternal painters were to a larger extent born in the 2000s and had younger mothers than children of mothers in other occupations.
Table 1
Characteristics of children with occupationally active mothers according to maternal occupation
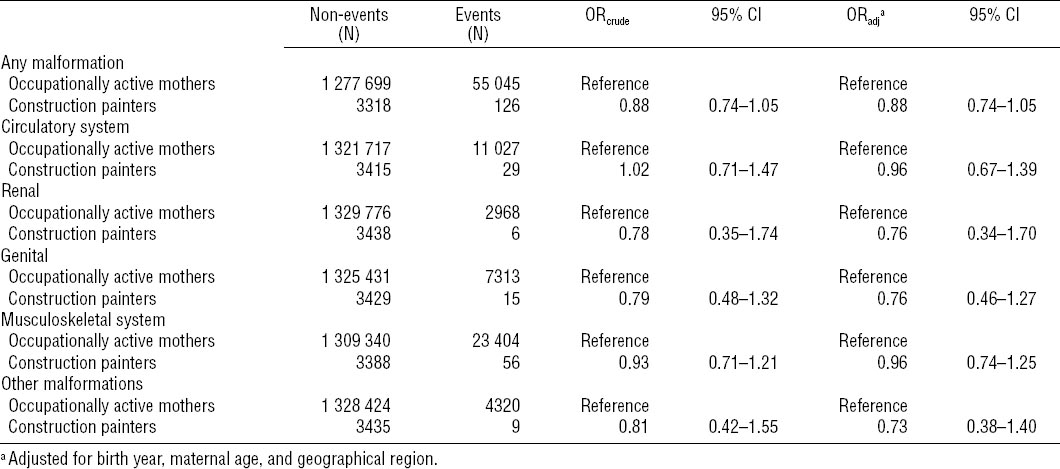
Congenital malformations
Of the children in the maternal cohort, 55 171 (4%) were diagnosed with at least one malformation within the first year (table 2). Of these, 126 children had mothers working as construction painters at the time of pregnancy. This corresponded to an OR of 0.88 (95% CI 0.74–1.05) for malformations among children of maternal construction painters compared to women in all other occupations. The risk of malformations was not significantly associated with exposure as painter in any of the organ-specific groups, and the upper limits of the 95% CI stayed <1.70.
Supplementary analyses
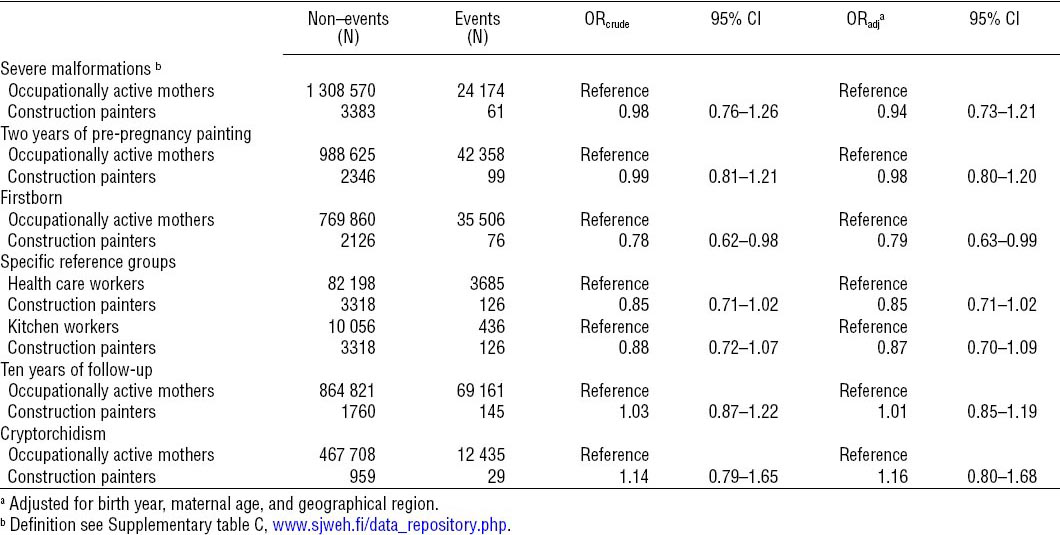
For severe malformations (24 235 events), the OR was 0.94 (95% CI 0.73–1.21) (table 3). When the analysis was restricted to firstborns, the risk of malformations among children of female painters was statistically significantly lower than mothers in other occupations: OR 0.79 (95% CI 0.63–0.99) (table 3). In the analyses with the alternative reference groups, the OR of malformations among children of female painters were 0.85 (95% CI 0.71–1.02) and 0.87 (95% CI 0.70–1.09) compared to healthcare assistants and kitchen workers, respectively. Of the 481 131 boys, 12 464 (3%) were diagnosed with cryptorchidism before the age of 10 and the OR was 1.16 (95% CI 0.80–1.68) when boys of maternal construction painters (29 cases) were compared to boys of mothers in other occupations. Results of the analysis with a strengthened exposure definition, including children of women with ≥2 years of pre-pregnancy painting, and the analysis with an extended time window for diagnosis to 10 years are shown in table 3. The results of the analyses stratified by maternal age, birth year, and child’s sex are shown in table E (www.sjweh.fi/data_repository.php), and we did not find results that suggested an increased risk among children of maternal construction painters relative to other occupationally active mothers for any of these covariates or substrata.
Table 3
Association between congenital malformations and maternal occupation restricted to firstborn, severe malformations, longer exposure, 10 years of follow-up and cryptorchidism. [OR=odds ratio; ORadj=adjusted OR; 95% CI=95% confidence interval.]
When focusing on occupationally active fathers, 62 929 children (including 401 exposed) were diagnosed within the first year of life (OR=1.06, 95% CI 0.96–1.18) (table F, www.sjweh.fi/data_repository.php). Again, no significant associations were found overall or in specific groups of circulatory, renal, genital, musculoskeletal, and other malformations.
Discussion
Our nationwide register study of congenital malformations revealed no increased risk among children of male or female construction painters, either overall or in organ-specific groups. Our results contrast with Hjortebjerg et al’s finding of increased risk of renal malformations (OR 2.16, 95% CI 1.02–4.58) among children of pregnant women who, based on antenatally collected information, were domestically exposed to paint fumes in the first trimester from 2001–2003 (11). To our knowledge, this is the first study where the risk of congenital malformations in relation to occupational painting has been investigated by a register-based approach. Some previous studies have focused on maternal exposure to volatile organic compounds (VOC) and have shown an increased risk of congenital anomalies among the children (19–21).
In Denmark, the paint used for professional construction painting is regulated by the Danish Working Environment Authority (WEA). From 1982, all paint products have been code numbered (MAL code). Codes provide the painters with immediate information as to the contents of concern, such as organic solvents. In addition, executive orders on work with code-numbered products have been published and include legislation on the use of personal protective equipment (22, 23). According to newer WEA guidelines for pregnant painters, exposure to solvents during a working day should not exceed 1/10 of the established Danish threshold limit values (24). This specific recommendation did however not apply in the earlier versions of the guideline (25). Specifically for painters, the Danish Painters’ Occupational Health Service has undertaken a massive work in making recommendations for pregnant construction painters as to which paints are prohibited, and which can be used under specific conditions. The chemicals of concern for pregnant painters are primarily VOC, coalescing agents/co-solvents, some metals, and plasticizers (2, 7). In Denmark, the substitution of VOC (eg, white spirits in paints for interior walls) with water started in the 1970s (1). White spirits (and benzene as part of white spirits) were probably present until the mid-1980s in paint for interior wood frames (Hansen, MK, Danish Painters Occupational Health Service, Copenhagen, Denmark, personal communication, 4 November 2014). Also, teratogenic glycol ethers (eg, ethyl glycol) and formaldehyde could be found in paint until the mid-1980s. These have, however, been phased out almost completely by now. Earlier, lead was also used in paint but was phased out during the 1970s with the exception of its use as siccative in paint until the mid-1990s. Even in present day, manual removal of old paint from windows may cause exposure. Chromium and cadmium were used in industrial but not construction paint. The use of phthalates (especially the teratogenic DEHP) has decreased in paints since the mid-1980s, but they are still present in sealants.
Due to the compositional change of paint during the study period from 1980–2010, it was suspected that exposure to paints in the 1980s might be more deleterious to reproduction than exposure in more recent years. To examine possible calendar time specific effects, we stratified by decade. However, we found no support for the notion that children born in the 1980s of maternal construction painters had a higher relative risk of congenital malformations than children born in the 1990s or 2000s.
Unexpectedly, we found a statistically significantly lower risk among the firstborns of maternal construction painters. This restricted analysis was made because birth order can be a predictor for the outcome if the firstborns generally experience a longer postnatal hospital stay and are examined more thoroughly (26). Insufficient control of maternal age could be an explanatory factor for our finding. The average age of maternal painters was lower than that of mothers in other occupations. But young maternal age is not associated with reduced risk of non-chromosomal malformations. Studies have shown that the risk of non-chromosomal malformations is higher among mothers with lower maternal age (<20 years) (27).
Another factor that could affect the estimates is the threshold for contacting the healthcare system in different social groups. Søndergaard et al (28) found that participation in the preventive child healthcare examinations in Denmark is lower among the socioeconomically deprived part of the population. Consequently, a delayed diagnosis of children born to maternal painters would explain the seemingly lower risk of congenital malformations in the analysis of firstborns. However, this does not seem to be the case. In both groups, ≥50% of the newborns with malformations were diagnosed before they left the hospital. Furthermore, a descriptive study from 2014 reports equality between parental social groups in Denmark regarding time to diagnosis of cryptorchidism (29).
We included children who died within the first year of life because congenital malformations are the leading cause of infant mortality in developed countries (30). We restricted follow-up to one year, which makes frequent minor anomalies contribute relatively less as these do not require hospital care in the first year of life. At the same time, this restriction excludes late-detected malformations such as cryptorchidism. Cryptorchidism is the most common congenital malformation with a prevalence of 1.9% of three-month-old boys in Denmark (31). We made a separate analysis for cryptorchidism in boys in the cohort with ten years of follow-up to contribute to the investigation of environmental factors (such as hormone disrupting chemicals) in the etiology of cryptorchidism (32). Our results did not suggest maternal occupational construction painting as a risk factor for cryptorchidism.
Also, paternal chemical exposures have been associated with congenital malformations (33–35). Theories involve mutagenesis and epigenetic modifications in sperm cells during the 69 days of spermatogenesis as well as teratogenesis following transmission of harmful chemicals from the seminal fluid to the female reproductive tract at sexual intercourse during pregnancy (36). We assessed the association between the father’s occupation as a construction painter and the risk of congenital malformations but found no increased risk.
Study limitations
Our exposure measure does not rely on quantitative data such as biomonitoring or exact duration or concentration of paint exposure, but solely on register data. We chose a very specific definition of construction painting, but there is a possibility of non-differential misclassification as we use annually collected data on occupation. As data on sick leave and unemployment benefits were not included, we do not know if the woman was absent from work during the critical weeks of embryogenesis.
Concerning the outcome definition, interobserver variability is of course an issue. It is likely that children born at hospitals with a low level of specialization are diagnosed less frequently and accurately than children born at university hospitals with a higher level of specialization and expertise in treating rare malformations (29). Therefore the analyses are adjusted for geographical region. Our supplementary analysis of severe malformations is also a method of diminishing misclassification of the outcome because severe malformations are less likely to be overlooked. The malformations were classified according to ICD-10. This classification is based on morphological and not etiological characteristics, though mechanistic causes of birth defects do not necessarily follow the morphological classes (37). If anything, this categorization based on morphology may bias the result towards the null. However, knowledge on the etiology of birth defects is still too limited to allow for a classification based upon etiologies.
Available data did not allow for control of potentially confounding effects of parental lifestyle habits (eg, alcohol consumption and smoking), use of medications, and preventive factors (eg, folic acid intake). If our exposed group of skilled and unskilled construction painters has more known risk factors than other occupationally active women, we might expect a higher prevalence of congenital malformations among the children of painters. A study in the Danish National Birth Cohort evaluated all major malformations and organ-specific malformations in different socio-occupational groups (38). Only respiratory malformations were correlated with low socio-occupational status of the parents and adjustment for unevenly distributed risk factors such as maternal body mass index, paternal age, parental smoking, maternal alcohol consumption, and folic acid intake did not change the estimates substantially. A Swedish study showed no association between congenital malformations and socioeconomic groups (39). Thus it seems that lack of adjustment for lifestyle factors and socioeducational background in our study could not seriously bias the results. Still, awareness of possible differences in risk factors and time to diagnosis among socioeconomic groups made us compare the maternal construction painters with reference groups (healthcare assistants and kitchen workers) of presumably comparable social and educational status. These alternative comparisons revealed results similar to those with all occupationally active mothers.
As we did not have complete data on miscarriages and stillbirths, teratothanasia was not dealt with in this study. The prevalences of malformations in stillbirths and terminations of pregnancy for fetal anomaly (TOPFA) are estimated by EUROCAT. According to EUROCAT, the prevalence of fetal deaths (stillborn from week 20) with a major anomaly fluctuated between <0.1–0.2% among all births during the study period, while the prevalence of live births with malformations fluctuated between 1.8–3.0%. This indicates that stillbirths with malformations make a small proportion of the total prevalence among all births. The prevalence of TOPFA has increased from <0.1% of births in 1980 to 0.8% in 2010. In this study, we have only evaluated the impact on live-born children, so we cannot reject a potential association between construction painting and fatal pregnancy outcomes related to malformations. A study on cases registered in United Kingdom’s fetal anomaly screening program showed no variation in the risk of detected anomalies among socioeconomic groups (40). But the rate of terminations after antenatal diagnosis of a congenital anomaly was statistically significantly lower in the most deprived compared to the least deprived group. Consequently, there was a higher rate of live-born children with anomalies in the socioeconomically deprived group. This finding does not suggest that our failure to reject the null hypothesis is due to a higher rate of TOPFA among the painters.
A theory of an inverse dose–response relationship in toxicological studies of reproductive outcomes has been suggested (41). It claims that a high exposure to toxic chemicals during pregnancy is likely to cause severe damage to the unborn child and early fetal loss (probably recognized as subfertility or infertility), whereas a low exposure is associated with congenital malformations among live born children. According to this theory, women with a high exposure to toxic chemicals may have a higher risk of early fetal loss, but – among the fitter fetuses that survived pregnancy despite the high exposure – the prevalence of malformations may actually be lower than among the children of women with a low exposure. Even though the likelihood is unknown of such inverse dose–response relationship between occupational exposure to chemicals in paint and congenital malformations, this theory might be an alternative explanation of our findings of a lower risk of congenital malformations among children born to occupational painters.
Concluding remarks
In this nationwide cohort study, we observed no increased association between maternal construction painting and congenital malformations in the children overall, in stratified analyses, or in several sensitivity analyses. Neither was a paternal exposure associated with congenital malformations. Our findings are reassuring with no indications of increased risk of congenital malformations among the children of construction painters.