Low-back pain (LBP) is a major global health problem (1) with a lifetime prevalence in developed countries of 75–84% (2). Furthermore, LBP in the working population constitutes a major cause of absenteeism in Western countries (3, 4) with serious implications for the individual, workplaces, and society (2, 5, 6). The origin of back pain is multifactorial (7), but LBP is a very important estimate of sickness absence (8), indicating that the individual worker’s perception of pain is an important element with respect to the consequence for sickness absence, regardless of the underlying pathology. LBP has also been shown to be occupationally related and therefore substantial efforts have been made to identify risk factors for LBP, particularly among blue-collars workers (9, 10) where the risk of sickness absence from LBP is higher (8).
One of the suggested significant work-related risk factors for LBP is forward bending of the trunk (11), and Murtezani et al (8) found trunk flexion among production workers to be one of the main risk factors for sickness absence due to LBP. Forward bending introduces cumulative doses of biomechanical loading of the spine and back muscles, which may induce wear and tear on the muscles and ligaments, leading to LBP (12–14). However, studies on the association between forward bending of the trunk and LBP show conflicting results (11). One reason for the conflicting results can be differences in methodology used to measure forward bending of the trunk (15). The majority of studies investigating the association between forward bending of the trunk and LBP (11) have been criticized for using self-reported measures (16, 17) or the short window of observations (18–21). Therefore, valid objective measurements using accelerometers are preferable due to higher precision (22) and possibility for longer measurement periods (23).
We recently reported that blue-collar workers with long duration of objectively measured forward bending of the trunk did not have higher likelihood of high LBP intensity (LBPi) compared to workers with short–moderate duration of forward bending among 198 blue-collar workers in Denmark (23). On the contrary, we observed that workers having short–moderate duration of forward bending had tendencies towards increased likelihood of high LBPi compared to workers with long duration of forward bending during work. The reasoning for this observed tendency could be: (i) workers with high LBPi are likely to eschew forward bending due to discomfort or pain, representing fear avoidance behavior (24, 25); (ii) workplaces or work teams may adjust the strenuous work tasks based on LBPi of the worker (26); or (iii) the healthy worker effect, increasing the risk of workers with a combination of a work implying long duration of forward bending and high LBPi to withdraw from the labor market (23).
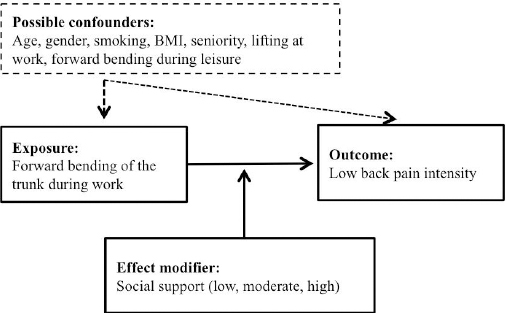
With respect to reasoning (ii), high social support from colleagues and management has been shown to be an important aspect in relation to work-related health (27). In Denmark, a rather comprehensive focus on working conditions makes it plausible that social support for workers influences the allocation of strenuous work task among the workers. If that is the case, the worker’s ability to influence how forward bending of the trunk is performed may be lower among workers with low social support compared to those with high social support, irrespective of the total duration of forward bending. In this study, we therefore hypothesized that social support would modify the association between forward bending of the trunk and LBPi (23, 28), see figure 1.
Figure 1
Illustration of the hypothesis that social support modifies the association between forward bending of the trunk during work and low-back pain intensity. [BMI=body mass index.]
The aims of this study were to investigate the association between forward bending of the trunk and LBPi among blue-collar workers in Denmark, and assess whether the level of social support modifies the association between forward bending of the trunk and LBPi.
Methods
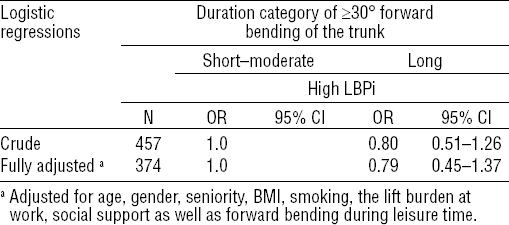
Study population and protocol
This study is based on baseline data from the field study called Danish Physical Activity Cohort with Objective Measurements (DPhacto) (29). For demographic information of the study population, see tables 1, 2 and 3. All companies gave consent for their employees to participate during working time. All workers from the included companies were given information of the aim, form, and content of the study at a pre-information meeting and invited to participate in the study voluntarily. Workers willing to participate gave their signed informed consent to measurements of anthropometric and objective diurnal measurements using accelerometers as well as completion of a questionnaire (see below). All blue-collar workers aged 18–65 were eligible for inclusion. Criteria of exclusion were plaster allergy, fever, or pregnancy. Workers with status as trainees, apprentices or canteen employees were also excluded. An overview of the flow of participants is shown in figure 2.
Table 1
Descriptive characteristics of the blue-collar workers stratified by low-back pain (LBP) intensity.
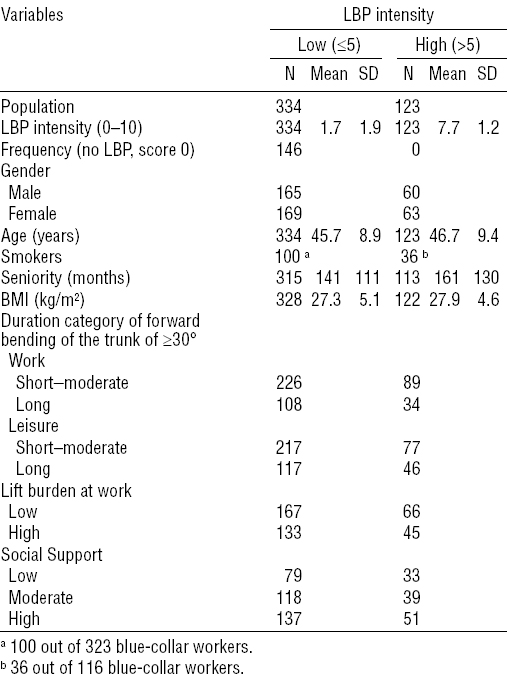
Table 2
Descriptive characteristics of the blue-collar workers stratified by the level of social support. [LBP=low-back pain.]
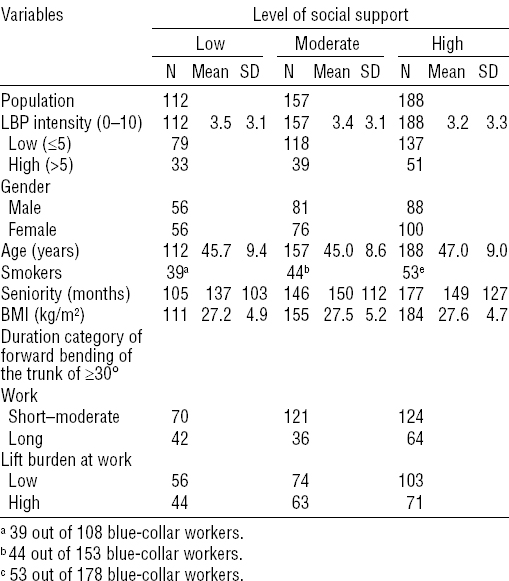
Table 3
Descriptive characteristics of the blue-collar workers (N=457) stratified by short–moderate and long duration category of ≥30° forward bending of the trunk while standing still or moving slightly during work. [SD=standard deviation.]
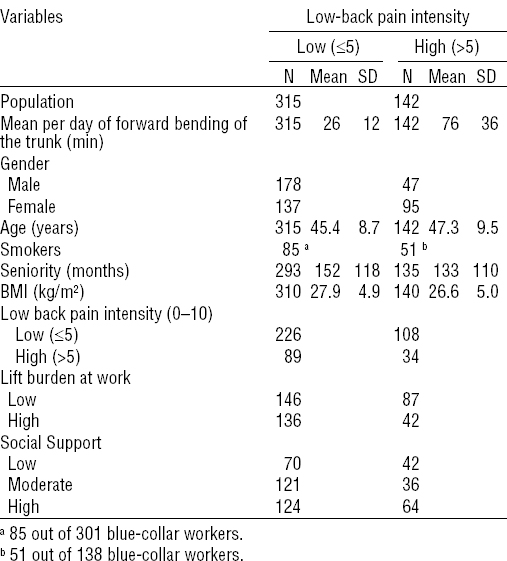
Figure 2
Flow chart containing information about study procedure, participation, inclusion, and exclusion criteria for the study population.
Data collection was conducted from December 2011 to March 2013. The Danish Data Protection Agency has accepted the handling and storage of data (29). The local Ethics Committee (H-2-2012-011) approved the study, which was conducted in accordance with the Declaration of Helsinki. The reporting of the study follows the Strengthening the Reporting of Observational studies in Epidemiology (STROBE statement) (30).
Objective measurements of types of physical activity and body positions
For measures of upper- and lower-body positions and movements, two tri-axial accelerometers (ActiGraph GT3X+, ActiGraph LLC, Pensacola, FL, USA) were mounted with the x-axis pointing downwards and y-axis and z-axis horizontally (31). The accelerometers are small, wireless, light-weighted (19 grams) and enable unobstructive recording of daily activities. The accelerometers were placed at the processus spinosus at the level of T1-T2 and at the halfway mark on the vertical line between spina illiaca anterior superior and the patella (31). If the workers experienced itching influencing their sleep, discomfort, or felt the accelerometers were interfering with their work, they were instructed to remove them. The workers filled in a diary incorporating information about working hours, leisure hours, sleep, non-wear time and specific time for the reference measurements (ie, upright stance for 15 seconds while standing still in neutral position). A Matlab-based program Acti4 (National Research Centre for the Working Environment, Copenhagen, Denmark and Federal Institute for Occupational Safety and Health, Berlin, Germany) was used to determine when the worker was standing still or moving slightly defined as a standing position, including small movement, without regular walking (23, 31).
Within the included study population, all recordings during non-working days, bedtime or sleep intervals and non-wear periods for each individual were excluded from the analysis. Non-wear periods were defined: (i) as periods of >60 minutes without any detected accelerations, (ii) as non-wear periods reported by the participant, and (iii) by visual inspection of the accelerometer data (28). We scrutinized the observed data into activities during working and leisure time. We included days with (i) ≥4 hours of recordings of working time or ≥75% of average self-reported working time, and (ii) ≥4 hours measured during leisure time or ≥75% of average self-reported leisure time per day if the worker had ≥2 days of recordings. Workers with only one day of recording were included if this comprised (i) ≥4 hours of recordings of working time and ≥75% of average self-reported working time, and (ii) ≥4 hours measured during leisure time and ≥75% of average self-reported leisure time during that specific day. This resulted in a population with objective measurements of N=657.
Forward bending of the trunk while standing still or moving slightly
Using the individual reference measurements obtained at the beginning of the recordings, the duration (minutes/day) of forward bending in the frontal and sagittal planes was computed with a cut-point of ≥30° from the individual reference point (23, 32). This cut-point was protocol-based on a previous study where different cut-points on the association between forward bending and LBPi were tested (23). Forward bending was divided into two categories representing long (upper tertile of the population with objective measurements) and short–moderate (remaining tertiles of the population with objective measurements) duration of forward bending (23). Working time was comprised of the time spent at work; leisure time was comprised of the remaining time during the working day, except when the workers were in bed at night. In all statistical analyses, only forward bending while standing or moving slightly was included to avoid including forward bending while sitting or lying.
Low-back pain intensity
The workers were asked to rate the worst intensity of LBP during the last three months on a numeric rating scale from 0–10 anchored with 0: ‘no pain’ and 10: ‘worst imaginable pain’ (33). The LBPi was then divided into two categories representing low (≤5) and high (>5) LBPi in line with previous studies (23,34). An additional categorization with no LBP (score 0) and LBP (score 1-10) was also performed.
Potential confounders
The potential confounders in this study included individual risk factors: age, gender, smoking habits, and body mass index (BMI) (35–37) as well as work-related risk factors: social support as explained below (38–41) and seniority in addition to lift burden at work (42). Moreover, forward bending of the trunk during work was adjusted for forward bending during leisure. Age and gender were obtained and crosschecked with the questionnaire. Seniority at the job and smoking habits were obtained through the questionnaire. The BMI was calculated using weight and height. The lift burden at work was established using an inquiry about the typical weight lifted at work (kg) times the duration of lifting the burden (minutes). The typical lift burden was self-reported through the question “During your workday, what is the magnitude of the mass you typically are carrying/lifting? (≥1 kg and ≥5 minutes/day)?” and then verified using dumbbells (1–5–10–15–30 kg). The self-reported time with lifting during a workday was also determined through the question “Total time spent carrying/lifting this weight on a typical working day (minutes/day)?” The lift burden variable was then stratified using a median split of the population with objective measurements.
Social support at work
Social support at work in general covers two items: social support among colleagues and from supervisors to employees (43), shown to be of importance for work-related health, satisfaction, and sick leave (27). In this study we used the Torp et al (27) approach, addressing social support at work through two questions: “Is there a good cooperation between the management and the employees?” and “Is there good cooperation between the colleagues at work?” (43, 44). Social support was then coded into a scale ranged from 0–100, with 100 representing the highest degree of social support (45). The social support scale was subsequently categorized into tertiles indicating low, moderate, and high social support. Concerning the questionnaire on social support, data were not collected in the last three companies and therefore handled as data not missing at random. The final study population for the current study was thus 457 blue-collar workers, see figure 2.
Statistical analysis
The statistical analyses were conducted in accordance with our earlier study (23), where short–moderate and long duration of forward bending during work was regressed on low and high LBPi using binary logistic regressions in a crude model as well as in a fully adjusted model with forced entry of covariates (ie, age, gender, seniority, BMI, smoking, the lift burden at work, social support and, forward bending during leisure time). Further, additional similar analyses with a categorization of no LBP (score 0) and LBP (score 1–10) were performed. To investigate if social support was associated with the duration of forward bending and LBPi, both Pearson’s Chi test on dichotomized variables and one-way analyses of variance with the continuous variables were conducted. Further, sensitivity analyses were performed to test the robustness of the main analyses: lower (ie, ≤4 on the 0–10 scale) and higher (ie, ≤6 on the 0–10 scale) cut-points for LBPi, as well as using percentage of time spent forward bending during work.
Effect modification by social support
The recommendations for analyzing and presenting effect modification by Knol and VanderWeele (46) were followed to explore whether social support modified the association between forward bending and LBPi. Binary logistic regressions with forced entry of covariates were performed for all six combined groups of forward bending and social support (ie, two categories of forward bending × three categories of social support) on LBPi. Moreover, odds ratios (OR) between forward bending and LBPi within each stratum of social support were analyzed. Finally, we tested for the interaction effect between forward bending and social support on LBPi. Further analyses for the effect modification were performed with an additional categorization of LBPi of no LBP (score 0) and LBP (score 1–10).
OR are presented with 95% confidence intervals (95% CI). Statistical significance was considered at P≤0.05. All statistical analyses were conducted using the Statistical Package for the Social Sciences (IBM Corporation SPSS statistics, Version 22.0, Armonk, NY, USA).
Results
On working days, the total measured hours of working time used for the main analyses was 8932 and 10 374 hours for work and leisure time, respectively. For work and leisure, the average recorded hours with accelerometer measurements was 19.6 [standard deviation (SD) 8.2] hours and 22.7 (SD 8.8) hours per worker, respectively. The accelerometers were on average worn for 2.6 (SD 1.0) working days. Fifty-four percent of the workers wore the accelerometers for ≥3 consecutive days (tables 1 and 2). Of the total population of workers, the cleaning sector represented 28%, manufacturing 59% and transportation 13%. In the male population, 68% worked in manufacturing, 25% in transportation, and 7% in the cleaning sector. Similarly, 50% of females were employed in manufacturing, 49% in cleaning, and 1% in transportation. The mean BMI was 27.5 (SD 4.9) kg/m2 and average age was 46.0 (SD 9.0) years, 31% were smokers and 27% reported high LBPi.
The average daily duration of forward bending was 41 (SD 32) minutes during work and 33 (SD 19) minutes during leisure time. The descriptive characteristics of workers with high LBPi compared with workers having low LBPi were similar (table 1). No significant associations between social support and the dichotomous variable of LBPi or the continuous LBPi variable (F=0.33) were observed. The descriptive characteristics did not reveal any noticeable differences for workers having long compared with short–moderate duration forward bending during work (table 3). Neither the crude nor the fully adjusted models showed any significant associations between forward bending during work and LBPi (table 4). The additional analyses on the association between forward bending and LBPi categorized into no LBP (score 0) and LBP (score 1–10) overall showed similar estimates as the main analyses (data not shown).
Table 4
Logistic regressions between duration of ≥30° of forward bending of the trunk during work and high low-back pain intensity (LBPi >5 on a scale from 0–10) among blue-collar workers. [OR=odds ratio; 95% CI=95% confidence interval.]
Furthermore, the sensitivity analyses using percentage of time spent forward bending during work showed very similar associations with LBPi as observed in the main analysis (data not shown). Accordingly, the sensitivity analyses using different cut-points for low and high LBPi (ie, ≤4 and ≤6 on the 0–10 scale) resulted in very similar estimates as observed in the main analysis (data not shown).
Effect modification by social support
Workers with low level of social support and long duration of forward bending had higher likelihood of high LBPi (OR 2.97, 95% CI 1.11–7.95) compared to workers with high level of social support and long duration of forward bending (table 5). Among workers with low social support, workers with long duration of forward bending had higher likelihood of high LBPi (OR 3.28, 95% CI 0.99–10.90) compared to workers with short–moderate duration of forward bending. Within the stratum of workers with high social support, workers with long duration of forward bending during work showed reduced likelihood of high LBPi (OR 0.39, 95% CI 0.16–0.95) compared to workers with short–moderate duration of forward bending. The interaction analyses showed a significant interaction between forward bending during work, social support, and LBPi.
Table 5
Effect modification of the duration of ≥30° forward bending of the trunk while standing still or moving slightly during work on the level of low-back pain intensity (low LBPi ≤5 and high LBPi >5 on scale from 0–10) by social support (low, moderate and high) among blue-collar workers. [OR=odds ratio; 95% CI=95% confidence interval.]
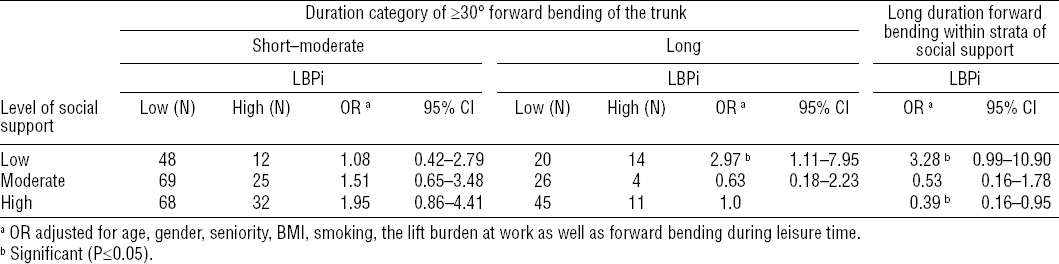
The analyses for effect modification by social support using the categorization of LBPi into no LBP (score 0) and LBP (score 1–10) revealed a similar increased OR for LBPi in the group with long duration of forward bending and low level of social support (OR 3.35, 95% CI 1.26–8.90) referencing the group with long forward bending duration and high level of social support as found for the main effect modification analyses.
Discussion
This study showed no statistically significant association between duration of forward bending of the trunk and LBPi in this cohort based on objective measurements among blue-collar workers. In line with our hypothesis, social support modified the relationship between forward bending of the trunk and LBPi. For example, workers experiencing low social support and having a long duration of forward bending during work were almost three times as likely to have high LBPi, compared to workers with high level of social support and long duration of forward bending.
Forward bending, low back pain, and social support
The lack of association between forward bending and LBPi was evident both in the crude analyses and when taking individual, lifestyle, and work-related risk factors into account. The additional analyses on the association between forward bending and LBPi categorized into no LBP (score 0) and LBP (score 1–10) supported this finding. This study therefore contradicts the general assumption that forward bending is a major work-related risk factor for LBP (11, 41). For example, a systematic review reported a moderate-to-strong relationship between forward bending during work and severe LBP (11), and forward bending for ≥ 2 hours every day during work was strongly associated with LBP in a recent prospective study (47). However, a recent review from the Swedish Council on Health Technology Assessment pointed out that there are conflicting results regarding the association between forward bending and LBP (28, 48). These conflicting results might be explained by the different cut-points used to dichotomize LBPi. However, the sensitivity analyses of our study using different cut-points for low and high LBPi (ie, ≤4 and ≤6 on the 0–10 scale) showed overall similar estimates as for the main analyses, as did applying the categorization of LBP into no LBP (score 0) and LBP (score 1–10). However, future studies should consider specifically investigating if there are cut-points for the risk of LBP from both determinants and effect modifiers. The cut-point of ≤5 and >5 of LBPi was chosen in this study due to its clinical relevance in workers’ risk for sickness absence (34).
The current study confirmed our previous findings, that there is no cross-sectional association between forward bending and LBPi among blue-collar workers in Denmark (23). Using objective measurements, our studies constitute an important contribution to the investigation of the association between work-related forward bending and LBPi because previous studies have mainly relied on self-reported measures (11). Furthermore, this study is – to our knowledge – among the first using long-term objective measurements of forward bending during longer time periods, circumventing drawbacks due to selected time windows and short recording periods (18–21).
Another important finding of this study was the observation that social support modified the association between forward bending and LBPi. Workers with the combination of long duration of forward bending and low level of social support had almost three times higher OR for high LBPi compared to workers with long duration of forward bending and high level of social support (table 5). This finding remained in the additional analyses using a different cut-point for LBPi [no LBP (score 0) versus LBP (score 1–10)].
A general concern of investigations of the psychosocial work environment and LBP is common method bias (49), in which the reporting rate of LBP is shown to be affected by the psychosocial work environment, such as low job satisfaction and other unsatisfactory aspects of work (49). However, this concern does not seem to be the case in this study because no significant associations between social support and LBPi could be found.
Other plausible explanations for our findings may be that social support from colleagues and managers can influence the workers’ needs and resources in a manner that facilitate tailoring of the work tasks to the pain state of the worker (28). This may entail that the worker’s influence on how (but not how much) forward bending is performed may be lower among workers with a low level of social support compared to those with higher levels of social support. For example, workers with higher levels of social support may perform forward bending in a manner inducing lower risk for LBP, such as having fewer long lasting uninterrupted periods of forward bending, taking breaks and rest to ensure restitution, and having a greater opportunity for variation in work tasks, compared to workers with a low level of social support. Future studies should explore the potential mechanisms between forward bending of the trunk and LBP, for example by using methods for investigating time patterns of trunk movement (eg, exposure variation analyses) among workers with different levels of social support (50).
Strengths and limitations
In this study we followed a data protocol based on our previous study (23), but this time we introduced a large sample size allowing for stratified and sub-population analyses with a statistical power that enabled adjustment for possible confounders and effect modification (29).
We have measured the duration of workers’ forward bending over several days continuously during both working and leisure hours, leaving other important aspects of the mechanical exposure, such as range of motion (51) and frequency of forward bending (52), unaddressed. This entails that our findings must be interpreted with care. One method of studying the aspects of range and frequency of ergonomic exposures like forward bending of the trunk is exposure variation analysis (EVA). EVA enables to capture the exposure variation pattern of forward bending, containing information on changes over time (53), including frequency (54), the extent of the changes (55) as well as capturing uniformity of exposure sequences (56). Implementing EVA is out of the scope for this study, but it would be of interest to implement in future studies. However, practitioners working in the occupational safety and health field often use indicators of amount of time forward bending during work to estimate exposure and risk of LBP, and therefore the impact of time duration as such is likely to be easily applicable to practitioners work. Other important factors to consider when assessing physical risk factors of LBP are occupational pushing, pulling, lifting and twisting (11, 57). Since these aspects can affect the association between forward bending and LBP, we included self-reports of occupational lift burden as confounding variables in the analyses. Factors like muscle pain tend to bias self-reported measures of physical work demands (16, 17), since workers having pain can overestimate the physical exposures, thus leading to erroneous interpretations of associations between physical exposure and pain (23). However, obtaining valid diurnal objective measures of lifting and pulling for several consecutive days in a cohort of this size is, to the authors’ knowledge, not yet feasible, leaving only self-reported measures available. It is a limitation of this study that we only use objective measures of the duration of forward bending of ≥30°. Further, we adjusted for the occupational lifting burden using self-reported measures. The interpretations of our findings should be made in light of lacking information regarding frequency and effect of the many other exposure variables that relate to forward bending.
Finally, self-reported questions on psychosocial work factors and health outcomes were used, which can be considered a limitation. Subjective measures of psychosocial factors at work increase the probability of false positive findings, that is workers experiencing problems are more likely to report certain psychosocial exposures than healthy workers (58). For example, if a worker experiences a low level of social support at work, this may induce a higher pain report compared to workers experiencing high levels of social support. This is a common source bias in cross-sectional studies with self-reported health outcomes, introducing risk of differential misclassification, and in this case an over estimation of the true modifying effect of social support. This is particularly an issue when measuring exposures and outcomes simultaneously (59). However, our data did not show any association between levels of social support and reporting of LBPi.
Social support at work in this study covered two aspects: social support among colleagues and from supervisors to employees (43). A frequently used questionnaire for addressing social support at work from colleagues and supervisors is the second version of the Copenhagen Psychosocial Questionnaire (COPsOQ II) where several questions are used to determine social support from supervisors as well as colleagues (43). In this study, two questions were used in agreement with Torp et al (27). Choosing solely two questions to establish social support may impact the accuracy and precision of the variable of social support. However, due to the comprehensive amount of questions in the DPhacto study [addressing several issues such as sociodemographic measures, lifestyle and health, musculoskeletal disorders, musculoskeletal pain-related sickness absence, productivity loss, work ability as well as perceived physical exertion during work (29)], a balance between precision of the inquired variables and the response burden on the participants was needed. Thus, this general trade-off was an inevitable limitation (43) that we acknowledge. Since the two applied questions do not provide a comprehensive measure of social support, we suggest future studies investigate the interactions between forward bending, social support, and LBP by using a full-scale questionnaire battery of social support. Finally, one should note that due to the cross-sectional study design, we cannot establish a causal relationship between forward bending and LBPi. However, prospective follow-up on frequent pain measures would be of interest.
Concluding remarks
This study indicates that there is no cross-sectional association between forward bending and LBPi in a general population of blue-collar workers in Denmark. However, social support modified the association between objectively measured forward bending and LBPi among blue-collar workers. Workers with long duration of forward bending during work and low social support were almost three times as likely to report high LBPi compared to workers with long duration of forward bending and high social support. Social support may therefore play a role in the association between duration of forward bending and LBP.



