Long-term sickness absence is an important public health issue. At the societal level, long-term sickness absence is associated with substantial economic costs related to production loss and benefit claims (1–3). For the persons afflicted, sickness absence may initially provide respite from work and time to recover from underlying health problems (4, 5). Over time, though, long-term sickness absence may lead not only to financial strain (6) but also social isolation (4), reduced self-esteem (5), decreased career opportunities (7), job loss and labor market exclusion (8, 9).
One risk factor for sickness absence is sleep problems (10–14), in particular symptoms of insomnia (15, 16). Some studies have also suggested a link between specific sleep problems, such as sleep deprivation, and reduced cognitive performance, eg, reduced learning of new tasks, slowed response times, and declined recall of working memory (17, 18). As such, sleep problems may limit employees’ functioning at the workplace by decreasing the capacity to cope with workplace demands, thus leading to an increased risk of long-term sickness absence. Sleep problems may also be a marker of other underlying health problems (19, 20), which could contribute to the association between sleep problems and long-term sickness absence.
Another risk factor for long-term sickness absence is exposure to adverse psychosocial working conditions (21–25). It is possible that the association of sleep problems with sickness absence may be exacerbated among employees with adverse psychosocial working conditions, if sleep problems do indeed decrease the capacity to cope with adverse working conditions. In other words, sleep problems, and psychosocial working conditions may interact in their associations with long-term sickness absence. If this is the case, then work modifications may be a useful strategy to reduce the risk of sickness absence among employees with sleep problems. Moreover, such interaction would also imply that workplace interventions to reduce adverse psychosocial working conditions may be particularly effective in preventing long-term sickness absence when targeted towards employees with sleep problems.
Despite this, the interplay between sleep problems and psychosocial working conditions has as yet received little research attention. To fill this gap, we set out to examine the joint associations of sleep problems and psychosocial working conditions with long-term sickness absence. Following the STROBE guidelines (26), we tested interactions as both departure from additivity and departure from multiplicativity. We focused on the following psychosocial working conditions: quantitative demands, emotional demands, influence at work, recognition form supervisor, leadership quality, social support from supervisor, and social support from colleagues. We chose these specific working conditions because they have previously shown associations with long-term sickness absence (21–23).
Methods
Data
We included survey data from the Danish Work Environment Cohort Study (DWECS 2005) and the Copenhagen Psychosocial Questionnaire study (COPSOQ II), which we merged with information on long-term sickness absence through the DREAM database, a Danish register containing weekly information on all social benefits payments since 1991 (27). Both DWECS 2005 and COPSOQ II were studies of random samples of the Danish working population conducted in 2004–2005 and contained similar measurements of selected working conditions and health-related factors. Both cohorts included new random samples and follow-up of participants who were randomly drawn at previous data waves, all of which were included in the present analyses to maximize the number of participants. Details of the cohorts are published elsewhere (28, 29).
Measurement of long-term sickness absence
The DREAM register includes all individuals with a Danish personal identification number (CPR) assigned to Danish residents at birth or migration (30), who received social benefits or transfer payments since 1991 (27). DREAM contains some 100 codes for various social transfer payments, but for the present paper we included only codes regarding sickness absence (890–899), benefits related to maternity leave (code 881), unemployment (codes 111–113, 124–126, 130–139), studying (codes 651, 652) or retirement (code 998). We used data from the years 1999–2011. In DREAM, sickness absence is recorded on a weekly basis when the employer is entitled to reimbursement of the sickness pay. During our follow-up, the period during which the employer received no reimbursement changed from 14 days of sickness absence to 15 days (April 2007) and then to 21 days (June 2008) (31). To define long-term sickness absence consistently throughout this period, we defined it as sickness absence >21 calendar days, corresponding to at ≥4 consecutive weeks in DREAM coded 890–899.
Selection of study participants
There were a total of 18 426 participants in the two studies (12 413 and 6013, respectively). We excluded participants who could not be linked with their personal identification number (N=117), who were not employed (N=5231), self-employed (N=1198), on maternity leave or sick-listed at baseline (N=313) or had missing data on key variables (N=815), yielding a total study population of 10 752 participants. Due to a high number of missing data on leadership/managerial support and social support from colleagues (N=1082), individuals with missing data on these items were not excluded but combined with the category “not relevant”, as they likely did not have relevant managers or colleagues.
Measurement of sleep problems
We measured sleep problems as a combination of self-report and national register data on purchases of prescription medication through the Danish National prescription registry (32). To measure self-reported symptoms of sleep problems, we used four items from the Karolinska Sleep Questionnaire (KSQ) (33, 34) assessing sleep quality (sleeping poorly and restlessly), initiation (difficulty going to sleep) and maintenance (waking up too early or when should be sleeping). The four items were included in the COPSOQ II questionnaire and the questionnaire used in DWECS. We defined sleep problems by indicating any of the self-reported symptoms at least “A large part of the time” (COPSOQ II) / “Most of the time” (DWECS) and/or having purchased any type of hypnotic or sedative medication (ATC code N05C) during one year prior to baseline. The KSQ has previously shown good psychometric properties (33).
Measurement of psychosocial working conditions
We measured the psychosocial working conditions quantitative demands, emotional demands, role conflict, influence, recognition from supervisor, quality of leadership, social support from supervisor, social support from colleagues using items and scales from the COPSOQ II questionnaire (28). The exact wording of each item and the scales are presented in the Appendix (www.sjweh.fi/index.php?page=data-repository). The development and validation of the COPSOQ II questionnaire is described elsewhere (28). The questionnaire has been further validated in a series of studies evaluating construct validity (35), predictive validity (21), test-retest reliability (36) and minimal important score differences (37). To construct the scales we used those items of each construct that were similar in the two studies. For some factors (influence and quality of leadership), we applied the full COPSOQ II scales but for others only reduced scales were available in both studies. All factors were operationalized identically in the two studies except role conflict, which was measured with a single item in DWECS but the full scale in COPSOQ II.
We scored each item equally spaced 1–5 with higher scores indicating higher levels of the factor and calculated a scale value by the mean of each item, if half or more items were responded to. All scales showed moderate-to-good internal consistency (Cronbach’s α=0.68–0.89). We dichotomized each scale using 3 as a cut-off point in the main analyses and conducted a sensitivity analysis where they were dichotomized by median split.
Measurement of potential confounders
We derived participant sex and age from their personal identification number (30). We measured occupational position by national register data on occupation (38), coded according to the Danish version of the International Standard Classification of Occupations version 88 (DISCO-88) (39). For the main, analysis occupational position was classified as low, intermediate or high, following the simple version of the 3-class categorization of the European Socioeconomic Classification (40, 41). In a sensitivity analysis, we included the full DISCO-coding at the 2-digit level to account for more detailed for occupational differences. We also included self-reported data on working part-time (<37 hours per week), chronic somatic illness at baseline (yes/no: diabetes, cancer, heart-disease and stroke), poor mental health (DWECS: Mental Health Inventory ≤52 points, COPSOQ II: COPSOQ depressive symptoms scale ≥9 points), and regular use of non-prescription pain medications.
Statistical analysis
We analyzed data using Cox regression to estimate how the joint exposure to sleep problems and psychosocial working conditions were associated longitudinally with the risk of long-term sickness absence. Using “weeks since questionnaire response” as the time unit, participants were followed up for five years in the DREAM register, from responding to the questionnaire until the first event of long-term sickness absence or censoring because of maternity leave, unemployment, initiating fulltime studying, retirement, migration, death or end of follow up, whichever came first. We tested the proportional hazards assumption visually by inspecting the log(-log(survival)) plots and found no indication of non-proportionality.
We tested for effect-modification by sex of the joint association between sleep problems and sickness absence for each psychosocial working condition in the Cox model (departure from multiplicativity). As we found no indication of sex-specific effects, we conducted all analyses for men and women together. All analyses were adjusted for age, sex, occupational position, working part- versus full-time, and method of data-collection (mailed questionnaire, web survey or phone) (main model). As sensitivity analyses, we further (i) examined if patterns were similar when dichotomizing the working conditions by median split, (ii) changed the cutoff point for self-reported symptoms of sleep problems in COPSOQ II to “all the time”, (iii) adjusted for self-reported chronic illness at baseline, poor mental health and regular use of non-prescription pain medications, (iv) accounted for history of long-term sickness absence (excluding participants with long-term sickness absence during 12 months prior to baseline and adjusting for long-term sickness absence during 5 years before baseline), (v) adjusted for occupation (two-digit DISCO groups), (vi) excluded participants with children <7 years in the home and (vii) excluded participants with missing data on leadership/managerial support and social support from colleagues.
To quantify any interaction between sleep problems and the psychosocial working conditions we calculated relative excess risks due to interaction (RERI, also known as interaction contrasts) (42, 43) and tested statistically for departure from additivity using Aalen’s additive hazards modeling (44) using the R package timereg (45). Although we present tests regarding interaction both as departure from additivity and departure from multiplicativity, as recommended by STROBE (26), we base our conclusions regarding interaction on departure from additivity as this is particularly relevant from the clinical and public health perspectives (26, 42, 46, 47). All statistical models accounted for clustering of data within each original study by inserting study as a strata variable in the Cox models and as a cluster variable in the Aalen models.
Results
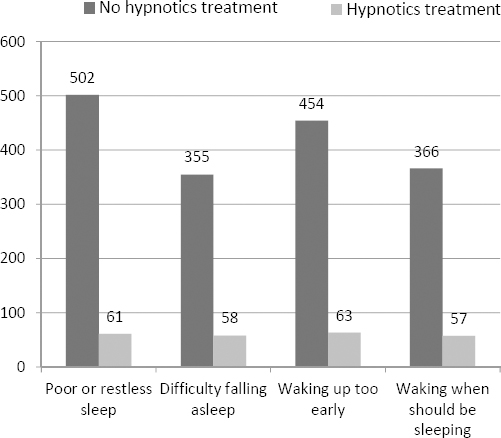
Table 1 shows the characteristics of the study population and the distribution of the examined psychosocial working conditions in relation to sleep problems. Slightly more participants were women (52%) than men, and the mean age was 43 years. During the mean of 195 weeks of follow-up (3.8 years), we identified 2313 (22%) participants with an episode of long-term sickness absence. A total of 1247 (12%) participants were defined as having sleep problems. Figure 1 shows the prevalence of self-reported symptoms and hypnotics purchases among those participants.
Table 1
Participant characteristicsa, b and joint distributions of sleep problems and psychosocial working conditions.
Figure 1
Number of participants with sleep problems in relation to self-reported symptoms and hypnotics treatment.
Sleep problems were associated with an increased risk of long-term sickness absence (HR 1.54, 95% CI 1.38–1.73). Table 2 presents the joint associations of sleep problems and psychosocial working conditions with long-term sickness absence. Quantitative demands at work modified the association between sleep problems and sickness absence with a stronger association between sleep problems and sickness absence among employees with higher quantitative demands at work. Compared to employees without sleep problems and low quantitative demands, the HR for sickness absence was 1.41 (95% CI 1.21–1.64) for employees with sleep problems and low quantitative demands whereas it was 1.77 (95% CI 1.51–2.06) for those with sleep problems and high quantitative demands. Supervisor recognition buffered the association between sleep problems and sickness absence with a HR of 1.54 (95% CI 1.33–1.80) and 1.30 (95% CI 1.10–1.54) for employees with low and high supervisor recognition, respectively. High supervisor social support, on the other hand, was associated with a decreased risk of long-term sickness absence only among employees without sleep problems.
Table 2
Time to first long term sickness absence in relation to sleep problems and psychosocial working conditions. [HR=hazard ratio; 95% CI=95% confidence interval; RERI=relative excess risk due to interaction.]
Sensitivity analyses
When we re-analyzed the data dichotomizing the working conditions by median split, results were similar to those presented except for quality of leadership, which now showed a statistically non-significant tendency towards buffering (RERI=-0.2142, full results available on request). Results were also similar when changing the cut-off point for self-reported symptoms of sleep problems in COPSOQ II, after adjusting for occupation or excluding participants with either children <7 years at home or missing data on leadership/managerial support and social support from colleagues (results available on request). The pattern of the joint associations were similar when adjusting for poor chronic somatic illness, poor mental health and regular use of non-prescription pain medications at baseline, or accounting for history of long term sickness absence (table 3). There was some indication, though, that the association between sleep problems and long-term sickness absence in the context of good psychosocial working conditions was attenuated when adjusting for these indicators of baseline somatic and mental health.
Table 3
Time to first long-term sickness absence in relation to sleep problems and psychosocial working conditions, with additional adjustments and exclusions. [HR=hazard ratio; 95% CI=95% confidence interval; RERI=relative excess risk due to interaction]
| Low | High | RERI | |||
|---|---|---|---|---|---|
|
|
|
||||
| HR | 95% CI | HR | 95% CI | ||
| Quantitative demandsa | |||||
| No sleep problems | 1 | reference | 1.00 | 0.91–1.10 | |
| Sleep problems | 1.20 | 1.02–1.41 | 1.49 | 1.26–1.75 | 0.2856 |
| Emotional demandsa | |||||
| No sleep problems | 1 | reference | 1.37 | 1.23–1.52 | |
| Sleep problems | 1.40 | 1.21–1.62 | 1.53 | 1.27–1.83 | –0.2455 |
| Role conflicta | |||||
| No sleep problems | 1 | reference | 1.11 | 1.01–1.23 | |
| Sleep problems | 1.29 | 1.11–1.51 | 1.48 | 1.25–1.76 | 0.0775 |
| Influencea | |||||
| No sleep problems | 1 | reference | 0.90 | 0.83–0.99 | |
| Sleep problem | 1.25 | 1.07–1.45 | 1.29 | 1.08–1.54 | 0.1362 |
| Recognition from supervisora | |||||
| No sleep problems | 1 | reference | 0.89 | 0.81–0.98 | |
| Sleep problem | 1.32 | 1.13–1.55 | 1.15 | 0.97–1.37 | –0.0670 |
| Quality of leadershipa | |||||
| No sleep problems | 1 | reference | 0.90 | 0.81–0.99 | |
| Sleep problem | 1.25 | 1.06–1.47 | 1.25 | 1.04–1.50 | 0.0952 |
| Social support from supervisora | |||||
| No sleep problems | 1 | reference | 0.85 | 0.77–0.94 | |
| Sleep problem | 1.11 | 0.92–1.35 | 1.23 | 1.05–1.46 | 0.2652 |
| Social support from colleaguesa | |||||
| No sleep problems | 1 | reference | 0.95 | 0.86–1.06 | |
| Sleep problem | 1.16 | 0.95–1.42 | 1.34 | 1.15–1.58 | 0.2321 |
| Quantitative demandsb | |||||
| No sleep problems | 1 | reference | 1.03 | 0.93–1.14 | |
| Sleep problems | 1.28 | 1.08–1.52 | 1.74 | 1.46–2.06 | 0.4266 |
| Emotional demandsb | |||||
| No sleep problems | 1 | reference | 1.41 | 1.26–1.58 | |
| Sleep problems | 1.52 | 1.30–1.77 | 1.72 | 1.42–2.08 | –0.2141 |
| Role conflictb | |||||
| No sleep problems | 1 | reference | 1.19 | 1.07–1.31 | |
| Sleep problems | 1.44 | 1.22–1.70 | 1.67 | 1.40–1.99 | 0.0459 |
| Influenceb | |||||
| No sleep problems | 1 | reference | 0.88 | 0.80–0.97 | |
| Sleep problem | 1.34 | 1.14–1.57 | 1.42 | 1.18–1.71 | 0.2050 |
| Recognition from supervisorb | |||||
| No sleep problems | 1 | reference | 0.88 | 0.79–0.97 | |
| Sleep problem | 1.43 | 1.21–1.69 | 1.26 | 1.05–1.52 | –0.0470 |
| Quality of leadershipb | |||||
| No sleep problems | 1 | reference | 0.84 | 0.76–0.93 | |
| Sleep problem | 1.34 | 1.12–1.59 | 1.30 | 1.07–1.57 | 0.1169 |
| Social support from supervisorb | |||||
| No sleep problems | 1 | reference | 0.81 | 0.73–0.90 | |
| Sleep problem | 1.21 | 0.98–1.48 | 1.27 | 1.06–1.51 | 0.2511 |
| Social support from colleaguesb | |||||
| No sleep problems | 1 | reference | 0.90 | 0.80–1.00 | |
| Sleep problem | 1.26 | 1.01–1.56 | 1.40 | 1.18–1.65 | 0.2428 |
Discussion
The main findings of this study were that high quantitative demands exacerbated the association of sleep problems with sickness absence whereas high supervisor recognition buffered the association. Our findings are in line with previous studies showing increased risk of long-term sickness absence in relation to either sleep problems (10–16) or adverse psychosocial working conditions (21–25). To the best of our knowledge, though, this study is the first to examine their joint associations with long-term sickness absence.
The causal mechanisms underlying the associations between sleep problems, psychosocial working conditions and sickness absence are likely complex. Risk factors for sleep problems are numerous and include age, alcohol- and caffeine intake, and obesity (19), but also occupational factors such as shift work and psychosocial working conditions (48). Furthermore, somatic and mental disorders may be associated with sleep problems (19, 20), and it is possible that the observed association between sleep problems and long-term sickness absence could be due to sleep problems being a marker of other health problems or an early marker of the development of other as yet undetected health problems. Our results regarding the patterns of the joint associations did not change when adjusting for chronic somatic illness, poor mental health, and regular use of non-prescription pain medications, indicating that the effect-modification we observed was not due to underlying illness affecting both the risk of sleep problems and the ability to cope with the adverse psychosocial working conditions. However, we did observe some attenuation of the association between sleep problems in the context of good psychosocial working conditions and sickness absence, when including these adjustments and accounting for previous long-term sickness absence. This suggests that this observed association may be partly due to sleep problems being a marker of existing health problems, and the causality of the association between sleep problems and long-term sickness absence warrants further scientific investigation in future. Regardless of the causality of such association, though, the observed interaction between sleep problems and psychosocial working conditions in their association with long-term sickness absence indicates that individuals with both sleep problems and certain psychosocial working conditions are particularly high risk groups. Workplace interventions to prevent long-term sickness absence may prove more effective when targeting this group, though such effects need to be established in future using experimental designs.
The examined psychosocial working conditions may have been related to the development of the observed sleep problems, as indicated by the higher frequency of sleep problems in participants with, eg, high compared to low quantitative demands at work (14.2 % versus 10.0%). A reverse association of sleep problems affecting the reporting of psychosocial working conditions is also possible, given previous evidence (49), and the temporality of the association between sleep problems and working conditions cannot be disentangled in the present study as they were both measured simultaneously. Any causal effects of psychosocial working conditions on both sleep problems and long-term sickness absence may be related to stress-reactions, which could be triggered by psychosocial working conditions and increase the risk of sleep problems, health problems, and consequently sickness absence (50–52). It should be noted, though, that the empirical evidence regarding the role of biological stress mechanisms in explaining associations between psychosocial working conditions and health outcomes is mixed (53–55). This potentially complex interplay between the examined factors should be kept in mind when interpreting the results. Regardless of the directionality of the associations between sleep problems and psychosocial working conditions, though, the joint exposure to these conditions seems important risk factors for long-term sickness absence.
We defined sleep problems by a combination of self-reported symptoms and data on purchases of prescribed hypnotics. We reasoned that a purchase of prescription hypnotics, and the underlying medical assessment required to obtain the prescription, suggests the presence of a sleep problem that is substantial from the patient perspective and clinically significant from the doctors’ perspective. Furthermore, we combined this data with self-reported symptoms to identify sleep problems among participants with untreated sleep problems. Based on this definition, 11.6% of the study participants had sleep problems, as indicated either by hypnotic treatment or self-reported symptoms. For comparison, a general population study from Norway found a prevalence of self-reported insomnia symptoms of 13.5% (56) and a UK study found a prevalence of clinically assessed sleep problems of 29% (57). Concerning clinically diagnosed insomnia disorders, a general population study of participants from France, the United Kingdom, Germany, Italy, Portugal, Spain and Finland found a prevalence of 6.6% (58). Because our sample comprised employed individuals only, some healthy worker selection is likely, which would result in a lower prevalence of sleep disorders in our population than in the general population. Together, though, these numbers suggest that we successfully identified individuals with marked sleep problems using the applied approach.
Regarding the role of the supervisor, we found conflicting results: the association of sleep problems with risk of sickness absence was weakened in the context of high supervisor recognition but not high supervisor social support. The items for social support, both from supervisor and colleagues, assessed the enacted aspect of social support (59), that is the amount of support the employee received (ie, how often the supervisor was willing to listen to problems at work or provided help and support to the employee). This type of social support measure is in contrast to measures of perceived availability of support, where the respondent is asked whether social support would be available if needed (59). It is possible that when assessing the enacted aspect of social support, this actually also taps into the level of problems at work the employee has, as there would be no reason for the supervisor to give social support if this was not needed. This may explain why social support did not seem to protect employees with sleep problems against long-term sickness absence, whereas supervisor recognition did.
Our results point to the importance of quantitative demands and supervisor recognition at work in preventing long-term sickness absence among employees with sleep problems. Workplace modifications might benefit such employees and reduce their risk of becoming long-term sickness absent from work. On the other hand, interventions aiming to reduce quantitative demands may be particularly effective in preventing long-term sickness absence if targeted towards employees with sleep problems. Given the observational nature of our study though, evidence from intervention studies is needed to determine causality of the relations and assess any costs and benefits from such targeted workplace modifications.
The strengths of this study include the relatively large sample size, the register-based outcome data and the application of Aalen’s additive hazards modelling to test for effect-modification on the additive scale. The sample size allowed for meaningful examination of interactions, which require large data for sufficient statistical power (60). The register-based outcome data meant that loss to follow-up was virtually evaded and the test for interaction as departure from additivity is considered particularly important from a public health perspective (26, 42, 46, 47, 61).
Some limitations of our study should be noted. We measured psychosocial working conditions and sleep problems only at a single point in time (questionnaire baseline), whereas long-term sickness absence was measured continuously throughout the 5-year register follow-up. Participants may have changed exposure levels throughout this period which might have resulted in misclassification of exposure. If this misclassification was unrelated to the exposure level – or differential so that persons with poor psychosocial working conditions or sleep problems were more likely to change exposure – such misclassification may have resulted in an underestimation of the association of these factors with long-term sickness absence. Also, we could not account for physical working conditions as this information was not included in the COPSOQ II study. We included only sickness absence of >3 weeks duration and had no information regarding the cause of the absence. Thus our results may not generalize to sickness absence of shorter duration, which may have other mechanisms (62, 63). We also do not know if the examined associations vary in relation to the cause of absence. Furthermore, it should be noted that sickness absence is a context-depending phenomenon and that sickness absence legislations vary substantially between countries (64) and over time (65). Our analysis was based on Danish data collected during 2003–2011. Since then, some changes have been implemented in the legislation, including an increase of the period during which employers get no compensation. Though we have no reason to think that these changes have impacted the external validity of our findings, any generalization of our findings outside a Danish (or Scandinavian) context should be done with caution. Further, the definition we applied to measure sleep problems was not validated against clinical data. Consequently, our results may not be applied to clinically diagnosed insomnia, whether primary or secondary.
To conclude, we found that sleep problems interacted with psychosocial working conditions in relation to the risk of long-term sickness absence. The joint exposure to sleep problems, and quantitative demands particularly, strongly predicted sickness absence, whereas high supervisor recognition appeared particularly important in decreasing risk of long-term sickness absence among employees with sleep problems. To prevent long-term sickness absence among employees with sleep problems, workplace modifications focusing on these conditions may be considered, and such interventions at the workplace level may be particularly effective if targeted towards this group. However, the costs, benefits and feasibility of such interventions need to be established in future.



