In Western society low-back pain (LBP) is a common health problem (1). A recent review estimates high worldwide prevalence of LBP and predicts a substantial increase in the coming decades globally due to the aging population (2). The causes of LBP are known to be multiple and are difficult to determine despite numerous studies (3–5).
Several physical work demands are generally well-established risk factors for LBP (6, 7), such as heavy lifting (7, 8) and forward bending of the trunk (9–11). Forward bending of the trunk is a relatively frequently occurring activity, particularly among blue-collar workers (12). Accordingly, LBP is shown to be more prevalent among blue- than white-collar workers (13). The current ergonomic exposure limits of forward bending are predominantly based on self-reported information, observations of shorter time-periods and ergonomic expert opinions (14). Because our study is among the very few existing studies with technical long-term measurements of forward bending of the back over several days (15), we think that our exposure recordings cannot be directly compared with the current ergonomic exposure limits based on different exposure measurement methods. There is a great need for additional studies with technical long-term measurements of forward bending of the back over several days in a wide variety of occupational groups in different countries in order to optimize and strengthen the documentation for occupational exposure limits for forward bending of the back
However, previous studies on the association between forward bending and LBP show varying results (11, 16), which may be the result of shortcomings in the methods used to assess both forward bending and development and aggravation of LBP (9,11,17). Most studies have used self-reported measures of the exposure, which can be biased by current pain state, causing differential misclassification (18). New methods for objective field measurements of forward bending offer an interesting opportunity to investigate the association with LBP. In this association, heavy lifting would act as potential effect modification. Another obstacle for establishing causal associations is that definitions of an LBP case differ in terms of intensity, duration and “bothersomeness” with different cut-off points and assessment methods (self-report versus clinical). Furthermore, LBP is considered to be a fluctuating condition – an episodic and typically cyclic disorder (5, 19). Therefore, a case of LBP can be difficult to define from a single time point with a long recall time (4), while frequently measured LBP may potentially capture the progress of LBP (20). Thus, reliable objective measurements of forward bending with prospective follow-up on LBP are recommended (20, 21).
In order to enable time-to-event analyses and avoid bias of the exposure, the unadjusted association between an exposure and LBP is often investigated among workers reporting no pain at baseline (22). However, with a fluctuating outcome as LBP, it is difficult to define a “pain-free” population and a pain event (23). Furthermore, exclusion of workers with pain may increase the risk for healthy worker or survivor effect, and it can be argued that inclusion may be important to investigate if forward bending aggravates LBP among workers reporting pain at baseline.
The aim of this paper was to investigate if high objectively measured daily duration of forward bending of the trunk increases the risk of development or aggravation of LBP over one year among a working blue-collar population by examining (i) the incidence rate of LBP among workers reporting no LBP at baseline, and (ii) the aggravation of LBP among workers reporting LBP at baseline.
Two hypotheses were tested: (i) high levels of objectively measured daily duration of forward bending >60° during work (FBW) increases the risk of developing LBP among workers reporting no LBP at baseline (LBP intensity=0), and (ii) high levels of FBW increases the risk for aggravation of LBP among workers reporting LBP at baseline (LBP intensity >0).
Method
Design and study population
This study is based on data from the Danish Physical Activity Cohort with Objective Measurements (DPhacto) (24). DPhacto data is collected primarily from blue-collar workers. Approximately 2100 workers were invited from 15 different companies in the manufacturing (N=9), cleaning (N=4) and transportation (N=2) sector in Denmark. Data in DPhacto was collected from April 2012 to May 2014 with 1-year follow-up for each company. The protocol of DPhacto is described in detail elsewhere (24). The Danish Ethics Committee (H-2-2012-011) approved the study and the Danish Data Protection Agency accepted data handling and storage. The study was conducted in accordance with the Declaration of Helsinki.
Data collection
All blue-collar workers were invited to participate in the study and received oral and written information about the aim, content and activities of the study prior to providing signed informed consent/non-consent. Data collection consisted of baseline measurements with questionnaire, health and physical capacity measurements, followed by 4–6 days of diurnal objective measurements of physical activities, body postures and movements. Furthermore workers were invited to participate in a 1-year monthly follow-up on LBP intensity.
Objective measurement of daily duration of forward bending of the trunk
Three accelerometers (ActiGraph GT3X+, ActiGraph, LLC, Pensacola FL, USA) were used for measurement of physical activities, FBW and forward bending of the trunk during leisure time (FBL) on working days. The ActiGraph GT3X+ is a small (19 g, 4.6 × 3.3 × 1.5 cm), wireless and waterproof triaxial accelerometer that can be worn all day and night and during water-based activities. One accelerometer was placed on the right thigh (medially between the iliac crest and the upper border of the patella) and one on the hip (near the upper point of the iliac crest) to measure physical activities (eg, walking, running, cycling and rowing) and body postures (eg, standing, sitting and lying). The third accelerometer was placed on the upper back (at processus spinosus below T1) to capture the inclination of the trunk, as a measure of the forward bending. The accelerometers were attached directly to the skin with a layer of Fixomull (Fixomull BSN medical GmbH, Hamburg, Germany) to protect the skin, double-sited tape (3M, Hair-Set, St. Paul, MN, USA) to properly place the accelerometers and Flexifix (OpSite Flexifix, Smith & Nephew, London, UK) to finally fix and ensure the right position throughout the entire measurement. Workers were instructed to (i) remove the accelerometers and tape if experiencing excruciating discomfort affecting sleep or daily activities and (ii) keep a diary, noting the time for work, leisure, sleep, non-wear periods and a daily reference measurement of 15 seconds of upright stance. Working, leisure, and wakening time (work + leisure time) were assessed from the diary.
The manufacturer’s software ActiLife (version 5.5, ActiGraph LLC, Pensacola FL, USA) was used for initialization and download of data. For all further analyses, a custom-made MatLab-based software [Acti4, The National Research Centre for the Working Environment, Copenhagen, Denmark (25)] was used to determine physical activity types, body postures and inclination of the trunk. The Acti4 software is described in details elsewhere (25). The Acti4 software has been validated in a number of studies of movement of the arm and upper body, and step count and frequency in walking and running in semi-standardized settings. All studies were evaluated with high sensitivity of ≥95% and specificity ≥93% for detecting physical activity types and body postures (25–27). Furthermore, a number of studies (28) have validated the software for various activity types, eg, sitting, standing and walking, in free-living conditions.
In this study, forward bending is defined as the daily duration (minutes/day) of inclination of the trunk while standing or moving slightly (ie, not while sitting, walking, cycling etc.) and covers the mean of the daily duration over the measured days. We considered three different degrees of FBW based on previously used cut-off points of inclination (11, 29–31). In addition to the pre-specified FBW with daily duration of trunk inclination >60°, we considered FBW >30° and FBW >90°. Acti4 has proven valid in detecting inclination of the trunk of >30°, >60° and >90° with the accelerometer placed on the upper back (26).
Baseline and prospective assessments of LBP intensity
LBP intensity was measured with a modified version of the standardized Nordic Questionnaire for the Analysis of Musculoskeletal Symptoms (32). At baseline, workers were asked “On a scale of 0–10, grade the worst pain you have experienced in your lower back within the past three months (0=no pain, 10=worst possible pain)” in a structured self-administered questionnaire.
During the follow-up, workers were asked “On a scale of 0–10, grade the worst pain you have experienced in your lower back within the past month? (0=no pain, 10=worst possible pain)” posed by text messages every four weeks over a 1-year period (14 times in total). Text messages were send on Sundays, with a reminder on Monday, and, if still not answered, a personal follow-up by a telephone call the following week was performed.
The internet-based software “SMS-Track®” (https://sms-track.com) was used to distribute and collect LBP assessments.
Baseline measurements
A structured, self-administered questionnaire contained information on sociodemographic factors (eg, age and gender) and working conditions (eg, seniority and lift factor at work) (33). The lift factor at work described the self-reported magnitude (kg) and duration (minutes per workday) of the weight typically lifted at work. Body mass index (BMI, kg/m2) was calculated based on measurements of height (Seca model 123, Birmingham, UK) and weight (TANITA Segmental Body Composition Analyzer model BC418 MA, TANITA Corporation, Tokyo, Japan).
Inclusion criteria
All blue-collar workers who provided baseline assessment of the LBP intensity covering the past three months, objectively measured daily duration of forward bending during work, and participated in prospective monthly follow-up on LBP were included in the study.
Statistical analyses
Two prespecified primary hypotheses were tested as specified in the DPhacto protocol (24).
In the first hypothesis stating that “high levels of objectively measured FBW >60° increases the risk of developing LBP among workers reporting no LBP at baseline (LBP intensity=0)”, we analyzed the LBP incidence rate using Cox’s proportional hazards model applied to grouped survival data (34). Time since baseline was used as the time scale, and the workers were censored at the first missing value of the monthly LBP measurement during the follow-up.
In the second hypothesis stating that “high levels of objectively measured FBW >60° increases the risk for aggravation of LBP among workers reporting LBP at baseline (LBP intensity >0)”, we analyzed the aggravation of LBP using a mixed-model for repeated measurements (MMRM) approach. The MMRM analysis was based on the 14 monthly reported assessments of LBP intensity, and considered the change in LBP from baseline with the effect of the daily duration of FBW. The model included a full 2-way interaction of baseline LBP intensity over the past three months and time point in follow-up, using the observed cases and an unstructured variance-covariance matrix.
The analyses of the two hypotheses were conducted in several steps. First the protocol pre-specified analysis (24) investigated the association between the daily duration of FBW >60° and LBP among workers with forward bending >5 minutes per day (N=463), assuming a linear association. The 5-minute cut-off point was pre-defined in the protocol paper as we believed that there would be no increased risk for LBP for increased forward bending of the trunk <5 minutes a day. Secondly, the assumption of linearity was evaluated using linear splines as pre-specified in the protocol paper. A linear spline is linear between knots but allows the slope to change at the knots. Knots were placed at durations of 7.5, 10 and 15 minutes of forward bending for both hypotheses to obtain similar amounts of statistical information in all intervals. We investigated whether we could include workers with an exposure of <5 minutes of forward bending >60° and assume a linear association across the complete range of exposure, by considering a linear spline with a single knot at 5 minutes of duration.
The main analyses of both hypotheses investigated the association between LBP and the daily duration of FBW >60° in the relevant subset of the complete population (N=682).
Four secondary analyses were used to further investigate the association between LBP and forward bending. First, we looked at the domain specific exposure (ie, during work and during leisure) and analyzed the mutually adjusted associations of LBP with FBW >60° and FBL >60°, respectively. We estimated the association between LBP and the total daily duration of forward bending during wakening hours (working hours + leisure time). Secondly, we investigated the associations of LBP with duration of forward bending using different cut-off points (ie, >30° and >90°) for degree of forward bending. Third, we investigated whether the association between LBP and forward bending >60° measured at baseline changed with time since the measurement of the exposure, considering the time intervals; the 1st month, the 2nd–3rd month, the 4–6th month and 7–12th month. For the analyses of the LBP incidence rate, this is an evaluation of the assumption of proportional hazards; for analyses of aggravation of LBP, this is an evaluation of a potential interaction between exposure and the time since measurement.
Finally, the main analysis model was applied to a reduced population based on criteria for sufficient amount of measured working time, due to the risk that workers with short durations of valid measurements could be a selected population. Therefore, we generated a population including only workers with ≥4 hours of measurements or measured for ≥75% of the working time registered in the diary (N=644). The choice of criteria is based on previous studies among similar populations and with identical measurements (12,35,36).
One worker was identified as an outlier in the exposure measurements based on an abnormally large measured duration of forward bending of 324 minutes compared to the remaining study population, which varied between 0–58 minutes. This worker was excluded from all analyses.
All statistical analyses were conducted using SAS version 9.3 (SAS Institute, Cary NC, USA) for the Windows platform.
Results
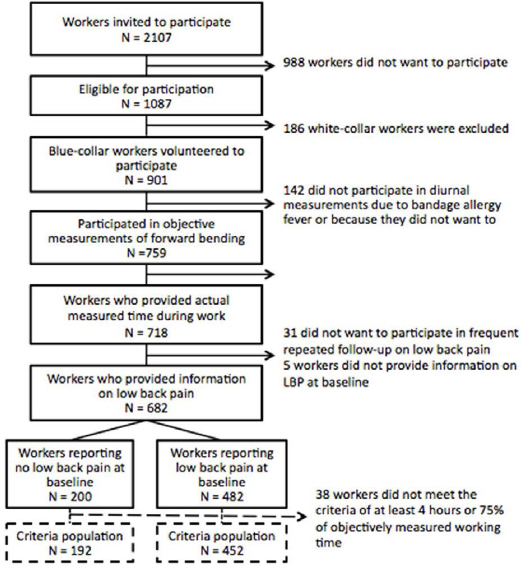
Initially, 2107 workers were invited from 15 different companies in the manufacturing, cleaning and transportation sector in Denmark. Of the 901 blue-collar workers eligible for participation, 682 provided objectively measured FBW and participated in the follow-up on LBP. At baseline, 200 workers reported no LBP in the past three months (LBP intensity=0) and were included in the investigation of the LBP incidence rate. The remaining 482 workers reported LBP intensity >0 in the past three months and were included in the investigation of aggravation of LBP analyzed with MMRM. The criteria-based population of workers with ≥4 hours or ≥75% of reported working time measured included 192 and 452 workers in the two subpopulations, respectively (figure 1).
Figure 1
Diagram illustrating the flow of participants in the study, and the division of the population into workers reporting no or some low-back pain (LBP) at baseline.
In total, workers were measured on working days for 15 647 and 18 262 hours of working and leisure time (without sleeping hours), respectively. FBW >60° ranged between 0–58 minutes per day.
Table 1 presents the descriptive characteristics of the workers divided into groups with workers reporting no or some LBP at baseline. No notable difference was seen in daily duration of FBW and FBL between the two groups. The groups of workers were also similar according to age, gender distribution, seniority, BMI and leisure-time physical activity. The reported magnitude (kg) and duration (minutes/day) of lifting burden at work were slightly lower among workers reporting no LBP at baseline compared to workers reporting LBP at baseline.
Table 1
Descriptive characteristics of the DPhacto study population stratified according to workers reporting no low-back pain (LBP) at baseline (LBP intensity=0 on a scale from 0–10) and workers reporting LBP at baseline (LBP intensity >0 on a scale from 0–10), respectively. [FBW=forward bending of the trunk >60° at work; FBL=forward bending of the trunk >60° during leisure time.]
The distribution of the workers’ daily duration of FBW >60° stratified on baseline LBP intensity is presented in figure 2, showing whether workers with higher LBP levels tend to bend forward less.
Figure 2
Box plot presenting the distribution of daily duration (minutes) of forward bending of the trunk >60° during work according to baseline low-back pain intensity during the past 3 months, in the DPhacto cohort (N=682). The boxes represent the lower and upper quartiles of the forward bending, with the median of the group marked by the horizontal line inside the box. Whiskers present the 10th and 90th percentiles, and the circles represent workers outside the 10th (bottom) and 90th (top) percentiles. N for each group of workers with 0–10 baseline low back pain intensity are presented below the x-axis of the plot.
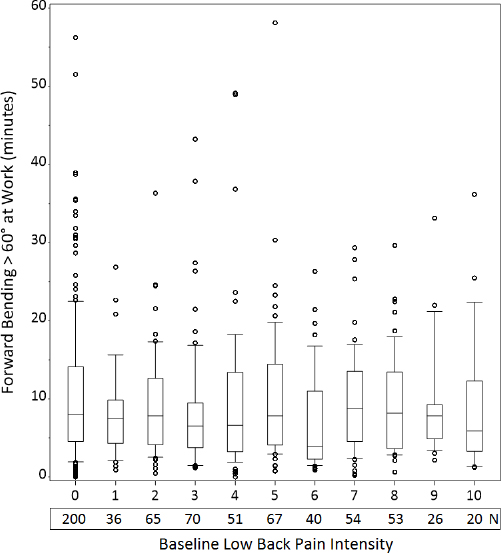
The majority of workers rate their LBP in the lower half of the 0–10 scale. The widespread of the circles above the boxes (figure 2) indicates a large variation in FBW >60°. The tight clustering of workers below the boxes disclose that a greater part of workers have a fairly low duration of FBW >60°. The median duration is fairly stable across the groups and does not indicate any systematic trend across increasing LBP ratings at baseline.
Forward bending and LBP
The prespecified analyses of the association between FBW >60° and LBP within the pre-specified population of workers with FBW >60° >5 minutes per day, showed no significant associations (table 2). The LBP incidence rate among workers reporting no LBP at baseline was decreased corresponding to a hazard ratio (HR) of 0.87 [95% confidence interval (95% CI) 0.61–1.19] per 15 minutes difference of FBW >60° (table 2). The population reporting LBP at baseline showed an insignificant aggravation of LBP of 0.18 (95% CI -0.20–0.56) on the 0–10 LBP intensity scale per 15 minutes difference of FBW >60° (table 2).
Table 2
Association between objectively measured daily duration of forward bending of the trunk at work (FBW) and low-back pain (LBP) among blue-collar workers in DPhacto. The incidence rate was evaluated among workers reporting no LBP at baseline. Aggravation was evaluated among workers reporting LBP at baseline. [HR=hazard ratio; PE=parameter estimate; 95% CI=95% confidence interval.]
| Daily duration of forward bending of the trunk | LBP incidence rate a among workers reporting no LBP at baseline (N=200) | Aggravation of LBP b among workers reporting LBP at baseline (N=482) | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| N | HR | 95% CI | P-value | N | HR | 95% CI | P-value | |
| Pre-specified population c | ||||||||
| FBW >60° (per 15 minutes) | 143 | 0.87 | 0.61–1.19 | 0.41 | 320 | 0.18 | −0.20–0.56 | 0.36 |
| Main analyses, entire population d | ||||||||
| FBW >60° (per 15 minutes) | 200 | 0.79 | 0.58–1.04 | 0.09 | 482 | 0.14 | −0.17–0.46 | 0.37 |
| Secondary analyses d | ||||||||
| Domain-specific forward bending >60° | ||||||||
| Working hours e (per 15 minutes) | 200 | 0.76 | 0.55–1.02 | 0.07 | 482 | 0.12 | −0.21–0.45 | 0.48 |
| Leisure time e (per 15 minutes) | 200 | 1.08 | 0.75–1.51 | 0.67 | 482 | 0.07 | −0.29–0.44 | 0.69 |
| Wakening hours (work + leisure; per 15 minutes) | 200 | 0.89 | 0.72–1.06 | 0.20 | 482 | 0.10 | −0.11–0.31 | 0.36 |
| Different degrees of forward bending f | ||||||||
| FBW >30° (per 15 minutes) | 200 | 0.87 | 0.78–0.97 | 0.01 | 482 | 0.07 | −0.05–0.19 | 0.24 |
| FBW >90° (per 15 minutes) | 200 | 0.73 | 0.29–1.59 | 0.45 | 482 | 0.54 | −0.30–1.38 | 0.21 |
| Criteria-based reduced population g | ||||||||
| FBW >60°(per 15 minutes) | 192 | 0.85 | 0.67–1.05 | 0.14 | 452 | 0.10 | −0.13–0.32 | 0.40 |
b Analyzed using a mixed model for repeated measurements adjusted for baseline LBP by time point interaction.
c The pre-specific population comprised workers with >5 minutes of daily duration of forward bending >60° at work (FBW>60°) (N=463).
The linearity of the associations between FBW >60° and LBP were investigated in the prespecified populations (N=143 and N=320 reporting no LBP and LBP, respectively, at baseline) using linear splines with knots at 5, 7.5, 10 and 15 minutes of FBW >60°. For both the LBP incidence rate and aggravation analyses, linearity could be assumed (LBP incidence rate: P=0.65; LBP aggravation: P=0.32, data not shown).
When including the workers with <5 minutes of FBW >60°, ie, the complete population (N=682), we found no differences between workers with <5 minutes of FBW versus those with >5 minutes regarding the association between daily duration of FBW >60° and the LBP incidence rate (P=0.27, data not shown) or the aggravation of LBP (P=0.66, data not shown).
The analyses including the entire population showed similar and insignificant results. The LBP incidence rate was decreased by HR 0.79 (95% CI 0.58–1.04) per 15 minutes difference in duration of FBW >60°, and LBP was aggravated by 0.14 (95% CI -0.17–0.46) per 15 minutes difference in duration of FBW >60°.
Domain-specific forward bending and LBP
We investigated the association of LBP with daily durations of the domain specific (work or leisure) forward bending >60°. None of the associations were significant. The LBP incidence rate was insignificantly reduced by HR 0.76 (95% CI 0.55–1.02) per 15-minute difference in duration of FBW >60° and insignificantly increased by HR 1.08 (95% CI 0.75–1.51) per 15-minute difference in duration of FBL >60° in mutually adjusted analyses (table 2). The association between the LBP incidence rate and the duration of forward bending did not depend on the domain (P=0.20, data not shown), thus the two durations could be added to a total daily duration of forward bending >60° during wakening hours. For forward bending during wakening hours (work + leisure), we found an insignificantly decreased LBP incidence rate, HR 0.89 (95% CI 0.72–1.06) per 15-minute difference in duration (table 2). The analysis of aggravation of LBP showed no significant association with FBW and FBL, with very low aggravation of LBP of 0.12 (95% CI -0.21–0.45) and 0.07 (95% CI -0.29–0.44), respectively, per 15-minute difference in forward bending, when mutually adjusted (table 2). The association between aggravation of LBP and forward bending did not depend on the domain either (P=0.88, data not shown). The association between forward bending during wakening hours and LBP showed an insignificant aggravation of LBP of 0.10 (95% CI -0.11–0.31) per 15-minute duration of total daily forward bending >60°.
Different degrees of forward bending and LBP
For the associations between LBP and the duration of FBW >30° and FBW >90°, we found similar patterns as for FBW >60°. However, the decrease in the LBP incidence rate was statistically significant for FBW >30°, HR 0.87 (95% CI 0.78–0.97), while not for FBW >90°, HR 0.73 (95% CI 0.29–1.59) (table 2). No significant association was seen in the analysis of aggravation of LBP, with an estimated effect of forward bending on aggravation of LBP of 0.07 (95% CI -0.05−0.19) for FBW >30° and 0.54 (95% CI -0.30–1.38) for FBW >90° per 15-minute difference in duration in forward bending of the trunk (table 2).
Effect of follow-up time and LBP
No signs of effect modification of follow-up time since exposure measurement was found (LBP incidence: P=0.29; LBP aggravation: P=0.96; data not shown).
Forward bending and LBP in criteria-based population
The association between FBW >60° and LBP was evaluated in the population of workers with measured time of bending forward for >4 hours or ≥75% of the working time. We found similar insignificant results as seen in the aforementioned analyses. The LBP incidence was insignificantly reduced by HR 0.85 (95% CI 0.67–1.05) per 15-minute difference in daily duration of FBW >60° and the LBP was insignificantly aggravated by 0.10 (95% CI -0.13–0.32) per 15-minute difference in daily duration of FBW >60° (table 2).
Discussion
This study consistently found no significant association between daily duration of forward bending ≤1 hour and development or aggravation of LBP. The hypotheses are therefore not supported. The main analyses showed an insignificant protective association for the workers reporting no LBP at baseline and an insignificant diminutive increase in LBP for the workers reporting LBP at baseline.
This study is based on objectively measured FBW for several consecutive days along with monthly repeated assessments of LBP. The study’s main strength is precise and valid objective measurements and prospective design with frequent follow-up. Main limitations include self-reported lifting burdens and the lack of measurement of external forces. Furthermore, the exposure in this study is regularly up to about 40 minutes of forward bending and even up to 60 minutes. The study can therefore only conclude on possible associations in this given exposure range. Strengths and limitations are elaborated conclusively in the discussion.
There may be several interpretations of our findings. We suggest three possible explanations for the results: (i) there is no association between forward bending and LBP, (ii) there is a positive association between forward bending and LBP, which is diminished for design or methodological reasons, and (iii) the association works when a third factor is present, only under specific circumstances, or in specific populations (effect modification).
Explanation (i): no association between forward bending and LBP
Even though previous studies point towards a positive association, it may actually be that forward bending is not an independent risk factor for LBP. This may be because previous studies were based mainly on self-reported exposure or cohorts without frequent follow-up. Some studies report a positive association (8, 10) but comparison with our study is highly challenged by the aforementioned different exposure measurements between studies (11, 16). A few studies support our finding of lack of association between forward bending and LBP (12, 37). The Villumsen et al study (12) also used objective measurements of forward bending but in a cross-sectional design, while Harkness et al (37) reported lack of association between self-reported forward bending and new onset of LBP among newly hired workers. Therefore, to our knowledge, this is the first prospective study of the association between objective exposure measurements of forward bending and prospectively registered LBP. Thus, the documentation for the lack of positive association between forward bending and LBP is still scarce and further investigation with convincing methodology is needed.
Explanation (ii): positive association is diminished for design or methodological reasons
For various reasons, our data may have failed to show an actually existing association between forward bending and LBP. One possibility could be the possible floor effect in our data, with a population of workers not having long enough duration of forward bending to increase the risk of LBP. To our knowledge, no previous literature with objective field measurements has established cut-off points on duration of forward bending in order to avoid an increased risk of LBP. Our population consisted of blue-collar workers who are generally considered to conduct manual work tasks involving long duration of forward bending. However, our objective data document a high variation with many workers in the lower exposure duration of forward bending.
Secondly, it could be speculated that the accumulated daily duration of forward bending in itself does not increase the risk of LBP. Instead, it could be longer continuous periods of static forward bending of longer duration or frequent repetitive short duration forward bending which increases the risk of LBP. In this paper, forward bending is analyzed as the total mean daily duration, not considering the time pattern of forward bending (eg, time of forward bending in long continuous periods). Future analyses should address the association between the time pattern of forward bending and LBP.
Explanation (iii): the association works when a third factor is present, only under specific circumstances, or in specific populations
Another possible explanation for the lack of association between forward bending and LBP in our study can be that forward bending is only a risk factor for LBP when a third factor is present, under certain co-occurring circumstances, or among certain populations. The plausibility behind the hypothesis of increased bending presenting a risk of LBP is that forward bending increases the load on the lower-back structures by an increase in the torque causing both increased disc compression and shear forces (38). This is in particular the case when bending is combined with rotation or if lifting, pushing and pulling impose an external force on the hands (8, 11). Therefore an increased risk of LBP may only be present when forward bending is combined with handling of heavy burdens or rotation of the back. Unfortunately, the objective measures in the present study could not assess a simultaneous external force or rotation of the back while forward bending.
Of note is that we excluded forward bending while sitting, to increase the likelihood that the forward bending position was performed unsupported.
Additionally, other circumstances in the work environment factors may modify the effect of forward bending on LBP. A recent cross-sectional study from the DPhacto study, found that high duration of forward bending increased the odds of LBP among workers experiencing low but not high social support at work (12). It could therefore be suggested that social support at work acts as a modifier also on the prospective association between forward bending and LBP.
Finally, individual characteristics could be speculated to modify the association as the relative loading of the back depends on the individual capacity. A high back endurance has been recognized to decrease the risk of LBP development (39). Also, effect modification could be present in this population of study, who could be considered as “healthy survivors” as workers might leave the workplace if they are unable to handle the work tasks. In this study, we investigated the step prior to including potential confounders by considering different aspects of forward bending and prospective LBP in an unadjusted association.
Strengths and limitations
One of the main strengths of this study was the precise and valid diurnal objective measurement of forward bending of the trunk over several days and the prospective design with long and frequent follow-up on LBP.
A limitation is the lack of measurement of external forces applied on the hands (eg, lifting and pulling) and rotations of the back during work. The data collection included self-reported lifting of burdens, which will be considered in future analyses of modifying factors. A possible limitation is the self-reported nature of LBP assessments. This measure is highly subjective and individually founded, but very relevant in terms of investigating the impact on the individual. Furthermore, as earlier mentioned, the healthy worker effect may be present and introduce a selection bias because the population of study may be selected due to unhealthy workers not participating because they are on sick leave or left the workforce. The low exposure to forward bending compared to findings in other populations can be seen as a limitation in external validity.
The present data cover the exposure variation over the entire workday for consecutive days. Nevertheless, the lack of the exposure variation between weeks, months and years and also seasonal changes is a limitation. More repeated whole-day measurements to cover such possible variation would be of great value in future studies.
The DPhacto dataset also allow for investigation of the kinematics of the arms during forward bending, which may be considered for future analyses. These more comprehensive analyses on the valid objective measurements are important to improve preventive initiatives for LBP in workplaces. Further studies with objective long-term field measurements are important to be able to provide recommendations and guidelines regarding forward bending and LBP. Furthermore, future investigations of other factors that may affect the association between forward bending of the trunk and the development of LBP should also consider how factors influence the association; confounding, mediation and effect modification. The theoretical causal relation should be addressed, and there will be a need for testing the exact impact on the association from the potential influencing factors.
Concluding remarks
This study is original in investigating the association between objectively measured daily duration of forward bending and the development or aggravation of LBP over one year in a working blue-collar population. In spite of thoroughly investigating forward bending at work and leisure, different degrees of forward bending, and different follow-up times of LBP, no significant associations between forward bending ≤1 hour and LBP were found.
Therefore, this study does not support a positive association between daily duration of forward bending and development or aggravation of LBP.



