The global burden of occupational injuries is enormous. The International Labor Organization (ILO) highlights that every day 6300 people die as a result of occupational accidents or work-related diseases, resulting in more than 2.3 million deaths per year. More than three million accidents occur on the job annually, with many of these resulting in extended absences from work (1). In the year 2003, China accounted for around 27% of the ILO estimated fatal accidents attributable to work (2). The estimated annual workplace fatality rate for China was 12.3 per 100 000 workers, compared to a rate of 4.9 per 100 000 workers in the United States (3). The cost of accidental occupational injuries is huge, including medical costs, disability compensation, sickness absence and poses a heavy financial burden on the employers, workers, and society in general (4).
Occupational health and safety (OHS) education or training is widely practiced as a means to reduce accidental occupational injuries. However, the contribution of training to the reduction of accidental injury rates remains uncertain (5–7). A few before-and-after comparison studies have reported that training programs could reduce accidental injury incidence rates among construction workers (8–10). However, the evidence was limited due to the absence of control groups.
Traditional OHS education and training stereotype workers as passive participants receiving new knowledge and instructions from experts, but active participation of workers has been emphasized in more recent years, especially in small and medium-sized enterprises (SME) in Asian countries (11–16). Several randomized-controlled trials (RCT) have examined whether a participatory ergonomics intervention could prevent musculoskeletal disorders/low-back and neck pain (17–19) but failed to document the effectiveness. The effects on accidental work injuries have also not been evaluated. Participatory OHS training was first introduced to mainland China in the early 2000s (14), and we found it opportune to conduct a proper evaluation of its effectiveness in preventing accidental work injuries before more widespread promotion of such a training approach. We carried out an RCT with the objectives of documenting the effectiveness of participatory OHS training in preventing accidental work injuries and comparing the effectiveness of this training approach to conventional training.
Methods
Design and study population
We conducted an RCT in Shenzhen, a large industrial city in southern China, during the period June 2008 to November 2009. We first randomized participating factories into experimental and control factories, and further randomized the selected workers in each experimental factory into an intervention and control group, respectively. The Survey Ethics Committee of the Chinese University of Hong Kong approved the study, and all participants gave informed consent before participating.
Factory recruitment
We identified eligible factories from the local factory registries. The inclusion criteria were (i) medium-sized industrial enterprise (300–2000 employees); (ii) could be matched with another factory by industry and production processes; and (iii) <30% turnover rate of workers in the year before recruitment. We then paired each eligible factory with another factory in the same industry with similar production processes and employment size. Using the above criteria, we invited 235 factories to participate and 220 factories (110 matched pairs) agreed to be included in the sampling frame (93.6% response rate). We randomly selected 30 pairs of factories for the RCT and randomly assigned (by tossing a coin) one factory from each matched pair as the experimental and control factory, respectively.
Worker selection
We recruited employees as participants from each factory using the following inclusion criteria: frontline workers and having been employed in the current factory for >12 months. We excluded employees in administration, design or logistics positions, or those who were illiterate or seasonal migrant workers. The factory managers identified about 60 workers fulfilling the inclusion/exclusion criteria in each factory and invited them to participate in the study. The sample size would allow the detection of an incidence rate difference of 5/100 with 80% power (1 – beta or Type 2 error) and a Type 1 error (alpha) of 5% using the formula (20):
N=[(Zα/2+Zβ)2×{(p1(1-p1)+(p2(1-p2))}]/(p1-p2)2
where N=sample size required in each group; p1=proportion of workers in control group with injury=0.10 (estimated from pilot study); p2=proportion of workers in intervention group with injury=0.05; Zα/2=1.96 [Z score for alpha with 2-sided test – the number of standard deviations from null hypothesis mean covering the confidence interval corresponding to alpha]; Zß=0.84 [Z score for beta – the number of standard deviations from the alternative hypothesis mean corresponding to the power (1-ß) of the study].
Based on the above formula, a sample size of 432 was required per group. Adjustments were made for an estimated 30% dropout rate and possible intra-cluster correlation (ρ) using the variance inflation factor (21) and adopting a conservative estimated ρ of 0.01.
Worker allocation
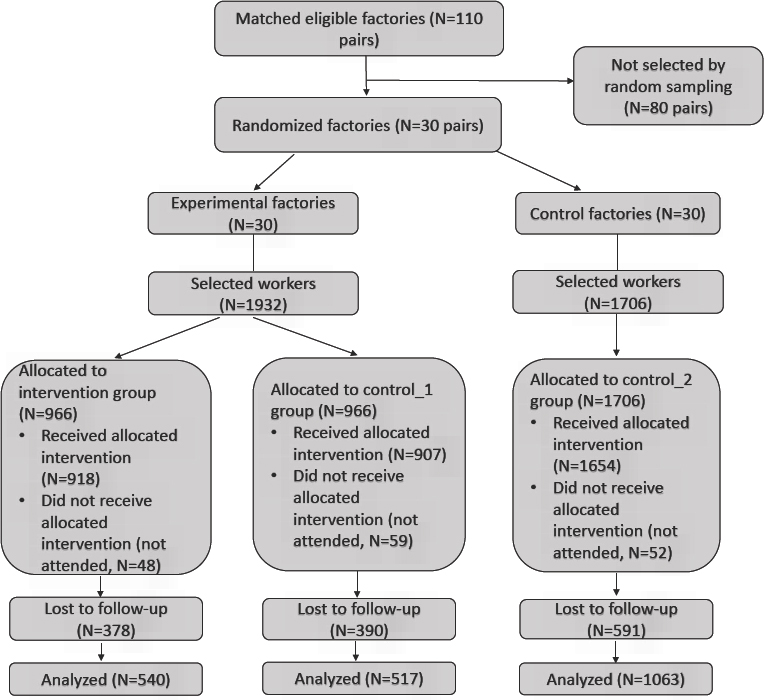
After receiving a list of workers’ names from each experimental factory, we used the randomization function of Microsoft Excel to allocate workers into either the intervention or control group (control_1 group). We then sent back the two lists of names to the factory, and the manager made arrangements for the workers to attend the randomly allocated training programs. We assigned all workers from the control factories into the control_2 group. During this period, we concealed the allocation codes from both factory managers and workers in the experimental factories. The workers were only told to attend an OHS training course, without being informed about the hypotheses of the intervention study. Management selected a total of 1932 workers in the 30 experimental factories and 1706 workers in the 30 control factories. Less than 5% in each group were unavailable on the training days. Finally 918, 907, and 1654 workers in the intervention, control_1, and control_2 groups, respectively, participated in the training sessions (figure 1).
Intervention
The workers in the intervention group received participatory training and workers in the two control groups received didactic training (representing conventional OHS training) during the period June 2008 to November 2009. We invited eight occupational health experts as instructors to conduct the training activities throughout the study. They had received relevant training on teaching methods in both participatory training and didactic training before conducting training in the 60 factories.
Participatory training
A participatory training model called “Participatory Occupational Health and Safety Improvement” (POHSI) was developed (22) referencing the original POSITIVE (Participatory Oriented Safety Improvements by Trade union InitiatiVE) training program developed by the Japan International Labor Foundation in cooperation with the Institute for Science of Labor in the 1990s (23). The POHSI training program focuses on learning good examples – solutions to OHS issues that could be achieved quickly and at low cost from other workplaces or factories and developing concrete and practical action plans on OHS improvements (22). Four main steps were involved in each training workshop: (i) The whole group (around 30 trainees) was first given a brief introduction to some basic concepts of OHS and successful examples on improving OHS in other workplaces; (ii) The large group was then divided into 3 small groups of around 10 workers to conduct a workplace inspection exercise using an action checklist (see Appendix 1, www.sjweh.fi/index.php?page=data-repository) for identifying existing good examples and the areas that need improvement; (iii) This was followed by small group discussions to agree on the list of good/successful examples and to find actions/solutions for the areas that needed improvement; (iv) The small groups reported back to the whole training group, now with the management representatives joining in, on their priority lists of action plans for improvements. Participating employees and management representatives then sorted the priorities for both immediate and long-term improvement plans.
The various large group sessions were enriched by demonstration and practice of personal protective equipment (PPE), including various forms of masks for dust and chemicals and hearing protectors, as well as stretching and strengthening exercises and games. Each participatory training workshop conducted at the experimental factory for the intervention group lasted, on average, five hours. See Appendix 2 for details, www.sjweh.fi/index.php?page=data-repository.
The contents in each training workshop in the current study covered three core areas of OHS and three elective areas. The three core areas were work station (including ergonomics and materials handling), machine safety, and working environment (including workers’ welfare). The training activities of all the factories included these contents. In addition, we chose one elective area among three (chemical safety, dust control, or noise control) for each pair of factories according to the specific industry type.
Didactic training
The training contents and materials were the same as in participatory training, covering the same four areas/topics. However, only a short presentation was given on each topic, without group discussions, games or workplace visits. Each didactic training workshop conducted at the experimental or control factories lasted on an average of two hours. See Appendix 2 for details, www.sjweh.fi/index.php?page=data-repository.
Data collection
Each participant completed a self-administered questionnaire under the guidance of a field investigator before the training sessions and then again one year after training. The questionnaire enquired information on demographic and job characteristics and accidental work-related injury events during the previous 12 months. Accidental work-related injury events referred to acute traumatic injuries at work that required medical attention or treatment or interfered with work activities. We also collected information on co-interventions, such as other training programs, health inspections, and other occupational health services, from the management in each factory during the follow-up period.
Data analysis
We used EPIData 3.1 (to set up the questionnaire and for data entry, and SPSS 16.0 (SPSS Institute, Cary, NC, USA) for Windows for subsequent data analyses. This was a cluster randomized study with the worker as the unit of analysis. We evaluated the incidence rate (IR) of accidental injury based on both the number of workers reporting injuries (person-based IR) and the number of reported injury events (event-based IR) in the intervention and control groups. We used generalized estimating equations (GEE) to compare the before/after person-based injury IR difference (24) between the intervention and two control groups by incorporating a product term (group×time), while controlling for age and sex, and considering the correlation at both the factory and individual level by including indicators for subjects and factories in the model as random effects. We used the two-proportion Z-test to compare the event-based IR before and after training in the three groups. Re-injuries were workers with injuries at baseline, a subset of all participating workers, who suffered from accidental injuries during the follow-up year. We compared the re-injury rates in the three groups using binary logistic regression with the intervention group as the reference.
Results
From June 2008 to November 2010, 3479 frontline workers in 60 factories participated in the training programs. A variety of industries were involved: 22 (37%) electronic, 8 (13%) printing, 8 (13%) toy, 6 (10%) plastic, 4 (7%) optical, 4 (7%) footwear, 4 (7%) jewelry, 2 (3%) metal products, and 2 (3%) pharmaceutical factories/companies. Details on the sociodemographic backgrounds of the participants have been reported before (25). There were no statistically significant differences in age, gender, education level, duration of employment, training experience, prior work experience, and accidental work injury history among the three groups [table 1 in ref 25]. No other training programs, health inspections, and basic occupational health services were conducted in these factories during the year after the training programs.
Table 1
Self-reported person-based incidence rates (IR) of accidental injury in the past 12 months at baseline and at one year after training in different groups. [OR=odds ratio; 95% CI=95% confidence interval.]
| Accidental Injury | Total | IR (/1000) | ORa | 95% CIa | P-value | ||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Yes | No | ||||||
| Intervention | 1.00 | ||||||
| Baseline | 82 | 836 | 918 | 89.3 | |||
| 1 year later | 28 | 509 | 537b | 52.1 | |||
| Decrease in incidence | 37.2 | 0.002 | |||||
| Control_1 | 1.78 | 1.04–3.04 | |||||
| Baseline | 67 | 840 | 907 | 73.9 | |||
| 1 year later | 37 | 480 | 517 | 71.6 | |||
| Decrease in incidence | 2.3 | 0.724 | |||||
| Control_2 | 1.77 | 1.13–2.79 | |||||
| Baseline | 141 | 1513 | 1654 | 85.4 | |||
| 1 year later | 87 | 975 | 1062b | 81.9 | |||
| Decrease in incidence | 3.5 | 0.576 | |||||
Substantial numbers of trained workers were lost to follow-up in the year after training, as a result of production line closures or lay-offs associated with the global economic crisis that began in late 2008 (25). The overall follow-up rate one year after training was 60.9% (2120/3479): 58.8% (540/918) for the intervention, 57.0% (517/907) for control_1, and 64.3% (1063/1654) for control_2 groups (figure 1). Workers lost to follow-up were younger, more likely to be female and had shorter duration of employment. However, the proportion with accidental injuries reported at baseline was similar (6.46% versus 6.71%) and there were also no differences in baseline accidental injuries among the three study groups, P=0.454 and 0.436 respectively, for those successfully followed up and those lost to follow-up. For the workers successfully followed up, significant differences were found for age (P=0.032) and gender (P=0.002) among the three groups.
Person-based incidence rates of accidental injury
Common accidents observed mainly involved machine injuries, slips and falls, hit by objects and against objects, as well as manual handling. The IR of accidental injury in the intervention group decreased from 89.3 per 1000 workers at baseline to 52.1 per 1000 workers at one year after training, a reduction of 41.7%. The IR of accidental injury also decreased in the year after training in the two control groups, but to a lesser extent (table 1). The P-value for the interaction term (group×time) in the GEE was 0.019, showing that the before/after accidental injury rate difference (time effect) was different among the three groups (P=0.037 for intervention versus control_1 group, P=0.013 for intervention versus control_2, P=0.994 for control_1 versus control_2 group). Compared with the intervention group, the risk of accidental work injury over time was higher in control groups, with OR 1.78 (95% CI 1.04–3.04) and 1.77 (95% CI 1.13–2.79) for control_1 and control_2 groups, respectively.
Event-based incidence rate of accidental injury
The IR of event-based accidental injury events in the intervention group reduced significantly from 138.3 per 1000 person-years at baseline to 74.5 per 1000 person-years at one year after training (Z=3.687, P=0.0002). The incidence rates of accidental injury in the two control groups also decreased in the year after training, but was not statistically significant (table 2).
Table 2
Self-reported event-based incidence rates (IR) of past 12 months at baseline and at 1 year after training in different groups.
| N (events) | N (workers) | IR (/1000 person-yrs) | Z-valuea | P-value | |
|---|---|---|---|---|---|
| Intervention | |||||
| Baseline | 127 | 918 | 138.3 | 3.687 | 0.0002 |
| 1 year later | 40 | 537b | 74.5 | ||
| Decrease in incidence | 63.8 | ||||
| Control_1 | |||||
| Baseline | 88 | 907 | 97.0 | 0.500 | 0.6169 |
| 1 year later | 46 | 517 | 89.0 | ||
| Decrease in incidence | 8.0 | ||||
| Control_2 | |||||
| Baseline | 201 | 1654 | 121.5 | 1.200 | 0.2303 |
| 1 year later | 113 | 1062b | 106.4 | ||
| Decrease in incidence | 15.1 |
Re-injury after training
In the intervention group, 27.1% (13/48) workers reporting accidental injury at baseline suffered from another accidental injury during the 1-year follow-up after training. The corresponding proportions were 41.7% (15/36) and 52.6% (51/97) in control_1 and control_2 groups respectively, and the re-injury rate in control_2 group was statistically higher than that of the intervention group (table 3).
Table 3
Accidental injury 1 year after training by injury status before training in different groups. [OR=odds ratio; 95% CI=95% confidence interval.]
| Injury at baseline | Total | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Yes | No | |||||||
|
|
|
|
||||||
| N | % | N | % | N | % | OR | 95%CIa | |
| Intervention | ||||||||
| Accidental injury 1 year later | ||||||||
| Yes | 13 | 27.1 | 15 | 3.1 | 28 | 5.2 | 1.00 | |
| No | 35 | 72.9 | 474 | 96.9 | 509 | 94.8 | ||
| Subtotal | 48 | 100.0 | 489 | 100.0 | 537 | 100.0 | ||
| Control_1 | ||||||||
| Accidental injury 1 year later | ||||||||
| Yes | 15 | 41.7 | 22 | 4.6 | 37 | 7.2 | 1.92 | 0.77–4.82 |
| No | 21 | 58.3 | 459 | 95.4 | 480 | 92.8 | ||
| Subtotal | 36 | 100.0 | 481 | 100.0 | 517 | 100.0 | ||
| Control_2 | ||||||||
| Accidental injury 1 year later | ||||||||
| Yes | 51 | 52.6 | 36 | 3.7 | 87 | 8.2 | 2.99 | 1.41–6.33 |
| No | 46 | 47.4 | 929 | 96.3 | 975 | 91.8 | ||
| Subtotal | 97 | 100.0 | 965 | 100.0 | 1062 | 100.0 | ||
| Total | ||||||||
| Accidental injury 1 year later | ||||||||
| Yes | 79 | 43.6 | 73 | 3.8 | 152 | 7.2 | ||
| No | 102 | 56.4 | 1 862 | 96.2 | 1 964 | 92.8 | ||
| Subtotal | 181 | 100.0 | 1 935 | 100.0 | 2 116 | 100.0 | ||
Discussion
The current RCT confirmed that participatory training in occupational health and safety was effective in reducing accidental work injuries among frontline factory workers by >40%. Traditional didactic training with the same training contents and instructors, on the other hand, could not reduce accidental work injuries to any significant extents, and the risk of accidental injuries over time was higher in the two control groups, with OR of 1.78 and 1.77 respectively. Re-injuries were also reduced compared to the two control groups.
RCT have been regarded as the standard of proof in intervention studies, yet very few have been conducted in the field of accidental occupational injury prevention. Key challenges include study group contamination, small sample size, short duration of follow up and worker turnover (26). A large scale RCT involving about 4000 postal workers found that an educational program designed to prevent low-back injury and conducted by physiotherapists did not reduce the rate of low-back injury, the median cost per injury, the time off from work per injury, the rate of related musculoskeletal injuries, or the rate of repeated injury after return to work (27). Participatory ergonomics interventions in preventing low-back and neck pain (17) or musculoskeletal disorders (18) have also been found to be ineffective in a few RCT. According to our knowledge, ours is the first large-scale randomized controlled trial to study accidental injury prevention in industrial workers and successfully documented the effectiveness of participatory OHS training in preventing accidental work injuries.
Participatory OHS training programs are not just educational, but also experiential, as they enlist the active participation of workers and engage them in improving the working environment through conducting inspections of their own work sites using an action check list. With participatory training, workers are more aware of the existing hazards in their job sites and are more likely to adopt safe practices and take necessary actions to ensure their own health and safety. Hence, such programs should lead to better practices, as well as targeting specific improvements in individual worksites. The intervention we administered was rather small, just five hours of training and group work, but significant reductions of accidental work injuries were already observed. In view of the huge numbers of accidental work injuries and the resulting disease burdens in both developed and developing countries, participatory training programs should be more widely experimented and practiced in the future.
Our large scale study of more than 2000 workers being followed-up at one year involved 60 factories from quite a range of manufacturing industries and hence has wide potential applications. Allocation concealment was practiced and a very high participation rate (>95%) of randomized workers was achieved, suggesting that selection and self-selection bias as a result of breaking allocation concealment was unlikely. We adopted a design with two-level randomization (factories and individual workers) in minimizing confounding or non-comparability of subjects (within experimental factory control group), as well as avoiding possible contaminations (control group from another factory). We applied GEE to analyze the data with repeated measurements, considering the correlation of the before/after work-related incident injury from the same worker, as well as the potential correlation among the workers within the same factory. Our results indicated that confounding or contaminations, if present, were minimal, as changes in accidental injury and re-injury rates were pretty similar in the two control groups, but differed substantially from the intervention group. The lack of significant reductions of accidental injury rates in the control group in the experimental factories (control_1 group) suggested that the workplaces might not have been made safer through the process of participatory training. The reduction of accidental injury rates in the intervention group could be more probably attributed to changes in awareness and safer practices. This was particularly true for re-injuries.
A big challenge of such intervention trials at the shop floor level is worker turnover. Our study did suffer from substantial loss to follow-up (39%) and might result in self-selection bias. Although we made every effort to achieve high follow-up rates at one year, the unfortunate coincidence with the “economic tsunami” during the follow-up period led to substantial loss of workers as a result of production line closure or layoffs. It is inevitable to have loss to follow-up with any longitudinal study, which also tends to increase with time. Rates of 50-80% follow-up have been suggested as acceptable by some researchers when data were “missing completely at random” (28–30). We compared the background characteristics between workers lost to follow-up and those successfully followed up and found that the former were younger, more likely to be female and had shorter duration of employment. On the other hand, the proportion with accidental injuries reported at baseline was similar. We adjusted for age and gender in our analyses as a result of having significant differences for age and sex among the three groups at follow-up.
Participating workers were identified by the management of individual factories and might not be totally representative of other workers. This might affect external validity or generalizability, but the random allocation of the participating workers to the intervention and control groups ensured internal validity. The effectiveness of the randomization process was supported by the lack of statistically significant differences in age, gender, education level, duration of employment, training experience, prior work experience, and accidental injury history among the three groups. The exclusion of illiterate people from the study also limits the applicability to those who have received little or no education.
We counted the accidental injury cases and events based on self-reporting of the workers and this might raise concern about information bias (26, 31), which could not be totally avoided. However, there are no reasons to believe that over- or under-reporting of accidental injuries would be differential in the three groups. Our earlier report on self-reported musculoskeletal disorders, which showed no statistically significant changes in the proportion of workers reporting musculoskeletal disorders in any body part after the intervention, also supported that such biases should be minimum (25).
In conclusion, our study documented the effectiveness of a participatory approach to OHS training in reducing accidental work injuries and re-injuries among frontline workers in manufacturing industries at one year of follow-up, though more long-term effects are not yet known.