Musculoskeletal problems, such as low-back pain (LBP), neck pain, and pain in the lower and upper extremities, have shown to be highly prevalent (1). In the working population, such problems, which we will from this point forward refer to as musculoskeletal disorders (MSD), can result in sick leave (2), work disability (3), and early retirement (4), so that it can be concluded that MSD put a large burden on the (working) society (5). Because of this high burden, MSD are among the most prominent occupational health issues, and primary prevention remains a key item on the MSD research agenda (6, 7).
In the last decades, a wide range of biopsychosocial factors have been shown to be associated with either the incidence or recurrence of MSD (8). This includes psychological factors such as health beliefs, mood, and the tendency to worry about common somatic symptoms (somatizing tendency) (9, 10); mental comorbidities (11), sleep problems (12), and pain sensitivity and/or augmented central processing of sensory information (13, 14). Also, personal (eg, age, gender and physical capacity) (15) and (work-related) psychosocial factors (eg, stress, social support and job satisfaction) (16, 17) are known to play a role in the occurrence of MSD. Apart from these factors, however, research into the factors associated with MSD has for a vast amount focused on work-related physical risk factors, including manual lifting, repetitive hand/arm movement (such as computer work) and awkward body postures, for the prevention of LBP (18), upper-extremity symptoms (19) and MSD in general (20), respectively. These work-related physical factors contribute to a substantial extent to the occurrence of MSD (21). For example, it has been estimated that the cumulative contribution to LBP of work-related physical risk factors is around 37% (22). In this paper, using a perspective of work-related physical factors, we will focus on primary prevention of MSD. We will therefore refer to these disorders as “work-related MSD”. Furthermore, although we acknowledge that the aforementioned factors can play a role in the incidence, recurrence and persistence of work-related MSD, to limit the complexity of this paper we will mainly target the reduction of work-related MSD incidence. From this point forward we will therefore refer to MSD by talking about its incidence. However, we fully acknowledge that MSD are recurrent in nature (23), and thus earlier episodes of MSD cannot be disregarded.
Despite the knowledge on factors associated with work-related MSD, interventions on primary prevention of MSD through modifications of the physical work-related factors, such as through manual handling advise (24) and ergonomic workplace redesign (25), have not shown to be overly successful in preventing MSD. Moreover, while there are numerous preventive measures and strategies (eg, workplace interventions or ergonomic guidelines) in place, the global burden of MSD seems to have increased rather than decreased over the last years (26). The latter is, however, not the case in all topographic areas (27). Even if interventions have rendered limited or no success, which for instance seems to be the case for job rotation (28) and advice on lifting techniques (24), they are still frequently applied in work settings.
Reasons for the lack of success in MSD prevention could be due to theory and/or program failure; ie, a lack of understanding of etiological mechanisms and/or limited translation of such knowledge into well-designed intervention programs, respectively (6). A combined research framework can link disciplines, which may reduce theory and program failure by improving theories about etiological mechanisms and strengthening the development and implementation of prevention strategies for work-related MSD. Such a framework can help to understand work-related risk factors and corresponding mechanisms, develop ideas to modify these risk factors (with interventions being compatible with sustainable work production), test and, once proven effective, implement these modifications in the workplace.
In the previous decades there has been an increase in the number of studies regarding primary prevention of MSD, across a wide range of scientific disciplines, including epidemiology (29), applied physiology (30), biomechanics (31), physical and organizational (macro) ergonomics (25, 32), behavioral sciences (33), production engineering (34), organizational management (35), health and business economics (36), and implementation science (37). These disciplines vary largely in their contribution to work-related MSD prevention research, ranging from classic injury surveillance and etiological studies to detailed laboratory studies and animal models exploring injury mechanisms, and studies evaluating interventions and implementation. It has been argued that, for MSD prevention, multi-disciplinary interventions integrating quantitative and qualitative methods from the aforementioned disciplines are needed (38). By doing so, different disciplines can contribute research methodologies and paradigms from their respective fields. As such, several models from various disciplines have been proposed addressing different aspects of work-related MSD prevention, for instance providing focused approaches to mechanisms for work-related risk factors and preventive interventions or implementation (table 1). Apart from work-related physical risk factors, these models address other factors that may play a role in the development of MSD, such as personal factors (eg, age, gender and physical capacity) (15) and (work-related) psychosocial factors (eg, stress, social support and job satisfaction) (16, 17). Although these models could, in theory, be compatible with one another, none of them fully covers all research disciplines that link mechanisms with interventions and implementation. The advantage of such an over-arching framework is that it can lead to exchange of ideas and results among the different research disciplines, which may reduce existing theory and program failure, increasing prevention effectiveness.
Table 1
Models for aspects of the cycle of prevention, from musculoskeletal disorder (MSD) research and other related research fields.
| Aspect of the cycle | First author (year of publication) | Description |
|---|---|---|
| Association work-related risk factors with MSD | Armstrong et al, 1993 (100) | Conceptual model for work-related neck and upper-limb MSD, in which pathogenesis of the disorders is described. The model consists of a sequence of exposure, dose, capacity and responses, such that response at one level can act as dose at the next. According to this model, the response to one or several doses can impact on the capacity for responding to future doses. |
| Westgaard & Winkel 1996 (101) (based on Winkel & Mathiassen, 1994 (102) | Describes the physiological responses to biomechanical risk factors, using an exposure-effect model. The model distinguishes external exposures (being risk factors in the work environment, expressed in intensity, frequency and duration) and internal exposures (being the forces acting on and in the body while being exposure to the external exposure). The internal exposure is assumed to lead to biological responses (acute and chronic) effecting organs, tissues, cells and molecules. | |
| Hoozemans et al, 1998 (103) | Model for musculoskeletal risk factors associated with pushing and pulling. The model presumes a certain pushing and/or pulling task, which is associated with a certain posture or movement of the body and exertion of forces (external exposure). This external exposure causes an internal exposure (eg, compressive forces at the lower back intervertebral discs), which is associated with acute or chronic physical response. Work capacity of the worker (physical, cognitive, and mental characteristics) plays an important role in the model as it impacts on the association of external and internal exposure and that of internal exposure and the response. | |
| Barr & Barbe, 2004 (104) | Physiological model for the development of tissue injury as a result of repeated postural risk factors through a vicious cycle of pain and motor recruitment. The model addresses the role of the inflammatory responses in tissue as a result of exposure to risk factors and its contribution to chronic or recurring tissue injury, related to behavioral indicators of discomfort and movement dysfunction. | |
| Visser & van Dieen, 2006 (105) | A model of pathophysiology of upper extremity muscle disorders consisting of five saccades: 1) sustained muscle activity may be a primary cause of disorders as a result of which 2) skeletal muscle may show changes in morphology, blood flow, and muscle activity; and 3) accumulation of calcium ions in the muscle sarcoplasm may take place causing damage of muscle cells. Therefore, 4) suboptimal blood flow appears to plays a role in pathogenesis of muscle disorders, 5) while also additional mechanisms, such as sensitization may play a role. | |
| Westgaard and Winkel, 1997 (73) | Model for the relationship between biomechanical exposure and musculoskeletal health effects, integrating organizational and contextual aspects. External exposure is influenced by factors at the company level such as production system, personnel and their organization and organizational culture. On the other hand, activities and decisions made at the company level are influenced by factors in the community, including legislation, market forces and technology developments. | |
| National Research Council & Institute of Medicine, 2001 (45) | Describes risk factors for MSD in a comprehensive model in which external load, organizational factors, social context, and individual factors were included, identifying different pathways for the hypothesized injury mechanisms. | |
| Westgaard & Winkel, 2011 (106) | Model describing work-related musculoskeletal and mental health effects of production system rationalization as well as organizational-level measures. | |
| Punnett et al, 2009 (107) | Model describing the multi-factorial origin of MSD by identifying shared risk factors of MSD with other worker health outcomes, such as cardiovascular and metabolic disorders (including the physical and psychosocial conditions of work, and individual health behaviors). | |
| Development of preventive interventions | Holtermann et al 2010 (54) | The FINALE model outlines the pathway through which prevention might take place. An imbalance between individual resources and work demands was hypothesized to increase the risk of physical deterioration. Improved individual resources or reduced work demands was hypothesized to prevent physical deterioration. |
| Backholer et al 2014 (64) | Framework for the likely impact of obesity prevention strategies (which could also be applied to MSD prevention). According to the model, the degree of impact required to influence behavior change is influenced by agentic (the problem is perceived as a personal one), agento-structural (the problem is considered to be caused by the environment in which unhealthy behaviour takes place, but also of individual behaviour is important), and structural factors (individuals behave within the constraints of the persuasive environment, and behaviour is not viewed as free will). | |
| Implementation of preventive interventions | van der Molen et al 2005 (92) (based on Grol et al, 1997 (108)) | A model taking an implementation approach that focused on defining intervention measures and, ultimately, implementation strategies aiming at the reduction of physical work demands due to manual materials handling among construction workers. The model contains of six steps: 1) selection of intervention measures; 2) analysis of social and organizational context; 3) goal setting; 4) selection of intervention strategies; 5) development of implementation plan for intervention measures; and 6) implementation of intervention measures and evaluation of its progress. |
| Rivilis et al 2006 (109) | Model describes how interventions operate, to result in the desired effects. It was hypothesized that with greater process implementation intensity, greater change in exposures to MSD risk factors as well as improvements in health outcomes would be achieved. |
Comprehensive research frameworks exist in other research fields, such as the “sequence of prevention” of sport injuries (39), the “Translating Research into Injury Prevention Practice” (TRIPP) framework (40) and the framework for disease prevention in behavioral epidemiology (41) (table 2). We did, however, not find a framework fitting work-related MSD prevention research, hence our objective is to define such a framework. The framework will be described in this paper, and examples of how the framework can be used (mainly from the perspective of work-related physical risk factors) will be provided.
Table 2
Frameworks for primary prevention from related research fields.
| First author (year of publication) | Research field | Description |
|---|---|---|
| Tugwell et al, 1985 (110) | Health | This model describes 7 steps consisting of 1) the burden of the illness, 2) etiology of causation, 3) community effectiveness, 4) efficiency, 5) synthesis & implementation, 6) monitoring of programme and 7) reassessment. |
| van Mechelen et al, 1992 (39) | Sports injury prevention | Framework for the general ‘sequence of prevention’ of sport injuries consisting of four steps: 1) establishing the extent of the sports injury problem; 2) establishing the etiology and mechanisms of injuries; 3) introducing preventive measures; and 4) assessing their effectiveness by repeating step 1. |
| Finch et al, 2006 (40) | Sport injury prevention | The Translating Research into Injury Prevention Practice (TRIPP) framework for research, leading to sports injury prevention. The framework consists of seven steps: 1) a detailed understanding of the etiology of injuries; 2) development of interventions to directly address the identified mechanisms of injury; 3) formal testing of these interventions under controlled conditions; 4) understanding of the sporting and individual athlete behaviors context in which the interventions are to be implemented; 5) potential modification of interventions to take the implementation context into account; 6) assessment of potential factors associated with the real-world introduction and application of safety measures and development of implementation strategies; and 7) formal evaluation of the effectiveness of injury prevention measures within the implementation context. |
| The TRIPP framework distinguishes scientific evaluation of the intervention under ‘ideal conditions’ (i.e. efficacy studies), description of the intervention context, and evaluation of the intervention in implementation context (i.e. effectiveness studies). | ||
| Sallis et al, 2000 (41) | Behavioral epidemiology | Framework for the classification of phases of research on health promotion and disease prevention consists of 5 steps: 1) establish links between behaviors and health; 2) develop methods for measuring the behavior; 3) identify factors that influence the behavior; 4) evaluate interventions to change behavior; and 5) translate research into practice |
The framework of MSD prevention research
We propose a framework for work-related MSD preventive research utilizing a repeated sequence approach based on comparable frameworks from other research areas (39–41), and the “risk identification, assessment, control and evaluation framework” that is a basis for international occupational policy and practice (42). The proposed framework is composed of an order of 6 steps (figure 1):
Figure 1
Proposed research framework describing a repeated sequence for prevention of work-related musculoskeletal disorders (MSD). Ideally, one can follow the sequence starting with step 1 and ending with step 6 (solid lines) after which the sequence can be repeated. Alternatively, if interventions have not proven to be effective in step 5, one could return to either step 2, 3 or 4 (dashed lines).
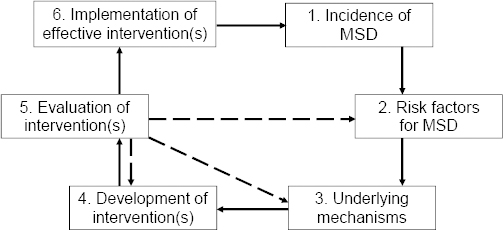
Step 1. Incidence and severity of MSD
Step 2. Risk factors for MSD
Step 3. Underlying mechanisms
Step 4. Development of intervention(s)
Step 5. Evaluation of intervention(s)
Step 6. Implementation of effective intervention(s).
Below, the framework will be explained step-by-step, after which two examples will be provided, showing the advantages of an exchange of ideas and results among the different research disciplines.
Step 1. Incidence and severity of MSD
In the first step, the extent and severity of MSD in the (working) population of interest needs to be identified. For this initial step, descriptive epidemiological data (such as MSD incidence) can be used, in which severity and the resulting impact (eg, sick leave or work disability) of the MSD could also be considered. Information on MSD impact can be valuable for companies and society, since costs related to sick leave, work disability, and productivity loss are the principal drivers of the financial burden of MSD (43).
Step 2. Risk factors for MSD
The second step identifies (work-related) risk factors that may play a role in the incidence of MSD. Epidemiological observational studies are required to gain insight into these risk factors with cross-sectional studies identifying associated factors, and prospective studies being able to make a better distinction between causes and effects (44). It is postulated that exposure to physical risk factors, combined with lack of recovery, is an important group of risk factors for the incidence of MSD (45), with epidemiological evidence for manual lifting/materials handling, awkward postures and whole-body vibration to be associated with MSD (18, 20). However, it should be noted that the etiology of MSD is multi-factorial and that various other factors are involved in the onset of work-related MSD, such as work-related psychosocial factors (including high job demands and poor social support at work) (16, 17) and individual factors (including age, gender and physical capacity) (15), but also psychological factors such as health beliefs, mood and somatizing tendency (9, 10); mental comorbidities (11), sleep problems (12), and pain sensitivity and/or augmented central processing of sensory information (13, 14). These factors may either be independent risk factors or factors modifying the association of physical risk factors and MSD. Overall, more etiological research is needed to strengthen this body of research.
Step 3. Underlying mechanisms
The third step unravels the underlying mechanisms and pathways for the association of work-related physical risk factors and MSD, also taking into consideration relevant factors from other domains. Studies designed to shed light on the underlying mechanisms can take place either at the workplace and/or in a laboratory. In certain studies, work activities can be simulated allowing to study possible risk factors in detail during controlled conditions [eg, (46)] while enabling to isolate the effect of single factors. For example, tissue damage based on cadaver studies (47) or animal models (48) can be used, or the influence of a specific physical risk factor (such as different office workstations or temporal loading patterns) on short-term effects as proxies for MSD, such as localized muscle activity (49), can be studied. These types of studies might be initiated by step 2 in which, for example, the duration of computer mouse use appeared to be a risk factor for upper-extremity pain among office workers (50). A laboratory study can then be used to assess effects of computer work on localized muscle contractions. More information on such mechanisms (ie, etiology and the effect of different work settings) is needed to generate possible solutions. For example, if sustained muscle contractions due to prolonged exposure to non-neutral hand postures while holding a mouse are the underlying cause of upper-extremity pain in computer workers, then interventions should aim at improving the workstation design (or more specific, the computer mouse) to influence this risk factor.
Also the underlying mechanisms for work-related psychosocial risk factors should be considered, as these factors can interact with work-related physical risk factors (51). For example, time pressure can be the cause of a rise in the volume of work performed, and hence of an increase in biomechanical loading (49). Alternatively, psychosocial stressors may be associated with increased muscle tension (52), or may trigger (sustained) stress reactions, which may cause physiological responses contributing to the development of MSD (53). Generally, in work-related MSD prevention, not just physical risk factors, but also other factors can be considered in a multi-component intervention (54). In such interventions, also the workers’ own perception of underlying mechanisms may play an important role (55).
Mechanisms from other (eg, personal, psychological or central sensory) domains can play an important mediating or modifying role with the exemplified mechanisms as mentioned above. However, as the focus of the current paper was on work-related physical factors, we will not further elaborate on such mechanisms.
In summary, formulating the underlying mechanisms for the onset of MSD could help understanding the exact association of a certain risk factor with MSD and should largely determine the content of interventions to prevent MSD.
Step 4. Development of intervention(s)
The fourth step is to develop and introduce an intervention, which is likely to reduce the incidence of MSD. These interventions are preferably based on an understanding of underlying etiological mechanisms of MSD, as identified in step 2 and 3, and often focus on reducing a possible risk factor, also taking other (non-physical and/or work-related) factors into consideration. Key issues in developing the intervention are whether the risk factor is amendable to change, the relative contribution of the risk factor to the MSD (how much can be avoided; efficacy) and the success of interventions in reducing this risk factor (how much reduction can be achieved; effectiveness) (56). The latter will depend on the implementation, efficacy and sustainability of the intervention (57). It is therefore important to pay attention to optimal feasibility and acceptability of the intervention in advance (58), by understanding barriers and facilitators of the intervention, on the level of the individual worker and of companies and/or employers.
In interventions focusing on work-related physical factors, the work environment (including the technological environment), the organization and/or the behavior of the individual worker could be (re)designed such that the risk of MSD incidence is minimized. Interventions can be designed according to the “risk control hierarchy model”, which recommends elimination of the risk where reasonably practicable, or alternatively minimization of the risk (59).
Step 4 requires an understanding of the work organization where the intervention is being implemented, as workers respond to the work context and need support to learn how to implement the intervention into daily working life through training (60) or through a more comprehensive approach, in cooperation with employers and other stakeholders (61). These approaches can often address multiple pathways including psychosocial factors and the physical conditions at work, but should also acknowledge the multi-factorial causes of work-related MSD (62). As such, multi-factorial interventions (not only focusing on the physical risk factor) may be proven to be effective in future research. Moreover, a profound understanding of how to effectively change people’s behavior within the context of work (in addition to understanding how to change and/or capitalize on organizational attitudes and procedures) is required when designing a workplace intervention (63, 64).
In accordance to the general principles of evidence-based medicine (65), the development of preventive interventions should be based on know-how and skills of workers and companies/employers combined with scientific evidence on underlying mechanisms of MSD. To optimize feasibility and acceptability, active involvement of workers, employers and other stakeholders in the development of interventions has received more attention. This can involve participatory processes (66, 67) or even a full intervention mapping (IM) procedure (68). IM originates from health education and is a stepwise process for development of theory-, evidence- and practice-based interventions, which stimulates involvement of stakeholders during the entire process of program development, implementation and evaluation.
Step 5. Evaluation of intervention(s)
The fifth step is to evaluate the effectiveness of preventive interventions. This can start with efficacy studies under well-controlled circumstances and can move on to effectiveness studies in a real working-life situation. To do so, changes in the risk factors along the hypothesized pathway of the intervention and changes in proximal outcomes, which can be expected to sustain in the investigated setting (69), should be evaluated. Such interventions can focus on a work-related physical risk factor, but may also consist of elements from other domains.
Various studies on relatively simple interventions have been published, such as on redesign of the workstation, established a decrease in exposure to risk factors or short-term discomfort as a result of the intervention (70). In such studies, however, MSD outcomes (such as incidence and impact of MSD) have only sparsely been used. Moreover, as it has often been observed that the effectiveness of an intervention on MSD outcomes may attenuate after a certain (effective) intervention period (71), also long-term effects should be studied.
To improve chances of implementation, but also to better understand the efficacy of the intervention and potential theory or program failures, process evaluation assessing practical feasibility alongside the effectiveness study should be performed (56). Such evaluations should include process tracking that measure possible barriers or facilitators of the implementation (eg, fidelity to and reach of the intervention) (72). Process evaluation and research into effectiveness, in terms of measuring exposure to risk factors and MSD outcomes, allow for the assessment of theory and/or program failure for further improvement of a (partly) ineffective intervention. It is possible that a well-designed study (in which the intervention implementation went as planned) offers “negative” effectiveness (50, 73) after which one might be forced to study risk factors (short-cut to step 2) and/or the underlying mechanisms (short-cut to step 3) again, after which step 4 and 5 can possibly be repeated. Alternatively, this exercise can cause researchers to realize that earlier thought mechanisms are not that well understood, as a result of which different interventions should be developed. In case of positive efficacy and effectiveness results, however, the intervention study should ideally be replicated to investigate its effects in other populations and contexts, while also cost-effectiveness or cost-benefit analyses can be performed.
Step 6. Implementation of effective intervention(s)
Finally, step 6 is large-scale implementation and scale-up of the study results in the working society, with an amenable trade-off between effectiveness and required (economic or productivity) resources. Implementation research can evaluate the implementation process and its effects, while a better insight into fidelity of an intervention can help to design good implementation strategies at organizational and community levels. Two of the most extensive examples of MSD interventions implementation at the community level are the Australian mass media campaign to change back pain beliefs and disability (74), which was followed-up in Scotland (75) and Canada (76); and the Washington State ergonomics rule, which reduced employer-reported risk factors (77). The latter rule, however, was repealed three years after its implementation.
In an optimal situation, large-scale implementation would result in a positive effect on the occurrence, severity and/or impact of MSD as monitored in a repetition of the first step. Hence, the circle is closed towards the first step.
Examples of how the framework may work
In the following, two examples as to how the proposed framework may work are outlined. Although interventions on other factors and even multi-component interventions are imaginable and well suitable to be designed using our framework, these examples were chosen from a work-related physical risk factors perspective.
Example 1: Lower-back pain and manual lifting
In the industrialized world, large proportions of the population suffer from LBP (1), with LBP prevalence in sub-groups with high physical workload (eg, scaffolders) (78) being even higher (step 1). As mentioned before, there are many risk factors for the onset of LBP (step 2), and most of these factors result in an increased risk of LBP with the cumulative contribution to LBP of physical work-related risk factors estimated to be around 37% (22) (although such numbers may differ between specific occupational sub-groups). It should therefore be realized that the potential for primary prevention of LBP by fully taking away work-related physical risk factors is limited to 37%. Manual lifting has been found to be one of the prominent risk factors for LBP, with lifting >25 kg or >25 times per day estimated to lead to an increase in the one-year LBP incidence by 4.3% and 3.5%, respectively (18).
According to results from laboratory studies, manual lifting is associated with substantial loads on the lower back (31), while causal mechanisms assume damage to intervertebral discs and endplates, facet joints, ligaments, or muscles because of these loads (79). Moreover, biomechanical studies help in understanding underlying mechanisms of LBP in terms of, for instance, motor control during lifting, tissue tolerance to forces, and physiologic responses to repeated lifts (80). Such mechanisms have, however, not been confirmed in epidemiological studies assessing the association of spinal pathologies and back pain symptoms (81). As such, biomechanical research performed in step 3 and epidemiological research performed in step 2 and 4 remain distant from each other, since controlled laboratory studies will only show short-terms effects of the studied risk factors while in epidemiological studies it is hard to isolate the contributing risk of a single factor. Therefore, underlying mechanisms causing LBP due to lifting are still not fully understood. Possibly because of a lack of understanding of mechanisms, interventions targeting lifting to prevent LBP have not been shown to be overly successful (24).
The following example illustrates an intervention on lifting education and instruction for which, in the framework for MSD prevention research, research has jumped from step 2 to step 4. For this intervention it has been assumed that lifting technique is a major cause for LBP and that LBP would be prevented by training workers to lift “properly” (ie, using their legs during a squat lift rather than their back in a stoop lift). The hypothesized mechanism would be that compressive loading of the back, which is high in manual lifting, may lead to spinal injury (based on cadaveric studies), and that a good lifting technique helps to reduce such compressive loading. While scientific literature has yet to prove the effectiveness of lifting education for the prevention of LBP (24) (step 5), millions of workers around the world received such lifting instructions and many still get them (step 6). Since the results of the evaluation of the intervention are disappointing (step 5), we need to go back to the earlier steps. Although the scientific debate remains open, literature reviews have shown that there is not a single best lifting technique, as low-back load hardly differs between squat and stoop lifts (82, 83), nor does the association of lifting and LBP appear be the result of mechanisms of tissue damage (81). This means that the aforementioned intervention of lifting education or instruction had theory failure.
Program failure in the development of interventions might be another reason for the lack of effectiveness in lifting interventions for the prevention of LBP. For example, an intervention introducing a new technology to reduce the load on the lower back, such as ceiling hoists for patient care workers, requires workers to use and engage with the technology. However, such a change in behavior is difficult to achieve and requires attention to determinants of behavior within the particular occupational context (84). Only few of such studies have been performed in the field of work-related MSD (85, 86).
In conclusion, the example of interventions based on lifting to prevent LBP shows that it is not only important to use information from step 2 and 3 to prevent theory failure, but also to develop a feasible intervention (step 4) to prevent program failure, before moving to step 6.
Example 2: MSD and bricklaying work
A recent review showed that bricklayers have an increased risk of developing MSD, including LBP and pain in the upper and lower extremities (87), with bricklayers experiencing even more MSD than other construction workers (88) (step 1). The risk factors for MSD among bricklayers have been well documented from several workplace studies (step 2), with manual materials handling being the most prominent (87, 88). These studies showed that for bricklaying assistants, manual materials handling needed for transportation of bricks, blocks and mortar is the most physically demanding task. The most demanding task for workers using traditional bricks consisted of repetitive one-handed lifting of bricks, often in awkward working postures, and for those who perform masonry work using large blocks, physical work demands include two-handed lifting of heavy concrete, gypsum or calcareous blocks.
Several experimental laboratory studies have investigated physical risk factors in terms of biomechanical load associated with varying intensities and frequencies of manual material handling in this job (89) (step 3). Based on this evidence, the hypothesis for the underlying mechanism for MSD among bricklayers is that repetitive manual handling imposes biomechanical load on the back and upper extremity structures, exceeding the worker’s strength and capacity (due to the limited opportunities for recovery during work), causing damage of musculoskeletal structures and thereby MSD.
Using this etiological hypothesis, several (consensus-based) preventive interventions have been developed (step 4) (88), in which the most important interventions can be categorized into: (i) adjusting working height of bricks, blocks and mortar, (ii) mechanization of block laying, and (iii) mechanization of the transportation of materials. The efficacy of these interventions has been investigated in field studies that showed mixed results (step 5), ranging from a substantial reduction of trunk flexion and local musculoskeletal discomfort (88) to no effects on physical risk factors among workers using gypsum blocks (90).
Workplace effectiveness was examined in a controlled intervention study, with measurements before and 10-month after the introduction of stools and consoles for raised bricklaying (91). The intervention significantly reduced several risk factors (including trunk flexion and arm elevation) and resulted in a statistically significant decrease in sick leave, but had no effects on the prevalence of MSD.
When barriers and facilitators for the implementation of ergonomic measures in bricklaying were qualitatively studied among stakeholders (92), it appeared that employers/planners were not fully aware of the health risks of not implementing ergonomic measures, while foremen/bricklayers were more often aware of this. The majority in both stakeholder groups, however, understood the ergonomic measures and wanted to provide the bricklaying teams with these measures, but did not intent to actually buy or hire the materials needed. Hence, only slightly more than half of the bricklayers and their assistants reported to adopt the intervention measures (93). Both stakeholder groups mentioned several other barriers impeding the ability to actually use the ergonomic measures in practice, such as the extra work regarding maintenance and logistics. The supportiveness of the work environment (considering the compatibility with an effective production) should therefore be taken into consideration (64).
In an optimal situation, implementation of this intervention (step 6) would cause a reduction of MSD incidence as monitored among bricklayers’ populations in a repetition of step 1 of the framework.
Discussion
In this paper we proposed a research framework for work-related MSD prevention research, with two examples demonstrating how prevention impacting on work-related physical factors could reduce the MSD burden using the research framework’s repeated sequence. In example 1, information from step 2 and 3 is required to prevent theory failure and step 4 is necessary to develop a feasible intervention to prevent program failure, before moving to step 5 and 6. Example 2, on the other hand, showed a more sound understanding of mechanisms (step 3), and intervention barriers and facilitators (step 4) and its associated health and productivity outcomes (step 5), which is more likely to result in a positive implementation (step 6). Although the focus of this framework is on work-related physical factors and examples provided in this paper target the reduction of incidence of MSD, a similar sequential approach can be used for non-physical factors and/or for the prevention of MSD recurrence. However, when focusing on other musculoskeletal outcomes, other issues that have not been described in this manuscript, such as the timing of the intervention, should be considered.
Different scientific disciplines have been focusing on parts of the framework of work-related MSD prevention research (table 1). For instance, occupational epidemiology studies the incidence of work-related MSD (step 1), risk factors of MSD (step 2), and the effects of relevant interventions (step 5). Occupational epidemiologists, however, perform few studies on the pathways and mechanisms causing diseases and disorders (step 3). Although there are some examples of integration of laboratory-based methods in epidemiological studies, for example in studying the role of pain tolerance in upper-limb disorders (94) and performing detailed assessment of low-back load and its association with LBP (29), laboratory and epidemiological studies often remain distant. Moreover, in epidemiology the expertise and knowledge for the development of interventions (step 4), and large-scale implementation of proven effective interventions (step 6) is lacking but could be obtained from adjacent research disciplines, such as ergonomics, public health and sports medicine.
A better understanding of the underlying mechanisms and barriers and facilitators of interventions and implementation would help the development and implementation of effective interventions. It should, however, be noted that not all steps are conditional, and primary prevention can still be successful without taking all sequential steps. For example, the occupational disease scurvy had a high incidence in sailors on ships in the 17th century (step 1), leading to high mortality rates. In the middle of the 18th century James Lind, a surgeon in the British Royal Navy, proved that scurvy could be prevented and treated with citrus fruit (step 5) (95). However, the Royal Navy did not implement his advice for several decades (step 6). The incidence of this occupational disease finally dropped when fresh citrus fruit and/or sauerkraut was provided to sailors during the journey (step 4). It would take until 1932 to know that nutritional deficiency of vitamin C caused scurvy (step 2), not to mention the underlying mechanism and pathogenesis (step 3). Hence, it is possible to obtain an effective intervention while skipping one or more steps of the framework, although preventive interventions based on knowledge obtained in step 2 and possibly also step 3 may have a larger potential. Moreover, this scurvy example illustrates the importance of implementation of proven effective interventions (step 6).
The argument made in this paper is that, in intervention research, paying more attention to steps 3, 4 and 6 would increase the potential of MSD prevention in the occupational setting. This would require a more close collaboration of scientific disciplines (using quantitative and qualitative research methodologies) to adhere to the repeated sequence of work-related MSD prevention research. Moreover, in the development of interventions, also factors that are not physical or work-related should be considered. For step 2 and 3 epidemiological and ergonomic field studies should be integrated more with laboratory experimental studies that start from a theory and formulate hypotheses based on deduction. Epidemiology can provide data on which such theories and hypotheses can be based, and can study the effectiveness of experimental results on a large scale. This requires a stepped approach where epidemiological and ergonomic field studies and experimental laboratory research are performed repeatedly in a sequential order. One could think of experiments within a prospective cohort study, or detailed biomechanical assessments of work-related physical risk factors using field-based assessment methods. By doing this, laboratory-based risk factors, such as muscle activity, awkward body postures and biomechanical load, and their association with short-term effects (including local discomfort), can be linked to the actual onset of MSD. Results from these studies could give insight into whether peak or cumulative exposure to a risk factor (29), or alternatively, lack of variation in movement (96) contributes to the onset of MSD. Such mechanistic knowledge would be crucial for the development of preventive interventions. In general, however, the research gap between epidemiological studies and experimental laboratory studies should be bridged from both sides.
In step 4, behavioral sciences and industrial/organizational psychology can become more involved in the development of interventions for the prevention of work-related MSD, in which the intervention should be tailored to the occupational context. To do so, feasibility of the interventions and potential compliance should be tested in an early stage (using qualitative methods). Step 5 consists of an epidemiological effectiveness study, if possible through a randomized controlled trial, while process evaluations should be performed alongside this trial being the start of implementation research that is the heart of step 6. Currently, implementation research is almost non-existing in the prevention of work-related MSD, while this has received more attention in other research fields [eg, physical activity research (97)]. Progress from these fields can be translated and used in the occupational setting.
In essence the proposed research framework is similar to a continuous improvement cycle used for the quality of production and health and safety management systems (98). Through its multi-disciplinary approach this framework can also guide practitioners in developing MSD prevention efforts within an organization and/or community, conducting surveillance of injury, evaluating risk factors in the field, creating interventions with understanding of underlying mechanisms, implementing programs within the context of the organization, and evaluating the interventions through efficacy and process tracking to determine facilitating factors and barriers to implementation.
It should be noted that, apart from the steps described in this framework, there are a number of prerequisites for MSD research that should be taken into consideration, which play a role in all steps of the sequence for prevention of work-related MSD (99). Firstly, there is a lack of international consensus regarding the operational definition of work-related MSD, with different definitions likely leading to different MSD incidence in the same population. Secondly, there is no straightforward way for the assessment of physical risk factors in workers with different assessment methods (eg, objective, observational or self-reported measures) and measurement regimes (eg, continuous measurements for a particular timespan or sampled measurement), each with their specific trade-off between accuracy and feasibility. Moreover, it is important to realize that there is no “one size fits all” intervention to prevent MSD. Therefore, implementing the same preventive regime for all to prevent MSD, regardless of personal, psychological and social characteristics as well as other comorbidities, would be irrational. It is proposed that the effectiveness of any specific intervention on preventing MSD should be examined in individuals who will theoretically benefit from such an intervention, keeping in mind that the potential for prevention of the MSD by fully taking away work-related risk factors is limited to about one-third.
Concluding remarks
We present a framework for optimal work-related MSD prevention linking research disciplines. This framework can help to improve theories and strengthen the development and implementation of prevention strategies for work-related MSD. To obtain the best possible work-related MSD prevention result, in research we should develop interventions based on an identified problem (step 1) targeting risk factors that appear to be associated with an MSD problem (step 2), possibly with a sound understanding of the underlying mechanisms and pathogenesis (step 3). Moreover, the intervention should be optimally targeted to the specific occupational population and setting (step 4), while a proven effective preventive interventions (step 5) should be widely implemented, using evidence-based implementation strategies (step 6).



