Semi- and unskilled (blue-collar) workers have a higher risk of premature drop-out from the labor market than skilled and white-collar workers (1). An important explanatory factor is the high physical work demands faced by semi- and unskilled workers (such as spending a large proportion of one’s worktime standing, walking and forward bending) which impose an adverse effect on health and act as a barrier to sustainable employment (2). However, these employee groups also face various psychosocial work conditions which may deplete personal resources (3). If ample recovery opportunities are not available, the resulting continuous depletion of resources can lead to adverse effects on workers’ well-being and health (4). Ultimately, in the absence of adequate recovery, negative long-term effects such as exhaustion, losses of function, and physical and mental impairment can occur (4, 5).
Long-term effects of poor recovery from work are often preceded by acute symptoms, measured by the need for recovery inventory (ie, a person’s desire to be temporarily relieved from demands in order to restore his or her resources) (5, p330). If sufficient recovery is not achieved, the worker must exert additional effort to meet the demands of their job the next day, and this process may start a vicious cycle leading to prolonged fatigue and exhaustion (5). Poor recovery is shown to predict high employee turnover (6), poor well-being (7), high sickness absence (6), and poor sleep and emotional complaints among workers (8).
Work ability is another scientific concept reflecting whether employees can perform their job without strain (9, 10). Work ability is defined as “how good is the worker at present, in the near future, and how able is he/she to do his/her work with respect to work demands, health, and mental resources” (11, p3). Building on a balance model, factors that contribute to strain are described as demands, while resources are described as factors that prevent or reduce strain (12). The work ability concept takes an inclusive view of demands and resources as factors that can be found both at the workplace (as in the job demands-resources model) as well as in the individual (11, 13). This makes the model compatible with a job demands–resources approach, while remaining cognizant of potential influence from other demands or resources than those described in the extant literature. A decreased work ability has been documented to be associated with high work demands (14, 15), low personal resources, stress and burnout (16, 17), as well as future sickness absence (14, 18), and early retirement (14, 19).
Blue-collar workers more often experience fatigue (20, 21) and impaired work ability compared to other occupational groups (22–24) reflecting an imbalance between work demands and resources, which can partly explain their increased prevalence of early labor market dropout (14). Intervention studies have aimed to improve the work ability and recovery in a variety of study populations, but with minor or no improvements (25–29). Beneficial intervention results have been observed for healthcare workers’ recovery (30, 31). However, the generalizability of these interventions to other work sectors is uncertain given the large differences in work demands, resources and the organization of work. A reason for the lack of positive intervention effects on recovery and work ability of many interventions could be that most previous studies did not, as it has been recommended, target a sufficiently wide array of organizational, psychosocial, and physical factors using a multi-dimensional approach (25–27, 32). Predominantly, the individual worker level has been targeted in previous interventions on recovery and work ability (26, 27, 30, 33, 34). In contrast, organizational interventions (35, 36) have the potential to reduce or remove the causes of strain for entire workgroups (primary prevention) (37) and not only for workers in need. Thus, integration of the organizational and individual levels in workplace interventions are recommended for improving workers’ health and well-being (38).
Additionally, most previous interventions have been expert-driven, which can lead to a mismatch between the intervention content and the expectations and needs of the participants (27). Instead, using a participatory design with high involvement of the participating workers through all phases of the intervention contributes to a better fit between the intervention content, the perceived needs of the participants, and the organizational context (35, 39, 40). However, a limitation of participatory interventions is the uncertainty of which problems the participants will choose to target and which actions plans will be decided (41), making participatory interventions difficult to evaluate.
We aimed to evaluate the effectiveness of a participatory physical and psychosocial workplace intervention (known as PIPPI) based on the aforementioned recommended features on recovery and work ability among industrial workers. The primary hypothesis was that the intervention would improve recovery and work ability. The secondary hypothesis was that the intervention would improve the workers’ productivity, mental health, and well-being as well as physical work demands and resources.
Methods
Study design and study population
This study reports the effectiveness of a one-year cluster-randomized controlled trial (RCT) (41). This trial has been registered in the Danish Data Protection Agency register (Journal number: 2013-54-0329) and in the International Standard RCT Register (ISRCTN76842602). Moreover, the Ethical Committee for the regional capital in Denmark evaluated this study (Journal number: H-2-2013-FSP13), and it was conducted in accordance with the Helsinki declaration (42).
Three large Danish industrial workplaces, which employed workers organized in teams and mainly carrying out manufacturing work, were recruited. A shortlisting of eligible workplaces was conducted in collaboration with worker and workplace/trade unions. The detailed recruitment strategy and the inclusion and exclusion criteria at the workplace, team, and individual levels are detailed elsewhere (41). For each workplace, two or more departments were selected for inclusion in the study allowing for randomization at cluster level to reduce contamination between closely interrelated work teams. All workers in the pre-determined departments of the recruited workplaces were offered to participate in the study. As the intervention was organizational, there were no individual exclusion criteria for taking part in the intervention activities.
Intervention
Many interventions target multiple levels of the worksite in an attempt to provide a coherent and adequate solution to the often complex health or well-being problems that motivate the intervention, and such interventions sometimes lead to synergistic effects relative to single-level alternatives (43, 44). One way to describe such an approach is by way of the IGLO concept, which refers to how relevant actions often can be found at both the individual (I), group (G), leader (L), and organizational (O) levels. The IGLO concept also facilitates categorization and comparison of interventions by highlighting which of these four levels interventions target. In this study, the intervention (PIPPI) targeted all IGLO levels of the workplaces by one or more of the intervention activities. This was done to ensure the integration between PIPPI activities themselves and between the intervention and ongoing organizational procedures, such as health and safety initiatives or management decision making processes. The specific intervention activities are listed below according to the level of the organization involved, starting at the group level since this held the most elaborate activities. A more comprehensive description of the intervention components can be found in the study protocol (41).
Group level
The core activities of PIPPI were a series of workshops at the work team level. The workshops were attended by the team workers, their line manager, and a process facilitator who was either a member of the research group or an external consultant.
The first workshop on visual mapping employed a collaborative screening process of the team’s work environment based on the cognitive mapping interview technique (45). To ensure a balanced mapping, both positively and negatively experienced aspects of the work environment1 were targeted (46), using a methodology especially tailored to the study population of industrial blue-collar workers. At the subsequent action planning workshop, the participants used the positively and negatively experienced aspects of the work environment identified at the visual mapping workshop to develop action plans aiming to restore or improve the balance between work demands and resources for the team. Here, another intervention-specific methodology in the form of visual kaizen-inspired boards was introduced. These boards facilitated the prioritization of potential actions plans and also allowed for workers’ systematic follow-up of action plans between workshops. In prioritizing action plans, the participants evaluated how the plans would contribute to productivity, well-being, and product quality as well as their cost-effectiveness. The action planning workshops were held approximately two months after the visual mapping workshops.
The last follow-up workshop evaluated the implementation of the previously developed action plans. To address the risk of lack of implementation (47, 48), the workshop provided an opportunity for the line manager and workers to discuss the implementation of action plans and whether modifications or additional plans were needed. The follow-up workshop was performed two to three months after the action planning workshop.
Individual level
Workers were invited to voluntarily participate in an individual visual mapping talk with their line manager based on the tools from the visual mapping and action planning workshops. Line managers were trained beforehand in conducting these talks and instructed to assist workers in identifying important positively and negatively experienced aspects of the work environment which could affect their work ability. The session resulted in the development of individual action plans if the worker agreed to.
Leader level
At the leader level, an ambassador workshop was conducted at each participating company. Besides line managers, local union representatives and health and safety representatives also participated in parts of the program. The objective was to provide information about the overall aim and background of the intervention and how to support the intervention activities based on a participatory approach. This was done so the participants would be able to handle common questions or decisions at the workplace related to the intervention. Furthermore, the line managers were trained to take a central role in the workshops and individual sessions described above. The participants in the ambassador workshops would meet again after the follow-up workshops in learning workshops to discuss how the participants could support the teams in further implementing action plans.
Organizational level
The research group carried out an audit of the organizational systems, functions, and facilities related to worker’s health and the work environment in order to assess whether they were currently used by the organization members as intended, how their use could potentially be optimized, and how these systems, functions and facilities could potentially be used to support the intervention. The audit results were fed back to local intervention steering committee (including upper and line management, local union representatives, and health and safety representatives) in the individual organizations, and potential courses of action targeting the problems identified by the audit were discussed.
Initiatives supporting intervention implementation
Three overall initiatives were taken to increase the chances of successful implementation. First, the positively and negatively experienced work environment aspects identified at the visual mapping workshop were analyzed, and an overview was provided to the steering committees in each of the participating organizations to help raise issues which were outside the span of control of individual workers or work teams, such as problems related to company policies.
Second, the workplaces were provided with visual boards inspired by the Kaizen boards from lean manufacturing (49, 50). The visual boards were used for monitoring the action plans in the team setting and for facilitating the workers’ development of new action plans. The implementation of action plans in the team was to be discussed monthly or bi-weekly at team meetings, preferably at pre-existing meetings to avoid additional workload for the workers.
A final element of implementation was that intervention work teams were presented with the option of contacting an experienced ergonomic consultant to provide expertise in solving difficult ergonomic issues. Three hours of ergonomic assistance were allotted per work team.
Sample size and randomization
The sample size was calculated prior to the study based on an expected medium effect size of 0.50 SD difference between intervention and control groups in outcome scores at follow-up after correcting for baseline scores. Based on a level of significance (α) of 0.05, a desired statistical power (1-β) of 0.9, a team-level intra-class correlation of 0.05, and an expected variance inflation factor of 1.53 due to correlation between workers in the same work teams (based on 22 workers per team and an intra-team correlation of 0.05), approximately 200 workers in each group would be required.
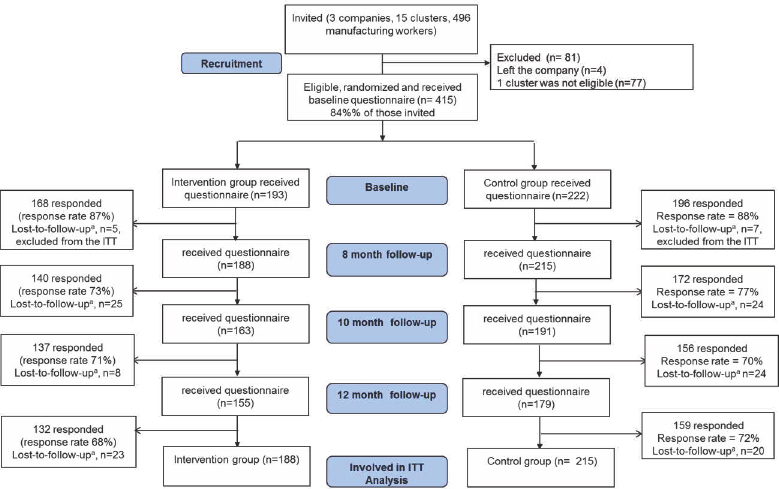
As previously mentioned, the work teams were randomized to either the intervention or control groups utilizing cluster level randomization. Contamination was minimized by assigning teams in geographical proximity or who shared leaders to the same cluster. These clusters were then randomized into either the control or intervention groups using a computer-generated randomization schedule. This means that the number of clusters was somewhat lower than the number of participating work teams (15 clusters versus 21 teams). Accordingly, 494 workers in total were invited to participate, of which 415 workers were included in the randomization. Accordingly, 193 (9 work teams) and 222 (12 work teams) workers were randomized to the intervention and the control group, respectively (figure 1).
Figure 1
Flow diagram of the workers involved at various stages of the PIPPI intervention study. aLoss-to-follow-up was defined as the workers who ended participation after a follow-up measurement (ie, dropped out). Five and seven workers (lost-to-follow-up at the baseline) from the intervention and control group respectively did not respond to any survey rounds and were excluded from the Intention-to-treat (ITT) analysis. As a result, 188 of 215 workers from the intervention group and 215 of 222 workers from the control group were included in the ITT analyses.
Outcome measures
As previously mentioned, evaluating participatory interventions can be challenging as it is not possible to know in advance which problems in the work environment participants choose to address or how. We therefore chose a number of outcome measures covering many different aspects of the work environment based on the expectation that this would enable us to detect an effect of the intervention even if the participants chose to address different problems. The primary outcomes of this study were worker’s recovery and work ability. Secondary outcomes were mental health, well-being, physical work demands, and resources, as well as productivity. All outcomes were measured at baseline and 12-month follow-up while the primary outcomes (ie, recovery and work ability) were also measured using short questionnaires at 8- and 10-month follow-up. The measurement details of all outcomes, descriptive variables and process evaluation measures are shown in Appendix A (www.sjweh.fi/show_abstract.php?abstract_id=3689).
Statistical analysis
To evaluate the effect of the intervention, we applied a multi-level mixed model for the between-intervention and the control group comparisons. We assessed differences from baseline to 8-, 10-, and 12-month follow-up separately for each of the primary outcomes (ie, work ability, recovery), and at baseline and 12-month follow-up for the secondary outcomes (ie, productivity, well-being, mental health and physical demands and resources). The four levels included in the model were time (measurement time points), worker, work team, and company. The multi-level analyses concurrently took into account the clustering of observations of workers within the working team, as well as the repeated measurements within each worker. However, these levels accounted for almost no variance while the individual-level variance was large and thus dominated the other levels. The lower variance of these levels is likely due to the few observation points (for example only three companies) within each level.
For each outcome variable, two analyses were performed: (i) the crude analysis (ie, the assessment of between-group differences at 10- and 12-month follow-up, adjusted for the corresponding baseline on outcome variable) and (ii) the crude analysis with additional adjustment for smoking. Smoking was chosen as a confounder based on theoretical considerations of which background variables were most likely to affect the outcome variable and on the differences between the intervention and control groups at baseline.
For all analyses, the group and measurement time interaction was the intervention effect of interest. P-values <0.05 were considered statistically significant. The analyses were performed according to the intention to treat principle (ITT), including randomized workers responding to questionnaires at least one of the time-points only. Thus, five and seven workers from the intervention and control group, respectively, were excluded from the ITT analyses due to non-response to any questionnaires (figure 1). To assess the presence of bias due to missing outcome response at different data collection time points, the results of the ITT analyses were compared to the per-protocol analyses (ie, including those workers in the analyses who responded to the questionnaires at every time point).
Dropout analysis was performed by comparing descriptive information of the randomized workers who responded to questionnaires at all time points compared to those who did not.
The implementation of PIPPI was measured by determining the dose delivered (ie, number of the intervention activities conducted as planned) and dose received (ie, workers’ participation in the planned intervention activities as measured by responses to questionnaires filled out at each respective intervention activity).
Results
Participants
figure 1 outlines the complete flow of eligible workers for participating in the study from the three participating companies. In total, 496 workers from 15 clusters were invited for intervention information meetings. Of the 496 workers, 4 workers (who left the company) as well as a whole cluster consisting of 77 workers were deemed ineligible for the randomization. The exclusion of a whole cluster from the randomization process was caused by the decision of the company that the cluster would not be able to perform the intervention within the first year due to massive local organizational changes.
Thus, of the remaining 415 workers within 14 clusters, the randomization process allocated 7 clusters in the intervention (N=193) and 7 clusters in the control group (N=222). As 12 workers (ie, 5 and 7 workers from the intervention and control group, respectively) did not respond to any survey rounds, only 403 workers (ie, 188 and 215 workers from the intervention and the control group, respectively) were included in the ITT analyses.
In total, 364 workers responded to the baseline questionnaire (response rate: 88% of those randomized) while 291 workers responded to T3 follow-up (response rate: 70%). In total, 124 workers dropped out (ie, lost to follow-up) of the study during the four survey rounds. Of these, 53 workers left the companies during the intervention period, which corresponds to 43% of the total dropouts. We do not know the reasons for dropping out from the study for the remaining 71 randomized participants.
Table 1 shows the baseline characteristics of the workers in the intervention and the control groups. No significant differences between the intervention and the control groups with respect to age, gender, height, weight, marital/cohabiting status, job seniority, shift work, and working hours were found, but a significant difference in smoking status was observed.
Table 1
Baseline characteristics of the workers in the intervention (N=188) and control (N=215) group participating in the intervention. The baseline characteristics of the workers in control and intervention group were compared using independent t-test for continuous variables and Pearson’s chi-square test for categorical variables. [SD=standard deviation.]
| Variables | Control group (N=215) | Intervention group (N=188) | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Mean | SD | N | % | Mean | SD | N | % | |
| Age (years) | 43.8 | 10.8 | 44.4 | 10.3 | ||||
| Males | 123.0 | 69.5 | 99.0 | 71.2 | ||||
| Height (cm) | 177.3 | 8.7 | 176.7 | 8.4 | ||||
| Weight (kg) | 83.0 | 15.6 | 83.9 | 17.2 | ||||
| Smokers | 65.0 | 36.7 | 35.0 a | 25.2 | ||||
| Cohabitation | 132.0 | 75.0 | 106.0 | 76.8 | ||||
| Job seniority (years) | 10.1 | 8.6 | 11.3 | 9.3 | ||||
| Shift work | ||||||||
| Fixed day work | 78.0 | 44.6 | 64.0 | 46.7 | ||||
| Fixed night work | 24.0 | 13.7 | 15.0 | 10.9 | ||||
| Shift work with/ without night work | 73.0 | 41.7 | 58.0 | 42.3 | ||||
| Work hours (hours) | 37.7 | 3.3 | 37.7 | 3.9 | ||||
| Good health b | 74.0 | 42.3 | 66.0 | 47.5 | ||||
| Need for recovery (0–100%) | 37.3 | 16.1 | 34.5 | 16.5 | ||||
| Work ability (0–10) | 8.3 | 1.4 | 8.5 | 1.5 | ||||
| Productivity (0–10) | 8.1 | 1.4 | 8.3 | 1.3 | ||||
| Physical exertion (0–10), | 5.3 | 2.3 | 5.6 | 2.4 | ||||
| Physical demand scale (1–6) | 3.9 | 0.8 | 3.8 | 0.9 | ||||
| Physical resources scale (0–10) | 5.8 | 1.6 | 6.1 | 1.9 | ||||
| Well-being index (0–100%) | 68.7 | 14.7 | 69.7 | 16.3 | ||||
| Mental health index (0–100%) | 79.9 | 13.7 | 79.3 | 14.6 | ||||
Workers who responded to the questionnaires at all time points were generally similar to those who did not respond to the questionnaires all time points except for being somewhat older, of higher weight and higher job seniority (see Appendix B, www.sjweh.fi/show_abstract.php?abstract_id=3689).
Dose delivered
All of the planned activities were delivered (table 2). This applied both to the 73 compulsory workshops (ie, visual mapping workshop, action planning workshop, and follow-up workshop) and that all voluntary individual visual mapping sessions and ergonomic workshops intervention activities were offered.
Table 2
Descriptive of the dose delivered and received among industrial workers in the intervention group participating in the physical and psychosocial intervention for balancing the demands and resources of industrial workers (PIPPI, N=193) a
| Intervention activities | Dose delivered | Dose received | ||
|---|---|---|---|---|
|
|
|
|||
| Planned N | Delivered % | N | % b | |
| Visual mapping workshop | 24 | 100 | 145 | 75 |
| Action planning workshop | 24 | 100 | 137 | 71 |
| follow-up workshop | 25 | 100 | 119 | 61 |
| Individual visual mapping talk | - | - | 71 | 37 |
| Ergonomic workshop | - | - | 63 | 32 |
Dose received
Table 2 shows the number of workers who participated in each of the intervention activities. 75%, 71% and 61% of the workers in the intervention group participated in the compulsory visual mapping workshop, action planning workshop, and follow-up workshop, respectively. We have no direct information from workers about the reasons for non-participation in the compulsory intervention activities. Typically, the verbal information offered by coworkers and managers in workshops was that the non-participation was caused by sick leave, training or production emergencies. 37% and 32% of the intervention group participated in the voluntary individual visual mapping talk and ergonomic workshops, respectively.
On average for each work team, 15 positive and 17 negatively experienced aspects of the work environment were identified in the visual mapping workshop, and the mapped aspects spanned a number of areas, including prevention of musculoskeletal disorders, improving the social relations among the employees, reducing stressful errors or unnecessary tasks, or improving aspects of the work environment related to the employees’ comfort (see Appendix C for examples, www.sjweh.fi/show_abstract.php?abstract_id=3689). In the action planning workshops, about seven action plans were developed on average per work team. Similar to the mapped positively and negatively experienced aspects, the actions plans targeted a breadth of factors, both physical and psychosocial in the work environment (see Appendix C). It should also be noted that the action plans were quite different in scope, ranging from small and easily-implemented to action plans that were unlikely to be implemented during the one-year follow-up period.
Regarding the action plans, five process evaluation questions focused on the relevance and implementation. Of the participants, 76% reported agreeing (partially to highly) that they have discussed the action plans in their team, for instance on meetings, and 72% reported agreeing (partially to highly) that they have had time allocated to work on the action plans; 75% reported having continuously revisited the action plans, and 79% reported having implemented the planned plans. Finally with regards to the relevance of the action plans, 84% (partially to highly) agree that they were targeting the most important problems.
On an overall project level, 83% of the responding workers in the intervention group at 12 months follow-up had a positive opinion about the activities in PIPPI, and 73% of the intervention group responded that they agreed to the PIPPI activities having led to lasting changes at the workplace at 12 months follow-up. Additionally, 59% of them would like the workplace to continue using the activities in PIPPI, and only 6 % responded that they would not, while 35% replied that they did not know.
Intervention effects
Results of the intention-to-treat (ITT) analyses
Table 3 shows the averages for work ability, recovery, physical demands and resources, physical exertion, well-being, mental health and productivity at baseline and at 8-, 10- and 12-month follow-up stratified on the control and intervention groups. Additionally, the intervention effects on these outcomes using ITT analyses are reported in table 3. No statistically significant overall effects on any of the outcomes were found. However, a tendency towards an overall increased poor recovery in the intervention group was found, which was significant at the 10- and 12-month follow-up. Adjustment for smoking in the statistical models did not modify the results.
Table 3
Descriptive of work ability, need for recovery, productivity, physical work demands and resources, physical exertion at work mental health and well-being and their differences between the intervention and control groups at 8-, 10- and 12-month follow-up in the intention-to-treat analysis. [SD=standard deviation; β=estimated difference between the intervention and control group from the statistical models; 95% CI= 95% confidence intervals.]
| Variable | Control group | Intervention group | Model 1 a | Model 2 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||||
| M | SD | M | SD | β | 95% CI | P-value | β | 95% CI | P-value | |
| Primary outcomes | ||||||||||
| Need for recovery | ||||||||||
| Baseline | 37.28 | 16.13 | 34.47 | 16.52 | ||||||
| 8-months | 39.80 | 18.29 | 35.84 | 16.86 | -2.51 | -6.97–1.95 | 0.25 | -2.29 | -6.91–2.34 | 0.31 |
| 10-months | 39.17 | 17.80 | 38.84 | 18.85 | 4.17 | 0.19–8.15 | 0.04 | 4.15 | 0.16–8.14 | 0.04 |
| 12-months | 37.60 | 18.30 | 37.50 | 18.32 | 4.32 | 0.33–8.31 | 0.03 | 4.30 | 0.31–8.29 | 0.04 |
| Overall effect | 0.06 | 0.06 | ||||||||
| Work ability | ||||||||||
| Baseline | 8.29 | 1.39 | 8.55 | 1.46 | ||||||
| 8-months | 8.45 | 1.33 | 8.59 | 1.21 | -0.00 | -0.32–0.31 | 0.98 | -0.01 | -0.33–0.31 | 0.93 |
| 10-months | 8.64 | 1.15 | 8.48 | 1.28 | -0.28 | -0.63–0.07 | 0.11 | -0.28 | -0.62–0.06 | 0.10 |
| 12-months | 8.36 | 1.23 | 8.31 | 1.49 | -0.10 | -0.45–0.26 | 0.58 | -0.09 | -0.46–0.27 | 0.60 |
| Overall effect | 0.25 | 0.24 | ||||||||
| Secondary outcomes | ||||||||||
| Productivity | ||||||||||
| Baseline | 8.09 | 1.42 | 8.26 | 1.27 | ||||||
| 12-months | 8.31 | 1.24 | 8.47 | 1.39 | 0.03 | -0.38–0.44 | 0.88 | 0.02 | -0.39–0.42 | 0.92 |
| Physical exertion at work | ||||||||||
| Baseline | 5.33 | 2.32 | 5.60 | 2.45 | ||||||
| 12-months | 5.47 | 2.20 | 5.88 | 2.24 | 0.36 | -0.14–0.87 | 0.15 | 0.37 | -0.14–0.87 | 0.15 |
| Physical demands | ||||||||||
| Baseline | 3.92 | 0.79 | 3.82 | 0.95 | ||||||
| 12-months | 3.89 | 0.83 | 3.82 | 0.83 | -0.02 | -0.16–0.12 | 0.78 | -0.02 | -0.16–0.12 | 0.78 |
| Physical resources | ||||||||||
| Baseline | 5.82 | 1.62 | 6.12 | 1.88 | ||||||
| 12-months | 6.14 | 1.65 | 6.11 | 1.71 | -0.02 | -0.34–0.30 | 0.89 | -0.05 | -0.37–0.27 | 0.74 |
| Well-being index | ||||||||||
| Baseline | 68.75 | 14.71 | 69.68 | 16.28 | ||||||
| 12-months | 69.44 | 15.57 | 70.10 | 16.14 | -0.98 | -5.32–3.35 | 0.60 | -0.79 | -5.17–3.59 | 0.68 |
| Mental health | ||||||||||
| Baseline | 79.88 | 13.75 | 4.97 | 0.73 | ||||||
| 12-months | 79.33 | 14.56 | 5.03 | 0.81 | 0.02 | -0.13–0.18 | 0.79 | 0.02 | -0.13–0.18 | 0.77 |
Results of the per-protocol analyses
The results of the per protocol analyses (Appendix D, www.sjweh.fi/show_abstract.php?abstract_id=3689) were similar to the results of the ITT analyses, except that the difference in the development of work ability between the groups became statistically significant. Specifically, the intervention group had a significant decrease in work ability compared to the control group at 10-month follow-up. The adjustment for smoking in the statistical models did not modify the results. In addition, after adjusting for smoking, there was a non-significant (P=0.09) trend towards decreased physical resources in the intervention relative to the control group at 12-months follow-up. The results of per protocol analyses for other outcomes, ie, recovery, physical demands, physical exertion, well-being, mental health, and productivity were similar to those obtained in the ITT analyses.
Discussion
The present study showed that the PIPPI intervention was not effective in improving either the primary outcomes recovery and work ability or the secondary outcomes of workers’ physical demands and resources, physical exertion, well-being, mental health, and productivity among industrial workers from three companies in Denmark.
The results of no improvement in work ability and recovery from workplace interventions are in line with several previous studies (25–29, 34). We also observed an overall tendency of poorer recovery (being statistically significant at 10- and 12-month follow-up) and decreased work ability (in the per protocol analyses) among intervention group compared to control group. Similarly, we observed no improvement in our secondary outcome, work productivity, and physical work demands and resources, mental health and well-being index which corroborate many previous studies (26, 29, 51). Several possible explanations can be offered: for one, we might have observed a regression-toward-the-mean effect, as the intervention group started out with slightly favorable scores on a number of the outcomes. Relatedly, when randomizing participants at a cluster rather than an individual level, events unrelated to the intervention are more likely to affect the intervention and control groups differently, potentially introducing changes in the outcomes that blend with any effects from the intervention, thereby creating falsely augmented or diminished effect sizes. Another potential reason for an adverse effect of the intervention could be that participating in the workshops and implementing actions plans presents an additional work task, which might lead to higher overall work-related demands and effort from the participants. For example, in one company, because of logistical reasons, workshops were required to be held on days where the workers were off-duty, causing the workers to go to work and attend workshops instead of being at home. The potential adverse effects on poor recovery and work ability from participating in intervention activities might be a particular concern for blue-collar workers already facing high demands and efforts at work.
The failure of PIPPI to improve recovery and work ability could either be explained by a theory failure (ie, the program theory being erroneous) or implementation failure (ie, inadequately designed or implemented), or a combination of both (52). However, it seems unlikely that the lack of effects can be attributed to implementation failure alone due to the fact that (i) 100% of the planned intervention workshops were delivered, (ii) there was a moderate-to-high participation rate (61–75%), (iii) workers identified many issues to be addressed and planned several action plans to solve these issues, and (iv) a high percentage of intervention group workers reported being satisfied with the activities (83%) and that the action plans for solving the issues were implemented as planned (79%). However, because the practical implementation of action plans occurred at different worksites and around the clock at the employees’ discretion, it was not possible to directly monitor the implementation of action plans. Since action plans could rarely account for all contingencies involved in implementing the proposed solutions, the plans typically described the first few steps towards a solution, making it possible that some employees have reported the implementation rate based on whether these were carried out, rather than whether the proposed solution was eventually implemented as intended.
On the other hand, the lacking positive effects from PIPPI could be caused by theory failure. For example, the implemented action plans might not sufficiently reflect the predetermined outcomes. Because the problems chosen to be targeted and the resulting actions plans to be implemented are unknown a priori in participatory interventions (41), there is an increased risk for a mismatch between the implemented intervention activities and the measured outcomes, and thus theory failure. To meet this challenge of evaluating participatory interventions, we chose rather broad primary and secondary outcomes that might potentially be influenced by a large variety of implemented intervention activities related to balancing the work demands and resources of the workers. However, while the problems identified were relevant to the workers, and appropriate actions planned were developed and implemented during intervention, these actions might not have been sufficiently focused on the predetermined primary and secondary outcomes, which would explain the findings of the study.
Strengths, limitations, and methodological consideration
A strength of the study is the cluster RCT design, inclusion of the three companies of different sizes and industries within manufacturing, and the inclusion of intervention and control groups within each company. Another strength is the multiple measurements of recovery and work ability, which provide additional statistical power. Additionally, employing a relatively long follow-up period of one year and 100% dose delivered of the intervention are strengths of the study.
Limitations of the study include the inability to collect specific information about which action plans were completed and the specific reasons for workers dropping out from the study. Another limitation is that the data was collected via questionnaires which generally induce a potential risk of reporting bias, for example for physical work demands (53, 54).
One of the methodological considerations in this study is that the workers who responded to all survey rounds (those involved in per protocol analyses) and those who did not respond to all survey rounds were predominantly similar in baseline characteristics except that the former group was slightly older, heavier, and had high job seniority. However, the results, analyzed using the per-protocol design, were similar to those obtained via ITT analyses. This indicated that the effect of the intervention was not affected by the non-adherence or deviation from the protocol. A limitation of the study was that psychosocial demands were not measured. Instead, we used, as per the study protocol (41), the WHO5 (5-item World Health Organization Well-Being Index) and well-being index, which are indicators of mental health, and not psychosocial demands per se. The reason for not including specific psychosocial work demands was that the participants could choose to intervene on numerous different psychosocial demands or resources (eg, influence at work, predictability, effort–reward (im)balance, emotional demands, social support, etc.), but that only a small number of participants would likely implement action plans influencing any of these outcomes specifically, thereby leaving our analysis clearly underpowered. Another limitation is the aforementioned issue of evaluating participatory interventions because in this kind of intervention, the predetermined outcomes are not necessarily being specifically targeted and are not tailored to the identified problems, actions plans, and implementation by the individual workers. This issue is also listed in the study protocol as an inherent risk of participatory designs such as the one used in PIPPI (41). Thus, effective evaluation methodologies better suited to address the challenges posed by participatory interventions, such as the diversity in problems identified and action plans developed and their potentially weak relation to pre-decided outcome variables, should be developed.
Concluding remarks
In conclusion, our participatory physical and psychosocial intervention for balancing the demands and resources of industrial workers was not effective in improving work ability, recovery, productivity, physical exertion, physical demands and resources, well-being or mental health.
This result can have several explanations. There could have been a regression-toward-the-mean effect, the intervention could have put an additional burden on the participating industrial workers who already faced high work demands, there could have been an insufficient match between the intervention components implemented and the predetermined primary and secondary outcomes, or implementation failure could have occurred. These potential explanations of the results will be further investigated using extensive process evaluation data.



